Abstract
Background
Sleeve gastrectomy (SG) has been used as a multipurpose surgical procedure for the treatment of morbid obesity. The aim of the study was to analyze gastric morphology and histology at two different time points after SG in rats.
Methods
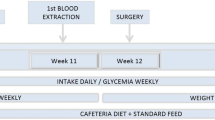
Thirty-five male Wistar rats were fed ad libitum during 3 months on a high-fat diet to induce obesity. Subsequently, 25 diet-induced obese rats underwent either SG (n = 12) or a sham operation (n = 13). The remaining ten obese animals encompassed the nonoperated control group (Co). Four weeks postoperatively, 15 rats (n = 5 rats/experimental group) were sacrificed, while the remaining 20 rats were sacrificed after 16 weeks (animals/group; Co = 5, sham = 8, SG = 7) to compare the gastric morphological and histopathological changes over time. Body weight and food intake were regularly recorded.
Results
For both time periods, the Co groups exhibited the highest body weight, while the rats undergoing the SG showed the lowest weight gain (P < 0.05). Initially, significant differences (P < 0.005) in food intake relative to body weight were observed between the Co rats and animals undergoing surgery, which disappeared thereafter. The actual total stomach size after both experimental periods in the SG group was similar to that of non- and sham-operated rats mainly due to a forestomach enlargement, which was more pronounced after 16 weeks. Traits of gastritis cystica profunda characterized by gastric foveolae elongation with hyperplasia and cystic dilatation of the glands were observed in the residual stomachs of the sleeve-gastrectomized rats. These findings were mostly observed after 16 weeks of performing the SG, although they were also detected occasionally following 4 weeks postoperatively. No intestinal metaplasia was observed.
Conclusion
After SG gastric macro- and microscopic changes with functional implications in both the short and long term take place.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the current scenario of a worldwide epidemic of obesity, in which the full range of potential underlying causes is still being elucidated [1], bariatric surgery provides a safe and effective treatment in carefully selected morbidly obese patients. Laparoscopic sleeve gastrectomy (SG), in particular, has emerged in the last years as a relatively easy to perform surgical technique with reduced risk weight loss for these patients [2–4] in its different forms of application either as a primary, staged, or revisional operation due to its proven simplicity, safety, as well as short- and midterm efficacy [5–11]. Nonetheless, SG also has a number of disadvantages and associated risks derived from the direct intervention on the stomach. Thus, two major perioperative complications are staple line leak and hemorrhage, whereas postoperative upper gastrointestinal alterations may include gastritis and dysplasia [12, 13]. For this reason, it is important to gain further insight into the potential impact of this restrictive intervention on the stomach. Therefore, the aim of the present study in rats was to examine the morphological and histopathological changes taking place after SG in the intervened stomach over time.
Materials and Methods
Animals
In order to induce obesity, in a first experimental phase, thirty-five 8–10-week-old male Wistar rats with a mean body weight of 220 ± 15 g (obtained from the University of Navarra breeding house) were used. Housing characteristics included an ambient temperature of 22 ± 2°C, a 12:12-h light–dark cycle (lights on at 0800 hours), pathogen-free conditions, individual caging, and ad libitum feeding during 3 months on a high-fat diet (HFD), which provided 59% of total calories as fat, 27% as carbohydrate, and 14% as protein (diet F3282; Bio-Serv, Frenchtown, NJ, USA). Daily records of body weight and food intake were carried out during the 12 weeks on the HFD to check progression of the diet-induced obesity (DIO) model.
Surgical Procedures
The effect of SG on the stomach was analyzed in a second experimental phase in which surgical interventions were performed on the diet-induced obese rats under general inhalatory anesthesia using isoflurane in spontaneously breathing animals as previously described [14]. In brief, preoperative fasting of solid food took place for at least 14 h, while access to water was allowed. Anesthesia induction was achieved with 4% vaporized isoflurane (Laboratorios Esteve S.A., Barcelona, Spain) administered in an oxygen mixture at a constant flow of approximately 0.6 l/min. The anesthetized animal was then placed in a supine position on the operating table adjusting a nosecone around the head. Anesthesia maintenance was provided by 2% isoflurane vaporization administered via the nosecone. Sterile surgical materials were used, accompanied by antibiotic prophylaxis with intramuscular administration of 25 mg of enrofloxacin per kg body weight (Laboratorios Esteve S.A., Barcelona, Spain). Twenty-five diet-induced obese rats underwent the surgical protocols consisting in either SG (n = 12) or a sham operation (n = 13) as described previously by our group [14]. Briefly, loose splenic and hepatic connections of the stomach were released along the greater curvature. In order to isolate the stomach, the great omentun was ligated and divided down to the level of the pylorus. The manipulated stomach was subsequently rested on a saline-moistened gauze pad outside the abdominal cavity. A TA30V3L load encompassed by three rows of staples of 2.5 mm was placed with the AutoSuture TA automatic stapler (DST seriesTyco Healthcare Group LP, Norwalk, Connecticut, USA) 3–5 mm from the pylorus to warrant free passage of food to the duodenum, thereby leaving a smaller gastric pouch (stomach volume reduction of approximately 60–80%), with a tubular shape that included most of the forestomach and glandular stomach. Subsequently, a continuous polypropylene 6/0 hand-sewn suture was performed to reinforce the automatically placed staple line in order to warrant long-term integrity. As described previously by our group [14], the same laparotomy incision together with the placement of the stomach out of the abdominal cavity was carried out in the sham surgery, thereby resembling the manipulations of the SG.
Postsurgical Manipulations
All animals were administered subcutaneously 0.03 mg/kg buprenorphine (Schering-Plough S.A., Madrid, Spain) as analgesic measure as well as 5 ml saline to avoid dehydration. During the first 48 h after surgery, rats received a liquid diet with 5% glucose and 0.9% saline solution, having ad libitum access to solid food thereafter, consisting of the same HFD that animals had been eating prior to surgery. For comparative purposes and as an additional control group (Co), the ten rats not undergoing surgery also continued with free access to the HFD. Once 4 weeks of the surgery had elapsed, 15 rats (n = 5 rats per experimental group) were sacrificed, while the remaining 20 rats were followed for a longer period of time and sacrificed after 16 weeks to compare the gastric histopathological changes on two different time points. The sham- and SG-operated groups were composed by eight and seven rats, respectively, while the Co group encompassed five animals. All rats were pathogen free with no bacterial infection of the stomach, including Helicobacter pylori.
The rats were kept in individual cages throughout the experimental period. Body weight and food intake were recorded daily for 4 weeks in all animals, and twice weekly, thereafter, until 16 weeks postoperatively. The rats were sacrificed by decapitation [15], the gastrointestinal system was carefully dissected out as previously described [16], and the entire stomach was fixed for 24 h in Bouin’s solution. After fixation, the stomach was cut longitudinally along the greater curvature, cleaned up its content, dehydrated in ethanol, and embedded in paraffin. Five-micrometer sections were stained with hematoxylin–eosin and periodic acid Schiff (PAS) for histological analysis.
The European Guidelines for the Care and Use of Laboratory Animals was strictly followed with all experimental procedures being approved by the Ethical Committee for Animal Experimentation of the University of Navarra (050/09).
Statistical Analysis
The obtained results are shown as mean ± standard error of the mean. Given the small number of animals in each experimental group, nonparametric tests were applied. The Kruskal–Wallis test was applied to analyze differences between all experimental groups, which was followed by the pairwise comparison of the diverse surgical and dietary groups by means of U Mann–Whitney tests. The SPSS/Windows version 15.0 statistical package (SPSS Inc., Chicago, IL, USA) was used to carry out the analyses setting the statistical significance level at P < 0.05.
Results
During the 12 weeks of DIO, the rats doubled their body weight. After the surgical interventions, as expected, the Co groups exhibited the highest body weight, while the rats undergoing the SG showed the lowest weight gain (P < 0.05) for both time periods. During the first 4 weeks postsurgery, the SG group experimented only a 38.3% weight gain as opposed to the 51.2% of the Co animals with the sham-operated rats running in between them. These differences were maintained following 16 weeks of the surgical interventions, with rats undergoing the SG showing a 148 ± 16-g weight gain, whereas the increment in the sham-operated and Co rats was 166 ± 32 and 198 ± 19 g, respectively. Initially, statistically significant differences (P < 0.005) in food intake relative to body weight were observed between the Co rats and the animals undergoing surgery. In fact, during the first and second postoperative weeks, the sleeve-gastrectomized rats exhibited a statistically significant (P < 0.001) reduction in food intake of the HFD as compared to the sham-operated animals. Thereafter, the rats in the SG groups also started to experience a progressive increase in calorie consumption. The initial decreased food intake observed in the SG groups compared to the non- and sham-operated groups vanished and did not reach statistical significance. This normalization in the amount of food consumed by the sleeve-gastrectomized rats was paralleled by a weight-stable period during the third week, with the further food intake elevation leading to a weight regain phase during the fourth week. In the long term, the lack of differences in food intake between the three experimental groups was maintained.
Figure 1 depicts the macroscopic changes in the gastric morphology observed after 4 and 16 weeks of the SG. Noteworthy, in spite of the partial gastrectomy undergone by the SG group, the actual total size of the stomach after both experimental periods was pretty similar to that of nonoperated rats mainly due to the enlargement of the forestomach (Fig. 1e, f), the nonglandular gastric portion. Moreover, the important dilatation of the nonglandular portion of the stomach following the gastric restrictive procedure was accompanied by a thickness reduction of the stratified squamous epithelium (Fig. 2). This dilatation was not observed in the sham-operated and control groups, whereas it was even more pronounced in the stomachs studied 16 weeks after the SG.
Representative macroscopic view of the stomachs obtained from a control rat (a, d) in comparison to those of sleeve-gastrectomized animals following 4 (b, e) and 16 (c, f) weeks after the intervention. The upper panel shows the stomachs fixed with Bouin (a–c), while the lower panel depicts their resultant histological sections stained with hematoxylin–eosin (d–f); ng nonglandular stomach, g glandular stomach
Comparison of the histological sections of the forestomach of a control animal (a) and a sleeve-gastrectomized rat 16 weeks after the surgery (b) showing the decrease in the thickness of the epithelium caused by the important dilatation of the nonglandular portion of the stomach following the gastric restrictive procedure. Hematoxylin–eosin staining
At low magnification the glandular region did not show relevant modifications. The gastric mucosa exhibited a normal appearance, except in the sutured area (Fig. 3). This region was characterized by gastric foveolae elongation together with hyperplasia and cystic dilatation of the gastric glands (Fig. 3a–c). No intestinal metaplasia was observed, while foci of inflammation (lymphocytes, plasma cells, and neutrophils) in the submucosa were detected (Fig. 3d). Some cysts showed stratifications of proliferative epithelial cells. In other cases, cysts were lined by flattened epithelium and contained abundant mucin content (Figs. 4 and 5). In the present study, after 16 weeks of undergoing the SG, all rats exhibited these anatomopathological traits; these features were also observed in the residual stomachs of at least half of the animals analyzed after 4 weeks of performing the SG, though the histopathological characteristics were much less pronounced. A loss of specialized cells, particularly, of parietal cells was also evident.
Pairs of histological sections of the gastric mucosa obtained from two rats after 4 weeks of undergoing a sleeve gastrectomy. Note the tortuous aspect of the foveolae (a, c) and the cystically dilated glands lined by mucin containing epithelial cells (b, d). Hematoxylin–eosin (a, c) and PAS (b, d) stains
Discussion
In the last years, laparoscopic SG has been introduced as a multipurpose, effective, and safe restrictive procedure for the treatment of obese patients [5–12]. Undoubtedly, SG is considered a treatment of choice for producing a good degree of weight loss in carefully selected morbid obese patients based on its already well-known as well as proven safety and effectiveness. The present study focused on the short- and long-term effects following SG on the residual stomach, in addition to analyzing the impact of the procedure on body weight and food intake. After both 4 and 16 weeks of performing the SG, the actual total size of the operated stomachs did not differ to that of sham- or nonoperated rats, which is in agreement with previous observations [17]. Our study revealed that the effect on the gastric morphology and size was mainly due to the marked enlargement of the forestomach, the nonglandular gastric portion. This finding underlies the lack of differences in food intake at the end of both study periods between the sleeve-gastrectomized rats and both the Co and sham-operated animals, while SG being a restrictive procedure. Noteworthy, the forestomach dilatation was more pronounced in the long term and was accompanied by a reduction in the thickness of the stratified squamous epithelium. It has to be clearly stated that the gastric anatomical and functional differences between humans and rats do not allow direct extrapolation of results. Although the capacity of the stomach can also reportedly increase in humans late after SG even after performing a narrow gastric tubulization [18], it is necessary to underline that the postoperative dilatation of the residual stomach in the rat model is not fully comparable with the clinical situation given the species-specific gastric anatomical differences. The rat has a forestomach, a nonsecretory region with a keratinized epithelium with the ability to greatly dilate [19]. Noteworthy, in spite of an impeccably performed SG from a technical and surgical point of view, it is also true that residual gastric volume can increase over time in patients, especially so in those that do not strictly follow the dietary recommendations. Assuming and acknowledging the human versus rat peculiarities, it is also important to measure objectively residual gastric volume in humans after SG and its eventual increase in patients experimenting an inadequate weight loss in order to consider a potential retreatment strategy.
From a histopathological point of view, no relevant alterations of the glandular region of the stomach of sleeve-gastrectomized rats were evident at low magnification. In general, the gastric mucosa exhibited a normal appearance, except in the sutured area, which was characterized by gastric foveolae elongation together with hyperplasia and cystic dilatation of the gastric glands. The presence of the gastric changes only in the proximity of the suture line points to a suture-induced and dilation-independent phenomenon. In this respect, the next aspects to be addressed pertain to the causal relation to the specific material used and to the potential dependence on the type of bariatric surgery performed. To our knowledge, no evidence on this topic in experimental models has been published so far, given that most studies carried out in animals do primarily address the weight, metabolic, and hormonal differences between the diverse bariatric surgery techniques [20–22]. In the present study, staples reinforced with hand-sewn sutures were applied for the SG. Although this topic was not the primary focus of a previous study, our group has also observed similar gastric histopathological changes using only automatic stapling for the partial gastrectomy in a different bariatric procedure like the biliopancreatic diversion [23]. The foveola-opening phenomenon, which is a convincing sign of mucus production, has been shown to correlate with a cytoprotective, antiulcerogenic effect [24], and can be thus viewed as a defense mechanism against the trauma imposed by gastric suturing due to the partial gastrectomy. This is in line with the foci of chronic inflammation observed in the submucosa containing lymphocytes, plasma cells, and neutrophils. Noteworthy, no intestinal metaplasia was observed.
The present study identified in the residual stomachs of the sleeve-gastrectomized rats after 16 weeks of the intervention traits of gastritis cystica profunda (GCP), a relatively rare disorder in humans that was first described by Littler and Gleibermann [25]. GCP is characterized by polypoid hyperplasia of the gastric mucosa that develops in patients who have undergone gastroenterostomy with or without gastric resection [26]. Histopathologically GCP characteristically exhibits elongation of the gastric foveolae with hyperplasia and cystic dilatation of the gastric glands, extending into the submucosal layer [27]. Given that GCP is rarely found in the unoperated stomach, mucosal prolapse and reflux of intestinal contents have been put forward as potential causes of its appearance [25, 27, 28]. Abdominal pain, bloating, bleeding, and ulceration are among the clinical manifestations of GCP [29]. Moreover, GCP has been associated with carcinoma development [30].
In summary, the macro- and microscopic changes observed at two different postoperative time periods after SG performed in rats highlight the presence of morphologic and histopathological changes in both the short and long term. The present study does not question at all the long-term safety of the SG procedure in humans given the anatomophysiological differences between rats and humans, which do not allow direct extrapolation of results. In this line, postoperative endoscopic screening in humans that have undergone an SG procedure may be low yield, though useful in both guiding clinical decision making and in identifying potential dangerous tissue transformation.
Abbreviations
- SG:
-
Sleeve gastrectomy
- HFD:
-
High-fat diet
- GCP:
-
Gastritis cystica profunda
References
Frühbeck G, Gómez-Ambrosi J. Rationale for the existence of additional adipostatic hormones. FASEB J. 2001;15:1996–2006.
Gumbs AA, Gagner M, Dakin G, et al. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17:962–9.
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for Sleeve Gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–96.
Gagner M, Deitel M, Kalberer TL, et al. The Second International Consensus Summit for Sleeve Gastrectomy, March 19–21, 2009. Surg Obes Relat Dis. 2009;5:476–85.
Gumbs AA, Pomp A, Gagner M. Revisional bariatric surgery for inadequate weight loss. Obes Surg. 2007;17:1137–45.
Braghetto I, Korn O, Valladares H, et al. Laparoscopic sleeve gastrectomy: surgical technique, indications and clinical results. Obes Surg. 2007;17:1442–50.
Parikh M, Gagner M. Laparoscopic hiatal hernia repair and repeat sleeve gastrectomy for gastroesophageal reflux disease after duodenal switch. Surg Obes Relat Dis. 2008;4:73–5.
Gagner M, Gumbs AA, Milone L, et al. Laparoscopic sleeve gastrectomy for the super-super-obese (body mass index >60 kg/m2). Surg Today. 2008;38:399–403.
Rubin M, Yehoshua RT, Stein M, et al. Laparoscopic sleeve gastrectomy with minimal morbidity. Early results in 120 morbidly obese patients. Obes Surg. 2008;18:1567–70.
Shi X, Karmali S, Sharma AM, et al. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20:1171–7.
Gagner M. Laparoscopic sleeve gastrectomy with duodenojejunal bypass for severe obesity and/or type 2 diabetes may not require duodenojejunal bypass initially. Obes Surg. 2010;20:1323–4.
Abu-Jaish W, Rosenthal RJ. Sleeve gastrectomy: a new surgical approach for morbid obesity. Expet Rev Gastroenterol Hepatol. 2010;4:101–19.
Behrens C, Tang BQ, Amson BJ. Early results of a Canadian laparoscopic sleeve gastrectomy experience. Can J Surg. 2011;54:138–43.
Valentí V, Martín M, Ramírez B, et al. Sleeve gastrectomy induces weight loss in diet-induced obese rats even if high-fat feeding is continued. Obes Surg. 2011;21:1438–43.
Gómez-Ambrosi J, Frühbeck G, Martínez JA. Leptin, but not a beta 3-adrenergic agonist, upregulates muscle uncoupling protein-3 messenger RNA expression: short-term thermogenic interactions. Cell Mol Life Sci. 1999;55:992–7.
Muruzábal FJ, Frühbeck G, Gómez-Ambrosi J, et al. Immunocytochemical detection of leptin in non-mammalian vertebrate stomach. Gen Comp Endocrinol. 2002;128:149–52.
Cai J, Zheng C, Xu L, et al. Therapeutic effects of sleeve gastrectomy plus gastric remnant banding on weight reduction and gastric dilatation: an animal study. Obes Surg. 2008;18:1411–7.
Braghetto I, Cortes C, Herquiñigo D, et al. Evaluation of the radiological gastric capacity and evolution of the BMI 2–3 years after sleeve gastrectomy. Obes Surg. 2009;19:1262–9.
DeSesso JM, Jacobson CF. Anatomical and physiological parameters affecting gastrointestinal absorption in humans and rats. Food Chem Toxicol. 2001;39:209–28.
Pereferrer FS, Gonzàlez MH, Rovira AF, et al. Influence of sleeve gastrectomy on several experimental models of obesity: metabolic and hormonal implications. Obes Surg. 2008;18:97–108.
Cunha Medeiros A, Meneses Rego A, Medeiros Azevedo I, et al. Metabolism and gastric remnant changes after Roux-en-Y gastric bypass in rats. J Investig Surg. 2011;24:109–14.
Masuda T, Ohta M, Hirashita T, et al. A comparative study of gastric banding and sleeve gastrectomy in an obese diabetic rat model. Obes Surg. 2011;21:1774–80.
Mendieta-Zerón H, Larrad-Jiménez A, Frühbeck G, et al. Larrad biliopancreatic diversion in Sprague–Dawley rats. Analysis of weight loss related to food intake. Obes Surg. 2009;19:484–9.
Balint GA, Hulesch H. The effect of different prostaglandins on rat gastric mucosa. Scanning electron microscopic investigations. Exp Toxicol Pathol. 1995;47:71–4.
Littler E, Gleibermann E. Gastritis cystica polyposa (gastric mucosal prolapse at gastrectomy site, with cystic and infiltrative epitherial hyperplasia). Cancer. 1972;29:205–9.
Tomizuka T, Mazaki T. A case of gastritis cystica profunda. Surgery. 2008;143:449–50.
Hirasaki S, Tanimizu S, Tsubouchi E, et al. Gastritis cystica polyposa concomitant with gastric inflammatory fibroid polyp occurring in an unoperated stomach. Int Med. 2005;44:46–9.
Park JS, Myung SJ, Jung HY, et al. Endoscopic treatment of gastritis cystica polyposa found in an unoperated stomach. Gastrointest Endosc. 2001;54:101–3.
Kurland J, DuBois S, Behling C, et al. Severe upper-GI bleed caused by gastritis cystica profunda. Gastrointest Endosc. 2006;63:716–7.
Mitomi H, Iwabuchi K, Amemiya A, et al. Immunohistochemical analysis of a case of gastritis cystica profunda associated with carcinoma development. Scand J Gastroenterol. 1998;33:1226–9.
Acknowledgments
This work was supported by Fondo de Investigaciones Sanitarias (FIS PS0902330) from the Spanish Instituto de Salud Carlos III, Ministerio de Sanidad y Consumo. The authors gratefully acknowledge the valuable collaboration of all the staff of the breeding house of the University of Navarra, in particular Elena Ciordia and Juan Percaz as well as the advice of Javier Guillén.
Disclosure statement
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Additional information
Marina Martín and María A. Burrell worked equally.
Rights and permissions
About this article
Cite this article
Martín, M., Burrell, M.A., Gómez-Ambrosi, J. et al. Short- and Long-Term Changes in Gastric Morphology and Histopathology Following Sleeve Gastrectomy in Diet-Induced Obese Rats. OBES SURG 22, 634–640 (2012). https://doi.org/10.1007/s11695-012-0606-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-012-0606-3