Abstract
Background
Because of the growing interest in surgery to treat morbid obesity, this study examined changes in the utilization and in-hospital outcomes of bariatric surgery in the United States over a 10-year period.
Methods
Data were obtained from the Nationwide Inpatient Sample, the largest all-payer discharge database in the United States. International Classification of Disease (ICD-9) codes were used to identify all bariatric procedures performed for adults from 1990 to 2000. Population-based rates of surgery for each year were calculated by applying sampling weights and U.S. Census data. Secular trends in annual rates of surgery, changes in patient characteristics, and in-hospital mortality and complications were analyzed.
Results
From 1990 to 2000, the national annual rate of bariatric surgery increased nearly six fold, from 2.4 to 14.1 per 100,000 adults (p = 0.001). There has been more than a ninefold increase in the use of gastric bypass procedures (1.4 to 13.1 per 100,000; p < 0.001). This represents an increase from 55% of all bariatric procedures in 1990 to 93% of such procedures in 2000 (p < 0.001). The rates of in-hospital mortality were low (0.4% overall), but increased slightly over time (0.2% in 1990 to 0.5% in 2000; p = 0.009). There is no significant difference in adjusted mortality for the past 8 years, but a slight rise did occur over the full 10-year period. The rates for reoperation (1.3%) and pulmonary emboli (0.3%) remained stable. The rates for respiratory failure associated with bariatric surgery declined from 7.7% in 1990 to 4.5% in 2000 (p < 0.001). Over this time, the mean length of hospital stay declined from 6.0 to 4.1 days (p < 0.001).
Conclusions
The annual rate of bariatric surgery in the United States increased nearly six fold between 1990 and 2000, with_little change in in-hospital morbidity and mortality. This appears to be driven largely by the increasing popularity of gastric bypass procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of obesity in the U.S. population is increasing at an alarming rate [29, 30, 32, 33]. Nearly one-third (30.5%) of the U.S. population is currently considered obese, as defined by the National Institutes of Health (NIH). The prevalence of obesity (body mass index [BMI] = 30) more than doubled, from 13.3% to 30.9% between 1960 and 2000. The main rise in obesity prevalence has occurred in the past 20 years [9]. The prevalence of extreme obesity (BMI = 40) rose from 2.9% to 4.7% from 1988 to 2000. This represents a dramatic rise from 0.8% in 1960 [9, 10]. Recent mortality figures indicate that poor diet and physical inactivity may soon surpass tobacco as the leading cause of death [3]. These trends have increased awareness of the health risks associated with obesity among health care providers, health policymakers, and the general public.
Conventional methods of weight loss such as diet and exercise have been ineffective in achieving sustained weight loss in the morbidly obese population. In fact, the best weight loss programs have been able to maintain a sustained excess body weight loss of only 10% [35, 37, 43, 49]. This small reduction in excess body weight has little if any effect on obesity-related comorbidities in the morbidly obese population.
The only treatment that produces significant, sustained excess body weight loss is bariatric surgery. Several studies of surgical weight loss have demonstrated reductions in obesity-related morbidity, including diabetes, hypertension, obesity hypoventilation, sleep apnea, and gastroesophageal reflux [1, 2, 5-7, 12-16, 18, 24, 39-41, 45, 46, 48]. Public awareness of the benefits of bariatric surgery has been fueled by increased media attention and by the successful treatment of several high-profile celebrities. This interest has been further advanced by the development of laparoscopic approaches to various bariatric procedures.
Secular trends in the use of bariatric surgery in the U.S. have not been examined despite this newfound popularity. High-volume experienced centers have published case series of the relatively low perioperative risks associated with both open and laparoscopic bariatric surgery. A goal of this study was to discern whether similar results are achieved in the broader population.
To determine secular trends, we used administrative data from the Nationwide Inpatient Sample, the largest source of all-payer discharge information in the United States that can be evaluated. Specifically, we sought to determine how much population-based rates of surgery for morbid obesity changed between 1990 and 2000. We also examined trends in patient characteristics and in-hospital outcomes over this period.
Materials and methods
Database
Discharge data from the Nationwide Inpatient Sample (NIS) for the years 1990 to 2000 were obtained from the Healthcare Cost and Utilization Project of the Agency for the-Healthcare Research and Quality. The NIS data consist of all patient-level discharge abstracts from a 20% stratified probability sample of acute care, nonfederal hospitals in the United States (approximately 1,000 hospitals in 2000) [21].
Patient selection
We used International Classification of Diseases (ICD-9) procedure and diagnosis codes to identify all hospitalizations during which a bariatric surgical procedure was performed. Bariatric surgery discharges were identified by the presence of a code for gastric bypass (44.31, 44.39) and/or gastroplasty (44.69) and an accompanying ICD-9 diagnostic code for obesity (278.0, 278.00, 278.01, 278.1, 278.8). For discharges coded for both gastric bypass and gastroplasty (less than a 4% average overlap), gastric bypass was assumed. To increase the homogeneity of the cohort, we excluded all patients with a diagnostic code for an abdominal neoplasm (150.0 through 159.9).
Statistical analysis
We calculated the national population-based rate of bariatric surgery for each year from 1990 to 2000. The annual number of procedures performed in the United States (numerator) was estimated using sampling weights provided with the NIS data. Adult (age, >17 years) population estimates (denominator) were obtained from the U.S. Census.
Demographic characteristics (patient age, gender, and comorbidities) and perioperative outcomes (in-hospital mortality, pulmonary embolus, reoperations, respiratory complications, and median length of stay) were evaluated from the NTS cohort for each year. The Charlson comorbidity index was used to measure severity of illness [8, 42]. This index is a weighted score of patient comorbidity based on ICD-9 diagnostic codes for prior myocardial infarction (412), peripheral vascular disease (440.0 to 443.9), chronic pulmonary disease (415.0, 416.8, 416.9, 491, 491 to 494, 496), dementia (290.0 to 290.9, 331.0, 331.2), diabetes mellitus (250.0 to 250.39), diabetes mellitus with complications (250.4 to 250.99), mild liver disease (571.2, 571.5, 571.6, 571.8, 571.9), severe liver disease (572.2 to 572.4, 456.0 to 456.29), chronic renal failure (585.0 to 586.9, V420, V451, V56.0 to V56.9), various cancers (140.0 to 171.9, 174.0 to 195.9, 200.0 to 208.8, 273.0 to 273.3, V104.6), and metastatic solid tumor (196.0 to 199.9). Complications were identified by the presence of the discharge abstract of specific ICD-9 codes for pulmonary embolus (415.1); reoperation for hemorrhage, anastamotic leak, abscess, or dehiscence (54.11, 54.12, 54.19, 54.61); and respiratory complications including prolonged mechanical ventilation for more than 96 h (96.72), tracheostomy (519.0, 519.00, 519.01, 519.02, 519.09, 31.1, 31.2, 31.21, 31.29, 96.55, 97.23), pneumonia (519.8, 997.3), respiratory failure (518.5, 518.81, 518.82, 518.84), and respiratory arrest (799.1).
Secular trends were tested for statistical significance using logistic regression for dichotomous variables (gender, procedure type, in-hospital mortality, pulmonary embolus, reoperations, and respiratory complications), with year as a continuous independent variable. Nonparametric rank-sum tests were used to test secular trends for continuous dependent variables (patient age, comorbidities, and median length of hospital stay).
Multiple logistic regression was used to calculate adjusted mortality rates for each year [23]. Age and gender were selected as covariates for the final model following stepwise comparison of nested models.
Population sampling weights from NIS were applied to all statistical computations to account for the stratified, clustered survey design. Significance for all tests was set at a p value less than 0.05. All p values are two-tailed. All the analyses were performed using statistical computer software (STATA 7.0, STATA Corporation, College Station, TX, USA).
Results
Patient characteristics
Patient age increased over the study period, and there were significantly more patients with one or more major comorbidites (17.9-27.6%; p < 0.001). No gender trends were observed over the 10-year study period.
Rates of surgery
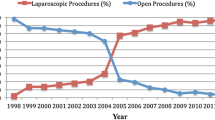
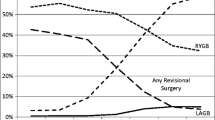
From 1990 to 2000, the national annual rate of bariatric surgery increased almost sixfold, from 2.4 to 14.1 per 100,000 adults (p < 0.001) (Fig. 1). The rate more than doubled in the first 7-year period (2.4 per 100,000 adults in 1990 to 5.9 per 100,000 adults in 1997), then more than doubled again in the final 2 years (5.8 to 14.1 per 100,000 adults in 1998 to 2000; p < 0.001). There was a definite shift toward the use of gastric bypass procedures over this 10-year period. The use of gastric bypass significantly increased from 1.4 to 13.1 per 100,000 adults, whereas gastroplasty utilization declined (Fig. 2). As a proportion of all bariatric procedures, gastric bypass increased from 55% in 1990 to 93% in 2000.
In-hospital outcomes
Unadjusted in-hospital mortality showed a slight upward trend from 0.2% in 1990 to 0.5% in 2000 (p = 0.006). There was no significant difference in adjusted mortality for the final 8 years, but we did find a slight rise over the full 10-year period (p = 0.009).
The rates for reoperation (1.2%) and pulmonary emboli (0.3%) remained stable. The rates for respiratory failure associated with bariatric surgery, which include prolonged ventilation, tracheostomy, pneumonia, respiratory failure, and respiratory arrest, declined from 7.7% in 1990 to 4.5% in 2000 (p < 0.001). Over this time, the mean length of hospital stay declined from 6 to 4.1 days (p < 0.001).
Discussion
The rates for bariatric surgery use in the United States increased more than ninefold between 1990 and 2000, from 2.4 to 14.1 per 100,000 adults. The use of gastric bypass has been the primary driving force in this trend.
We first observed more than a twofold increase in the use of bariatric surgery from 1990 to 1997 [38]. A similar trend over the same period also was reported in a national study from Sweden [26]. The in-hospital mortality rates were similar in both studies. Remarkably, the rate of bariatric surgery use in the United States more than doubled again in the following 3-year period.
There was a decrease in the use of bariatruic surgery from 1994 to 1995 in both the United States and Sweden. This decline correlates with the introduction and popularization of fenfluramine-phentermine (fen-phen). Fenfluramine prescriptions grew from 50,000 per year in 1994 to more than 1 million in 1995 [17]. Fenfluramine was removed from the market in 1997, the same year a sharp rise in bariatric surgery utilization was observed. A second dramatic rise in utilization of bariatric surgery occurred in 1999, which can be attributed to increased media attention to the procedure, largely driven by a laparoscopic approach and celebrity patients.
The in-hospital mortality rate rose slightly over the 10-year period, but this increase was not statistically significant for the final 8 years. We did find a slight in-hospital mortality increase over the full 10-year period. This may reflect the “learning curve” of some surgeons performing bariatric surgery for the first time. The in-hospital outcomes for bariatric surgery were similar to those reported in large published clinical series. The operative mortality rates in large clinical series were 0.24% for vertical banded gastroplasty [28] and 0.4% after both gastric bypass and biliopancreatic diversion [44, 47], with a range from 0% to 2% in published reports [1, 3, 4, 11, 18-20, 22, 24, 25, 27, 34, 36, 41, 48, 50].
The in-hospital complications rates identified from NIS were consistent with published rates for bariatric procedures [1, 4, 19, 22, 25, 27, 39, 41, 47, 50]. Perioperative outcomes such as pulmonary emboli and reoperations remained stable, whereas respiratory complications improved over this time. Pulmonary emboli occurred in approximately 0% to 0.4% of patients, which is similar to the rates of 0% to 0.5% in large published series [1, 22, 39, 41, 50]. Published reoperation rates ranged from 1% to 2.8% whereas we observed rates of 1% to 1.6% [1, 25, 39, 41].
The use of administrative data imposed several limitations. The NIS data capture only in-hospital data, whereas most clinical series capture both in-hospital and out patient outcomes after surgery. Hence, adverse outcomes after discharge were not captured in our study.
Our results most likely underestimate the true number of bariatric procedures performed the over the 10-year study period because of absent ICD-9 codes and the coding practices at various institutions. Many bariatric procedures, particularly laparoscopic procedures, have no designated ICD-9 codes. Nonspecific codes such as “other gastroenterostomy bypass” (44.31) required that the accompanying diagnostic code for obesity be captured for inclusion in this study. These code combinations are highly dependent on the coding practice of the institutions and the number of comorbidity codes that may be preferentially used by some institutions. Also, the number of comorbid conditions experienced by many of these patients may fill the maximum number of diagnostic codes allowed, essentially forcing the elimination of the diagnostic code for obesity.
Finally, information regarding patients’ baseline operative risk difficult to ascertain from administrative data, limiting our ability to adjust for case mix differences.
There appears to be a definite shift to the use of gastric bypass procedures for the treatment of obesity. The ability to perform bariatric surgery laparoscopically has fueled a renewed interest in obesity surgery among surgeons and the public. Gastric banding, approved by the Food and Drug Administration, may shift interest back to restrictive procedures if efficacious. The development of innovative endoscopic bariatric procedures or promising weight loss drugs could dramatically alter these trends.
Conclusions
Utilization of bariatric surgery in the United States increased nearly sixfold from 1990 to 2000. This trend appears to be linked to an increase in the use of gastric bypass. The development of minimally invasive bariatric procedures along with increased public awareness and a growing prevalence of obesity may continue to increase bariatric surgery utilization further.
References
BM Balsiger FP Kennedy HS Abu-Lebdeh M Collazo-Clavell MD Jensen T O’Brien DD Hensrud SF Dinneen GB Thompson FG Que DE Williams MM Clark JE Grant MS Frick RA Mueller JL Mai MG Sarr (2000) ArticleTitleProspective evaluation of Roux-en-Y gastric bypass as primary operation for medically complicated obesity Mayo Clin Proc 75 673–680 Occurrence Handle1:STN:280:DC%2BD3czovVagsQ%3D%3D Occurrence Handle10907381
PN Benotti B Bistrain JR Benotti G Blackburn RA Forse (1992) ArticleTitleHeart disease and hypertension in severe obesity: the benefits of weight reduction Am J Clin Nutr 55 586S–590S Occurrence Handle1:STN:280:By2C38rislY%3D Occurrence Handle1733133
PN Benotti J Hollingshead EA Mascioli A Bothe SuffixJr BR Bistrian GL Blackburn (1989) ArticleTitleGastric restrictive operations for morbid obesity Am J Surg 157 150–155 Occurrence Handle1:STN:280:BiaD1cnmtFA%3D Occurrence Handle2910120
GA Bray (1985) ArticleTitleComplications of obesity Ann Intern Med 103 1052–1062 Occurrence Handle1:STN:280:BimD2cbgtVM%3D Occurrence Handle4062125
RE Brolin HA Kenler JH Gorman RP Cody (1992) ArticleTitleLong-limb gastric bypass in the super obese: a prospective randomized study Ann Surg 215 387–395 Occurrence Handle1:STN:280:By2B3MvpvFA%3D Occurrence Handle1558421
I Charuzi P Lavie J Peiser R Peled (1992) ArticleTitleBariatric surgery in morbidly obese sleep apnea patients: short- and long-term follow-up Am J Clin Nutr 55 594S–596S Occurrence Handle1:STN:280:By2C38rislA%3D Occurrence Handle1733135
I Charuzi A Ovnat J Peiser H Saltz S Weitzman P Lavie (1985) ArticleTitleThe effect of surgical weight reduction on sleep quality in obesity-related sleep apnea syndrome Surgery 97 535–538 Occurrence Handle1:STN:280:BiqC1MzgtlE%3D Occurrence Handle3992478
LM Ellison JA Heaney JD Birkmeyer (2000) ArticleTitleThe effect of hospital volume on mortality and resource use after radical prostatectomy J Urol 163 867–869 Occurrence Handle1:STN:280:DC%2BD3c7ltVOjsA%3D%3D Occurrence Handle10687994
KM Flegal MD Carroll RJ Kuczmarski CL Johnson (1998) ArticleTitleOverweight and obesity in the United States: prevalence and trends, 1960-1994 Int J Obes 22 39–47 Occurrence Handle1:STN:280:DyaK1c7kt1GqtQ%3D%3D
KM Flegal MD Carroll CL Ogden CL Johnson (2002) ArticleTitlePrevalence and trends in obesity among U.S. adults, 1999-2000 J Am Med Assoc 288 1723–1727
MA Fobi H Lee R Holness D Cabinda (1998) ArticleTitleGastric bypass operation for obesity World J Surg 22 925–935 Occurrence Handle10.1007/s002689900496 Occurrence Handle1:STN:280:DyaK1czotlWntA%3D%3D Occurrence Handle9717418
EF Foley PN Benotti BC Borlase J Hollingshead GL Blackburn (1992) ArticleTitleImpact of gastric restrictive surgery on hypertension in the morbidly obese Am J Surg 163 294–297 Occurrence Handle1:STN:280:By2C2s7gs1Y%3D Occurrence Handle1539761
Gastrointestinal Surgery for Severe Obesity. NIH Consensus Statement 1991, Mar 25–27; 9: 1-20
JJ Gleysteen (1992) ArticleTitleResults of surgery: long-term effects on hyperlipidemia Am J Clin Nutr 55 591S–593S Occurrence Handle1:STN:280:By2C38rislc%3D Occurrence Handle1733134
JJ Gleysteen JJ Barboriak (1983) ArticleTitleImprovement in heart disease risk factors after gastric bypass Arch Surg 118 681–684 Occurrence Handle1:STN:280:BiyB3czjvVM%3D Occurrence Handle6847361
JJ Gleysteen JJ Barboriak EA Sasse (1990) ArticleTitleSustained coronary risk factor reduction after gastric bypass for morbid obesity Am J Clin Nutr 51 774–778 Occurrence Handle1:STN:280:By%2BB2c%2FhslU%3D Occurrence Handle2333834
Goldstein, N (1998) Prescribing drugs as a learned intermediary, Physician’s News Digest, Philadelphia, Vol 11, p 7
WO Griffen BA Bivins RM Bell KA Jackson (1981) ArticleTitleGastric bypass for morbid obesity World J Surg 5 817–822 Occurrence Handle7342476
WO Griffen VL Young CC Stevenson (1977) ArticleTitleA prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity Ann Surg 186 500–509 Occurrence Handle907395
JC Hall JM Watts PE O’Brien RE Dunstan JF Walsh AH Slavotinek RG Elmslie (1990) ArticleTitleGastric surgery for morbid obesity. The Adelaide Study Ann Surg 211 419–427 Occurrence Handle1:STN:280:By%2BB3M%2FntlA%3D Occurrence Handle2181950
(HCUP) HCaUiP (2002) Nationwide Inpatient Sample (NIS): Agency for Healthcare Research and Quality, Rockville, MD
L Howard M Malone A Michalek J Carter S Alger J Woert ParticleVan (1995) ArticleTitleGastric bypass and vertical banded gastroplasty: a prospective randomized comparison and 5-year follow-up Obes Surg 5 55–60 Occurrence Handle10.1381/096089295765558169 Occurrence Handle10733794
DW Hosmer S Lemeshow (1989) Applied logistic regression John Wiley New York
KB Jones ParticleJr (2000) ArticleTitleExperience with the Roux-en-Y gastric bypass, and commentary on current trends Obes Surg 10 183–185 Occurrence Handle10.1381/096089200321668659 Occurrence Handle10782184
JM Kellum EJ DeMaria HJ Sugerman (1998) ArticleTitleThe surgical treatment of morbid obesity Curr Probl Surg 35 791–858 Occurrence Handle1:STN:280:DyaK1cvhvVWnsw%3D%3D Occurrence Handle9745619
E Leffler S Gustavsson BM Karlson (2000) ArticleTitleTime trends in obesity surgery 1987 through 1996 in Sweden: a population-based study Obes Surg 10 543–548 Occurrence Handle1:STN:280:DC%2BD3M7ks1WisA%3D%3D Occurrence Handle11175963
KG MacDonald WJ Pories (1992) ArticleTitleRoux gastric bypass or vertical banded gastroplasty Prob Gen Surg 9 321–331
EE Mason JW Maheer DH Scott EM Rodriguez C Doherty (1992) ArticleTitleTen years of vertical banded gastroplasty for severe obesity Probl Gene Surg 9 280–289
AH Mokdad BA Bowman ES Ford et al. (2003) ArticleTitlePrevalence of obesity, diabetes, and obesity-related health risk factors, 2001 JAMA 289 76–79 Occurrence Handle10.1001/jama.289.1.76 Occurrence Handle12503980
AH Mokdad BA Bowman ES Ford F Vinicor JS Marks JP Koplan (2001) ArticleTitleThe continuing epidemics of obesity and diabetes in the United States JAMA 286 1195–1200 Occurrence Handle10.1001/jama.286.10.1195 Occurrence Handle1:STN:280:DC%2BD3MrhvVegsw%3D%3D Occurrence Handle11559264
AH Mokdad JS Marks DF Stroup JL Gerberding (2004) ArticleTitleActual causes of death in the United States, 2000 JAMA 291 1238–1245 Occurrence Handle10.1001/jama.291.10.1238 Occurrence Handle15010446
AH Mokdad MK Serdula WH Dietz BA Bowman JS Marks JP Koplan (1999) ArticleTitleThe spread of the obesity epidemic in the United States, 1991-1998 JAMA 282 1519–1522 Occurrence Handle10.1001/jama.282.16.1519 Occurrence Handle1:STN:280:DC%2BD3c%2Fht1Wrsw%3D%3D Occurrence Handle10546690
AH Mokdad MK Serdula WH Dietz BA Bowman JS Marks JP Koplan (2000) ArticleTitleThe continuing epidemic of obesity in the United States JAMA 284 1650–1652 Occurrence Handle1:STN:280:DC%2BD3cvmsFyqsw%3D%3D Occurrence Handle11015792
I Naslund (1987) ArticleTitleGastric bypass versus gastroplasty: a prospective study of differences in two surgical procedures for morbid obesity Acta Chirurg Scand Suppl 536 1–60 Occurrence Handle1:STN:280:BiiB1MvosFI%3D
InstitutionalAuthorNameNational Task Force on the Prevention and Treatment of Obesity (1993) ArticleTitleVery low calorie diets JAMA 270 967–974
NT Nguyen C Goldman CJ Rosenquist A Arango CJ Cole SJ Lee BM Wolfe (2001) ArticleTitleLaparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs Ann Surg 234 279–289 Occurrence Handle10.1097/00000658-200109000-00002 Occurrence Handle1:STN:280:DC%2BD3MvotVymtA%3D%3D Occurrence Handle11524581
MG Perri PR Fuller (1995) ArticleTitleSuccess and failure in the treatment of obesity: where do we go from here? Med Exerc Nutr Health 4 255–272
GD Pope JD Birkmeyer SRG Finlayson (2002) ArticleTitleNational trends in utilization and in-hospital outcomes of bariatric surgery J Gastrointest Surg 6 855–860 Occurrence Handle12504224
WJ Pories (1991) The surgical approach to morbid obesity DC Sabiston (Eds) Textbook of surgery: the biologic basis of modern surgical practice WB Saunders Philadelphia, PA 851–866
WJ Pories KG MacDonald SuffixJr EJ Morgan MK Sinha GL Dohm MS Swanson HA Barakat PG Khazanie N Leggett-Frazier SD Long (1992) ArticleTitleSurgical treatment of obesity and its effect on diabetes: 10-year follow-up Am J Clin Nutr 55 582S–585S Occurrence Handle1:STN:280:By2C38rislU%3D Occurrence Handle1733132
WJ Pories MS Swanson KG MacDonald SB Long PG Morris BM Brown HA Barakat RA deRamon G Israel JM Dolezal (1995) ArticleTitleWho would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus Ann Surg 222 339–350 Occurrence Handle1:STN:280:ByqH3cjps1I%3D Occurrence Handle7677463
PS Romano LL Roos JG Jollis (1993) ArticleTitleAdapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives J Clin Epidemiol 46 1075–1079 Occurrence Handle1:STN:280:ByuD3MrhvVU%3D Occurrence Handle8410092
DJ Safer (1991) ArticleTitleDiet, behavior modification, and exercise: a review of obesity treatments from a long-term perspective South Med J 84 1470–1474 Occurrence Handle1:STN:280:By2D1cnptFU%3D Occurrence Handle1749981
N Scopinaro E Gianetta GF Adami D Friedman E Traverse GM Marinari S Cuneo B Vitale F Ballari M Colombini G Baschieri V Bachi (1996) ArticleTitleBiliopancreatic diversion for obesity at eighteen years Surgery 119 261–268 Occurrence Handle1:STN:280:BymB3c3lsVE%3D Occurrence Handle8619180
HJ Sugerman RP Fairman PL Baron JA Kwentus (1986) ArticleTitleGastric surgery for respiratory insufficiency of obesity Chest 90 81–86 Occurrence Handle1:STN:280:BimB2cnlvVc%3D Occurrence Handle3720390
HJ Sugerman RP Fairman RK Sood K Engle L Wolfe JM Kellum (1992) ArticleTitleLong-term effects of gastric surgery for treating respiratory insufficiency of obesity Am J Clin Nutr 55 597S–601S Occurrence Handle1:STN:280:By2C38rislE%3D Occurrence Handle1733136
HJ Sugerman JM Kellum KM Engle L Wolfe JV Starkey R Birkenhauer P Fletcher MJ Sawyer (1992) ArticleTitleGastric bypass for treating severe obesity Am J Clin Nutr 55 560S–566S Occurrence Handle1:STN:280:By2C38ris1I%3D Occurrence Handle1733127
HJ Sugerman GL Londrey JM Kellum L Wolf T Liszka KM Engle R Birkenhauer JV Starkey (1989) ArticleTitleWeight loss with vertical banded gastroplasty and Roux-Y gastric bypass for morbid obesity with selective versus random assignment Am J Surg 157 93–102 Occurrence Handle1:STN:280:BiaD1cnmtlc%3D Occurrence Handle2910132
M Weintraub et al. (1992) ArticleTitleLong-term weight control study IV (weeks 156-190): the second double-blind phase Clin Pharmacol Ther 51 608–614 Occurrence Handle1:STN:280:By2B28nms10%3D Occurrence Handle1587075
CE Yale (1989) ArticleTitleGastric surgery for morbid obesity: complications and long-term weight control Arch Surg 124 941–946 Occurrence Handle1:STN:280:BiaA3svmtVE%3D Occurrence Handle2757508
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trus, T.L., Pope, G.D. & Finlayson, S.R.G. National trends in utilization and outcomes of bariatric surgery. Surg Endosc 19, 616–620 (2005). https://doi.org/10.1007/s00464-004-8827-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-004-8827-8