Abstract
Background
Obesity can negatively affect pulmonary function tests, with or without clinical symptoms, but the impact of bariatric weight loss is still debated. Aiming to document such profile in a consecutive homogeneous population, a prospective cohort study was undertaken.
Methods
Sixty-one patients (100% females, age 40 ± 8 years, BMI 49 ± 5 kg/m2 and without respiratory disease) were enrolled. Spirometric analysis was carried out to compare preoperative respiratory pattern with outcome after 6 and 12 months. Variables included vital capacity (VC), expiratory reserve volume (ERV), forced expiratory volume (1 s) (FEV1), FEV1/FVC ratio and maximum voluntary ventilation (MVV). Correlation of results with weight loss was examined.
Results
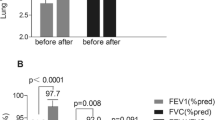
The following initial variables exhibited significant difference when compared to the 12-month postoperative control: FVC (P = 0.0308), FEV1/FVC (P = 0.1998), MVV (P = 0.0004) and ERV (P = 0.2124). Recovery of FVC and FEV1/FVC occurred earlier by 6 months. The most seriously depressed preoperative finding was ERV, which even after 1 year still remained inadequate.
Conclusions
(1) Pulmonary limitations were diagnosed in approximately one third of the population. (2) Changes were demonstrated for FVC, FEV1/FVC, ERV and MVV. (3) FEV1 and FEV1/FVC were acceptable due to the absence of an obstructive pattern. (4) Two variables increased by 6 months (FEV1/FVC and ERV), whereas recovery for others was confirmed after 1 year. (5) The only exception was ERV which continued below the acceptable range.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive body weight interferes with pulmonary static and dynamic properties, depending on degree of obesity, age, type of body fat distribution and other factors. Exaggerated thoracic and abdominal adiposity typically conducts to shallow, rapid and energy-wasting respiratory movements. For many years, heightened demand for ventilation, elevated work of breathing, respiratory muscle inefficiency and diminished respiratory compliance have all been associated with severe obesity. Other possible problem involves respiratory drive, breathing control, gas exchange and airflow obstruction. As a consequence, diminished exercise capacity and even severe dyspnea have been registered in this population [1–3].
All these troubles notwithstanding, conventional tests do not often unveil changes in asymptomatic morbidly obese subjects, and spirometry can be entirely normal in active and comparatively young adults that comprise the bulk of bariatric populations [1–3]. It has been well-established that severe obesity may alter spirometric values; however, these change very considerably in these individuals [4].
Should specific problems be confirmed, it is expected that post-operative weight loss will correct such abnormalities. Indeed a handful of studies have documented the impact of anti-obesity procedures on pulmonary function tests (PFT), and although noteworthy improvements are reported after weight loss, populations, profiles and endpoints tend to be heterogeneous, rendering it difficult to highlight the actual benefits [4, 5].
A prospective study was designed, aiming to compare the spirometric pattern of obese candidates before and after Roux-en-Y gastric bypass (RYGB).
Methods
Population
A consecutive group of bariatric candidates (n = 61, 100% female, age 40 ± 8 years, BMI 49 ± 5 kg/m2) was prospectively submitted to clinical and spirometric investigation.
Criteria of Inclusion
Males or females 18–65 years old, BMI > 40 or >35 kg/m2 with comorbidities, informed consent.
Criteria of Exclusion
Alcohol or drug addiction, asthma, chronic obstructive lung disease, hypoventilation syndrome, use of steroidal agents, bronchodilators, or ventilatory assistance/CPAP, reoperation or takedown of the bariatric procedure, fever or infectious foci in the last 30 days, hospitalization for any reason in the last 30 days and refusal to participate in the protocol.
Experimental Design
Subjects were seen preoperatively after 6 months and after 12 months. All underwent RYGB by the open technique. The same tests were conducted on these occasions by a single investigator.
Clinical Variables
Anthropometry (weight, height, BMI) and a questionnaire addressing smoking habits, respiratory symptoms and diseases, as well as inclusion and exclusion criteria were part of the protocol. Therapeutic prescriptions and medical records were examined to confirm suspected dysfunctions.
Lifestyle and Physical Activities
All bariatric subjects were routinely encouraged to lead an active life, employ a high-protein, low-calorie diet matched to energy expenditure and avoid sedentarism. Targeted alimentation or exercise protocols were not in use during this investigation.
Pulmonary Function Tests
Spirometry was carried out by an experienced physiotherapist using the Pony Spirometer Graphics—Cosmed (Rome, Italy). Predicted values were calculated according to Crapo et al. [4] and the reference value by Hankinson [6].
A minimum of three acceptable respiratory manoeuvres was recorded for each participant, but if the patient did not become tired, five tests were performed and the mean was calculated. ERV, FEV1, FVC, MVV and FEV1/FVC were selected for analysis.
To measure MVV, the subject should be tested in the sitting position wearing a nose clip. After the subject makes an airtight seal around the mouthpiece, at least three resting tidal breaths should be obtained, followed by breathing as rapidly and deeply as possible. The tongue and teeth must be positioned so as to not obstruct airflow. The technician should enthusiastically coach the subject throughout the manoeuvre and may need to suggest faster or slower breathing to achieve an ideal rate of 90–110 breaths/min, although subjects with disease may not always achieve this rate. The technician will need to carefully observe the subject with occasional glances at the tracing to help the subject to obtain an acceptable manoeuvre. An acceptable manoeuvre should be performed with maximal effort without evidence of leakage, hesitation or measurement artefact. The subject is instructed to breathe as deeply and rapidly as possible and the tidal volume (VT) during the manoeuvre should be greater than the subject’s resting VT.
Ethical Considerations
All patients gave written informed consent, and the study was approved by the institutional Internal Review Board.
Statistical Analysis
Values are presented as percentage or mean ± SD. Differences were investigated by analysis of variance followed by post hoc Bonferroni test. By means of linear regression analysis, associations between spirometric variables and BMI were scrutinized. For all statistical procedures by SAS (SAS Institute INC. Cary, NC, USA 1999–2001), version 8.2 was employed, and a P value of less than 0.05 was considered significant.
Results
There were no exclusions in this study, and all subjects tolerated the spirometric procedures and completed the protocol. No subject reported chronic obstructive lung disease or required any modality of pulmonary pharmacologic treatment or ventilatory support. A single patient reported a history of mild asthma in the past but was currently asymptomatic. Table 1 describes the general findings in the bariatric candidates.
All PFT tended to respond to bariatric weight loss, and confirmed results after 12 months were established for FVC (P = 0.020) and MVV (P = 0.003) (Table 2). FEV1/FVC and ERV increased earlier by 6 months. FEV1 and FEV1/FVC were initially normal, as no patient in this series suffered from an obstructive dysfunction. Recovery of ERV was incomplete even 1 year later, as results remained at approximately 60% of the predicted number.
A negative correlation between FVC and BMI (P < 0.03; Fig. 1) and between ERV and BMI (P = 0.03; Fig. 2) was demonstrated, as expected. There was a trend toward correlation between MVV and BMI as well (P = 0.088).
Discussion
The functional profile of early bariatric weight loss and its implications for pulmonary tests is only partially understood. It is admitted that visceral fat is gained and lost faster than somatic adiposity. In this sense, waist circumference should diminish first, with potential benefit for such variables as FVC and FEV1, which depend on efficient motility of respiratory muscles, and particularly of diaphragm excursions, in face of a heavy and voluminous upper abdomen. The waist circumference seems to reduce 50% more than hip circumference in the same time frame [7]. A difference at 6 months was indeed noticed for FVC, but improvement of most variables took 1 year to materialize.
In 1998, a study on the effects of body mass composition and fat distribution on respiratory function reported that the correlation between FVC and waist circumference was negative in males and positive in females. Although we found similar correlations in the present study, none reached the level of statistical significance [8]. Pulmonary function abnormalities are well reported complications of obesity; the most frequently reported abnormalities are reductions in lung volumes and expiratory flow rates [7–9].
Rasslan et al. [10] showed in their study that obese females presented significantly lower FVC and FEV1 values than non-obese females did, and the pulmonary function is altered in women suffering from class I or II obesity. In obese men, although pulmonary function is unaffected by BMI, we observed a significant negative correlation between BMI and ERV. However, ERV values were significantly lower in obese males and females when compared to those values obtained from non-obese males and females.
Bottai et al. [2] showed that over an 8-year follow-up, the detrimental effect of gaining weight might be reversible for many adults as most of those who reduced their body mass index values also increased their lung function. Overweight patients with ventilatory impairment should be routinely encouraged to lose weight for improving their lung function.
Airflow limitation, mirrored among other tests by FVC/FEV1 ratio, is more typical of extreme obesity. It was not a problem in this series (neither preoperatively nor on subsequent assessment). Low expiratory reserve value (ERV) is deemed the most common and representative derangement in all types of obesity and one that consistently improves after weight loss. Indeed, high statistical significance was achieved for this test; however, full recovery failed to materialize.
In a recent study in mildly obese females (BMI 30.0 ± 3.5 kg/m2) submitted to a regimen of diet plus exercise during 16 months, thoracic gas volume measured by air-displacement plethysmography markedly increased. Negative correlation with waist circumference was demonstrated, indeed suggesting participation of intra-abdominal fat accumulation in this phenomenon, and thus an early improvement. However, linear regression analysis was consistent with a role for total body fat as well. It is worth mentioning that although thoracic gas volume was assessed by a different procedure than ERV, it could partially explain the incomplete rehabilitation of ERV in this series [11]. Of course visceral and somatic fat are just some of the possible determinants of static and dynamic pulmonary measurements that are affected by post-bariatric body reshaping and rehabilitation [8].
One should not overlook such potential confounders as sedentarism, thoracic muscle mass and inspiratory muscle performance, closure of peripheral lung units, gas exchange efficiency, abnormalities of ventilation to perfusion ratio and respiratory drive; all of which may be influenced by bariatric interventions [8].
Some of our findings conflict with those of other studies. Marti-Valeri et al. [9] documented more severely diminished FVC, FEV1 and FVC/FEV1 ratio preoperatively. One year after RYGB, FVC and FEV1 had normalized but FEV1/FVC ratio continued somewhat aberrant.
In the experience of Zavorsky et al. [12], preoperative FVC was similar to that of our patients, but FEV1 and FEV1/FRC ratio were lower. In the follow-up, assessment values returned to normal.
Catheline et al. [13] investigated 77 subjects preoperatively only and also found more problems than in this series. FEV1/FVC ratio was more decreased and not less than 17% of the population was diagnosed with an obstructive syndrome, besides 6% with restrictive results.
These discrepancies could probably be attributed to less stringent exclusion criteria resulting in the acceptance of more smokers or patients with more severe respiratory dysfunctions. Collet et al. [14] highlighted that patients with mild or inconspicuous dyspnea displayed acceptable spirometric results, in contrast to those with more severe breathlessness where a markedly hindered pattern prevailed.
Our results are virtually coincident with those of Jones et al. [15], which examined comparatively healthy groups with different ranges of BMI up to severe obesity.
One of the aims of this protocol was to correlate BMI with such respiratory static and dynamic volumes. Although significance was achieved, the correlation indices were rather modest. In fact, it is not questioned that obesity interferes with pulmonary performance and elegantly documented in the alluded to sequential study of Jones et al. [15].
However, deterioration is not linear and a relatively wide scatter of results can be observed for each body mass interval, consistent with the heterogeneity of obese populations. Furthermore, it has been emphasized that most of the loss in spirometric variables tends to occur as BMI increases from 20 to 40 kg/m2, not above 40 kg/m2.
Conclusions
(1) Pulmonary limitations were diagnosed in approximately one third of the population. (2) Changes were demonstrated for FVC, FEV1/FVC, ERV and MVV. (3) FEV1 and FEV1/FVC were acceptable due to the absence of an obstructive pattern. (4) Two variables increased by 6 months (FEV1/FVC and ERV), whereas recovery for others was confirmed after 1 year. (5) The only exception was ERV which continued below the acceptable range.
References
Biring MS, Lewis MI, Liu JT, et al. Pulmonary physiologic changes of morbid obesity. Am J Med Sci. 1999;318:293–7.
Bottai M, Pistelli F, Di Pede F, et al. Longitudinal changes of body mass index, spirometry and diffusion in a general population. Eur Respir J. 2002;20:665–73.
Chen Y, Rennie D, Cormier YF, et al. Waist circumference is associated with pulmonary function in normal-weight, overweight, and obese subjects. Am J Clin Nutr. 2007;85:35–9.
Crapo RO, Kelly TM, Elliott CG, et al. Spirometry as a preoperative screening test in morbidly obese patients. Surgery. 1986;99:763–8.
Hakala K, Maasilta P, Sovijarvi AR. Upright body position and weight loss improve respiratory mechanics and daytime oxygenation in obese patients with obstructive sleep apnoea. Clin Physiol. 2000;20:50–5.
Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87.
Collins LC, Hoberty PD, Walker JF, et al. The effect of body fat distribution on pulmonary function tests. Chest. 1995;107:1298–302.
Lazarus R, Sparrow D, Weiss ST. Effects of obesity and fat distribution on ventilatory function: the normative aging study. Chest. 1997;111:891–8.
Koenig SM. Pulmonary complications of obesity: a review. Am J Med Sci. 2001;321:249–79.
Rasslan Z, Saad Junior R, Stirbulov R, et al. Evaluation of pulmonary function in class and II obesity I. Bras Pneumol. 2004;30:508–14.
Hansen JE, Sun XG, Wasserman K. Spirometric criteria for airway obstruction: use percentage of FEV1/FVC ratio below the fifth percentile, not <70%. Chest. 2007;131:349–55.
Zavorsky GS, Kim DJ, Sylvestre JL, et al. Alveolar-membrane diffusing capacity improves in the morbidly obese after bariatric surgery. Obes Surg. 2008;18:256–63.
Catheline JM, Bihan H, le Quang T, et al. Preoperative cardiac and pulmonary assessment in bariatric surgery. Obes Surg. 2008;18:271–7.
Collet F, Mallart A, Bervar JF, et al. Physiologic correlates of dyspnea in patients with morbid obesity. Int J Obes (Lond). 2007;31:700–6.
Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest. 2006;130:827–33.
Acknowledgement
This study was supported by a post-doctorate FAPESP grant number 06/51197-5. The valuable help of Prof. Antonio C. Valezi is appreciated.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Souza, S.A.F., Faintuch, J. & Cecconello, I. Spirometric Function Improves in the Morbidly Obese After 1-Year Post-surgery. OBES SURG 20, 1273–1277 (2010). https://doi.org/10.1007/s11695-010-0142-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-010-0142-y