Abstract
Background
Roux-en-Y gastric bypass surgery (RYGB) is an effective treatment for patients with type 2 diabetes (T2DM). Tight glycaemic control immediately after RYGB for T2DM may improve long-term glycaemic outcomes, but is also associated with a higher risk of hypoglycaemia. We designed a treatment algorithm to achieve optimal glycaemic control in patients with insulin-treated T2DM after RYGB and evaluated its feasibility, safety and efficacy.
Methods
Fifty patients following protocol-driven diabetes management were discharged on a fixed amount of metformin and glargine, with the insulin dose adjusted according to a standardised insulin sliding scale aiming for a fasting capillary glucose (FCG) of 5.5–6.9 mmol/L. Glycaemic outcome and remission of diabetes (defined as HbA1c < 6% and FCG levels < 5.6 mmol/L for at least 1 year without hypoglycaemic medication) were compared between patients who received protocol-driven treatment and a similar cohort of 49 patients following standard glycaemic management.
Results
At 1 year follow-up, the protocol-driven group showed a greater improvement in glycaemic control than the non-protocol-driven group (HbA1c −3.0 ± 0.2% vs. −1.2 ± 0.1%, P < 0.001; FCG levels −3.4 ± 0.2 vs. −2.0 ± 0.2 mmol/L, P = 0.02) and a higher remission rate from T2DM (50.0% vs. 6.1%, P < 0.001). No symptomatic hypoglycaemia was reported in either group.
Conclusions
The protocol-driven management proved to be feasible, safe and effective in achieving targeted glycaemic control in T2DM after RYGB. The next step will be to scrutinise the efficacy of protocol-driven management in a randomised controlled clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery and in particular Roux-en-Y gastric bypass (RYGB) have been demonstrated as effective treatment strategies for controlling glycaemia in morbidly obese [1] and overweight patients with type 2 diabetes (T2DM) [2, 3]. The incidence and prevalence of T2DM after bariatric surgery is significantly reduced compared to non-surgical management at 2 and 10 years following surgery [4]. Moreover, a recent meta-analysis of 135,246 bariatric surgery patients of whom 4,000 were diabetic reported that remission of T2DM could be achieved in 78.1% of patients [5]. Although the concept of remission of T2DM following RYGB has gained increasing acceptance in recent years, postoperative management of patients with T2DM poses a number of challenges.
Firstly, T2DM management after bariatric surgery varies extensively across centres, and secondly, the definition of remission or cure has long been controversial and thirdly no validated treatment algorithm exists to guide either patients or clinicians. Recently, the American Diabetes Association (ADA) has proposed new definitions of complete remission of T2DM, requiring a return to normal glucose values (HbA1c < 6%, fasting capillary glucose (FCG) < 5.6 mmol/L) for at least 1 year after bariatric surgery without glucose-lowering medication [6]. A previous commonly used definition for remission of T2DM only required a FCG < 7 mmol/L or a HbA1c < 6% in the absence of glucose-lowering medication [5].
This new definition from the ADA has implications for treatment as it suggests that more patients are presumed to benefit from glucose-lowering medications after bariatric surgery, causing a shift of therapeutic emphasis away from early discontinuation of glucose-lowering medications towards tighter glycaemic control after surgery. Suggestions on how to achieve the tighter glycaemic control whilst balancing the risk of hypoglycaemia have not yet been provided.
Thirdly, the time course of remission of T2DM following bariatric surgery can vary importantly from a few days to several months [5] depending on a variable improvement in insulin secretion and insulin sensitivity [7]. Therefore, predicting the timescale in which glycaemic control is achieved for any individual following bariatric surgery is often difficult [8]. In some cases, a rapid improvement in glycaemic control may necessitate a dose reduction or complete withdrawal of glucose-lowering medication immediately after surgery [9]. It is not an unusual practice in many centres therefore to stop glucose-lowering as well as antihypertensive and lipid-lowering medication directly after RYGB, in anticipation of ‘cure’ of these co-morbidities [1, 5]. Some clinicians and patients alike even tend to accept higher glucose levels in order to prevent the risk of hypoglycaemia. Other centres, however, favour tighter glycaemic control, accepting the continuation of glucose-lowering medication after surgery and the risk of hypoglycaemia associated with intensive pharmacological therapy [10, 11].
In order to establish a more standardised approach to post-bariatric surgery management of T2DM, we developed a postoperative treatment protocol based on the results of a landmark study investigating patients with T2DM folllowing biliopancreatic diversion [12]. In this study, patients were initially discharged with no glucose-lowering therapy and referred to their GP for glycaemic control [12]. The suboptimal glycaemic response achieved in this way urged the authors to manage the glycaemia of the patients intensively with frequent FCG measurements and long-acting insulin, leading to a substantial improvement in the longer term [12].
We hypothesised that a protocol widely used in the management of non-surgical patients with T2DM [13] is applicable also to a post-bariatric surgery patient population. We aimed to evaluate the feasibility, safety and efficacy of the novel treatment protocol in comparison to the glycaemic control achieved in a similar cohort of insulin-requiring T2DM patients following a non-protocol-driven management after RYGB surgery.
Methods
Patient Population and Study Design
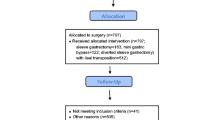
The study investigated two separate cohorts of patients to determine the outcomes of T2DM at 12 months after RYGB. The first 49 consecutively recruited patients underwent standard care for T2DM after surgery between 2009 and 2010, which did not involve a specific protocol (referred to as the non-protocol-driven management). The next 50 consecutively recruited subjects underwent protocol-driven treatment between 2010 and 2011.
Inclusion criteria included insulin-treated T2DM, aged between 18 and 65 years with a BMI ≥ 35 kg/m2 undergoing bariatric surgery. Exclusion criteria included type 1 diabetes mellitus and pregnancy.
All patients were seen in a specialist medical clinic for 3 to 6 months prior to surgery. During this period, body weight and T2DM were treated with medical therapy using the ADA and European Association for Study of Diabetes guidelines [14]. Complete remission of diabetes was defined according to the ADA consensus criteria as FCG levels of <5.6 mmol/L and HbA1c < 6% in the absence of active glucose-lowering pharmacotherapy for 1 year [15]. The study was approved by the Clinical Governance and Patient Safety Committee at Imperial College London (ref: 09/808).
RYGB Surgery and Postoperative Care
Laparoscopic RYGB was performed as previously described [16]. On admission to hospital, all regular oral glucose-lowering medication and insulin were stopped and short-acting insulin was given according to capillary glucose monitoring using a standard insulin sliding scale (Table 1). The target capillary glucose during the admission was between 5 and 8 mmol/L. Patients were allowed free fluids the morning after surgery followed by a semi-liquid diet. Glycaemic control and the use of glucose-lowering medication were assessed by the metabolic physicians at baseline and at 2 weeks and 3, 6 and 12 months after surgery, whilst patients were additionally seen by a member of the metabolic team at 10 days and 1 year after surgery.
Protocol-Driven Management
Upon discharge, 2 days after surgery, patients were prescribed metformin 1 g twice daily (if tolerated and only in cases where the estimated glomerular filtration rate was above 60 mL/min). A standard hospital inpatient sliding scale was used. The discharge dose of glargine was equivalent to a patient’s total insulin requirements during the 24 h prior to discharge. Patients were instructed to contact their designated physician daily via text message (SMS) to report their morning FCG levels obtained using Accu-Chek Advantage® (Roche Diagnostics Ltd, Hertfordshire, England, UK). Based on the reported fasting glucose values, insulin dosages were then adjusted based on a titration schedule (Table 1), aiming for FCG levels between 5.5 and 6.9 mmol/L. Patients were encouraged to additionally measure and record glucose levels if they experienced symptoms of hypoglycaemia at any point. The daily contact was discontinued once FCG values were documented between 5.5 and 6.9 mmol/L for at least three consecutive days. Thereafter, patients were encouraged to monitor their fasting and postprandial capillary glucose and to contact their physician if their glucose levels were <4.5 or >7.0 mmol/L. Plasma glucose and HbA1c levels were measured before and 3, 6 and 12 months after RYGB surgery. Metformin was continued for at least 3 months after surgery and only stopped when plasma glucose levels were ≤5.6 mmol/L.
Non-protocol-Driven Management
In the non-protocol-driven treatment group, postoperative management of glycaemia was carried out by the patient’s primary care physician or secondary care diabetologist. This approach included both the reduction and withdrawal or increase of glucose-lowering medications, but was not conducted in accordance with a standardised protocol.
Laboratory Measurements
Blood samples were obtained after an overnight fast. Commercial assays were used to measure glucose, insulin and HbA1c (Abbott, UK).
Statistical Analysis
Data are reported as means ± standard error of the mean (SEM). For comparison of continuous variables within groups, a repeated-measures ANOVA test was used to assess whether a difference in glycaemic control and in dosage of anti-diabetic drugs existed over time. For categorical data, the Cochran Q test was used. For comparisons between groups (protocol-driven versus non-protocol-driven glycaemic management), the χ 2 test was used for categorical and ANOVA for continuous variables. All P values are two-sided. A P value ≤ 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (version 17.0.1; SPSS, Inc., Chicago, IL, USA).
Results
Patient Characteristics
All 99 patients completed the 12-month follow-up assessment. The demographic characteristics of the patients are shown in Table 2. There were no significant differences between protocol-driven and non-protocol-driven patients in terms of age (46.7 ± 0.9 vs. 50.7 ± 0.9 years), sex (17:33 vs. 23:26 M/F), baseline BMI (47.6 ± 0.9 vs. 47.5 ± 0.4 kg/m2) and duration of diabetes prior to surgery (6.0 ± 0.4 vs. 6.3 ± 0.3 years). FCG was not different (P = 0.7), but baseline HbA1c levels were significantly higher (P = 0.002) in the protocol-driven management group compared to the non-protocol-driven group, suggesting a worse postprandial glycaemic control in the protocol-driven management group.
Glycaemic Control After Bariatric Surgery
In the protocol-driven group, FCG decreased significantly within the first week after surgery and plateaued within 2 to 4 weeks postoperatively (Fig. 1a). The greatest reduction in FCG concentration occurred within the first 2 weeks, with a decrease from 8.7 ± 0.3 mmol/L before to 6.7 ± 0.4 mmol/L after surgery (P < 0.0001). The mean time to reach the target FCG level (<7.0 mmol/L) was 6.0 ± 0.3 days postoperatively. Corresponding data in the non-protocol-driven group for the early postoperative phase were not collected.
At 12 months after surgery, patients in the protocol-driven group showed a mean reduction in FCG from 8.7 ± 0.3 mmol/L preoperatively to 5.3 ± 0.1 mmol/L and HbA1c from 9.1 ± 0.2% to 6.1 ± 0.1% (P < 0.001 for both). In the non-protocol-driven group, there was a mean reduction in FCG at 12 months from 8.5 ± 0.5 to 6.5 ± 0.4 mmol/L and in HbA1c from 8.0 ± 0.3% to 6.8 ± 0.6% (P = 0.007 and P = 0.009, respectively). The decrease in FCG and HbA1c at 1 year after surgery was significantly greater in the protocol-driven than in the non-protocol-driven treatment group (P < 0.001 and P = 0.02, respectively). As a result, more patients in the protocol-driven management group achieved the glycaemic target (P < 0.0001) at 1 year postoperatively than in the non-protocol-driven management group (Table 2).
Insulin Requirements
Changes in postoperative insulin requirement in the protocol-driven group are shown in Fig. 1b. All patients showed a reduction in their insulin requirements during the first postoperative week. Two weeks after surgery, the mean insulin dosage was reduced by 68 ± 2% from 50.4 ± 4 to 16.1 ± 1.4 U (P < 0.001, Table 3). Information on early changes in insulin requirements of the non-protocol-driven group was not available. After 12 months, 18% of patients in the protocol-driven group were still prescribed insulin or oral glucose-lowering medication, whilst in the non-protocol-driven group, 65% of patients were still on glucose-lowering medication (P < 0.001). The postoperative changes in glucose-lowering medication are summarised in Table 3.
Rates for Remission of Type 2 Diabetes at 12-Month Follow-up
In the protocol-driven group, 66% of patients achieved FCG levels < 5.6 mmol/L and 94% achieved FCG levels < 7.0 mmol/L at 12 months after surgery. This was significantly higher than in the non-protocol-driven group, where only 40.8% (P < 0.001) and 67.3% (P < 0.001) achieved these respective treatment targets. In the protocol-driven group, 50.0% of patients achieved a HbA1c < 6% compared to only 6.1% in the non-protocol-driven group (P < 0.001). HbA1c levels < 7% were achieved by an additional 40% of patients in the protocol-driven group and an additional 53.1% in the non-protocol-driven group (P < 0.05).
Based on the 2009 ADA consensus criteria, at 12 months after surgery, 25 patients (50.0%) in the protocol-driven group and three patients (6.1%) in the non-protocol-driven group were in complete remission of T2DM (P < 0.001). An additional 16 patients (32%) in the protocol-driven group compared to 14 (28.6%) patients in the non-protocol-driven group were in partial remission according to the ADA criteria (P = 0.08) [15].
Rates of Hypo- and Hyperglycaemia
Of the 1,558 fasting glucose measurements recorded in the protocol-driven group during the 12-month observation period, six measurements (0.4%) were <3.5 mmol/L (range 2.6–3.4 mmol/L). All six results were reported by three patients. No symptomatic hypoglycaemia with associated seizures, unconsciousness or other neuroglycopenic or autonomic symptoms was reported. For the non-protocol-driven group, these data are not available as patients were not asked to record this information, but none of the patients had documented hypoglycaemia in their hospital records.
In the protocol-driven group, four patients (7%) with postoperative wound infections showed temporarily increased insulin requirements. These patients exhibited repeated measurements with fasting glucose levels > 7.0 mmol/L during the treatment period of infections (highest measurement, 10.8 mmol/L). All four patients achieved HbA1c < 6% after 6 months.
Discussion
The findings of this study suggest that a standardised protocol for glycaemic management may offer a feasible and safe strategy for achieving glycaemic treatment goals and diabetes remission after gastric bypass. Although 50% of the patients achieved a HbA1c < 6% and another 40% a HbA1c < 7% at 12 months after surgery, only three patients had FCG recordings below 3.5 mmol/L (each patient had two recordings of a FCG < 3.5 mmol/L). No patient had any episode of clinically severe or symptomatic hypoglycaemia.
Achieving and sustaining appropriate glycaemic control in patients with T2DM undergoing bariatric surgery poses a major clinical challenge. The treatment protocol we implemented performed well despite the variations across individual patients in dietary intake, insulin resistance and insulin secretion. The most striking changes in glycaemic control were observed long before substantial weight loss occurred. This chronological sequence is consistent with the early beneficial effects of RYGB [9, 11, 17] and biliopancreatic diversion [12] on glycaemic control.
The aim of the algorithm was to achieve fasting glucose levels between 5.5 and 6.9 mmol/L, in accordance with the recently proposed new definition of diabetes remission by the ADA [6]. At a follow-up 12 months after surgery, rates of complete remission of T2DM were 50.0% in the protocol-driven treatment group and only 6.1% in the non-protocol-driven group. There was a significant difference in both glycaemic control as measured by HbA1c and FCG and in additional glucose-lowering medication used between the groups (18% in the protocol-driven group vs. 65% in the non-protocol-driven group were still on insulin at 12 months after surgery).
This study found lower remission rates than in previous studies. This probably reflects the more stringent criteria used for complete diabetes remission in our study [15] compared to those previously used [1, 5, 18, 19]. It cannot be excluded that a longer duration or an increased severity of T2DM among participants of our study may have negatively affected the remission rate [20]. The reported diabetes resolution rate of 78.1% in the 2004 meta-analysis from Buchwald et al. [5] combines data from three different surgical procedures, whilst our study refers only to patients after gastric bypass surgery.
Applying the previously used criteria of diabetes remission [5, 18, 19] to our study population, 41 patients (82.0%) in the protocol-driven group and 17 patients (34.7%) in the non-protocol-driven group achieved remission from diabetes at 1 year after surgery (Table 2). These observations are more in line with previous reports [5, 18, 19], whilst the complete remission rates based on the ADA consensus statement are consistent with recent studies referring to the same criteria [21].
The physiological mechanisms underlying the results of our study may be similar to those responsible for the results of the United Kingdom Prospective Diabetes Study, which demonstrated that tight glucose management reduces the long-term complications of T2DM [22, 23]. It is possible that the pancreas undergoes a period of regeneration within the early postoperative period, and a healthy glucose environment is beneficial for β cell function not only in the short, but in the long term. Glucotoxicity on the other hand can hamper the β cell glycaemic memory through direct and indirect immunological damage. More in depth, molecular research is needed to validate this hypothesis. Our data demonstrate that the vast majority of patients in the protocol-driven group reached the target glucose levels without an increase in adverse events. Similar results were observed in a recent randomised trial, which compared the use of once-daily glargine versus the traditional sliding scale insulin immediately after RYGB surgery [24]. In this study, control of postoperative hyperglycaemia was significantly better with the use of glargine compared to the sliding scale insulin, with few hypoglycaemic side effects.
Our results also suggest that new insulin analogues, such as insulin glargine, with more predictable activity profiles, have greatly reduced the risk of hypoglycaemia [25, 26]. In fact, close monitoring of capillary glucose levels and frequent adjustment of insulin doses may also have contributed to the low rate of hypoglycaemia seen in our study. Therefore, a systematic titration of the insulin dose as reported in the present study may offer the basis for a simple, standardised way to initiate basal insulin in routine practice. The algorithm appeared to be both feasible and safe. Nonetheless, it still needs to be determined whether better glycaemic control during the early postoperative period may also have a beneficial effect on wound healing, postoperative infection and surgical complications.
The most important limitation of our study is the non-randomised design. Another limitation of our treatment algorithm is the initial effect on the resources, mainly the increase in the workload of physicians or nurses due to the adjustment of insulin dosages daily in the first few weeks. Protocol-driven management meant about an extra 1 min per patient per day, but most patients only require 2 weeks of adjustment before becoming stable. Thus, even in very busy bariatric centres that focus on type 2 diabetes, the total number of patients does not accumulate above what can be reasonably managed. Moreover, as soon as a validated treatment protocol for post-surgery glycaemic management exists, patients can easily and independently continue with the daily adjustment. Even more important than the actual remission rate is the possibility that glycaemic control even for a short period of time may have a legacy effect impacting on long-term macrovascular outcomes [22].
In conclusion, this is the first study to examine the use of a standard basal insulin titration protocol for the glycaemic management of T2DM patients after RYGB surgery. The regime was successfully applied in clinical practice and was associated with low rates of hypoglycaemia. Randomised controlled trials with longer follow-up are needed to determine whether the treatment algorithm is actually better than traditional standard care with regard to efficacy.
References
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–56. e5.
Ramos AC, Galvao Neto MP, de Souza YM, et al. Laparoscopic duodenal–jejunal exclusion in the treatment of type 2 diabetes mellitus in patients with BMI < 30 kg/m2 (LBMI). Obes Surg. 2009;19(3):307–12.
Reed MA, Pories WJ, Chapman W, et al. Roux-en-Y gastric bypass corrects hyperinsulinemia implications for the remission of type 2 diabetes. J Clin Endocr Metab. 2011;96(8):2525–31.
Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
Arora S, Ashrafian H, Smock ED, et al. Total laparoscopic repair of sigmoid foreign body perforation. J Laparoendosc Adv S. 2009;19(3):401–3.
Pournaras DJ, Osborne A, Hawkins SC, et al. Remission of type 2 diabetes after gastric bypass and banding: mechanisms and 2 year outcomes. Ann Surg. 2010;252(6):966–71.
Hall TC, Pellen MG, Sedman PC, et al. Preoperative factors predicting remission of type 2 diabetes mellitus after Roux-en-Y gastric bypass surgery for obesity. Obes Surg. 2010;20(9):1245–50.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222(3):339–50. discussion 50–2.
Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009;360(2):129–39.
Scopinaro N, Adami GF, Papadia FS, et al. Effects of biliopanceratic diversion on type 2 diabetes in patients with BMI 25 to 35. Ann Surg. 2011;253(4):699–703.
Barnett A. Dosing of insulin glargine in the treatment of type 2 diabetes. Clin Ther. 2007;29(6):987–99.
American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33 Suppl 1:S11–61.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5.
Wyles SM, Ahmed AR. Tips and tricks in bariatric surgical procedures: a review article. Minerva Chir. 2009;64(3):253–64.
Buse JB. Can we become victims of our own success? Diabetes Care. 2009;32(11):2140–1.
Sovik TT, Irandoust B, Birkeland KI, et al. Type 2 diabetes and metabolic syndrome before and after gastric bypass. Tidsskr Norske Laege. 2010;130(13):1347–50.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–84. discussion 84–5.
Pories WJ, MacDonald Jr KG, Flickinger EG, et al. Is type II diabetes mellitus (NIDDM) a surgical disease? Ann Surg. 1992;215(6):633–42. discussion 43.
Pournaras DJ, Aasheim ET, Søvik TT, et al. Effect of the definition of type II diabetes remission in the evaluation of bariatric surgery for metabolic disorders. Brit J Surg. 2011. doi:10.1002/bjs.7704
Holman RR, Paul SK, Bethel MA, et al. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359(15):1565–76.
Nasr CE, Hoogwerf BJ, Faiman C. Effects of glucose and blood pressure control on complications of type 2 diabetes mellitus. Clev Clin J Med. 1999;66(4):247–53.
Datta S, Qaadir A, Villanueva G, et al. Once-daily insulin glargine versus 6-hour sliding scale regular insulin for control of hyperglycemia after a bariatric surgical procedure: a randomized clinical trial. Endocr Pract. 2007;13(3):225–31.
Yki-Jarvinen H. Management of type 2 diabetes mellitus and cardiovascular risk: lessons from intervention trials. Drugs. 2000;60(5):975–83.
Riddle MC, Rosenstock J, Gerich J. The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients. Diabetes Care. 2003;26(11):3080–6.
Acknowledgements
W.K.F. was supported by the German Research Society (DFG), C.W.leR. by a Department of Health clinician scientist award and A.D.M. was supported by the Medical Research Council. Imperial College London receives support from the National Institute for Health Research Biomedical Research Centre funding scheme.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This trial was registered at www.clinicaltrials.gov (NCT01213563).
Rights and permissions
About this article
Cite this article
Fenske, W.K., Pournaras, D.J., Aasheim, E.T. et al. Can a Protocol for Glycaemic Control Improve Type 2 Diabetes Outcomes After Gastric Bypass?. OBES SURG 22, 90–96 (2012). https://doi.org/10.1007/s11695-011-0543-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0543-6