Abstract
Background
Obesity has proven to be associated with respiratory symptoms and impaired pulmonary function, which could increase the incidence of postoperative complications after bariatric surgery. However, the component of obesity that has the most influence on pulmonary function has not been identified, especially in Asian-Pacific populations.
Methods
This cross-sectional study enrolled obese Chinese patients ≥18 years of age with a body mass index (BMI) >32 kg/m2, who were being evaluated for bariatric surgery. All patients performed pulmonary function test, and the results were analyzed according to various anthropometric measurements. Multiple-regression analyses were also conducted and adjusted for age, sex, and smoking history to determine the factors that impaired the pulmonary function of the obese patients.
Results
A total of 150 consecutive patients were enrolled from July 2007 to August 2008. We found that body weight, BMI, waist circumference (WC), hip circumference, and waist-to-height ratio but not waist-to-hip ratio had a significant correlation with decreased forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), total lung capacity (TLC), vital capacity (VC), and increased diffusing capacity of the lung for carbon monoxide to alveolar gas volume. After multiple linear regression analysis, only WC was associated with reductions in FEV1, FVC, TLC, and VC.
Conclusions
Obesity is associated with a restrictive pattern of impaired pulmonary function in various anthropometric parameters measured in obese Chinese adults in Taiwan. Among these parameters, WC had the greatest impact on pulmonary function, which could also implicate the rate of postoperative complication and the need of more intensive care after bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity poses a major public health challenge in the developed countries throughout the world, with consequences such as metabolic disorders, cardiovascular diseases, diabetes, rheumatoid arthritis, and cancer [1]. There is also increasing evidence demonstrating the profound adverse effects of obesity on the respiratory system, including obstructive sleep apnea, obesity hypoventilation syndrome, and obstructive airway disease [2–4]. Tai and Chang et al. had assessed and confirmed a significantly higher prevalence of gastroesophageal reflux disease (GERD) and a poorer health-related quality of life (HRQL) in morbidly obese Chinese patients before bariatric surgery [5–7]. Previous studies showed impaired pulmonary function could lead to increased postoperative complications and intensive care unit (ICU) admission after bariatric surgery [8, 9]. Body weight (BW) and body mass index (BMI) can be easily measured and, therefore, are frequently used in epidemiologic studies. However, these measures are limited in that they do not distinguish between fat mass and muscle mass, which have opposite effects on pulmonary function [10, 11]. There is increasing evidence that abdominal obesity, often referred to as a larger waist circumference (WC) or waist-to-hip ratio (WHR), is associated with a higher risk of diabetes, hypertension, cardiovascular disease, and cancer, as well as all-cause mortality [12–15]. Waist-to-height ratio (WHtR) is also associated with metabolic risks and cardiovascular disease [16, 17]. The negative effects of abdominal obesity (WC, WHtR, or WHR) were even more profound than those of BMI. More and more studies have also evaluated the relationship of WC and WHR with respiratory function [18, 19]. In addition to WC, hip circumference (HC) had the opposite association with metabolic syndrome and all-cause mortality [20, 21]. However, data on the relationship between the different fat distributions found in obesity and respiratory function in the Asian-Pacific population are sparse, and which component of obesity is the most important determinant of pulmonary function is not known.
The aims of our study are (1) to determine the prevalence of pulmonary function abnormality in obese Chinese patients before bariatric surgery and (2) to clarify the relationship between the various anthropometric measurements of obesity, including BW, BMI, WC, HC, WHtR, and WHR, to the impairment of pulmonary function.
Materials and Methods
Study Population
Patients ≥18 years of age who had a BMI >37 kg/m2 or a BMI between 32 and 37 kg/m2 with obesity-related comorbidities who were being evaluated for bariatric surgery from July 2007 to August 2008 were enrolled from the obesity center of E-Da hospital in Southern Taiwan. These inclusion criteria were based on a modification of the recommendations of the Asia-Pacific consensus [22]. All patients underwent a psychiatric interview before surgery to identify any mental illnesses or unrealistic expectations for the surgical treatment. Patients were excluded if they had one of the following conditions: a history of chronic lung disease, obstructive lung disease, pregnancy, endocrinopathy-induced obesity, or malignancy. Informed written consent was obtained before the study and the laparoscopic bariatric surgery. The study protocol was approved by the Human Ethics Committees of this institution.
BW and height were measured after overnight fasting. BMI was calculated on the basis of these measurements. A D-loop nonstretch fiberglass tape was used for the circumference measurements. WC was measured around the abdomen on the midpoint between the lower border of the rib cage and the iliac crest, while the participant was standing with the abdomen relaxed, both feet touching, and arms hanging freely at the end of a normal expiration. Where there was no natural waistline, the measurement was taken at the level of the umbilicus [23]. HC was measured at the maximum circumference between the iliac crest and the crotch while the participant was standing and was recorded in the same position. WHtR and waist-to-hip ratio were defined as WC/body height and WC/HC, respectively. All the obese patients received pulmonary function test (PFT) before the bariatric surgery. Clinical and demographic data were recorded.
Pulmonary Function Testing
PFT was performed with the patient in a sitting position, with nose clips in place, using a body plethysmography (Vmax 229, SensorMedics, Yorba Linda, CA, USA) and was carried out by the same team of technicians according to the American Thoracic Society/European Respiratory Society statement [24]. Each participant performed at least three tests (with at least two reproducible and acceptable maneuvers). The measurements included forced vital capacity (FVC), forced expiratory volume in 1 s (FEV1), vital capacity (VC), expiratory reserve volume (ERV), residual volume (RV), and total lung capacity (TLC). Results were considered reproducible if the second highest FEV1 and FVC values were within 5% of the highest values. The highest measured FEV1 and the corresponding measured value of FVC were coded for computer analysis. Diffusing capacity of the lung for carbon monoxide (DLCO) was measured with the single breath technique, and the values obtained were corrected for hemoglobin concentration. The results of these tests were expressed as percentage of the predicted normal values.
Statistical Analysis
For continuous parameters, data were presented as mean ± SD, and categorical parameters were presented as number and percentage. Pearson’s correlation coefficients were calculated to describe the relationship between the various anthropometric measurements of obesity and the parameters of PFT. Multiple-regression analyses were conducted to clarify the determinants for the impairment of pulmonary function. We used various parameters of PFT as the dependent variables, while the age, sex, smoking history, BW, BMI, WC, HC, WHtR, and WHR were included as the independent determinant variables. A forward stepwise strategy was applied to select significant independent variables, with P < 0.05 as the inclusion criterion. All analyses were performed using the commercial statistical software SPSS, version 9.
Results
Baseline Characteristics
Of the 162 consecutive obese Chinese patients from July 2007 to August 2008, 150 patients were enrolled, and 12 were excluded because of intolerance or inadequate performance of PFT. The demographic and various anthropometric parameters, including age, height, weight, BMI, WC, HC, WHtR, and WHR, are shown in Table 1. Baseline spirometric measurements are summarized in Table 2. Females were predominant in this study (59%), and the age range was 18–59 (32.5 ± 9.8) years. The average value of the PFT results of these patients was within normal limits (over 80% of the predicted normal values), except for mildly lower ERV with an average of 75.0 (range 21–117) and increased DLCO/VA with an average of 105.4 (range 88–141). A history of smoking, including those who had ever smoked (former and current), was noted in 28% of this study population.
The Relationship Between Anthropometric Parameters and Pulmonary Function Test
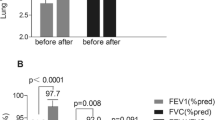
Pearson’s correlation coefficients were calculated to describe the relationship between various anthropometric parameters and the results of PFT. As shown in Table 3, BW, BMI, WC, HC, and WHtR, but not WHR, all had a significant negative correlation to FVC, FEV1, TLC, VC, and a positive correlation to DLCO and to alveolar gas volume (DLCO/VA). We found that WC had a more significant relationship with FEV1 (r = −0.252, P = 0.002) and FVC (r = −0.266, P = 0.001; Fig. 1). In addition, BMI, WC, and WHtR were negatively correlated with ERV. However, the WHR had no significant correlation with the parameters of PFT in this study. None of the anthropometric parameters of obesity had significant correlation with the value of FEV1/FVC.
Multiple Linear Regression Analysis of Anthropometric Parameters and PFT
Upon multiple linear regression analysis, after adjusting for the potential confounding factors age, sex, and smoking history, as summarized in Table 4, WC was shown to be a negative determinant for FEV1, FVC, TLC, and VC. Only HC was a positive determinant for DLCO/VA.
Discussion
This is the first study to address the relationship between the different methods of measuring obesity and respiratory function in an Asian-Pacific population. The major finding of this study was that BW, BMI, WC, HC, and WHtR, but not WHR, were all negatively correlated with FEV1, FVC, TLC, and VC and positively correlated with DLCO/VA. After adjustment for the potential confounding factors, including age, sex, and smoking history, only WC had a negative effect on FEV1, FVC, TLC, and VC. These results indicated that all the anthropometric parameters of obesity, except for WHR, were associated with a restrictive pattern of impaired pulmonary function.
Obesity can profoundly alter pulmonary function and diminish exercise capacity by its adverse effects on respiratory mechanics, resistance within the respiratory system, respiratory muscle function, lung volume, work and energy cost of breathing, control of breathing, and gas exchange. BMI is the most popular and practical tool for the evaluation of obesity and is frequently used in large-scale epidemiologic studies. However, an increasing number of studies have evaluated the relationships of WC and WHR with pulmonary function and suggested that abdominal fat deposition was a somewhat better predictor of pulmonary function than BMI [19, 25]. Two previous studies in Canada and UK found that WC was significantly associated with decreased FVC and FEV1, but not with FEV1/FVC [19, 26], which was consistent with the present study. Similarly, an epidemiologic study previously conducted in Taiwan also showed that BMI had only a slight effect on respiratory function [27]. However, another study in the UK found that WHR was negatively correlated with FVC and FEV1 [28], which was not found in our study. Gonzalez et al. reported that FEV1 <80% was independently associated with an increased likelihood of complicated postoperative management and ICU admission after bypass surgery for morbid obesity, which implied that the patients with a larger WC might need more intensive care after the bariatric surgery [8].
In obese patients, the prevalence of respiratory symptoms, especially dyspnea, may increase with increasing BMI [29]. The sensation of dyspnea can be partially explained by the increased ventilatory drive and reduced static lung volume [30, 31]. The work of breathing may be markedly increased [32]. VC as well as IC can be low, reflecting decreased performance of the inspiratory muscles [30]. The lung, thoracic cage, and the abdominal cavity comprise a closed system with the diaphragm as the connecting interface. When there is an increase in the abdominal and diaphragmatic pressure, the pleural pressure may be altered and a decrease in total lung capacity, pulmonary compliance, and pulmonary volume may follow [33]. Frezza et al. demonstrated that increases in BMI are associated with increases in intra-abdominal pressure [34]. However, Lambert et al. showed that the intra-abdominal pressure correlated to the sagittal abdominal diameter, an index of the degree of central obesity, but not BW or BMI [35]. Many studies have shown that obesity can lead to restrictive pulmonary function impairment, including reduced FEV1, FVC, ERV, and TLC [2, 30, 36]. This impaired pulmonary function may result from the increased abdominal load that alters the chest wall mechanics; thus, it is reasonable to suppose that abdominal obesity is more predictive than BMI. This hypothesis was supported by a previous study conducted by Hamoui et al., which showed that reduced VC was the strongest predictor of postoperative complications, reflecting increased intra-abdominal pressure and diminished chest wall compliance [9]. Our present study showed that VC was negatively correlated with BW, BMI, WC, HC, and WHtR. However, only WC had a negative effect on VC after adjustment for the confounding factors. Again, the result implies that an increased WC might increase the rate of postoperative complications.
A previous study conducted by Vishal Sekhri et al. emphasized the potential role of age and sex in the impact of obesity on pulmonary function [37]. In that study, subjects over 40 years of age had significantly lower FVC and FEV1/FVC than those aged below 40 years. Male sex also had greater impact on the FVC, FEV1, FEV1/FVC, TLC, and ERV. These results may be explained by the observation that abdominal obesity tends to increase with age. Furthermore, previous studies [38–40] have described a predominantly upper body or central (abdominal) pattern of obesity in men. In contrast, women had a predominantly lower body or peripheral (gluteal) pattern of fat distribution. The different body fat distributions between men and women may explain the different effects on pulmonary function, in which abdominal obesity leads to a greater compression of the thoracic cage by the excessive tissue. In the present study, when we adjusted for the potential confounders of age, sex, and smoking history, only WC was correlated with pulmonary function, especially with FEV1 and FVC.
There is heterogeneity in the effects of obesity on the change in DLCO, and the exact pathophysiologic mechanism is unclear. Most studies [36, 41], but not all [37], have demonstrated an increased DLCO in obese patients, and some even have a reduced DLCO [42]. Obese patients without clinically apparent heart disease may have a high-output state and elevated total and central blood volumes, which will increase the capillary blood volume and thereby result in elevated DLCO. However, reduced DLCO can also be found in obese individuals, which may reflect a structural change in the interstitium of the lung, resulting from lipid deposition, cellular hyperplasia, alveolar enlargement, and decreased alveolar surface area [30]. In this study, DLCO decreased as BMI, HC, and WHtR increased. In contrast, DLCO/VA significantly increased with BW, BMI, WC, HC, and WHtR, but not WHR, which is probably because of a decreased alveolar area in these obese patients. After adjustment for the confounding factors, however, only HC was positively correlated with DLCO/VA.
There are some limitations of this study. First, the analyses of the study were based on cross-sectional data and were limited to those individuals who came for evaluation for bariatric surgery. Longitudinal follow-up may be needed to clarify the potential for reversal of these effects after weight reduction. Selection bias may have existed, although we adjusted for some potential confounders. Also, we simplified smoking status (never, former, or current) and pack-years smoked as a single confounding factor.
In conclusion, the results of this study suggested that that all the anthropometric parameters of obesity measured in obese Chinese adults in Taiwan, except for WHR, were associated with a restrictive pattern of impaired pulmonary function. Among these parameters, WC had the greatest impact on pulmonary function, which could also implicate the rate of postoperative complication and the need of more intensive care after bariatric surgery.
Abbreviations
- ATS:
-
American Thoracic Society
- BMI:
-
Body mass index
- BW:
-
Body weight
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- DLCO/VA:
-
DLCO to alveolar gas volume
- ERV:
-
Expiratory reserve volume
- FEV1:
-
Forced expiratory volume in the first second
- FVC:
-
Forced vital capacity
- HC:
-
Hip circumference
- IC:
-
Inspiratory capacity
- PFT:
-
Pulmonary function test
- RV:
-
Residual volume
- TLC:
-
Total lung capacity
- VC:
-
Vital capacity
- WC:
-
Waist circumference
- WHR:
-
Waist-to-hip ratio
- WHtR:
-
Waist-to-height ratio
References
Conway B, Rene A. Obesity as a disease: no lightweight matter. Obes Rev. 2004;5:145–51.
Ray CS, Sue DY, Bray G, et al. Effects of obesity on respiratory function. Am Rev Respir Dis. 1983;128:501–6.
Guerra S, Sherrill DL, Bobadilla A, et al. The relation of body mass index to asthma, chronic bronchitis, and emphysema. Chest. 2002;122:1256–63.
Shore SA. Obesity and asthma: possible mechanisms. J Allergy Clin Immunol. 2008;121:1087–93. quiz 1094–95.
Chang CY, Huang CK, Chang YY, et al. Cross-validation of the Taiwan version of the Moorehead-Ardelt quality of life questionnaire II with WHOQOL and SF-36. Obes Surg 2009; in press
Tai CM, Lee YC, Wu MS, et al. The effect of Roux-en-Y gastric bypass on gastroesophageal reflux disease in morbidly obese Chinese patients. Obes Surg. 2008;19:565–570.
Chang CY, Huang CK, Chang YY, et al. Health-related quality of life in adult patients with morbid obesity coming for bariatric surgery. Obes Surg. 2009; in press.
Gonzalez R, Bowers SP, Venkatesh KR, et al. Preoperative factors predictive of complicated postoperative management after Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2003;17:1900–4.
Hamoui N, Anthone G, Crookes PF. The value of pulmonary function testing prior to bariatric surgery. Obes Surg. 2006;16:1570–3.
Wise RA, Enright PL, Connett JE, et al. Effect of weight gain on pulmonary function after smoking cessation in the Lung Health Study. Am J Respir Crit Care Med. 1998;157:866–72.
Santana H, Zoico E, Turcato E, et al. Relation between body composition, fat distribution, and lung function in elderly men. Am J Clin Nutr. 2001;73:827–31.
Folsom AR, Kushi LH, Anderson KE, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women’s Health Study. Arch Intern Med. 2000;160:2117–28.
Zhang C, Rexrode KM, van Dam RM, et al. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658–67.
Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167:1465–75.
Price GM, Uauy R, Breeze E, et al. Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death. Am J Clin Nutr. 2006;84:449–60.
Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27:610–6.
Lin WY, Lee LT, Chen CY, et al. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002;26:1232–8.
Wannamethee SG, Shaper AG, Whincup PH. Body fat distribution, body composition, and respiratory function in elderly men. Am J Clin Nutr. 2005;82:996–1003.
Chen Y, Rennie D, Cormier YF, et al. Waist circumference is associated with pulmonary function in normal-weight, overweight, and obese subjects. Am J Clin Nutr. 2007;85:35–9.
Snijder MB, Zimmet PZ, Visser M, et al. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: the AusDiab Study. Int J Obes Relat Metab Disord. 2004;28:402–9.
Bigaard J, Frederiksen K, Tjonneland A, et al. Waist and hip circumferences and all-cause mortality: usefulness of the waist-to-hip ratio? Int J Obes Relat Metab Disord. 2004;28:741–7.
Lee WJ, Wang W. Bariatric surgery: Asia-Pacific perspective. Obes Surg. 2005;15:751–7.
WHO. Obesity: preventing and managing the global epidemic Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253.
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Ochs-Balcom HM, Grant BJ, Muti P, et al. Pulmonary function and abdominal adiposity in the general population. Chest. 2006;129:853–62.
Chen R, Tunstall-Pedoe H, Bolton-Smith C, et al. Association of dietary antioxidants and waist circumference with pulmonary function and airway obstruction. Am J Epidemiol. 2001;153:157–63.
Tsai WL, Yang CY, Lin SF, et al. Impact of obesity on medical problems and quality of life in Taiwan. Am J Epidemiol. 2004;160:557–65.
Canoy D, Luben R, Welch A, et al. Abdominal obesity and respiratory function in men and women in the EPIC-Norfolk Study, United Kingdom. Am J Epidemiol. 2004;159:1140–9.
El-Gamal H, Khayat A, Shikora S, et al. Relationship of dyspnea to respiratory drive and pulmonary function tests in obese patients before and after weight loss. Chest. 2005;128:3870–4.
Koenig SM. Pulmonary complications of obesity. Am J Med Sci. 2001;321:249–79.
Collet F, Mallart A, Bervar JF, et al. Physiologic correlates of dyspnea in patients with morbid obesity. Int J Obes (Lond). 2007;31:700–6.
Kress JP, Pohlman AS, Alverdy J, et al. The impact of morbid obesity on oxygen cost of breathing (VO(2RESP)) at rest. Am J Respir Crit Care Med. 1999;160:883–6.
Torquato JA, Lucato JJ, Antunes T, et al. Interaction between intra-abdominal pressure and positive-end expiratory pressure. Clinics (Sao Paulo). 2009;64:105–12.
Frezza EE, Shebani KO, Robertson J, et al. Morbid obesity causes chronic increase of intra-abdominal pressure. Dig Dis Sci. 2007;52:1038–41.
Lambert DM, Marceau S, Forse RA. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005;15:1225–32.
Jones RL, Nzekwu MM. The effects of body mass index on lung volumes. Chest. 2006;130:827–33.
Sekhri V, Abbasi F, Ahn CW, et al. Impact of morbid obesity on pulmonary function. Arch Med Sci. 2008;4:66–70.
Krotkiewski M, Bjorntorp P, Sjostrom L, et al. Impact of obesity on metabolism in men and women. Importance of regional adipose tissue distribution. J Clin Invest. 1983;72:1150–62.
Bouchard C, Despres JP, Mauriege P. Genetic and nongenetic determinants of regional fat distribution. Endocr Rev. 1993;14:72–93.
Harik-Khan RI, Wise RA, Fleg JL. The effect of gender on the relationship between body fat distribution and lung function. J Clin Epidemiol. 2001;54:399–406.
Saydain G, Beck KC, Decker PA, et al. Clinical significance of elevated diffusing capacity. Chest. 2004;125:446–52.
Inselman LS, Padilla-Burgos LB, Teichberg S, et al. Alveolar enlargement in obesity-induced hyperplastic lung growth. J Appl Physiol. 1988;65:2291–6.
Disclosure
None of the contributing authors have any conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, YF., Wu, HD., Chang, CY. et al. The Impact of Various Anthropometric Measurements of Obesity on Pulmonary Function in Candidates for Surgery. OBES SURG 20, 589–594 (2010). https://doi.org/10.1007/s11695-009-9961-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-9961-0