Abstract
Background
Bariatric surgery in superobese (BMI > 50 kg/m2) and super-superobese (BMI > 60 kg/m2) patients can be a formidable technical and therapeutic challenge because these patients often present multiple medical, surgical, and anesthetic risks. Only a few dedicated reports on different surgical options in this kind of patient population are available. The aim of this study is the evaluation of laparoscopic adjustable gastric banding (LAGB) results in an unselected populations of super-superobese patients operated during the last 4 years.
Methods
Super-superobese (BMI > 60 kg/m2) patients who underwent LAGB were recruited from the prospective database of our institution. LapBand® System (Allergan, Irvine, CA, USA) was positioned in all cases via pars flaccida, 1–2 cm below the gastroesophageal junction and fixed anteriorly with three non-absorbable stitches. The band was not filled at the time of surgery. Operative time, co-morbidities, laparotomic conversion, intra- and postoperative complications, mortality, and weight-loss-related parameters were considered. Data were expressed as mean ± standard deviation, except as otherwise indicated.
Results
From January 2003 to December 2006, 823 patients underwent a bariatric surgical procedure, 95 of whom (11.5%) were BMI > 60 kg/m2 (59 F/ 36 M; mean BMI, 62.5 ± 4.2; range, 60.1–77 kg/m2; mean age 38.5 ± 13.5, range 18–61 years old). Mortality, intraoperative, and 30-day major complications were absent. One or more preoperative co-morbidities were diagnosed in 90 of 95 (94.7%) patients. After 1 year, co-morbidity-free patients increased from five of 95 (5.3%) to 27 of 95 (28%; p < 0.001). Patients with three or more co-morbidities decreased from 62 of 95 (65.3%) to 0 (p < 0.001). Mean BMI was 43.6 in 95 of 95, 37.9 in 55 of 55, 29.1 in 11 of 11, and 28.9 in five of five patients at 12, 24, 36, and 48 months, respectively. At the same time, %EWL was 53.6, 69.7, 81.3, and 82.1 and %EBL was 50, 66, 90, and 91.
Conclusions
LAGB can be considered an appropriate bariatric surgical option in super-superobese patients both for low morbidity rate and weight loss. The end-point of BMI < 30 can be achieved with a multidisciplinary follow-up. Additional studies with more patients and longer follow-up are needed to confirm these observations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery in superobese (BMI > 50 kg/m2) and super-superobese (BMI > 60 kg/m2) patients can be a formidable technical and therapeutic challenge [1–6]. These patients often present multiple medical, surgical, and anesthetic risks, and surgical treatment is mandatory because other available regimens are without effect. Different bariatric surgical options in this population have been reported, with different rates of efficacy, complications, and mortality [7–14].
The aim of this study is the evaluation of laparoscopic adjustable gastric banding (LAGB) results in an unselected population of super-superobese patients operated during the last 4 years.
Methods
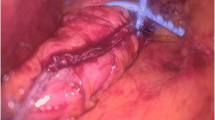
Super-superobese (BMI > 60 kg/m2) patients were recruited from the prospective database of our institution. A detailed informed consent with special statement on personal data treatment was signed by all patients. All those patients underwent LapBand® System (Allergan, Irvine, CA, USA) positioned via pars flaccida, 1–2 cm below the gastroesophageal junction and fixed anteriorly by gastric wall plication and three non-absorbable stitches. Three different bands were positioned: Allergan 10 cm band, AP small band, and AP large band. The band was not filled at the time of surgery. All patients underwent psychological, nutritional, and medical evaluation preoperatively and during the follow-up controls. Bioenterics intragastric balloon (BIB) was positioned in ten ASA IV patients to underscore the anesthetic risk. Intragastric balloon was positioned after diagnostic endoscopy and filled with saline (500 ml) and methylene blue (10 ml). During the first postoperative year, follow-up surgical controls were done every 3 months; during the following years, every 6 months. Patients follow up schedules through also different team members (psychologist, dietitian, endocrinologist, physical trainer). All patients were enrolled in occupational therapy and hobbies (i.e., music school, cooking school), and the most frequent controls and contacts (weekly) were done by a counseling staff. Band adjustment was performed “on demand” and X-ray control. The total volume inflated was calculated on the basis of time of band stricture clearing from barium enema. Operative time, co-morbidities, laparotomic conversion, intra- and postoperative complications, mortality, and weight-loss-related parameters were considered. Data were expressed as mean ± standard deviation, except as otherwise indicated. Statistical analysis was done by Fisher’s exact test, and p < 0.05 was considered significant.
Results
From January 2003 to December 2006, 823 patients underwent a bariatric surgical procedure, 95 of whom (11.5%) were BMI > 60 kg/m2 (59 F/ 36 M; mean BMI, 62.5 ± 4.2; range, 60.1–77 kg/m2; mean age 38.5 ± 13.5, range 18–61 years old). Thirty-two of 95 (33.7%) patients had central obesity. Ten of 95 (10.5%) ASA IV patients underwent preoperative BIB® to underscore ASA classification. BIB was well tolerated in all patients and removed after a minimum of 6 months. At time of removal, all were ASA III, and %EBL was 28.1. Mean operative time was 40 ± 20 (range 15–60) min. Mortality, intraoperative, and 30-day major complications were absent. Only two (2.1%) patients presented dysphagia and trocar bleeding, respectively, and were treated conservatively. Late complications were absent. All patients were present at follow-up.
Number and frequency of band adjustment were different in each patient. In three (%) patients, band adjustment was not necessary. In 24, 42, 16, and ten patients, one, two, three, and four band adjustments were, respectively, performed. In patients with one adjustment, ≤50% band was filled. In those with two, three, and four adjustments, the band was filled at >50% ≤60%, >60% ≤70%, and >70%, respectively.
One or more preoperative co-morbidities were diagnosed in 90 of 95 (94.7%) patients: hypertension (44 of 90; 49.3%), diabetes (11 of 90; 12.6%), sleep apnea and Pickwick syndrome (35 of 90; 39.4%), osteoarthropathy (65 of 90; 71.8%), dyslipidemia (22 of 90; 24.9%), NASH (ten of 90; 11.1%), others (44 of 90; 49.3%; Table 1). All patients with hypertension underwent 24-h map procedure. Sleep apnea was diagnosed by polysomnography, repeated after 1 year. NASH diagnosis was made and followed by ultrasound (US) scan and by biochemical modifications supported by liver biopsy at time of surgery. After 1 year, co-morbidity-free patients increased from five of 95 (5.3%) to 27 of 95 (28%; p < 0.001). Patients with three or more co-morbidities decreased from 62 of 95 (65.3%) to 0 (p < 0.001). The single co-morbidity 12-month results are reported in Table 2.
Mean BMI was 43.6 in 95 of 95, 37.9 in 55 of 55, 29.1 in 11 of 11, and 28.9 in five of five patients at 12, 24, 36, and 48 months, respectively. At the same time, %EWL was 53.6, 69.7, 81.3, and 82.1, and %EBL was 50, 66, 90, and 91 (Figs. 1 and 2).
Discussion
Super-superobese is considered a challenging field in bariatric surgery because of the high rate of morbidity and mortality related to multiple medical, surgical, and anesthetic risks [1–6]. The best surgical treatment in this population to achieve optimal weight loss is still a matter of concern. Surgical laparotomic or laparoscopic options reported include biliopancreatic diversion (BPD, duodenal switch (BPD/DS), Roux-en-Y gastric bypass (RYGBP), and LAGB eventually with previous intragastric balloon [1, 5, 9, 13]. Few comparative reports have been published. Mongol et al. [10] reported a significantly higher early complication rate in RYGBP (10%) than in LAGB (2.8%) superobese operated patients. Dolan et al. [15], comparing BPD, RYGBP, and LAGB in superobese patients, showed that BPD had significantly more complications (56.5%) than LAGB (8.3%) linked to anastomotic leak, wound-related problems and bleeding. Murr et al. [16] reported 30% morbidity in 11 patients with BMI > 60 who underwent BPD compared to 20% in 26 patients treated with distal RYGBP. In early non-comparative reports with laparoscopic Roux-en-Y gastric bypass (LRYGBP), Oliak et al. [17] and Artuso et al. [11] reported 10% and 5% complication rates, respectively, and both reported 5% mortality (Table 3). Regan et al. [9] recorded five complications in seven patients who underwent sleeve gastrectomy followed by LRYGBP. Fazylov et al. [8] reported 7.8% mortality and 29.4% complications in 102 patients who underwent BPD/DS. Because of the high rate of complications, super-superobese patients should be treated less aggressively, with a shorter and less invasive surgical approach. Fielding et al. [1] reported 76 super-superobese patients that underwent LAGB with three minor complications (patients with BMI > 100) with longer hospital stay. In the present experience with BMI > 60, LAGB-treated patients mortality was absent with only two minor complications (trocar bleeding and dysphagia).
Some authors have considered the end-point of bariatric surgery in superobese and super-superobese patients to be different from that in patients with BMI 45 kg/m2. Loss of co-morbidities was reported as the primary end-point in these patients, while it is considered unlikely that they will achieve BMI < 30 kg/m2 because of their extremely high initial BMI. Capella and Capella reported a BMI reduction from 60 to 32 kg/m2 in RYGBP-operated patients [2]. Murr et al. [16] reported a BMI reduction from 67 to 42 and from 64 to 37 in patients who underwent distal RYGBP and BPD, respectively. Brolin et al. [3] reported a BMI decrease from 67 to 37 and from 55 to 44 in patients who underwent long limb or standard RYGBP. It has been reported that weight loss is slower and more gradual in LAGB-operated patients as compared with more invasive bariatric procedures. Farkas, in a 2-year follow-up study, recorded a mean EWL of 67% in patients who underwent LRYGBP [12]. Fielding reported a BMI reduction from 69 to 33 in 76 LAGB-operated patients after 3 years of follow-up [1]. In the present experience, after 4 years of follow-up, BMI was 29.1, showing that it is possible to achieve the end-point of BMI < 30 kg/m2. These results seem to be related, above all, to modifications in follow-up of these patients and the presence of counseling staff that keep the patient in touch with the bariatric center at late weekly. The very close patient contact with the bariatric center increases the level of patients and bariatric staff motivation. Patients’ self-esteem increased also with group activities, where all patients were allocated after surgery.
Conclusions
LAGB can be considered an appropriate bariatric surgical option in super-superobese patients, both for low morbidity rate and weight loss. The end-point as BMI < 30 can be achieved with a multidisciplinary follow-up. Additional studies with longer follow-up and larger series are needed to confirm these results in these challenging patients.
References
Fielding GA. Laparoscopic adjustable gastric banding for massive superobesity (>60 body mass index kg/m2). Surg Endosc. 2003;17:1541–5.
Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass. Am J Surg. 1969;171:74–9.
Brolin R, LaMarca L, Kenler H, et al. Malapsorptive gastric bypass in patients with superobesity. J Gastrointestinal Surg. 2002;6:195–205.
Sarr MC, Felty CC, Hilmer DM, et al. Technical and practical considerations involved in operations on patients weighing more than 270 Kg. Arch Surg. 1995;1309:102–5.
Marceau P, Hold PS, Simmond S, et al. Biliopancreatic diversion with duodenal switch. World J Surg. 1998;122:947–54.
Angrisani L, Furbetta F, Doldi SB, et al. Results of the Italian multicentric study on 239 superobese patients treated by adjustable gastric banding. Obes Surg. 2002;12:846–50.
Myers JA, Sarker S, Shayani V. Treatment of massive superobesity with laparoscopic adjustable gastric banding. SOARD 2006;2:37–40.
Fazylov RM, Savel RH, Horovitz JH, et al. Association of super-super-obesity and male gender with elevated mortality in patients undergoing the duodenal switch procedure. Obes Surg. 2005;15:618–23.
Regan JP, Inabnet WB, Gagner M, et al. Early experience with two stage laparoscopic roux-en-Y gastric bypass as an alternative in the Super-superobese patient. Obes Surg. 2003;13:861–4.
Mongol P, Chosidow D, Marmuse JP. Laparoscopic gastric bypass versus laparoscopic adjustable gastric banding in the superobese: a comparative study of 290 patients. Obes Surg. 2005;15:76–81.
Artuso D, Wayne M, Kaul A, et al. Extremely high body mass index is not a contraindication to laparoscopic gastric bypass. Obes Surg. 2004;14:750–4.
Farkas DT, Vemulapalli P, Haider A, et al. Laparoscopic Roux-en-Y gastric bypass is safe and effective in patients with a BMI > 60. Obes Surg. 2005;15:486–93.
Helling TS. Operative experience and follow up in a cohort of patients with a BMI >70 Kg/m2. Obes Surg. 2005;15:482–95.
Parikh MS, Shen R, Weiner M, et al. Laparoscopic bariatric surgery in superobese patients (BMI > 50) is safe and effective: a review of 332 patients. Obes Surg. 2005;15:858–63.
Dolan K, Hatzifotis M, Newbury L, et al. A comparison of laparoscopic adjustable gastric banding and iliopancreatic diversion in superobesity. Obes Surg. 2004;14:165–9.
Murr MM, Balsiger BM, Kennedy FP, et al. Malabsorptive procedures for severe obesity: comparison of pancreaticobiliary bypass and very, very long limb Roux-n-Y gastric bypass. J Gastrointest Surg. 1999;3:607–12.
Oliak D, Ballantyne GH, Davies RJ, et al. Short-term results of laparoscopic gastric bypass in patients with BMI > or = 60. Obes Surg. 2002;12:643–7.
Acknowledgment
Here’s to Antonio J Cascardo, wonderful surgeon, great friend.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torchia, F., Mancuso, V., Civitelli, S. et al. LapBand System® in Super-Superobese Patients (>60 kg/m2): 4-Year Results. OBES SURG 19, 1211–1215 (2009). https://doi.org/10.1007/s11695-008-9760-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9760-z