Abstract
Background
The goal of this study is to compare the outcomes of laparoscopic adjustable gastric banding (LAGB) and laparoscopic Roux-en-Y gastric bypass (LRYGB) in obese adolescents.
Methods
We performed a retrospective review of all adolescents between the ages of 15 and 19 who underwent LAGB or LRYGB at our university affiliated Bariatric Center of Excellence from 2002 to 2011. Postsurgical weight loss at 1, 3, 6, 12, 18, and 24 months was noted and expressed as percentage of excess weight loss (% EWL).
Results
Thirty-two patients underwent LRYGB and 23 underwent LAGB. The LAGB group was younger (18.6 ± 0.6 versus 17.2 ± 1.5) than the LRYGB group. Other preoperative demographic factors including body mass index, gender, ethnicity, and comorbidities were similar between the two groups. The average % EWL was superior in the LRYGB group compared to the LAGB group at all time points studied (p < 0.05), although at 2-year follow-up, only 16 % (5/32) LRYGB and 30 % (7/23) LAGB patients were available for follow-up. Three patients with type II diabetes mellitus underwent LRYGB and all experienced remission of their diabetes. The number of complications requiring interventions was similar between the two groups.
Conclusions
In our study, adolescents undergoing LRYGB achieved superior weight loss compared to LAGB in the short-term follow-up. The complication rate for LAGB was similar compared to LRYGB. More studies are needed to monitor the long-term effects of these operations on adolescents before definitive recommendations can be made.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity in the adolescent population has reached epidemic proportions and become a major public health concern in the USA. Approximately 32 % of adolescents under the age of 19 are above the 85th percentile, and 17 % are above the 95th percentile for their aged-matched body mass index (BMI) [1]. Obese adolescents are at a significantly increased risk of becoming obese adults [2]. They also have an increased risk for developing diabetes mellitus (DM), hypertension, obstructive sleep apnea, hyperlipidemia, and premature mortality from coronary artery disease [3, 4]. In addition, obesity has a significant adverse impact on psychosocial well-being in adolescents [5].
Bariatric surgery continues to be the only option to provide effective and durable weight loss for morbidly obese adolescents compared to lifestyle changes [6]. In the past decade, bariatric operations have become safer and more widely adopted. The total number of bariatric operations performed in the USA has increased over ninefold since the early 2000, while bariatric case volume in the adolescent population has seen a threefold increase during the same time period [7–9].
Laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic adjustable gastric banding (LAGB) are the operations mostly commonly offered to obese adolescents [10–13]. However, no study has yet directly compared the results of these two operations in this population. The goal of this study is to compare the outcomes of these two procedures over a short-term follow-up in adolescents.
Methods
We performed a retrospective review of prospectively collected data after obtaining approval from the institutional review board. We studied 55 patients between the ages of 15 and 19 years who underwent LRYGB or LAGB performed at our Bariatric Center of Excellence from 2002 to 2011. All patients in our study met the National Institute of Health consensus guideline for bariatric surgery [14].
Prior to surgery, all patients in our cohort underwent a trial of exercise and diet under the guidance of our nutritionists. Only those who completed the trial were offered a bariatric operation for the treatment of their obesity. In addition, all patients attended mandatory educational sessions and underwent comprehensive psychological and nutritional evaluations before being offered an operation.
The decision to perform LRYGB versus LAGB was made on an individual basis by the surgeon in discussion with the patient. All patients were counseled on the specific risks associated with LRYGB and LAGB. Additionally, patients were informed of the general risks associated with abdominal operations. Specifically, we discussed the irreversible nature of LRYGB and the possibility of developing macro and micro nutrition deficiency due to the operation. Patients choosing LAGB were specifically informed of the risks associated with the band including slippage and migration.
LRYGB was performed by using three 5 mm-, one 12 mm-, and one 15 mm port. A 40-cm biliopancreatic limb and a 100-cm alimentary limb were constructed. The Roux limb was positioned in a retrocolic retrogastric fashion, and a linear gastric pouch of approximately 30 ml volume was created along the lesser curvature. Anastomosis was fashioned with the stapler or hand-sewn technique and all mesenteric defects were closed with suture.
LAGB was performed with three 5 mm-, one 12 mm-, and one 15 mm port. Pars flaccida technique was used to place the band on the proximal stomach and a gastrogastric suture placed to prevent migration and slippage of the band. Access to the abdomen was gained in the majority of cases with the use of Endopath®Xcel® trocars with Optiview Technology (Ethicone, Cincinnati, OH) for both LAGB and LRYGB. Band adjustments were made on follow-up visits as needed by removing or adding saline to the band tubing.
Postoperatively, all patients who underwent LRYGB were started on multivitamins. Routine postoperative laboratory values including cholesterol, vitamin D, iron, and vitamin B1 and B12 values were obtained on follow-up visits, and deficiencies were treated as needed with oral supplements.
Preoperative patient demographics, comorbidities, and BMI were noted. Postoperative weight loss was the primary endpoint, with adverse outcomes and comorbidity resolution being secondary endpoints. We compared weight loss between the two groups by using the excessive weight loss (% EWL) in percentage. EWL was calculated by using the following formula.
\( \% {\text{ EWL}} = { }\left[ {{{{\left( {{\text{Preoperative weight}} - {\text{Follow - up weight}}} \right)}} \left/ {{\left( {{\text{Preoperative weight }} - {\text{ Ideal body weight}}} \right)}} \right.}} \right] \times {1}00 \) [15].
All statistical analysis was performed on SPSS version 17 for Windows (Chicago, IL). Continuous variables were compared with Student’s t test and categorical variables were compared using chi-square test. In addition, all weight loss data were plotted on a scatter plot, and a linear regression model was constructed for LRYGB and LAGB. All tests were two-tailed and p value < 0.05 was considered significant.
Results
There were 32 LRYGB and 23 LAGB performed in our cohort of 55 patients. Patient demographics are shown in Table 1. The average age of the LAGB group was lower compared to the LRGYB group. The BMI, gender composition, and obesity related comorbidities in the two groups were similar. The age distribution of patients in this cohort is shown in Fig. 1.
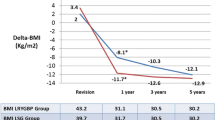
The scatter plot and the linear regression models reveal that patients who underwent LRYGB are more likely to achieve significant weight loss up to 2 years compared to those who underwent LAGB (Fig. 2). In addition, the average EWL achieved by the LRYGB group was superior compared to LAGB group at all studied time points (Table 2). Of note, at 2 year follow-up, only 16 % (5/32) LRYGB and 30 % (7/23) LAGB patients were still available for follow-up.
In terms of adverse outcomes, two patients who underwent LAGB required revisions. One patient had a band slippage requiring surgical intervention while the other patient elected to have the band removed. One patient who underwent LRYGB was re-admitted to the hospital for dehydration while a second patient developed a gastrogastric fistula 3 years postoperatively requiring repair.
There were three patients with type II DM in the LRYGB group requiring oral hypoglycemics and none in the LAGB group. All patients experienced remission of their DM, no longer requiring medications with all HgbA1c levels falling below 6.5. In addition, two patients in the LRYGB group and two in the LAGB group had dyslipidemia defined as total cholesterol greater than >200 mg/dl. Both patients in the LRYGB experienced resolution of dyslipidemia and no longer required with medications while only one patient from the LAGB had a similar outcome.
Preoperatively, seven patients were found to be iron deficient (five in LRYGB, two in LAGB group), while 18 patients had vitamin D deficiency (13 in LRYGB and 2 in LAGB group). There was no vitamin B12 deficiency in the cohort preoperatively. At 2 year follow-up, we did not detect vitamin B12 deficiency in this cohort, although only 12 patients were still available for follow-up. Of the 12 patients at follow-up, two patients had vitamin D deficiency, while one patient was found to have iron deficiency. Finally, one patient who underwent LRYGB developed schizoaffective disorder 2 years after the operation.
Discussion
The prevalence of adolescent obesity has reached critical levels in the USA [16]. Obese adolescents are at increased risk for becoming obese adults and are more likely suffer comorbidities and experience premature mortality compared to their peers [5, 17–20]. In addition, obese adolescents are more likely to experience negative psychosocial effects, which often translate into mood disorders such as depression and anxiety [21, 22].
Although a variety of behavioral therapies that combine diet modifications and physical activity as well as cognitive training have been evaluated for weight loss in this age group, such therapies have proven to be disappointing in providing adequate and sustainable weight loss [6]. In addition, pharmacotherapy has conferred small weight loss benefit that is often unsustainable, with no improvement in comorbidities [23–25]. The side effect profile of some of these weight loss medications has led to their recall [26].
Surgical therapy has consistently been shown to be the most successful therapy for achieving significant weight loss in the obese adult and adolescent populations. In the evaluation of LRYGB versus a behavioral pediatric weight management program, Lawson et al. [27] found a 37 % decrease in BMI of the surgical group compared to a 3 % decrease in BMI of the behavioral therapy group at 1 year. In addition, LRYGB was found to be associated with remission of type II DM while improving cardiovascular risk factors [28].
The treatment of metabolic disease provides another important driving factor for considering bariatric surgery in obese adolescents. All patients who underwent LRYGB in our study experienced remission of their type II DM, which is consistent with results from other studies [28]. Remission of diabetes at an earlier age prevents prolonged exposure to hyperglycemia and the end-organ damages that may result as a consequence. Furthermore, the anatomic and hormonal changes may lower the propensity for developing diabetes in the adult years as well as other obesity-related comorbidities.
Although LAGB is currently not FDA approved for those under the age of 18, its off label use continues to increase exponentially. Between 2005 and 2007, the number of adolescents undergoing LAGB exceeded LRYGB in the state of California [29]. In a preliminary report of their study, Nadler et al. [30] found that LAGB achieved 61 % decrease in the EWL at 2 years in an FAD-approved LAGB for adolescents. Similarly, in a randomized trial, O’Brien et al. [11] showed that LAGB produced more significant weight loss in the adolescent population when compared to lifestyle intervention albeit with a high rate of intervention.
To our knowledge, there have been no trials directly comparing LRYGB to LAGB in the adolescent population. In our study, we found that LRYGB achieves superior EWL in adolescents when compared to LAGB at 24 months follow-up. Furthermore, this effect was observed at all time points studied with the benefit of becoming more significant the further it is from the initial intervention.
One of the limitations of our study is that the follow-up is short term. At 2 year follow-up, only 16 % (5/32) LRYGB and 30 % (7/23) LAGB patients were available for follow-up. Studies in adults have shown that weight gain is more common after this period [31]. A longer follow-up period is necessary to evaluate the sustainability of weight loss into the adult years. Additionally, patients were lost to follow-up in both groups, highlighting the lack of compliance particularly associated with the adolescent population.
In our study, patients who underwent LRYGB were about a year older than those who underwent LAGB. This age difference may reflect a selection bias in which both the younger patients and the surgeon elect LAGB because it is considered less invasive. In addition, performing a LAGB leaves the option of conversion to LRYGB during adulthood.
Although patients in our cohort experienced few complications, studies have shown that patients undergoing LAGB typically require more interventions than LRYGB [11]. However, complications in LRYGB tend to be more severe, ranging from macro and micro nutritional deficiencies, to obstruction, stricture formations, fistula formation, and ulceration. Specifically, adolescents who are still developing may be more acutely affected by the deficiencies of vitamin B12, calcium, and folate [32–34]. Such complications can lead to severe consequences particularly in the adolescent who has to live with altered physiology and anatomy for a much longer period of time.
Bariatric surgery remains the only successful method for significant weight loss in morbidly obese adolescents who have failed to lose weight with lifestyle modifications. In addition, adolescents may see greater benefits than those achieved by adults because of the earlier nature of the intervention. This underscores the need for further establishment of practice guidelines for bariatric surgery in adolescents [35, 36].
Conclusions
LRYGB achieved superior weight loss in adolescents compared to LAGB in a short-term follow-up in our series. Randomized studies with long-term follow-ups will be needed before definitive recommendations can be made on the appropriate operation for this age group. Adolescents should also be counseled on the potential benefits and risks of both these operations before a deciding on an operation for the treatment of morbid obesity.
References
Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303:242–9.
Gupta R, Bhangoo A, Matthews NA, et al. The prevalence of non-alcoholic fatty liver disease and metabolic syndrome in obese children. JPEM. 2011;24:907–11.
Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–8.
Franks PW, Hanson RL, Knowler WC, et al. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–93.
Freedman DS, Mei Z, Srinivasan SR, et al. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. J Pediatr. 2007;150(12–17):e12.
Whitlock EP, O’Connor EA, Williams SB, et al. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125:e396–418.
Trus TL, Pope GD, Finlayson SR. National trends in utilization and outcomes of bariatric surgery. Surg Endosc. 2005;19:616–20.
Tsai WS, Inge TH, Burd RS. Bariatric surgery in adolescents: recent national trends in use and in-hospital outcome. Arch Pediatr Adolesc Med. 2007;161:217–21.
Nguyen NT, Masoomi H, Magno CP, et al. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg. 2011;213:261–6.
Rand CS, Macgregor AM. Adolescents having obesity surgery: a 6-year follow-up. South Med J. 1994;87:1208–13.
O’Brien PE, Sawyer SM, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010;303:519–26.
Nadler EP, Youn HA, Ginsburg HB, et al. Short-term results in 53 US obese pediatric patients treated with laparoscopic adjustable gastric banding. J Pediatr Surg. 2007;42:137–41. discussion 141–132.
Holterman AX, Browne A, Tussing L, et al. A prospective trial for laparoscopic adjustable gastric banding in morbidly obese adolescents: an interim report of weight loss, metabolic and quality of life outcomes. J Pediatr Surg. 2010;45:74–8. discussion 78–79.
Anonymous. NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med. 1991;115(12):956–61
Montero PN, Stefanidis D, Norton HJ, et al. Reported excess weight loss after bariatric surgery could vary significantly depending on calculation method: a plea for standardization. Surg Obes Relat Dis. 2011;7:531–4.
Ogden CL, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–90.
Must A, Jacques PF, Dallal GE, et al. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med. 1992;327:1350–5.
The NS, Suchindran C, North KE, et al. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304:2042–7.
Thompson DR, Obarzanek E, Franko DL, et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2007;150:18–25.
Zeller MH, Modi AC, Noll JG, et al. Psychosocial functioning improves following adolescent bariatric surgery. Obesity. 2009;17:985–90.
Anderson SE, Cohen P, Naumova EN, et al. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007;69:740–7.
Williams J, Wake M, Hesketh K, et al. Health-related quality of life of overweight and obese children. JAMA. 2005;293:70–6.
Chanoine JP, Hampl S, Jensen C, et al. Effect of orlistat on weight and body composition in obese adolescents: a randomized controlled trial. JAMA. 2005;293:2873–83.
Godoy-Matos A, Carraro L, Vieira A, et al. Treatment of obese adolescents with sibutramine: a randomized, double-blind, controlled study. J Clin Endocrinol Metab. 2005;90:1460–5.
Berkowitz RI, Wadden TA, Tershakovec AM, et al. Behavior therapy and sibutramine for the treatment of adolescent obesity: a randomized controlled trial. JAMA. 2003;289:1805–12.
Kang JG, Park CY. Anti-obesity drugs: a review about their effects and safety. Diabetes Metabol J. 2012;36:13–25.
Lawson ML, Kirk S, Mitchell T, et al. One-year outcomes of Roux-en-Y gastric bypass for morbidly obese adolescents: a multicenter study from the Pediatric Bariatric Study Group. J Pediatr Surg. 2006;41:137–43. discussion 137–143.
Inge TH, Miyano G, Bean J, et al. Reversal of type 2 diabetes mellitus and improvements in cardiovascular risk factors after surgical weight loss in adolescents. Pediatrics. 2009;123:214–22.
Jen HC, Rickard DG, Shew SB, et al. Trends and outcomes of adolescent bariatric surgery in California, 2005–2007. Pediatrics. 2010;126:e746–53.
Nadler EP, Youn HA, Ren CJ, et al. An update on 73 US obese pediatric patients treated with laparoscopic adjustable gastric banding: comorbidity resolution and compliance data. J Pediatr Surg. 2008;43:141–6.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28:53–8.
Gong K, Gagner M, Pomp A, et al. Micronutrient deficiencies after laparoscopic gastric bypass: recommendations. Obes Surg. 2008;18:1062–6.
Vargas-Ruiz AG, Hernandez-Rivera G, Herrera MF. Prevalence of iron, folate, and vitamin B12 deficiency anemia after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2008;18:288–93.
Morgan H, Chastanet R, Lucha Jr PA. Internal hernia after laparoscopic gastric bypass surgery: a case report and literature review. Postgrad Med. 2008;120:E01–5.
Apovian CM, Baker C, Ludwig DS, et al. Best practice guidelines in pediatric/adolescent weight loss surgery. Obes Res. 2005;13:274–82.
Pratt JS, Lenders CM, Dionne EA, et al. Best practice updates for pediatric/adolescent weight loss surgery. Obesity. 2009;17:901–10.
Acknowledgments
Authors would like to thank Ms. Dina Corjuc for assisting with data collection and analysis.
Financial Disclosure
Drs Lee, Guend, Park, Levine, Ross, and McGinty have no financial conflict of interest to disclose. Dr Teixeira is a consultant for Covidien and Allergan. No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, D.Y., Guend, H., Park, K. et al. Outcomes of Laparoscopic Roux-en-Y Gastric Bypass Versus Laparoscopic Adjustable Gastric Banding in Adolescents. OBES SURG 22, 1859–1864 (2012). https://doi.org/10.1007/s11695-012-0742-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0742-9