Abstract
Background
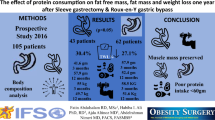
Daily protein intake recommendations have recently been proposed for the bariatric patient. We aimed to evaluate the accomplishment of these recommendations, and the influence of protein intake (PI) on fat free mass (FFM) and protein status changes following bariatric surgery.
Methods
We examined 101 consecutive patients undergoing laparoscopic Roux-in-Y gastric gypass (LGBP) or laparoscopic sleeve gastrectomy (LSG). Based on 3-day food records, PI from food and supplements were quantified at 4, 8, and 12 months after surgery. The association between PI and body composition (bioelectrical impedance), plasma albumin and pre-albumin was evaluated at all study time points.
Results
A PI <60 g/day was present respectively in 45%, 35%, and 37% of the cohort at 4, 8, and 12 months after surgery (p < 0.001 relative to baseline). Despite our universal recommendation of protein supplementation, supplements were taken only by 63.4, 50.5, and 33.7% of the participants at 4, 8, and 12 months. However, protein supplementation was effective in helping patients to achieve the daily protein intake goal. In linear regression analysis, male gender and weight loss, but not PI, were significantly associated with loss of FFM (p < 0.001). No significant correlation between PI and plasma albumin or pre-albumin was found.
Conclusions
Our study underscores the value of protein supplementation for the achievement of the recommended daily protein intake in the bariatric patient. However, our data does not help to define a PI goal as critical in determining the FFM and protein status changes following LGBP or LSG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Bariatric surgery is currently the most successful weight loss strategy for morbid obesity [1]. Despite the goal of weight loss in morbid obesity being loss of fat mass (FM), weight loss interventions are systematically accompanied by some degree of fat free mass (FFM) loss [2]. Importantly, not only a greater caloric restriction, but also certain types of bariatric surgery techniques such as Roux-in-Y Gastric Bypass (GBP) and Bilopancreatic Diversion (BPD) are accompanied by a larger loss of FFM [2]. In contrast, exercise [2], and a higher protein intake [3] have been demonstrated to influence body composition changes following weight loss in a way that spares FFM. Likewise, a higher protein intake has been shown to positively influence plasma protein status following GBP [4].
The current guidelines for nutritional support of the bariatric surgery patient state that protein intake with meals, including supplementation, should be in the range of 60–120 g/day [5]. Specifically for those with GBP, a daily protein intake ≥60 g is recommended. Nonetheless, this recommendation is not without limitations. First, as acknowledged by the guidelines writing committee, there is no conclusive evidence to support this recommendation [5]. Second, protein intakes in the range of 70–100 g/day or 0.8–1.5 g/kg ideal body weight (IBW)/day are typically advised in forms of caloric restriction comparable to that after bariatric surgery such as in the very low calorie diets (VLCD) [6]. Importantly, VLCD are designed to produce rapid weight loss while preserving lean body mass [2, 6]. Third, to our knowledge there is no data on the impact of supplementation on daily protein intake after GBP. Finally, it should be taken into account that no matter the daily protein intake goal, protein-deficient meals are common after GBP. This phenomenon has been largely attributed to the common development of intolerance to protein-rich foods occurring more often in the first year after surgery [7, 8].
Against this background, the purpose of the present study was to examine the accomplishment of the recommended protein intake, and the influence of protein intake on FFM and protein status following bariatric surgery.
Subjects and Methods
During the period October 2006 to April 2007, 101 consecutive patients scheduled to undergo laparoscopic Roux-in-Y gastric gypass [9] or laparoscopic sleeve gastrectomy (LSG) [9], and without evidence of clinical edema, were recruited to this observational study. Indications for surgery followed the National Institutes of Health criteria, i.e., a body mass index (BMI) >40 kg/m2 or a BMI >35 kg/m2 with obesity-related morbidity [5]. All patients signed informed consent before surgery, and the protocol was approved by our institution ethics committee.
Protein Intake Counseling
Prior to surgery, all subjects attended group and individual sessions including nutritional counseling according to the current guidelines for the bariatric patient [5]. Dietary advice was systematically given to the patients during hospitalization, and at 2 and 6 weeks after surgery, and then at 4, 8, and 12 months, to sustain a hypocaloric and protein-rich diet. Following hospital discharge, patients were universally advised to supplement dietary protein with 15 g of protein powder (Resource Protein, Nestlé, Vevey, Switzerland). Based on 3-day dietary food records, protein intake from food and supplements was quantified at each follow-up visit. Patients were categorized based on the accomplishment of two daily protein intake goals: ≥60 g/day or ≥1.2 g/kg IBW/day. The ≥1.2 g/kg IBW/day goal was based on the recommendations in VLCD [5, 9]. At each study visit, dietary and supplementation protein were advised to achieve the daily protein intake goals.
Body Composition Analysis
Anthropometry and body composition were evaluated prior to surgery, and a 4, 8, and 12 months after surgery. Patients were weighed and body composition was obtained using bioelectrical impedance analysis (BIA; Tanita BC-418 MA, Body Composition Analyzer). Patients were evaluated after an overnight fast, and according to the specifications from the manufacturer. BIA is based on the fact that lean tissue has more electrolyte and water content than fat. This difference in electrolyte content permits an estimate of fat free mass (FFM) measuring the amount of electricity that flows through the body from the source, to the sink electrodes. FFM estimates obtained from the body composition analysis, were used to derive total fat mass (FM), and the percent of body weight (BW) loss consisting of FFM at any particular study time point \( \left[ {{1}00*\left( {{\hbox{FFM}}{{\hbox{t}}_{\rm{t}}} - {\hbox{FFM}}{{\hbox{t}}_0}} \right)/\left( {{\hbox{BW}}{{\hbox{t}}_{\rm{t}}} - {\hbox{BW}}{{\hbox{t}}_0}} \right)} \right] \).
Biochemistry
Prior to surgery, and a 4, 8, and 12 months thereafter, blood samples were drawn following an overnight fast for the determination of albumin, pre-albumin, and total leukocyte count were measured using an Advia 2400 analyzer (Bayer Diagnostics, Tarrytown, NY, USA), high-sensitive C-reactive protein (hs-CRP) was determined by inmunonefelometry (Boehring Nephelometer analyzer; Dade Boehring, Marburg, Germany). Based on plasma protein levels, subjects were categorized as hypoalbuminemic (<35 g/L), or with mild pre-albumin deficiency (<0.170 g/L) [10].
Statististical Analysis
Values are given as mean ± SEM unless otherwise specified. Paired or unpaired non-parametric tests were used for comparisons between groups. Partial correlation analysis was used to evaluate the association between variables, while controlling for the pre-surgical BMI was performed. A one-way between-groups analysis of covariance was used to compare FFM loss between groups while adjusting for the pre-surgical BMI. P values <0.05 were considered significant. For linear regression analysis, variables were Ln-transformed. Data were analyzed using the Statistical Package for Social Science (SPSS 16.0; SPSS Inc, Chicago, IL, USA).
Results
The study cohort was composed by 76 females and 25 males with an age of 43.2 ± 1.0 years, and a pre-surgical BMI of 47.7 ± 0.7 kg/m2. LGBP and LSG were performed respectively in 66.3% and 33.7% of the cohort. The retention rate in the study was 96% or greater at all study time points.
Daily Caloric and Protein Intake
Data on daily caloric intake and protein intake are shown in Table 1. Total daily caloric intake was markedly reduced at 4 months after surgery and gradually increased over time. Similarly, daily protein intake was markedly reduced at 4, 8, and 12 months when compared to the pre-surgical situation (p < 0.001). Despite our universal recommendation of protein supplementation, supplements were taken only by 63.4, 50.5, and 33.7% of the study participants at 4, 8, and 12 months, respectively. The amount of protein from supplements varied widely among individuals (2.5–40.0 g/day). At 4, 8, and 12 months protein from supplements represented respectively 15.6 ± 3.1, 13.9 ± 0.9, and 12.2 ± 0.9% of the daily total protein intake.
At baseline, 5% and 32% of the study cohort reported, respectively, <60 g/day and <1.2 g/kg IBW/day of total protein consumption. The percentage of subjects consuming <60 g of protein per day was 45%, 35%, and 37%, respectively, at 4, 8, and 12 months after surgery (p < 0.001 for all comparisons relative to baseline). Likewise, the percentage of subjects consuming <1.2 g/kg IBW per day was 87%, 75%, and 68%, respectively, at 4, 8, and 12 months after surgery (p < 0.001 for all comparisons relative to baseline). No differences were found when the two types of surgeries were compared. As shown in Fig. 1 (panel A and B), protein supplementation was effective in helping patients to achieve the daily protein intake goals. At all post-surgical study points, a daily protein intake of ≥60 g/day (Fig. 1, panel A) and ≥1.2 g/kg IBW/day (Fig. 1, panel B) was attained significantly by a larger proportion of subjects consuming protein supplements when compared to those not adhering to the recommendation.
Percentage of patients achieving a protein intake ≥60 g/day (a) or ≥1.2 g/IBW/day (b) throughout the study according to their adherence to protein supplementation. IBW ideal body weight. Black bars patients not adhering to protein supplementation. White bars patients adhering to protein supplementation. a p < 0.001, b p < 0.005, c p < 0.05
Body Composition
Anthropometric and body composition data are shown in Table 2. On average, at 4, 8, and 12 months follow-up, patients had lost 38.2%, 57.5%, and 64.5%, respectively, of their pre-surgical excess body mass index. At all study time points, the majority of weight loss corresponded to loss of FM (4 months, 73.2 ± 8.9%; 8 months, 77.3 ± 7.1%; 12 months, 77.1 ± 8.4%). FFM loss as a percent of total body weight loss was larger at 4 months (26.3 ± 0.8%) compared to 8 months (22.2 ± 0.6%; p < 0.001), and 12 months (22.1 ± 0.8%; p < 0.001). A large inter individual variability in the amount of FFM loss relative to the total weight loss was observed (4 months, 6.9–56.8%, 8 months, 2.2–33.1%, 12 months, 3.3–51.5%). On partial correlation analysis, FFM loss was significantly correlated with total body weight loss at all study time points independently of the initial BMI (4 months, rho = 0.508, p < 0.001; 8 months, rho = 0.711, p < 0.001; 12 months, rho = 0.644, p < 0.001).
We did not find a significant correlation between the protein intake (expressed as grams of ingested protein per kilogram of ideal body weight) and FFM loss relative to total weight loss even when controlling for the pre-surgical BMI (4 months, rho =−0.06, p = 0.546; 8 months, rho = 0.07, p = 0.506, 12 months, rho = 0.02, p = 0.836). As shown in Table 3, using one-way ANCOVA analysis, the FFM loss relative to total weight loss adjusted for the pre-surgical BMI was not significantly different at any time point when subjects achieving or not the 60 g/day and 1.2 g/kg IBW/day protein intake goals were compared. Similarly, we did not find a significant correlation between protein intake and FFM loss relative to the pre-surgical FFM. The type of bariatric surgery did not influence the observed results.
Male gender was associated with a greater proportion of weight loss as FFM (4 months, male 28.9 ± 2.1%, female 23.8 ± 1.2%, p < 0.05; 8 months, male 26.3 ± 1.1%, female 20.9 ± 0.6%, p < 0.001; 12 months, male 26.7 ± 1.4%, female 20.6 ± 0.8%, p < 0.001). Moreover, male gender and weight loss were the only factors significantly associated with loss of FFM (p < 0.001) at all study time points in a linear regression analysis including also pre-surgical BMI, type of surgery, caloric intake, and protein intake as independent variables. This was despite daily protein intake adjusted per IBW being similar between the two gender groups (4 months, male 0.87 ± 0.28 g, female 0.85 ± 0.29 g, p = 0.767; 8 months, male 1.05 ± 0.29 g, female 1.00 ± 0.25 g, p = 0.343; 12 months, male 1.10 ± 0.37 g, female 1.07 ± 0.34 g, p = 0.695). In males, a daily protein intake <60 g (<60 g/day 31.5 ± 1.4%, ≥60 g/day 25.1 ± 1.8%; p < 0.05) but not <1.2 g/ideal body weight (p = 0.614) was associated with a larger FFM loss at 4 months after surgery. Significant associations were not found between protein intake and FFM loss at any other time points neither in males nor in females.
Biochemistry
As shown in Table 4, serum albumin and pre-albumin levels tended to decrease over time. However, no study participant presented with an albumin plasma concentration below the 35 g/L threshold. In contrast, 39%, 22%, and 18% of the study subjects presented pre-albumin plasma levels below normal (0.170 g/L) at 4, 8, and 12 months, respectively. Likewise, neither the plasma albumin or pre-albumin, nor the changes in these parameters relative to baseline were significantly different when subjects achieving the 60 g/day or the 1.2 g protein/IBW/day were compared. CRP and the total leukocyte count also decreased over time (Table 4, p < 0.001). CRP and pre-albumin levels were significantly inversely correlated at 4 months after surgery (rho = −0.233, p = 0.023). A tendency toward statistical significance between the two parameters was found at 8 months (rho =−0.181, p = 0.075), but not at 12 months (p = 0.564). Albumin plasma concentration was not significantly correlated with CRP or the leukocyte count. Inflammatory parameters were not significantly associated with the changes in FFM at any study time point.
Discussion
The data from our observational study show that protein intake is below the current recommendations (≥60 g/day) in a high proportion of subjects undergoing LGBP or LSG, and that protein supplementation facilitates achieving the proposed protein intake goals. Although achieving a daily protein intake ≥60 g may be beneficial in some subgroup of bariatric surgery patients, our data does not support this protein target as a strong determinant of FFM loss following bariatric surgery. Finally, our data show that systemic inflammation rather than protein intake is a determinant of the changes in plasma protein status in the early stages after bariatric surgery.
A low protein intake following GBP surgery has previously been described. Bavaresco et al. reported a mean total daily protein ranging from 37.1 ± 20.0 g during the third month to 46.6 ± 20.0 g/day at 12 months after surgery [11]. Moizé et al. reported a protein intake (g/day) of 45.6 ± 14.2 at 3 months and 58.5 ± 17.1 at 12 months after gastric bypass [7]. Daily protein intake in our study participants was slightly larger. However, this could be attributed at least in part to our universal recommendation of protein supplementation. In fact, in our cohort average protein intake in those not taking supplements was respectively 45.4 and 64.7 g/day at 4 and 12 months after surgery. Although a daily protein intake ≥60 g is currently recommended for bariatric patients [5], over one third of our study participants did not meet this goal. Previous studies on the bariatric patient, have not analyzed the proportion of subjects fulfilling this specific protein intake target [7, 11]. Insufficient protein consumption, possibly mediated by protein intolerance has been advocated as potential mechanism for the low protein intake following GBP [7]. Of note, in our study protein supplementation was useful to achieve the protein intake goal. Protein supplementation was recommended neither in Bavaresco’s nor in Moizé’s studies. In fact, Brolyn et al. [12] survey showed that protein supplements were routinely prescribed in 21% of BPD patients but not after GBP. Despite protein supplements being universally recommended in our study, data also showed a poor compliance with protein supplementation. Therefore, in the bariatric patient efforts should be made not only to universalize protein supplementation but also to increase the adherence to protein supplements in order to achieve a daily protein intake ≥60 g.
Loss of FFM may be undesirable if excessive as non-adipose tissues are responsible for the majority of resting metabolic rate and maintenance of function as the body ages. As shown with other weight loss interventions [2, 13], we found a large inter-individual FFM loss variability following surgery. We aimed to evaluate the relative contribution of protein intake on that variance in FFM loss. It has been proposed that following energy restricted diets, lesser FFM loss as a percentage of total weight loss is achieved with larger daily protein intakes [3, 14, 15]. In contrast to these findings, none of the protein intake estimates (total daily protein intake, daily protein intake/IBW, protein intake above or below 60 g/day or 1.2 g/IBW/day) was significantly correlated with FFM loss relative to total weight loss when all patients in our cohort were combined. In fact, only in males a protein intake of <60 g/day was significantly associated with a larger FFM loss at 4 months after surgery. A larger average FFM loss in males compared to females following different type of weight loss interventions has previously been reported [2, 16]. To our knowledge, no previous study has looked at the impact of protein intake on the changes in body composition following LGBP or LSG. Contradictory findings among different studies on the effects of protein intake on body composition may relate to the small sample sizes, different durations of follow-up, and differing methods of assessing body composition. Nonetheless, it should be taken into account that the factors influencing body composition changes associated with weight loss may differ depending on the weight-loss strategy [2].
Several mechanisms, including insufficient protein intake [4], may potentially lead to protein deficiency after bariatric surgery [17]. As shown by others [18, 19], in our cohort albumin and prealbumin levels decreased after bariatric surgery compared to the presurgical period. No individual in our cohort presented with a plasma albumin level <35 g/L. Despite deficits in albumin have been reported in as much as 13% of patients following the distal GBP, albumin deficiency has seldom been reported when the limb length does not exceed 150 cm as in our study [17–19]. The proportion of subjects in our cohort with plasma prealbumin <0.170 g/L varied between 18 and 39%. This is larger than previously reported by Coupaye et al. [19]. Nonetheless, in that study a prealbumin cut-off level of 0.110 g/L was considered. In fact, only 1% of our study cohort presented with prealbumin <0.110 g/L. We did not find a significant relationship between protein status and protein intake. This is in contrast with data reported by Rinaldi Schinkel et al. [4], who found a positive linear relationship between protein intake and serum albumin in patients undergoing GBP. However, subjects in that study were selected on the basis of the presence of postoperative complications requiring nutrition support services. Our finding on the significant correlation between CRP and pre-albumin levels at 4 months after surgery is in agreement with systemic inflammation being a determinant of prealbumin plasma levels after surgery [10].
It has been shown that diversionary surgery results in greater FFM loss than purely restrictive bariatric surgery procedures such as adjustable gastric banding, independently of initial BMI and the magnitude of weight loss [2]. In our study, body composition and protein status changes were comparable between LGBP and LSG. Likewise, the type of surgical procedure was not significant in the linear regression analysis on the factors potentially influencing FFM loss in our bariatric surgery cohort. This finding could be interpreted in the context of the several similarities between LGBP and LSG that support that the latter should not be considered as a purely restrictive procedure [9, 20].
We acknowledge that our study has several limitations. First, a small sample size and the observational nature may have underpowered our study to demonstrate the relationship between FFM loss and protein intake. Nonetheless, to our knowledge, no previous study has attempted to evaluate the effects of protein intake on the preservation of FFM following bariatric surgery. Second, we used BIA for body composition analysis. BIA represents a simple, inexpensive, non-invasive, and attractive method for repeated measurements of body composition assessment. However, BIA is not without limitations especially in the extremely obese population [2]. Although some authors have proposed the validity of BIA in the assessment of body composition after bariatric surgery [14, 21], future studies evaluating the importance of protein intake on FFM loss should be based on more accurate methods of body composition analysis. Second, we did not estimate physical activity. Data from rigorously supervised resistance and aerobic exercise programs has shown decreases in the loss of FFM attributable to physical activity [22, 23]. Even so, neither reported physical activity nor total or activity energy expenditure measured by doubly labeled water technique have been shown to be associated with body composition changes following GBP [14].
In summary, our study underscores the value of protein supplementation for the achievement of the currently recommended daily protein intake in the bariatric patient. However, our data does not help to define a protein intake goal as important in determining the body composition and protein status changes following LGBP or LSG. Future studies with a larger sample size, and using more accurate methods of body composition assessment are warranted to better establish this concept.
References
Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Chaston TB, Dixon JB, O’Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes (Lond). 2007;31:743–50.
Westerterp-Plantenga MS, Nieuwenhuizen A, Tomé D, et al. Dietary protein, weight loss, and weight maintenance. Annu Rev Nut. 2009;29:21–41.
Rinaldi Schinkel E, Pettine SM, Adams E, et al. Impact of varying levels of protein intake on protein status indicators after gastric bypass in patients with multiple complications requiring nutritional support. Obes Surg. 2006;16(1):24–30.
American Association of Clinical Endocrinologists. The obesity society and American Society for Metabolic and Bariatric Surgery Medical Guidelines for Clinical Practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Obesity. 2009;17 Suppl 1:S1–69.
Tsai AG, Wadden TA. The evolution of very low-calorie diets: an update and meta-analysis. Obesity. 2006;14:1283–93.
Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13:23–8.
Bock MA. Roux-en-Y gastric bypass: the dietitian’s and patient’s perspectives. Nutr Clin Pract. 2003;18:141–4.
Vidal J, Ibarzabal A, Romero F, et al. Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects. Obes Surg. 2008;18:1077–82.
Ingenbleek Y, Young VR. Significance of transthyretin in protein metabolism. Clin Chem Lab Med. 2002;40:1281–91.
Bavaresco M, Paganini S, Lima TP, et al. Nutritional course of patients submitted to bariatric surgery. Obes Surg. 2008;20(6):716–21.
Brolin RE, Leung M. Survey of vitamin and mineral supplementation alter gastric bypass and biliopancreatic diversión for morbid obesity. Obes Surg. 1999;5:150–4.
Das SK, Roberts SB, McCrory MA, et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr. 2003;78:22–30.
Mettler S, Mitchell N, Tipton KD. Increased protein intake reduces lean body mass loss during weight loss in athletes. Med Sci Sports Exerc. 2010;42(2):326–37.
Brehm BJ, D’Alessio DA. Benefits of high-protein weight loss diets: enough evidence for practice? Curr Opin Endocrinol Diabetes Obes. 2008;15:416–21.
Olbers T, Björkman S, Lindroos A, et al. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244:715–22.
Poitou Bernert C, Ciangura C, Coupaye M, et al. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33:13–24.
Ritz P, Becouarn G, Douay O, et al. Gastric bypass is not associated with protein malnutrition in morbidly obese patients. Obes Surg. 2009;19:840–4.
Coupaye M, Puchaux K, Bogard C, et al. Nutritional consequences of adjustable gastric banding and gastric bypass: a 1-year prospective study. Obes Surg. 2009;19(1):56–65.
Deitel M, Crosby RD, Gagner M. The First International Consensus Summit for sleeve gastrectomy (SG), New York City, October 25–27, 2007. Obes Surg. 2008;18:487–96.
Savastano S, Belfiore A, Di Somma C, et al. Validity of bioelectrical impedance analysis to estimate body composition changes after bariatric surgery in premenopausal morbidly women. Obes Surg. 2010;20(3):332–9.
Janssen I, Ross R. Effects of sex on the change in visceral, subcutaneous adipose tissue and skeletal muscle in response to weight loss. Int J Obes Relat Metab Disord. 1999;23:1035–46.
Rice B, Janssen I, Hudson R, et al. Effects of aerobic or resistance exercise and/or diet on glucose tolerance and plasma insulin levels in obese men. Diab Care. 1999;22:684–91.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial Support
This work was supported by a grant from the FIS of the Instituto de Salud Carlos III, PI 157/06 Madrid, Spain.
Rights and permissions
About this article
Cite this article
Andreu, A., Moizé, V., Rodríguez, L. et al. Protein Intake, Body Composition, and Protein Status Following Bariatric Surgery. OBES SURG 20, 1509–1515 (2010). https://doi.org/10.1007/s11695-010-0268-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0268-y