Abstract
Purpose
Underweight (BMI < 18.5) and obese (BMI ≥ 30) patients may not tolerate coronary artery bypass graft (CABG) surgery as well as other patients. High and low body mass indices seem to pose a substantial risk of developing post-operative pulmonary complications in subjects undergoing cardiac surgery. To what extent body mass index (BMI) influences postoperative pulmonary complications has not yet been defined.
Methods
Patients posted for CABG were divided into 4 groups based on the BMI. Before and after the surgery chest physiotherapy was administered; pulmonary function tests (PFT) were performed preoperatively and on the 7th postoperative day. Six-minute Walk test (6MWT) was performed preoperatively and postoperatively on the 5th day. The values were analysed and compared among the groups.
Results
Forced expiratory volume in one second (FEV1), Forced vital capacity (FVC) and Vital Capacity (VC) were significantly lesser in underweight and obese groups (p = 0.001). In 6MWT the maximum reduction in the distance covered was in the underweight group.
Conclusion
The underweight group experienced the greatest reduction in pulmonary function test values and 6MWT values after CABG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary artery bypass graft (CABG) is the most widely used coronary revascularization procedure and is the most commonly performed open heart surgery. With a strong foundation, and advancement in technology now CABG has become a standard treatment for severe coronary artery disease. It is a first option therapy in cases of coronary artery diseases [1]. In India, approximately 60% surgeries are off-pump and some major centres including the present study centre carry out 98% of their cases as off pump coronary artery bypass graft (OPCAB). The midline sternotomy is by far the most common incision used for performing CABG.
Among the complications seen after cardiac surgery, post-operative pulmonary complications (PPCs) have been suggested to be the most common. These pulmonary problems may be caused by effect of general anaesthesia, mechanical changes in the thoracic wall caused by the incision and internal mammary artery harvesting, and postoperative pain and lack of mobility. PPCs negatively affect the course of the postoperative period and may unduly prolong discharge [2, 3].
Chest physiotherapy is often prescribed to patients undergoing cardiac surgery in order to prevent or diminish postoperative complications.
Chest physiotherapy can start as soon as the patient’s condition has stabilised, usually 24 to 48 h after infarct or bypass surgery. Chest physiotherapy is used to clear secretions, prevent collapse of alveoli and prevent pneumonia. It is an integral part of pre-surgical and post-surgical care of cardiac patients, preventing pulmonary complications and facilitating bronchial hygiene and expansion of the lung [4,5,6].
The physical programme given after surgery includes early ambulation, frequent position changes, deep breathing techniques and assisted bronchial hygiene techniques including coughing, mechanical assistive devices like the incentive spirometer and positive expiratory pressure devices (PEP) are also used to help in improving cardiopulmonary status of the patients [7].
Pulmonary function test is a valid and reliable method to measure lung volumes. It is a non-invasive method that can be handled without any inconvenience to the patient especially after surgery [8].
The 6MWT was originally developed to assess the functional exercise capacity of patients with pulmonary and cardiac condition. Later it was learnt to be a valid and reliable tool to assess the extent of functional limitation in a variety of patient populations. The benefits of the 6MWT are its similarity to normal activities of daily living, when compared to bicycle treadmill exercise testing, it’s simplicity to administer, low cost and safety. The simplicity of the test usually makes it well acceptable to patients and easy to administer [9].
The BMI is a simple, safe, non-invasive, and cheap way of estimating body fat percentage and assessing a person’s health and nutritional status. The BMI is one of many anthropometric indices, but it is by far the most popular. Indeed, it is an internationally accepted index for defining obesity. The concept of the BMI dates back to the Belgian statistician Adolphe Quetelet, who in 1832, observed that an individual’s weight is approximately related to the square of their height (kg/m2) [10]. BMI is both highly correlated with adiposity and largely uncorrelated with height.
Obesity was thought to be a risk factor for both developing cardiovascular disease and for bad prognosis after cardiac surgery. It is accepted that the risk factors for cardiovascular disease such as hypercholesterolemia are more prevalent in the obese, but the data available on morbidity and mortality in obese subjects undergoing cardiac surgery is inconclusive. Several researchers have reported no association between obesity and bad prognosis in cardiac surgery [11, 12].
Though the general consensus has been that obesity is a risk factor for complications after cardiac surgery, some recent literature has shown that obesity might actually have a protective effect against postoperative complications and postoperative mortality. In fact, subjects with BMIs up to 36 kg/m2 have been shown to have the least risk of dying within a 30-day period after cardiac surgery. In contrast underweight subjects have the most risk of both mortality and morbidity during the same period [13].
Metabolic abnormalities and general organ function of patients can be related to the BMI of the patient. A low BMI can predict low nutritional status and thereby adverse outcomes in patients. Low BMI in older patients can cause sarcopenia and functional debility by adversely affecting nutritional status. Subjects with low BMI are susceptible to illness, falls and fractures which can require emergency care and hospitalisation [14].
Need for the study
Pulmonary function test values and functional exercise capacity is the most common and reliable outcome measures following coronary artery bypass graft. Even though cardiac rehabilitation is routinely practised, there is a dearth of literature regarding the influence of body mass index on pulmonary function test and 6MWT values in coronary artery bypass graft patients and the importance of chest physiotherapy in Phase I cardiac rehabilitation.
Experimental methodology
Purpose of the study
The influence of BMI on pulmonary complications and functional exercise capacity after CABG as well as the impact of BMI on the effect of chest physiotherapy after CABG is still under research. There is a marked lacuna in the literature studying the relationship between BMI and pulmonary function test and 6MWT values after CABG. Hence, the present study aimed at determining whether and to what extent BMI of the subjects influences the pulmonary function test and 6MWT values after CABG and the response of these values to chest physiotherapy.
We included both males and females posted for CABG, in the age group between 40-70 years, undergoing isolated off- pump CABG and with the ability to understand instuctions and provide informed consent. We excluded the subjects with known respiratory disease, on pump CABG, Bilateral internal mammary artery grafted patients, high risk patients undergoing CABG, those on prolonged ventilatory or BiPAP support and those with congenital and valve problems (Fig. 1).
Participants
The study design was cohort design. Two hundred and forty-six subjects were recruited who were posted for CABG by using purposive sampling; subjects were selected from the population group satisfying the inclusion criteria for the patients of the Department of Cardiothoracic Surgery, from a medical college hospital. The approval of the University ethics committee was obtained. All the subjects were required to sign an informed consent form after being explained the study. Informed consent form was given in the local language to those who required it.
BMI of patients posted for Coronary artery bypass grafting was calculated by the Quetelet Index [10]i.e.,
and divided into 4 groups. Group I BMI < 18.5, Group II BMI 18.5–24.9, Group III BMI 25–30 and Group IV BMI >30.
Prior to the surgery all the patients were seen by a physical therapist who was unaware of the study, who explained the need for physiotherapy after surgery and helped to clear secretions from the lung. Preoperative chest physical therapy (Incentive spirometer, coughing, huffing, chest manipulations, segmental expansion and mobilisation) was given, and the patients were informed what to expect in physical therapy postoperatively.
Postoperatively the chest physiotherapy started 1 hour after extubation. Chest physiotherapy was given twice daily postoperatively and included lung expansion therapy, change of position, breathing exercises and coughing techniques [15]. Day 1 exercises included diaphragmatic breathing exercises, incentive spirometry, re-expansion respiratory exercises, pursed lip breathing, splinted coughing, and huffing, sitting on the edge of the bed and active exercises to all extremities. Day 2 exercises included all the Day 1 exercises, ambulation around the bed, sitting on the back supported chair, spirometry in sitting position, chest percussion and vibration. Day 3 exercises included all the Day 2 exercises, ambulation 60 m, thoracic and shoulder mobilisation in standing position.
Day 4 exercises included all the Day 3 exercises, up and down 5 steps, side flexion, all the limb exercises and trunk exercises. Day 5 exercises included all the Day 4 exercises and ambulation 120 m. Day 6 exercises included all the Day 5 exercises and climbing up and down 15 steps. Day −7 exercises included Day 6 exercises, exercise prescription, explaining the dos and don’ts. All the above mentioned exercises were continued till the discharge. The frequency of the exercises was 2 sessions and duration 20–30 minutes.
Pulmonary function was measured before surgery and seven days after surgery using TrueFlow by ndd (CE0120) Switzerland. The PFT was performed in the morning time one hour after chest physical therapy. Calibration of the equipment was done every day before the measurement was taken. The patient sat on a chair with the nose clipped and the procedure was done according to the method recommended by the European Respiratory Society. The best of three readings, which were taken according to the correct technique, was taken as the final reading. At the outset, the vital capacity (VC) was measured using an inspiratory manoeuvre. After that the forced vital capacity (FVC) and forced FEV1 were measured [16, 17].
Measurements taken using the handheld spirometer have shown good reliability and validity when compared to the gold standard pulmonary function laboratory tests. These measurements also have been shown to be good early indications of pulmonary complications [18].
The 6-min walk test was performed preoperatively and postoperatively 5th day, the test was performed in morning time 1 hour after chest physiotherapy. The subjects were instructed to walk as much as possible over the 50 m marked corridor for six minutes. Subjects were asked to walk back and forth around the blocks kept in the corridor. Measurements of heart rate, blood pressure and rate of perceived exertion were taken at the beginning and the end of the test. No verbal or other encouragement was given during the test. The distance walked in the six minutes was calculated by using lap counter and markings in a corridor in meter with fractions of less than 6 in. rounded to previous unit and more than 6 in. to the next [19, 20].
The 6MWT has been seen to have a high test–retest reliability with an intra-class correlation of 0.90, 0.88, 0.91at baseline, 18 weeks and 43 weeks respectively when studied in a cohort of subjects with heart failure. The content validity of the 6MWT has also been established in subjects with pacemakers and severe heart failure [21, 22].
Results
Using SPSS software (IBM SPSS Version 20), the principal investigator first described the demographic, preoperative and postoperative evaluation data of each group using means and SDs for all variables.
Table 1 shows the demographic data and baseline clinical characteristics of the participants of the study. When the gender of the participants in various groups was compared, number of both males and females in the four groups was found to be significantly different, that is, males and females were not equally distributed in the four groups.
The mean age of the participants when compared between the groups was not significant, indicating that the four groups were age matched. When the mean BMI of the groups were compared there was a significant difference seen. Similarly, a significant difference was seen in the LVEF between the groups. The difference in the member of smokers in the groups was not significant. The difference in number of hypertensive subjects and those with diabetes mellitus was also not significant among the groups.
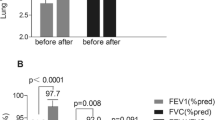
Results of pulmonary function test
Table 2 shows pre and postoperative comparison of FEV1, which shows a highly significant difference in the postoperative values in all the four groups. The underweight group (Group 1) had the most change in the value postoperatively (48.79%) followed by obese group (35.48%).
Table 3 shows the postoperative changes of FEV1 among the groups. The difference between Group 1 and Groups 2 and 3 was significant, but from Group 2 to 3, Group 2 to 4, and from Group 3 to 4 there is no significant difference.
Table 4 shows the preoperative to postoperative changes of FVC; a highly significant change was seen in post operative FVC values when compared to preoperative FVC values in all the groups. Underweight group (Group 1) showed more changes (54.73%) when compared to the other groups.
Table 5 shows the comparison of preoperative to postoperative FVC between groups. There was a significant difference between underweight to normal weight groups and overweight to obese groups. There was no significant difference between the other groups.
Table 6 shows pre- to post- comparison of vital capacity. All groups had a highly significant reduction in vital capacity pre to postoperatively, and maximum changes were seen in underweight group followed by the obese group.
Table 7 shows the comparison of pre- to post- differences of VC between the groups. There was a highly significant difference seen between Group 1 and Group 2, Group 2 and Group 4, and Group 3 and Group 4.
When the FEV1 comparison between groups was done, the difference between underweight to normal weight and underweight to overweight was highly significant (p = 0.001). The difference between underweight to obese was significant (p = .024), but there was no significant difference between the other groups.
On comparison of FVC between groups, the difference was highly significant (p=.001) between under weight to normal weight and underweight to overweight and there was a significant difference between underweight to obese. There was no significant difference between the FVC values of other groups. In the comparison of VC the difference between underweight to normal weight was highly significant (p = 0.000); the difference between normal weight to obese and over weight to obese was also highly significant.
Results of 6-MWT
Table 8 shows that preoperative to postoperatively the changes in distance walked had significantly changed in all the four groups and more changes occurred in the underweight group when compared to the other groups.
Table 9 shows the between group comparison of 6MWT. There was highly significant difference between Group 1 to Group 2, Group 3 and Group 4. When the comparison was done between Group 2 and Group 3 the difference was highly significant; no other groups shows significant difference.
6MWT was performed preoperatively and on 5th postoperative day. Postoperatively the distance covered by the patients significantly reduced in all the four groups, with the underweight group showing the most reduction. When the groups were compared, the difference between the underweight group to normal weight overweight and obese groups were all highly significant (p = 0.000). Normal weight to obese group also there was a highly significant difference.
Discussion
The result of the present study showed decreased lung volumes in the patients with high and low BMI. Obesity was seen to decrease lung volumes after surgery; one of the reasons for decreased expiratory volumes could be the flattening of the diaphragm due to the pressure exerted by excessive abdominal fat, which decreases the total space available for lung expansion.
Chen et al. (2007) [23] found pulmonary function and BMI of overweight and obese subjects to be correlated. The increased intra abdominal pressure affecting diaphragmatic excursion was postulated by them to be the cause for this negative effect of BMI on pulmonary function.
Melo et al. (2014) [24] in their systematic review found that obesity caused reduction in lung volumes and capacities including FEV1 and FVC.
Another possible reason for lung function in obese people getting adversely affected is the deposition of fat tissue over the rib cage, visceral cavity and abdomen, thus affecting the bucket handle and pump handle movements of the chest wall. The excessive load on the chest wall is probably the most important cause for reduced lung volumes. The excessive fat deposits in the abdomen also make downward movement of the diaphragm difficult.
Shah et al. (2012) [25] investigated dynamic lung function in underweight adolescent boys and found that nutritional status plays a major role in dynamic lung function. Diminished lung function is seen at both extremes of body mass (underweight or obese) and remains normal within the normal range of BMI.
Patients in the underweight BMI group experienced the greatest pulmonary complications after CABG in this study. It was seen that those with low BMI were at a higher risk to develop post-surgical complications when compared to those with normal BMI or even those with morbidly high BMIs. Underweight status and micronutrient deficiencies have been seen to cause a decrease in the efficiency of the immune system. This may have affected the lung function of the underweight subjects in the present study thus causing more of pulmonary complications. Diaphragmatic muscle mass, respiratory muscle mass and diaphragmatic excursion have been seen to reduce in underweight populations [26, 27]. Under nourishment reduces diaphragm contractility by reducing diaphragmatic muscle mass. The mass of other respiratory muscles is also seen to be decreased in underweight subjects.
The 6MWT was well tolerated in all patients. The 6MWT is commonly used to measure mobility using functional limitation to predict mobility. It has been shown that the 6MWT can be used as an overall predictor of disability. In the present study, distance walked by the underweight patients were the least, followed by the obese patients. This was true both preoperatively and post-operatively.
Fiorina et al. (2007) [28] stated that the 6-min walk distance which expresses the functional capacity is reduced significantly in a short period after cardiac surgery. They also recorded that it quickly improves after physical training, irrespective of baseline parameters like age, gender, co-morbid conditions and initial functional capacity.
Underweight or low BMI causes a proportionate decrease in muscle mass of the diaphragm as well as the trunk and limb muscles. Fast fibres are affected more by under nutrition than slow fibres, and the atrophied muscle cross- section reveals a greater percentage of slow oxidative fibres. The tension of muscles generated during basal and low intensity activities may be preserved in underweight subjects, but maximal and sub-maximal power output of the muscles may be affected. This could result in poor performance of sub maximal activities like the 6MWT.
Donahoe et al. [29] found an increased consumption of O2 in the ventilatory muscles in underweight patients suffering from chronic obstructive pulmonary disease. This increase in oxygen consumption of the ventilatory pump could be an exercise limiting factor in the underweight subjects by reducing the amount of total oxygen available to the working limb muscles, and thus affecting the performance in the 6MWT.
According to Enright, et al. [30], in overweight people, walking can be affected because the workload is increased for a given amount of exercise, thus causing the 6-min walk distance to be reduced with increased BMI or body weight.
In this study the pulmonary complications followed by CABG was more in the underweight group followed by obese group. It is a well-accepted fact that obesity is a major risk factor for developing diabetes and cardiovascular diseases. But it has also been shown that high BMI can be associated with less chance of mortality and better prognosis in many chronic diseases and health disorders. This strange and unlikely protective effect that obesity has on some diseases is known as the “obesity paradox” or “reverse epidemiology”. Due to the obesity paradox, overweight and obesity in patients suffering from chronic conditions like CAD may actually have a favourable prognosis [31].
In their investigation of how the obese body mass index affected hospital outcomes after CABG, Engel et al. [32] found that compared to those with obese BMI, underweight patients were at a greater risk to suffer from complications or mortality after CABG surgery. On the other hand, they did not find obesity to be able to independently predict morbidity or mortality after CABG.
Chang et al. [33] studied the protective effect of high BMI, i.e., the obesity paradox in Asians having undergone cardiac surgery and oxygenation of arterial blood during mechanical ventilation. They found overweight patients to have a better prognosis when compared to both underweight and normal weight.
Those with obesity also demonstrated better outcomes when chest physiotherapy was given. The elderly reported more prominent obesity paradoxes. The obesity paradox is probably due to the protective effect of better nutritional status in overweight and obese elderly people and the adverse effect of under nutrition in underweight subjects.
Age and nutritional status are well known determinants of the obesity paradox, but other factors which contribute to it have also been discussed. They are favourable body composition, less risky lower body obesity and Cardio respiratory fitness levels. It is a matter which needs to be discussed whether the term “obesity paradox” is an appropriate term to represent the protective effect of obesity. A different form which represents the factor which has a protective effect in each specific condition needs to be considered.
The precise pathophysiological mechanism of the obesity paradox is not known, but it is likely that the obese patients have associated conditions like diabetes and hypertension and are probably on drugs to aggressively control these conditions. The drugs they are likely to be on include beta blockers, statins and angiotensin II antagonists which are likely to improve cardiac outcome.
It is especially important to remember that in between the discussions over the obesity paradox, the proven effect of obesity as a risk factor to develop cardiovascular and metabolic diseases should not be underestimated. The need of comprehensive strategies to prevent and manage these diseases should be given utmost importance. It is also worth remembering that though the overweight and obese subjects had better cardiopulmonary outcomes than the underweight subjects, it was the subjects within normal BMI limits who had the most favourable outcomes. So, even though the adverse effects of underweight and obesity should be discussed and educated to the patients and the general public, the importance of maintaining a healthy weight should never be under-emphasised.
Conclusion
Lower-than-normal body weight (BMI < 18.5 kg/m2) should be taken as a risk factor when considering patients for cardiac surgery. Being underweight is a risk for developing complications and should be given due importance by clinical health providers. The findings of the present study emphasise the relevance of underweight status in patients undergoing CABG. Though underweight status is seen less frequently, those with underweight are more likely to undergo prolonged periods of hospitalisation after cardiac surgery. Overweight and obesity have since long been widely accepted as causes for poor prognosis in subjects undergoing cardiac surgery, but the underweight status of patients as a poor prognostic indicator has not been widely studied nor is common knowledge among clinicians working with cardiac surgery patients. In the light of these facts the results of the present study gain importance. The frequency and duration of physical therapy treatment can be increased in underweight and obese patients during hospital inpatient period after CABG.
Limitations
The limitations which have to be kept in mind while interpreting the results of the present study are as follows: Firstly, the medications taken by the patient and other parameters such as different intra operative procedures were not controlled. Secondly, the physiotherapy interventions were carried out only during the hospital inpatient phase, so long term pulmonary outcome could not be measured. Finally, evaluating the presence of atelectasis by chest x-ray as opposed to computed tomography scan and evaluating added sounds by stethoscope instead of ultrasonography was also a limitation of the study. In addition, the following factors may have confounded the results of the study to varying levels: the presence of COPD was not studied post operatively, though the patients who presented with COPD pre operatively were excluded. The incidence of low cardiac output syndrome was not ruled out post operatively, and the smoking status of the study subjects was not considered when including them in the study.
Scope for the further work
Further investigation can focus on randomised controlled trial to find out the pulmonary outcome after Phase II and Phase III cardiac rehabilitation; with these we can find out the long term effect of physical therapy after CABG. Future studies can measure long term functional outcome after CABG. Future investigations can focus to find out the intensity of pain and extent of pulmonary complications after CABG.
References
Mullany CJ. Coronary artery bypass surgery. Circulation. 2003;107:e21–2.
Brooks-Brunn JA. Postoperative atelectasis and pneumonia. Heart Lung. 1995;24:94–115.
Smetana GW. Preoperative pulmonary evaluation. N Engl J Med. 1999;340:937–44.
Cavenaghi S, Ferreira LL, Marino LH, Lamari NM. Respiratory physiotherapy in the pre and postoperative myocardial revascularization surgery. Rev Bras Cir Cardiovasc. 2011;26:455–61.
Lopes CR, de Brandäo CM, Nozawa E, Auler Júnior JO Jr. Benefits of non-invasive ventilation after extubation in the postoperative period of heart surgery. Rev Bras Cir Cardiovasc. 2008;23:344–50.
Eagle KA, Guyton RA, Davideff R, et al. ACC/AHA Guidelines for coronary artery bypass graft surgery: executive summary and recommendations a report of the American college of cardiology/American heart association task force on practice guidelines (committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation. 1999; 100:1464–80.
Westerdahl E, Lindmark B, Almgren SO, Tenling A. Chest physiotherapy after coronary artery bypass graft surgery. A comparison of three different deep breathing techniques. J Rehabil Med. 2001;33:79–84.
Kleinloog R, McFarlane T. Does cold blood cardioplegia solution cause deterioration in clinical pulmonary function following coronary artery bypass surgery? Perfusion. 2007;22:103–13.
Opasich C, De Feo S, Pinna GD, et al. Distance walked in the 6-minute test soon after cardiac surgery toward an efficient use in the individual patient. Chest. 2004;126:1796–801.
Florey CV. The use and interpretation of ponderal index and other weight-height ratios in epidemiological studies. J Chronic Dis. 1970;23:93–103.
Gurm HS, Whitlow PL, Kip KE. The impact of body mass index on short-and long term outcomes in patients undergoing coronary revascularization. Insights from the bypass angioplasty revascularization investigation (BARI). J Am Coll Cardiol. 2002;39:834–40.
Ringback WG, Eliasson M, Rosen M. Underweight, overweight and obesity as risk factors for mortality and hospitalization. Scand J Public Health. 2008;36:169–76.
Inzitari M, Doets E, Bartali B. et al. Nutrition in the age-related disablement process. J Nutr Health Aging. 2011;15:599–604.
Potapov EV, Loebe M, Anker S, et al. Impact of body mass index on outcome in patients after coronary artery bypass grafting with and without valve surgery. Eur Heart J. 2003;24:1933–41.
van der Peijl ID, Vliet Vlieland TP, Versteegh MI, Lok JJ, Munneke M, Dion RA. Exercise therapy after coronary artery bypass graft surgery: a randomised comparison of a high and low frequency exercise therapy program. Ann Thorac Surg. 2004;77:1535–41.
Ciesla ND. Chest physical therapy for patients in the intensive care unit. Phys Ther. 1996;76:609–25.
Jones A. Evidence-based physiotherapy in intensive care. Hong Kong Physiotherapy J. 2000;18:47–52.
Finkelstein SM, Lindgren B, Prasad B, et al. Reliability and validity of spirometry measurements in a paperless home monitoring diary programme for lung transplantation. Heart Lung. 1993;22:523–33.
American Thoracic Society. ATS statement: guidelines for the six- minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Baptista VC, Palhares LC, de Oliveira PP, et al. Six-minute walk test as a tool for assessing the quality of life in patients undergoing coronary artery bypass grafting surgery. Rev Bras Cir Cardiovasc. 2012;27:231–9.
Schoindre Y, Meune C, Dinh-Xuan A, Avouac J, Kahan A, Allanore Y. Lack of specificity of the 6-minute walk test as an outcome measure for patients with systemic sclerosis. J Rheumatol. 2009;36:1481–5.
King S, Wessel J, Bhambhani Y, Maikala R, Sholter D. Maksymowych W. Validity and reliability of the 6-minute walk in persons with fibromyalgia. J Rheumatol. 1999;26:2233–7.
Chen Y, Rennie D, Cormier YF, Dosman J. Waist circumference is associated with pulmonary function in normal- weight, overweight, and obese subjects. Am J Clin Nutr. 2007;85:35–9.
Melo LC, Silva MA, Calles AC. Obesity and lung function. A systematic review. Einstein. 2014;12:120–5.
Shah HD, Shaikh WA, Patel D, Singh SK. Dynamic lung function in underweight Gujarati Indian adolescents boys. National J Community Med. 2012;3:142–5.
Nair RH, Kesavachandran C, Shashidhar S. Spirometric impairments in undernourished children. Indian J Physiol Pharmacol. 1999;43:467–73.
Lewis MI, Sieck GC, Fournier M, Belman MJ. Effect of nutritional deprivation on diaphragm contractility and muscle fibre size. J Appl Physiol. 1986;60:596–603.
Fiorina C, Vizzardi E, Lorusso R, et al. The 6-min walking test early after cardiac surgery. Reference values and the effects of rehabilitation programme. Eur J Cardiothoraci Surg. 2007;32:724–9.
Donahoe M, Rogers RM, Wilson DO, Pennock BE. Oxygen consumption of the respiratory muscles in normal and in malnourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1989;140:385–91.
Enright PL, McBurnie MA, Bittner V, et al. The 6-min walk test: a quick measure of functional status in elderly adults. Chest. 2003;123:387–98.
Benedetto U, Danese C, Codispoti M. Obesity paradox in coronary artery bypass grafting: myth or reality? J Thorac Cardiovasc Surg. 2014;147:1517–23.
Engel AM, McDonough S, Smith JM. Does an obese body mass index affect hospital outcomes after coronary artery bypass graft surgery? Ann Thorac Surg. 2009;88:1793–800.
Chang CH, Lee FY, Wang CC, et al. An obesity paradox of Asian body mass index after cardiac surgery: arterial oxygenations in duration of mechanic ventilation. SciWorldJ. 2013; doi:10.1155/426097.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Authors agree that there was no source of conflict of interest.
Rights and permissions
About this article
Cite this article
Soman, A., Mundyat, G., Kumar, D. et al. Does body mass index influence pulmonary function test values and functional exercise capacity after chest physiotherapy following coronary artery bypass graft. Indian J Thorac Cardiovasc Surg 34, 116–124 (2018). https://doi.org/10.1007/s12055-017-0528-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12055-017-0528-8