Abstract
Background
Laparoscopic sleeve gastrectomy (LSG) is an accepted bariatric procedure. Swallow studies (SS) after LSG are not uniform and display different patterns with regard to contrast passage through the gastric sleeve. The impact of immediate postoperative contrast transit time on weight loss has not been studied. The influence of immediate fluid tolerance on weight loss after LSG is herein reported.
Methods
Ninety-nine patients after LSG were included. There were 67 females, mean age 41 (range 17–67), mean BMI 44.4 (range 37–75). A routine SS was performed on postoperative day (POD) 1. Pattern of contrast transit was noted. Patients were followed-up in our bariatric clinic.
Results
Percent excess weight loss was significantly lower in the patients with rapid contrast passage (Group 1, n = 50) than those with delayed passage (Group 2, n = 49). Group 1 achieved 62, 58, and 53 % at 1, 2, and 3 years, respectively, while Group 2 attained 69, 74, and 75 % at the same time points (p = 0.05, 0.001, and 0.04, respectively). Group 1 patients displayed a negative weight loss trend after 1 year whereas Group 2 patients plateaued after 2 years.
Conclusions
Tolerance of fluid intake after LSG is crucial for patient recovery and discharge. Distinct radiologic appearance on POD 1 helps predict this behavior. Mid-term weight loss after LSG appears to be dependent on immediate postoperative contrast transit time, whereas patients with slow contrast passage tend to lose more weight. Long-term follow-up will reveal whether this finding will hold true.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic sleeve gastrectomy (LSG) is an accepted bariatric procedure that has gained popularity over the last decade both with bariatric surgeons and patients. Its appeal is in its relative operative simplicity and lower risk profile, along with promising short and mid-term weight loss outcomes. The mechanism of weight loss is a combination of restriction and induction of favorable hormonal changes.
When implemented, water-soluble contrast-swallow studies (SS) are performed 1–2 days postoperatively [1–4]. Some surgeons utilize this test routinely, while others only in selected cases with clinical suspicion of leak or stricture [5–8]. There is yet no consensus regarding this issue.
In a previously published work, we identified two different patterns of contrast passage after LSG [9]. The patients with rapid contrast transit (<30″) tolerated oral fluids significantly better and were thus discharged earlier than those with hindered contrast flow (>30″). The purpose of the present study is to present follow-up after sleeve gastrectomy in light of postoperative swallow study patterns and ascertain whether the radiologic appearance noted immediately after surgery has any long-term influence.
Patients and Methods
We retrospectively analyzed our prospectively collected bariatric database regarding patients undergoing LSG in a single university hospital, between 2007 and 2010.
Ninety-nine consecutive patients (67 females) following LSG for morbid obesity were included, all fulfilling the 1991 NIH consensus criteria for bariatric surgery [10]. The mean age and BMI were 41 years (range 17–67) and 44.4 kg/m2 (range: 37–75), respectively.
Surgery was performed using a four-port technique to resect the greater curvature of the stomach using endoscopic linear staplers (Echelon 60 Endopath Stapler®, Ethicon Endosurgery, Cincinnati, OH) alongside a round-tipped silicone bougie (Pilling® Hurst Bougie Tungsten, Teleflex Medical, High Wycomb, UK). A fifth port was occasionally added for additional retraction. The stapler line was not oversewn. The bougie size used in the procedure was initially 46 F (n = 6), later the size was tapered to 42 F (n = 21), and finally to 32 F (n = 72).
A routine SS with water-soluble contrast material (Telebrix Gastro®, Guerbet, France) was performed on all patients on postoperative day (POD) 1. The time from contrast entrance into the sleeve to contrast flow into the duodenum was recorded. The patients were divided into two groups, according to the transit time.
Group 1 consisted of 50 patients who showed rapid contrast flow through the sleeve (transit time <30″). Group 2 consisted of 49 patients with delayed contrast flow through the sleeve (transit time ≥ 30″). Clear fluids were initiated on POD1 if no leak or obstruction was detected. Patients were discharged when they could tolerate a daily fluid intake of 2 L. Perioperative data, including operative time, estimated blood loss (EBL), intra- and postoperative morbidity and length of hospital stay were collected.
All patients were followed-up in our bariatric clinic according to our standard schedule. At each office visit, the patients would meet their surgeon and a dedicated dietician. Anthropometric measurements, percent excess weight loss (%EWL), as well as medication use, food tolerance, physical activity, and periodical lab tests were collected.
Statistical Analysis
Data are presented as mean values ± standard deviation. Paired student's t test was used for continuous normally distributed variables. Pearson correlation coefficient (r) and the significance for it (p) were calculated between variables. Statistical significance was considered as a probability of a type-1 error <5 %.
Results
There was no significant difference between the baseline characteristics of the two groups (Table 1). Average age and BMI for Groups 1 and 2 were 39 ± 11 years vs. 41 ± 12 years (p = 0.3) and 45 ± 6 vs. 44 ± 8 kg/m2 (p = 0.7), respectively. No mortalities, obstructions, or leaks occurred in the study period. As in our previously reported data, no correlation between bougie size and transit time was found.
Group 1 patients (transit time <30″, n = 50) tolerated oral fluids better and were thus discharged significantly earlier than Group 2 patients (transit time ≥30″, n = 49): 2.1 days vs. 3.6 days (p < 0.001).
During the first 6 months postoperatively, %EWL was practically identical between the two groups but diverged significantly from one year on (Fig. 1). Percent excess weight loss was 16, 34, 55, 62, 58, and 53 for Group 1 and 19, 33, 56, 70, 74, and 75 for Group 2 at 2 weeks, 2 months, 6 months, 1, 2, and 3 years, respectively (p = 0.05, 0.001 and 0.04 for the last 3 time points, respectively). Group 1 patients displayed a negative weight loss trend after 1 year whereas Group 2 patients continued to lose weight and plateaued after 2 years.
Percent excess weight loss (EWL) during follow-up of Group 1 (patients with rapid contrast transit time) and Group 2 (patients with delayed contrast transit time). Group 1 had a negative weight loss trend after 1 year, whereas Group 2 continued to lose weight and plateaued after 2 years. asterisk statistically significant difference, w weeks, m months
Perioperative characteristics were similar between the two groups (Table 1). EBL was 47 ± 53 ml and 51 ± 60 ml for groups 1 and 2, respectively (p = 0.82). Operative times for Groups 1 and 2 were 101 ± 42 min and 123 ± 43 min, respectively (p = 0.016). A history of previous bariatric procedures was present in 16 and 22 % of patients in Groups 1 and 2, respectively (p = 0.45; no difference in type of previous procedures). Patients were evenly distributed between the two groups regardless of their order in our series.
Discussion
Sleeve gastrectomy is a bariatric option gaining popularity worldwide. The proposed mechanism of action of this procedure is a combination of volume restriction, creation of a high-pressure system, and the induction of a favorable hormonal change [11]. Low plasma ghrelin levels were monitored up to 5 years after LSG [12]. Gastric emptying in obese individuals has been reported to be slower, faster, or the same as their lean counterparts [13]. Different authors, using various methods report conflicting results regarding gastric transit time following LSG [14–16].
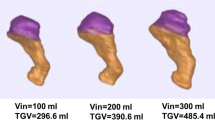
Sleeve gastrectomy is, at least partially, a restrictive bariatric procedure. It was assumed that the degree of restriction, as expressed by contrast transit through the sleeve, would impact on postoperative weight loss, at least in the short term. Several factors influence the degree of restriction.
The diameter of the sleeve: the thinner the sleeve, the less volume it has. This is determined by the bougie size selected for the procedure and by further constriction by staple line suturing, if performed. It should be noted that stomach tissue thickness potentially influences sleeve volume, but this factor is difficult to assess. Bougie size varied in our series but was not found to be correlated with transit time. Since this factor was not in the study design, it is possible that its effect was not detected due to small sample size of the larger bougies. Smaller bougie size is correlated to better weight loss results but, unfortunately, also to higher leak rates [17, 18].
Amount of Retained Antrum
Distance from the pylorus where stomach resection begins may influence both sleeve volume and sleeve emptying via the “antral mill” effect. Some authors strongly advocate retaining the antrum, arguing that the volume of the contracted antrum is negligible and that its function in facilitating gastric emptying is crucial [19]. Others report this potential reservoir to dilate and eventually lead to sleeve failure, recommending resection margin close to the pylorus [20]. The antrum contains ghrelin-producing cells, though to a lesser extent than the fundus so its resection might influence sleeve efficacy through another mechanism [21]. The recently published international sleeve gastrectomy expert panel consensus statement stated that resection should be initiated 2–6 cm from the pylorus (92 % consensus of the panel) [18]. We routinely begin our resection 5 cm from the pylorus. As this was uniform for all our patients, the difference in transit time cannot be attributed to this variable.
Retained Fundus
Fundic resection is of paramount importance in sleeve gastrectomy, both for maximal ghrelin cell removal, and excision of the region most amenable to stretch [19, 21]. When insufficient exposure of the posterior aspect of the stomach occurs, some of the fundus might be retained and cause both an inferior restriction (larger volume) and a delay of sleeve emptying due to pooling of contents in this reservoir, above a tight distal sleeve. In reviewing the radiographs in this study, we found 11 patients with a small retained fundus, not significantly different in distribution between the groups (four in Group 1 and seven in Group 2; p = 0.36).
A slightly longer operative time was found for the longer transit time group, which was statistically significant (20 min longer, p = 0.016). The clinical impact as far as operative time is not clear but it may hint at technically more challenging cases which resulted in diminished gastric emptying. This might be attributed to motility disturbance due to edema caused by more tissue manipulation in difficult cases. Other factors may be in play but no clear conclusions can be made at this point.
Contrary to our expectations that immediately after surgery patients with slower transit time would lose weight more rapidly, initial weight loss was practically identical between the two groups in the first 6 months. The %EWL diverged significantly at the 1-, 2-, and 3-year time points. It is possible that during the first few months all patients consume very small amounts owing to the drastic change in capacity and hunger sensation, and that the difference in sleeve emptying is not noticeable. After 6 months, and closer to a year from surgery, the patients with the more “efficient” sleeve (with slower postoperative transit time as a marker), continue to lose weight whereas those with a more pliable sleeve (faster postoperative transit time as a marker) are able to ingest more and thus demonstrate a negative weight loss pattern. It would be interesting to see if this trend will continue into longer follow-up periods.
We can hypothesize that the patients with type 1 pattern (rapid contrast transit) had a more lax sleeve and therefore had a propensity for sleeve dilatation and poorer long-term results and that the patients with type 2 pattern (slow contrast transit) tended to keep a “tighter” sleeve and therefore lose weight and maintain it, at least at the 3 year mark. However, since this was a retrospective study, looking at prospectively collected data but not designed to look into radiologic patterns during follow-up, we have no data regarding radiologic appearance of our patients’ sleeve after the initial POD 1 study. A prospective study designed to look at the “natural history” of sleeve morphology is warranted, but it is questionable whether review board approval will be awarded a study with multiple ionizing radiation exposures performed for this purpose only.
There is no consensus regarding the utilization of SS after bariatric surgery. Several surgeons use this modality routinely, while others advocate a more selective approach [5–8]. SS is performed in order to rule out complications, mainly leak and obstruction, and to give the surgeon a subjective feedback and documentation of his handiwork. This sometimes proves valuable when evaluating patients who have gained weight or lost their restriction several months or years postoperatively. A comparison of SS pictures from the present to those obtained immediately after surgery can shed some light as to the pathogenesis of this problem.
This study has some limitations. The study population is not uniform. There are patients that underwent primary sleeves and those who had SG as a conversion, mostly from LAGB (19 %). However, these patients were present in both groups in a similar proportion that did not reach statistical significance. In addition, various bougie sizes were used but no correlation was found between the size and transit time. This study was not designed to look for bougie size impact and the vast majority (71 %) had the same bougie (32 F). Finally, we did not perform volume assessment of the sleeves using the SS. This parameter is possibly important in long term outcome [11, 19].
In conclusion, we have found that contrast transit time pattern through the newly constructed sleeve, as depicted in SS performed shortly after sleeve gastrectomy, might be important as a predictor of future sleeve function. This is beyond the controversial, “classical” role of SS for complication detection and structural appraisal.
References
Ferrer-Marquez M, Belda-Lozano R, Ferrer-Ayza M. Technical controversies in laparoscopic sleeve gastrectomy. Obes Surg. 2012;22:182–7.
Keren D, Matter I, Rainis T, et al. Getting the most from the sleeve: the importance of post-operative follow-up. Obes Surg. 2011;21:1887–93.
Ortega E, Morinigo R, Flores L, et al. Predictive factors of excess body weight loss 1 year after laparoscopic bariatric surgery. Surg Endosc. 2012;26:1744–50.
Roa PE, Kaidar-Person O, Pinto D, et al. Laparoscopic sleeve gastrectomy as treatment for morbid obesity: technique and short-term outcome. Obes Surg. 2006;16:1323–6.
Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity. Surg Endosc. 2006;20:859–63.
Dallal RM, Bailey L, Nahmias N. Back to basics--clinical diagnosis in bariatric surgery. Routine drains and upper GI series are unnecessary. Surg Endosc. 2007;21:2268–71.
Kolakowski Jr S, Kirkland ML, Schuricht AL. Routine postoperative upper gastrointestinal series after Roux-en-Y gastric bypass: determination of whether it is necessary. Arch Surg. 2007;142:930–4. discussion 934.
Melissas J, Koukouraki S, Askoxylakis J, et al. Sleeve gastrectomy: a restrictive procedure? Obes Surg. 2007;17:57–62.
Goitein D, Goitein O, Feigin A, et al. Sleeve gastrectomy: radiologic patterns after surgery. Surg Endosc. 2009;23:1559–63.
NIH Conference. Gastrointestinal surgery for severe obesity. Consensus development conference panel. Ann Intern Med. 1991;115:956–61.
Yehoshua RT, Eidelman LA, Stein M, et al. Laparoscopic sleeve gastrectomy—volume and pressure assessment. Obes Surg. 2008;18:1083–8.
Bohdjalian A, Langer FB, Shakeri-Leidenmuhler S, et al. Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin. Obes Surg. 2010;20:535–40.
Buchholz V, Berkenstadt H, Goitein D, et al. Gastric emptying is not prolonged in obese patients. Surg Obes Relat Dis. 2012. doi:10.1016/j.soard.2012.03.008
Bernstine H, Tzioni-Yehoshua R, Groshar D, et al. Gastric emptying is not affected by sleeve gastrectomy—scintigraphic evaluation of gastric emptying after sleeve gastrectomy without removal of the gastric antrum. Obes Surg. 2009;19:293–8.
Melissas J, Daskalakis M, Koukouraki S, et al. Sleeve gastrectomy—a "food limiting" operation. Obes Surg. 2008;18:1251–6.
Shah S, Shah P, Todkar J, et al. Prospective controlled study of effect of laparoscopic sleeve gastrectomy on small bowel transit time and gastric emptying half-time in morbidly obese patients with type 2 diabetes mellitus. Surg Obes Relat Dis. 2010;6:152–7.
Gagner M. Leaks after sleeve gastrectomy are associated with smaller bougies: prevention and treatment strategies. Surg Laparosc Endosc Percutan Tech. 2010;20:166–9.
Rosenthal RJ. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8:8–19.
Weiner RA, Weiner S, Pomhoff I, et al. Laparoscopic sleeve gastrectomy–influence of sleeve size and resected gastric volume. Obes Surg. 2007;17:1297–305.
Baltasar A, Serra C, Perez N, et al. Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation. Obes Surg. 2005;15:1124–8.
Goitein D, Lederfein D, Tzioni R, et al. Mapping of ghrelin gene expression and cell distribution in the stomach of morbidly obese patients-a possible guide for efficient sleeve gastrectomy construction. Obes Surg 2012;22:617–22.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goitein, D., Zendel, A., Westrich, G. et al. Postoperative Swallow Study as a Predictor of Intermediate Weight Loss after Sleeve Gastrectomy. OBES SURG 23, 222–225 (2013). https://doi.org/10.1007/s11695-012-0836-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0836-4