Abstract
Background
Roux-en-Y gastric bypass (RYGB) is an effective treatment for morbid obesity. This bariatric procedure has also been noted to resolve hyperglycaemia in up to 70% of obese diabetics. We evaluated outcomes in diabetic patients undergoing RYGB in our institution, aiming to identify factors predicting diabetes remission.
Methods
One hundred ten type 2 diabetic (T2DM) patients undergoing RYGB were studied. Baseline demographics, diabetic status pre- and post-surgery and outcomes were evaluated. Outcomes were compared to a matched non-diabetic cohort.
Results
The mean age of the patients was 45 ± 11. The majority (70%; n = 77) were female and the mean baseline body mass index was 47 ± 7. Mean (±SD range) excess weight loss at 6, 12 and 24 months was 58.3 ± 26.4% (30.5−167%), 63.2 ± 17.2% (0−99.2%) and 84.1 ± 21.3% (16.5−121%), respectively. Diabetic medication was discontinued in 68.4% patients and reduced in a further 14.3%. Mean preoperative HbA1c was 7.1 ± 2.0 and mean postoperative HbA1c 5.48 ± 0.2. Patients with a baseline HbA1c >10 had a 50% rate of remission compared to 77.3% with an HbA1c of 6.5−7.9. The mean duration of T2DM preoperatively was 5.5 ± 7 years. A preoperative duration of T2DM greater than 10 years was shown to significantly reduce the chances of remission (p = 0.005).
Conclusions
RYGB for morbid obesity achieves significant weight reduction in diabetic patients with remission of pre-surgical hyperglycaemia in the majority. The study supports findings that a shorter duration and better control of diabetes prior to surgery corresponds to a higher rate of remission. It supports the argument for early surgical intervention in the morbidly obese diabetic patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbid obesity associated with type 2 diabetes mellitus (T2DM) is a problem because it has achieved epidemic proportions. According to the International Diabetes Federation, 80% of people worldwide with T2DM are obese at the time of diagnosis. In 2009, the prevalence of obesity in the UK was estimated at 9.9% (4.3 million individuals) and for diabetes at 5.1% (2.2 million individuals) [1]. The number of people diagnosed with diabetes increased by more than 145,000 last year [1].
“Metabolic syndrome” is defined by the World Health Organisation as a clustering of factors including dyslipidaemia, glucose intolerance and hypertension together with central adiposity. Its current prevalence estimate of 16% is expected to rise further [2, 3].
The cost implication for the linked pathologies of obesity and T2DM is vast and places a huge burden on the health care system. In the UK, an estimated 5% of the National Health Service (NHS) budget is spent on treating diabetes and its complications: this equates to £3.5 billion per year [4]. Furthermore, 10% of a hospital's budget is spent on treating diabetes and its complications [4]. Diabetics spend 1.1 million days per year in hospital for inpatient care and complications [5] and are spending over £500 million of their own money on coping with the condition, with Social Services costs for people with diabetes around £230 million [6].
Evidence suggests that T2DM can settle within days of bariatric surgery as a result of the rearrangement of small bowel anatomy and change in gastrointestinal hormones, leading to a change in insulin resistance [7–9]. In 2004, Buchwald's review of all modalities of bariatric surgery concluded that diabetes control improved in 86% and underwent remission in 76.8% [10]. This comprised an 83.7% remission in the roux-en-y gastric bypass (RYGB) cohort.
In light of these results, bariatric surgery has been proposed as an attractive option in the obese diabetic patient in whom metabolic surgery confers the potential additional benefit of cost-effective treatment of T2DM [11]. The improvements in glycaemic control are independent of weight loss and appear superior to medical treatment [12]. Indeed, it has been suggested that RYGB should be considered the standard treatment of T2DM in morbidly obese patients who are appropriate surgical candidates [12].
We conducted a study to evaluate the rates of T2DM resolution following RYGB in our institution and made attempts to identify, where possible, any predictors of remission with the hope that this may allow the selection of the optimal diabetic surgical candidate. We also included a matched non-diabetic cohort to compare other outcomes.
Methods
Patient population
Data from 621 patients undergoing RYGB at our institution from March 2000 to October 2008 were prospectively collected and entered into an electronic database. Four laparoscopic bariatric surgeons at a university centre with a comprehensive bariatric programme performed surgery. All patients met the National Institute of Clinical Guidelines (NICE) criteria for surgery [13].
Outcomes and definitions
T2DM was defined as treatment with diabetic medication preoperatively or having been diagnosed by the patient's general practitioner. Patients with ‘diet only’ controlled diabetes were not included. Outcomes measured were changes in preoperative HbA1c levels, remission of diabetes (as defined below), body mass index (BMI) and excess body weight loss. Excess weight was defined as operative weight minus ideal weight (based on a BMI of 25 kg/m2). Preoperative diabetic status and HbA1c was recorded in pre-surgical assessment clinic held within 4 weeks prior to RYGB. Postoperative diabetic status and HbA1c was recorded from the first review clinic after RYGB.
Postoperative remission of diabetes was defined as ‘cessation of hypoglycaemic agents and return to normal range glycosylated haemoglobin (HbA1c <6.5)’. Improvement was defined as a ‘reduced postoperative HbA1c or a reduction and/or discontinuation of a single hypoglycaemic agent in polytherapy management but that was inadequate to be defined as remission’. Recent guidelines suggest the term ‘remission’ of T2DM after bariatric surgery is more appropriate than ‘cure’ or ‘resolution’, as implicit in the former is the possibility of disease recurrence [14].
Evaluation of predictors for remission
Baseline HBA1c values were subdivided into groups to further evaluate any influence upon postoperative remission rates. Remission rates were further evaluated in the context of duration of diabetes.
Outcomes compared to non-diabetics
In order to assess postoperative weight loss for this cohort, we performed a case-matched comparison using each consecutive non-diabetic patient undergoing RYGB surgery in the same time period. Patients were matched for age, gender and baseline BMI.
Statistical analysis
SPSS v11.5 was used for analysis. Categorical data were analysed using the Pearson Chi square test. Paired data were analysed using the Student's T test for parametric data and Wilcoxon signed ranks for non-parametric data.
Results
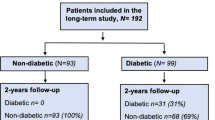
Of the 621 patients, 110 (17.7%) were diagnosed with T2DM, of whom 70% were female. Preoperatively, 28 patients were on insulin together with oral hypoglycaemic agents. The remaining 82 patients were on oral hypoglycaemic therapy only. Twelve patients were lost to follow-up.
The non-diabetic cohort was matched for median age and preoperative BMI (Table 1). There was a statistically higher prevalence of females in the diabetic patients (89% vs 69%, p = 0.001).
There was remission of T2DM in 68.4% (n = 67) and improvement in a further 14.3% (n = 14) subjects. Seven patients had a reduction in insulin and/or oral hypoglycaemic agent and seven had a reduction in oral agent alone. Pre- and postoperative HbA1c was available in 50 (45%) of the cohort. Mean preoperative (range) HbA1c was 7.1 ± 2 (5.3−13.5) and mean postoperative was 5.48 ± 0.2 (5.2−8.7). Postoperative HbA1c was measured a mean of 14 months (range 3−27) following surgery. Diabetic status postoperatively was recorded a mean 2.8 ± 1.8 months after RYGB in the follow up clinic. Medication use pre- and post-surgery is shown in Table 2.
The mean (range) percentage excess weight loss (%EWL) in the diabetic cohort at 6, 12 and 24 months was 58.3 (30.5−167, n = 103), 63.2 (0−99.2, n = 53) and 84.1 (16.5−148, n = 34), respectively. Our results revealed a tendency towards inferior weight loss in the diabetic cohort compared to non-diabetics after RYGB; this was not statistically significant (p > 0.05). The study did not evaluate differences in morbidity between the cohorts.
Preoperative duration (in years) of diabetes was available in 71 patients, representing 66% of the cohort. The mean duration (range) of diabetes was 5.5 years (1−21). As duration of diabetes increased, there was a trend towards reduced remission rates from 75% to 33% when duration was grouped in 2-year intervals (Fig. 1). Pearson Chi-square analysis confirmed that a preoperative duration of T2DM greater than 10 years conferred a significant reduction in successful diabetes remission after RYGB (p = 0.005).
Patients with a preoperative HbA1c >8 achieved lower postoperative normoglycaemia rates compared to those with a preoperative HbA1c <8, though this was not statistically significant (Pearson Chi-square p = 0.16, Table 3). One hundred percent of patients with available HbA1c data achieved a statistically significant drop in postoperative HbA1c irrespective of their baseline value (Student's T test, p < 0.05; Table 4).
Discussion
T2DM is regarded as a progressive disease with the pathophysiology being that of impaired tissue sensitivity to insulin. The course of the disease is traditionally controlled with life-style changes, dietary measures, oral hypoglycaemic agents and insulin. Non-surgical and medical therapy has, until now, been the popular method of achieving glycaemic ‘control’, with even the best treatment reducing the HbA1c only by 1−2% [15]. Additionally, the progressive nature of diabetes is epitomised by the failure of monotherapy to control diabetes after 3 years of the disease [16].
A strategy for the management of T2DM, even in brittle diabetes, does not yet include a surgical arm [17]. This is despite evidence that mortality is reduced with bariatric surgery in obese diabetic subjects. In addition to demonstrating a reduction in overall mortality from all bariatric procedures, the Swedish Obesity Subjects study in diabetic patients demonstrated that annual mortality could be reduced by 80% in the cohort treated surgically [18, 19]. This corresponded to 9% mortality in obese diabetics in the cohort treated surgically compared to 28% in the control group at 9 years. Adams et al. retrospectively compared nearly 10,000 RYGB patients to matched controls, noting diabetes-related mortality was reduced by 92% [20].
Studies have, in addition, demonstrated the positive economic impact of bariatric surgery as a whole. Previous studies, in the open surgery era, have suggested a 9-year period to recoup the costs of bariatric surgery [21]. More recent studies conclude that, when surgery is performed laparoscopically, the costs incurred are estimated to be recouped within 2 years and within 4 years for open surgery [22]. Ikramuddin et al. demonstrated that, when compared with medical management, RYGB for obese diabetics has a cost-effectiveness ratio of $22,000 per quality-adjusted life-year gained [23]. The study has, however, been criticised for overestimating the cost effectiveness of surgery as it failed to account for weight regain 2 years after RYGB.
Several factors may explain why historically few primary care physicians have counselled obese diabetics on surgical rather than pharmaceutical management of T2DM. These include poor dissemination of the increasing evidence of bariatric surgery's benefit, limited understanding of the mechanisms involved and a reluctance to accept a potential paradigm shift in treatment
The mechanisms behind the rearrangement of small bowel anatomy stimulating remission of T2DM are complex. Changes related to the bypass procedure include altered gut hormone secretion. Gut hormones such as incretins, ghrelin and glucagon-like peptide-1 have been implicated in the role of T2DM pathophysiology [24]. It may be the combination of such hormonal changes combined with foregut exclusion and increased nutrient delivery more distally that are responsible for the antidiabetic pathophysiology [25].
In our institution's experience, diabetes remission is achieved in 68.4% of obese subjects undergoing RYGB, which is similar to reported rates of remission in the literature. Buchwald's meta-analysis described a mean rate of T2DM remission after RYGB of 83.7% (95% CI 77.3−90.1%) [10]. Our lower remission rates might be explained by our strict definition of diabetes; some studies include impaired glucose tolerance subjects, who in turn may show increased propensity to respond to RYGB.
Our results suggest that a preoperative duration of diabetes greater than 10 years and poor preoperative glycaemic control (HbA1c >10) confer inferior remission rates in obese diabetics. The finding supports the results reported by other authors [26]. Although our findings suggest that obese diabetic subjects achieve a weight reduction comparable to that of non-diabetics, previous studies have shown inferior weight loss of diabetics compared to non-diabetics [26, 27].
Predictors of diabetes remission by other authors include EWL in excess of 31% at 6 months and a shorter duration of diabetes preoperatively [28, 29]. Torquati et al. found that patients with a smaller preoperative waist circumference and those on oral hypoglycaemics, as opposed to insulin, were more likely to achieve remission [11]. Whilst we found that a duration of diabetes greater than 10 years predicts remission, Schauer et al. concluded that patients with less than 5 years of the disease, diet controlled T2DM and the greatest weight loss after surgery were most likely to achieve complete remission of T2DM after RYGB [26]. The disparity in our results may be due to relatively smaller numbers, with diabetics representing only 17.7% of all RYGB performed in this time period. Further experience will be invaluable in clarifying the pattern of response.
Long-term weight control may be important for durable diabetes remission. In their 5-year follow-up study of RYGB outcomes in 177 obese diabetics, Chikunguwo et al. found that T2DM recurred in 43.1% of subjects, which was associated with the regaining of lost weight [30]. They also demonstrated higher rates of remission in the female population despite better durability in males. Our study also demonstrated higher rates of remission in females compared to males (74% vs 18%); however, the male group contained only small numbers (n = 11).
Controversy still exists over which bariatric procedure achieves the greatest rate of remission. Buchwald reported a lower rate with purely restrictive intervention (laparoscopic adjustable gastric band (LAGB)) when compared to the malabsorptive procedures (RYGB and biliopancreatic diversion (BPD)) [10]. In contrast, Parikh report an equivalent rate of remission between LAGB, RYGB and BPD despite the disparity in %EWL [28]. Parikh and colleagues described a %EWL at 1 and 2 years after RYGB of 66% and 68%, respectively. They reported the proportion of patients at 1 year requiring insulin at 7%, reduced from 28% preoperatively. Oral hypoglycaemic requirements at 1 year were 22%, reduced from 87% preoperatively. Our study complements these findings, demonstrating 1- and 2-year %EWLs at 63.2% and 84.1%, respectively. The proportion of patients at 1 year requiring insulin was 8.2%, reduced from 26.5% preoperatively, and for oral hypoglycaemics was 23.5%, reduced from 73.5% preoperatively.
Current NICE guidelines only permit surgery in diabetics with a BMI exceeding 35. Increasing interest surrounds the non-obese subject and the concept of ‘metabolic surgery’, although only a few small studies have examined subjects with a BMI <35. Shah et al. reviewed RYGB outcomes in 15 diabetics with a BMI between 20 and 34. Although lacking long-term follow up, these results demonstrated a 100% remission of T2DM at 9 months [31]. The mean postoperative HbA1c fell from 11 ± 3.5% to 5.9 ± 1.5%, with a mean BMI change of 2 ± 1.5 kg/m2. However, conflicting data have emerged from other authors. Lee et al. compared 44 subjects with a BMI <35 to 114 subjects with a BMI >35. They concluded that laparoscopic gastric bypass resulted in a return to normoglycaemia in 89.5% with a BMI <35 compared to 98.5 with a BMI > 35 at 12 months postoperatively [32].
Studies have demonstrated that the predisposition to central obesity, despite a relatively low BMI, is core to the development of high metabolic risk factors [33]. A study from China has noted that, in a population with a 4.3% prevalence of obesity, the prevalence of T2DM was more than double at 9.8% [34]. This suggests that the BMI definition may have limitations in the context of metabolic syndrome. In light of such findings, the Asia-Pacific Bariatric Society has altered its indication for bariatric surgery to subjects with T2DM and a BMI >32 [35]. Long-term data in non-obese diabetic subjects are yet to be published.
Our data confirm that laparoscopic RYGB for morbid obesity achieves significant weight reduction in the diabetic population with the additional benefit of achieving normoglycaemia in a substantial proportion. This study suggests that a shorter duration and better control of diabetes prior to surgery may predict a better rate of disease remission. It supports the argument for early surgical intervention in the morbidly obese diabetic patient.
References
Diabetes UK. www.diabetes.org.uk
National Institute for Health. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001;285(19):2486–97.
Wild S.H, Byrne C.D. The global burden of the metabolic syndrome and its consequences for diabetes and cardiovascular disease. The Metabolic Syndrome. 2005:1–43
National Service Framework for Diabetes: Standards, 2002
Coronary Heart Disease statistics, Diabetes supplement, British Heart Foundation Statistics Database 2001
Williams R, Gillam S, Murphy M. The true costs of Type 2 diabetes in the UK. Findings from T2ARDIS and CODE-2 UK. GlaxoSmithKline Uxbridge, UK; 2002
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg. 1995;222:339–50.
Rubino F, Marescaux J. Effect of duodenal–jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239:1–11.
Whitson B, Leslie D, Kellogg T et al. Entero-endocrine changes after gastric bypass in diabetic and nondiabetic patients: a preliminary. Study J Surg Res. 141;1:31−39
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-anlysis. JAMA. 2004;292:1724–37.
Torquati A, Lufti R, Abumrad N, et al. Is Roux en Y gastric bypass surgery the most effective treatment for type 2 diabetes mellitus in morbidly obese patients? J Gastrointest Surg. 2005;9(8):1112–6.
Keating CL, Dixon JB, Moodie ML, et al. Cost-efficacy of surgically induced weight loss for the management of type 2 diabetes. A randomised controlled trial. Diabetes Care. 2009;32:580–4.
NICE 2002/041. www.nice.org.uk/guidance
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? ADA consensus statement. Diabetes Care. 2009;32(11):2133–5.
Inzucchi SE. Oral antihyperglycaemic therapy for type 2 diabetes. JAMA. 2002;287:360–72.
Turner RC, Cull CA, Frighi V, et al. Glycaemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus. JAMA. 1999;281:2005–12.
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycaemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy. Diab Care. 2008;31:173–5.
Sjostrom C, Lissner L, Wedel H, et al. Reduction in incidence of diabetes, hypertension and lipid disturbances after intentional weight loss induced by bariatric surgery: the SOS intervention study. Obes Res. 1999;7:477–84.
Sjostrom L, Narbro K, Sjostrom D, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;23(357):741–52.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357:753–61.
Finkelstein EA, Brown DS. A cost benefit simulation model of coverage for bariatric surgery among full time employees. Am J Manag Care. 2005;11(10):641–6.
Cremieux PY, Buchwald H, Shikora SA, et al. A study on the economic impact of bariatric surgery. Am J Manag Care. 2008;14(9):589–96.
Ikramuddin S, Klingman D, Swan T, et al. Cost-effectiveness of Roux-en-Y gastric bypass in type 2 diabetic patients. Am J Manag Care. 2009;15(9):607–15.
Thaler JP, Cummings DE. Minireview: hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009;150(6):2518–25.
Rubino F, Moo TA, Rosen DJ, et al. Diabetes surgery: a new approach to an old disease. Diab Care. 2009;32(2):S368–72.
Schauer PR, Burguera B, Ikramuddin S, et al. Effect of laparoscopic roux-en y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–85.
Wittgrove A, Grove G. Laparoscopic gastric bypass, Roux en Y 500 patients: techniques and results, with 3-60 month follow up. Obes Surg. 2000;10:233–9.
Parikh M, Ayoung-Chee P, Romanos E, et al. Comparison of rates of resolution of diabetes mellitus after gastric banding, gastric bypass and biliopancreatic diversion. J Am Coll Surg. 2007;205(5):631–5.
Dolan K, Bryant R, Fielding GA. Treating diabetes in the morbidly obese by laparoscopic gastric banding. Obes Surg. 2003;13(3):439–43.
Chikunguwo S, Dodson PW, Meador JG et al. Durable Resolution of Diabetes after Roux en-Y Gastric Bypass is Associated with Maintenance of Weight Loss. Abstracts: 2009 Plenary Session/ SOARD 5 (2009) S1-S23. PL-101
Shah SS, Todkar JS, Shah PS. Should Gastric Bypass Operation be Done for Type 2 Diabetes in Subjects with Body Mass Index 20-34 kgs/m2? An initial Indian experience. Abstracts: 2009 Plenary Session/ SOARD 5 (2009) S1-S23. PL-107
Lee WJ, Wang W, Lee YC, et al. Effect of laparoscopic mini-gastric bypass for type 2 diabetes mellitus: comparison of BMI >35 and <35 kg/m2. J Gastrointest Surg. 2008;12(5):945–52.
Deurenberg P, Deaurenberg-Yap M, van Staveren WA. Body mass index and percent body fat: a meta-analysis among different ethnic groups. Int J Obes. 1998;22:1164–71.
Jia WP, Lu JX, Xiang KS, et al. Epidemiological study on obesity and its comorbidities in urban Chinese older than 20 years of age in Shanghai, China. Obes Rev. 2002;3:157–65.
Lee WJ, Wang W. Bariatric surgery: Asia-pacific perspective. Obes Surg. 2005;15:751–7.
Conflict of interest disclosure
The authors declare that they have no conflict of interest. Results were presented at the EAES congress 2009 (oral) and IFSO 2009 (poster).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hall, T.C., Pellen, M.G.C., Sedman, P.C. et al. Preoperative Factors Predicting Remission of Type 2 Diabetes Mellitus After Roux-en-Y Gastric Bypass Surgery for Obesity. OBES SURG 20, 1245–1250 (2010). https://doi.org/10.1007/s11695-010-0198-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0198-8