Abstract
Background
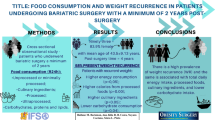
Weight loss and long-term weight maintenance in bariatric surgery patients are related to maintaining satiety. It can be related to glycemic load (GL) and carbohydrate (g CHO) intake. The aim of this study was to investigate the effect of g CHO and GL and in weight loss on patients who had undergone bariatric surgery.
Method
The following measurements/calculations were conducted as follows: current body weight (kg), current BMI, percentage of excess weight loss (PEWL), average monthly weight loss (AMWL), energy intake (kcal per day), and GL calculation. Correlations were found among the studied variables. A multiple linear regression analysis of diet variables executed with GL and weight loss.
Results
The population presented 66% of EWL. The average of total energy intake (TEI) was 1220 ± 480, and the calculated GL resulted in an average of 73.2. Negative correlations were found between AMWL and TEI (p = 0.04), and between AMWL and GL (p = 0.009); furthermore, a negative correlation was found between carbohydrate intake in grams and AMWL (p = 0.003). A positive correlation (p = 0.017) was found between GL and TEI. Weight loss and GL were also correlated. Among the intake variables, GL and g CHO consumed are held accountable for 62 percent of AMWL. The multiple linear regression analysis showed that GL and carbohydrate grams (g CHO) account for 62% of AMWL.
Conclusion
The glycemic load and grams of carbohydrate are intake factors that can be useful tools in weight loss and long-term weight maintenance on patients who have undergone Roux-en-Y Gastric Bypass (RYGB).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbid obesity is a disease refractory to diets and medications, but which is usually well responsive to bariatric surgery [1]. Of this type of surgery, the one most practiced in Brazil and in the USA is the Roux-en-Y gastric bypass (RYGB), since it has low morbimortality and is highly effective [2]. In general, about 65% to 80% of excess weight is lost in the first 12 to 18 months after surgery, stabilizing on about 50% to 60% by the end of the third year [3]. Consensus among researchers concerning the criteria for success in treating obesity with surgery is the loss of at least 50% of excess weight and long-term weight maintenance [4].
One of the factors that assures weight maintenance after surgery is the continuity of the sensation of satiation. The sensation of satiation is defined as satisfaction during an episode of food intake which contributes for the individual to stop eating or to feel the sensation of satisfaction between meals, thus resulting in a longer interval between them and lower calorie intake [5]. Patients who underwent RYGB have a tendency to reduce such sensation 6 months after surgery [6]; at this stage, patients tend to return to their traditional eating habits. Satiation takes place through hormonal, biochemical, and feeding mechanisms [7].
The reduction of appetite caused by RYGB cannot be attributed only to the precocious satiation caused by reduced gastric volume, once such sensation extends beyond the postprandial period [8]. A series of papers supports this hypothesis [8–11], thus demonstrating that a modification in the secretion of various hormones released after the RYGB has an important physiologic role in controlling appetite and satiation.
Ghrelin is a hormone produced almost entirely in the gastric fundus, which is an area that is excluded after the RYGB procedure [12]. This peptide is the only circulating orexigen known, and therefore has a stimulating effect on food consumption [13]. Frübeck et al. observed lesser plasma levels of ghrelin in patients who underwent RYGB in comparison with gastric bandage patients. These data are in conformity with other authors [14, 15]. Suppressing the ghrelin production seems to be one of the potential mechanisms by which RYGB causes an enhancement in satiation and triggers weight loss, in a process called override suppression (a paradoxical suppression of hormone production while its stimuli for secretion are still present) [8, 11].
Contrasting with ghrelin’s action, other intestinal hormones such as glucagon-like peptide-1 (GLP-1) and peptide YY (PYY) act as appetite-suppressing agents, thus being classified as anorexigens. PYY is a hormone secreted by L-cells in the final part of the small intestine in response to the presence of nutrients [16]. PYY slows down gastric and intestinal emptying and promotes better absorption. After RYGB, its postprandial secretion takes place prematurely and is more elevated [10, 17], which may be explained due to the absence of the pylorus and to the food mass passing quickly through the stomach [18]. This change in PYY secretion may contribute to food consumption reduction and to weight loss. GLP-1 promotes insulin secretion and inhibits glucagon secretion, as well as it reduces appetite and food consumption on obese patients. Its levels also tend to increase after RYGB, thus causing results similar to those of PYY [10].
As mentioned above, besides biochemical and hormonal factors, satiation also takes place through food factors. An important intake factor in maintaining satiation is related to glycemic index (GI) of foods. GI is the categorization of foods based on response of postprandial blood glucose compared to a reference food such as bread or glucose [19]. High-GI foods are thus classified because they raise blood glucose levels, which induces a greater hormonal response, i.e., a greater raise in insulinemia [20]. Since insulin is an anabolic hormone, there is a higher risk for excess calories to be stored in the form of fat. In addition, such foods provide a greater risk of causing reactive hypoglycemia due to the greater hormonal response generated [21]. In general, refined grains, potato, and saccharose have high GI. Inversely, low-GI foods are those which cause lower peaks and a lower area below the glycemic curve in the postprandial period, such as whole foods, vegetables, and whole grains. Studies have pointed out a reduction in hunger and/or increase in satiation after low-GI foods are consumed, in comparison with the consumption of high-GI foods [20, 21]. Such studies also showed that the average calorie intake in meals after high-GI foods were consumed was 29% higher than after low-GI foods were consumed. This analysis suggests that consuming high-GI carbohydrate may be associated with a higher calorie intake when compared with consuming low-GI carbohydrate [21]. Pawlak et al. [22] found that low-GI meals relate to lower appetite between meals, with a negative energy balance and consequent weight loss.
It is widely known that GI is a food characteristic, which does not consider the global glycemic effect of different foods consumed in a same meal. For addressing this glycemic effect of foods in a meal, the use of glycemic load (GL) has been praised as an important tool in studying the meal as a whole. It is the product of the available quantity of carbohydrate in a meal and the GI of foods that compose it [23, 24].
Taking into account the possibility of using glycemic load of meals as a managing tool for weight loss in this population, this study purported to investigate the effect of glycemic load of meals and the weight loss of patients who have undergone RYGB bariatric surgery.
Methods
This was a transversal, retrospective study which comprised a convenience sample with patients who were operated by means of the RYGB technique by the Gastrocirurgia staff of Brasília, in Brasília-DF.
The inclusion criteria were: to have been operated upon by the same surgeon, using the RYGB technique with a 6.8-cm restrictive band; to be between 16 to 65 years old; at least 6 months to have passed since the date of the operation; and to have periodical medical and nutritional follow-up (at least twice a year). The exclusion criteria were: patients who would not fit the inclusion criteria; patients in whom the restrictive band was not placed due to technical-surgical reasons; patients who studied nutrition or worked in such area; patients with psychiatric diseases (depression, phobias, etc.) which needed psychotropic treatment; bulimic and/or anorexic patients. The research was approved by the Research Ethics Committee of the University of Brasília’s Health Sciences Faculty. The contact with patients was made through telephone contacts. After their agreement to participate in the research, a day and time was set for data collection. The patient was interviewed only by the researcher. At the day of data collection, the patient firstly learned of the free-consent term, which was read and signed. A copy of it remained with the patient and another remained with the researcher.
The data collection consisted of anthropometric evaluation and the patient filling the 4-day food intake record. The following procedures were conducted as follows:
Weight and Height
The standard procedures of body weight and height measurement were followed, as recommended by Gordon et al. [25]. Such measurements were taken in fasting, with a digital scale with capacity for up to 300 kg and sensitiveness of 100 g (Filizola®, Brazil) and a wall stadiometer with sensitiveness of 5 mm. The body mass index (BMI) was then calculated (kg/m2). The adopted criterion for classification of nutritional state was the one from WHO [26].
Calculation of Excess Weight Loss
The criteria in the table from Metropolitan Life Foundation were followed [27].
The percentage of excess weight loss (PEWL) refers to the percentage of the difference between pre-surgery weight and current weight in relation to ideal weight. For weight loss speed analysis among patients with different postoperation periods, the average monthly weight loss (AMWL) variable was created. Thus, average monthly weight loss (AMWL) = percentage of excess weight loss (PEWL)/time lapsed after surgery in months. Considering that studies often present results in relation to 12 months of postsurgery period [28, 29], data obtained in this study were also categorized according to such period.
Food Intake
Patients were oriented to record 4 days of their food intake, one of which at least should be a weekend day. They were all supplied with instructions for filling the form and with photos of standard food serving sizes [30]. Those forms were taken home and subsequently, after having been filled in, they were returned to the researcher. The subjects were oriented to record freely all foods and drinks—except for water—they had consumed during day and night.
The average of the 4 day food record was calculated. The following averages were calculated: daily calories (kcal/day); protein (PTN), lipid (LIP), and carbohydrate (CHO) intake quantities, in grams per day and in percentage of the total energy intake (TEI) per day. The daily mean quantity of fibers consumed was also calculated. The calculation was carried out by using the Nutrisurvey® [31] nutrition support software. Household measures were turned into grams by using Pinheiro’s table [32]. Some receipts that were not previously listed in the program were calculated and included in it.
Glycemic Load of Meals
Initially, foods consumed by patients were classified as per their GI pursuant to the table published by Foster-Power et al. [23] GL was calculated by multiplying the quantity of carbohydrate existent in the consumed food serving by its GI, and the result was divided by 100. The meal GL was calculated by the sum of glycemic loads of foods in that meal [23, 33]. Bread or sugar can be adopted as standard for food GI. This study adopted the use of GI in relation to bread. For each patient, the average GL was calculated for each meal recorded during 4 days. Each patient had thus a GL value that represented the average of all meals in those 4 days. Foods that were not listed in the table and which were consumed with higher frequency among the studied population were analyzed in the Nutritional Biochemistry Laboratory of the University of Brasília in conformance with the protocol established by FAO [34].
Physical Activity
The patients were asked to inform if they practiced or not any kind of physical activity.
Statistical Analysis
The study analyzed if there was a correlation between average monthly weight loss (AMWL) and intake variables and components, such as calorie intake, macronutrients and GL of meals. Correlations were analyzed through Pearson’s correlation index. The statistical program used was the SAS version 8.2. In order to assess the effect of intake variables in the AMWL variable, the study used the multiple linear regression analysis. For the purposes of analysis, the adopted level of significance was 5%.
Results
Eighty-nine patients participated in the research, most of them being women (80%). The age average was 36.8 ± 10.7 years of age, ranging from 19 to 64. Forty-eight percent of patients were born in Brasília and 16% of them were born in the State of Minas Gerais. Fourteen percent of patients were civil servants and 10% of them were students.
Weight, BMI, and Weight Loss
Table 1 shows weight, BMI and weight loss data in the postoperation period. Among patients with less than 1 year after surgery, the mean of excess weight loss was 65%, and among patients with more than 1 year after surgery, such mean was 68% (Fig. 1). The AMWL of patients with less than 12 months after surgery was 8.6 ± 2.1% per month. Among patients with 12 months or more after surgery, such value fell to 4.0 ± 1.5%, with a significant difference between groups (p < 0.001) (Fig. 2).
Energy and Nutrient Intake, and Glycemic Load of Meals
Among the 89 patients who participated in the research, 55 subjects filled the food intake record forms. In two cases, the patient’s handwriting was illegible and they could not be found for clarifications. Consequently, their data were not analyzed (sample loss), so 53 food intake records remained. Among these, 35 patients filled in form record forms, 15 filled in) five record forms, and four subjects filled in three record forms.
The most common reasons among patients for not having filled in forms (n = 34) were: difficulty in remembering what they had eaten and difficulty in filling out the forms during 4 days.
Table 2 presents the energy and macronutrient intake dividing food intake data of patients with less than 12 months of postsurgery time from those of patients with 12 months or more of postsurgery time. It was observed that the studied population had low calorie intake. Protein intake was below the level recommended for patients who undergo bariatric surgery, which would be 80 g/day for women and 100 g/day for men [35].
The result of calculations in food intake records showed an average GL of 73.2 ± 10.6. The maximum value found was 95 and the minimum was 35.9. Among patients with less than 12 months after surgery, the mean GL was 71, and for patients with 12 months or more after surgery, the mean GL was 76 and there was significance between these groups. The minimum glycemic load among patients in the former group was 54 and the maximum GL was 95. Among patients in the latter group, minimum GL was 62.9 and maximum GL was 94.
Table 3 exemplifies the daily GL of two patients. It is observed that GL can be different among similar calorie intakes.
Correlation Between Intake and Anthropometric Variables
A positive correlation (r = 0.335) was found between GL and calorie intake (p = 0.017), i.e., the higher the glycemic load of meals, the higher the daily calorie intake. A positive correlation (r = 0.342) was also found between quantity of carbohydrate and GL (p = 0.015). A negative correlation (r = −352) was found between the percentage of calories in the menu proceeding from protein (%PTN) and GL (p = 0.012). Concerning protein intake in grams and GL, the correlation found was not significant (p = 0.193).
A negative correlation (r = −0.300) was found between AMWL and the number of daily meals (p = 0.034), i.e. the higher the number of meals, the lesser the weight loss. There was also a negative correlation (r = −0.373) between daily calorie intake and AMWL.
GL also presented negative correlation (r = −364) in relation to AMWL (p = 0.009), i.e., the lower the GL of meals, the higher the AMWL. Carbohydrate intake in grams (CHO) had negative correlation (r = −0.414) to AMWL (p = 0.003), and so did lipid intake (LIP; p = 0.044); both were significant. In relation to proteins, there was positive correlation between percentage of calories proceeding from proteins (r = 0.305, p = 0.029), but there was no correlation of AMWL to protein intake in grams.
AMWL Forecast Equation
In order to evaluate the influence of intake variables in weight loss in the studied population, a multiple linear regression analysis was carried out.
Initially, the simple correlation analysis was carried out by making use of Pearson’s correlation coefficient. The following variables were analyzed: GL, number of meals per day (no. meals/day), daily calorie intake (kcal/day), percentage of calories proceeding from proteins (PTN), protein intake per kg of body weight (PTN/kg), CHO (g), percentage of calories proceeding from lipids (LIP), LIP (g), and AMWL.
The simple correlation analysis indicated variables individually, as related to AMWL. Since the CHO (g) variable was the one which presented higher correlation to average monthly weight loss, it was the first variable to be selected in the model. It was observed that the CHO (g) variable is accounted for 28.28% of AMWL. Afterwards, once again the regression analysis was conducted including in the model the daily calorie intake (kcal/day) variable. With the result, it was concluded that the two variables can not be included simultaneously in the model, for they are highly correlated, thus causing a multicollinearity problem. Therefore, only the CHO (g) variable was kept.
The GL variable was then included, and there was significance (p < 0.0001). It was verified that such inclusion contributed for improving the adjustment, which turned from 28.28% into 62.87%. In addition, the two variables together in the model do not present multicollinearity.
Afterwards, the number of meals variable was included, but since it was not statistically significant (p = 0.6418), it was not kept in the model. The protein grams, lipid grams and percentage of carbohydrate variables were also excluded for not having significance.
From the adjustment of the various models of multiple linear regression, we observed that only the CHO (g) and GL variables were kept in the model, being that:
That is, the average monthly weight loss decreases 1.5 percentage points for every increment of 10 GL units, and it decreases 1.6 percentage points for every increment of 10 CHO grams. GL and the quantity in grams of carbohydrate consumed represent 63% of the observed average monthly weight loss (Fig. 3).
Physical Activity
Only 20% of the sample practiced a regular physical activity. We found no correlation between weight loss and the practice of physical activity.
Discussion
The patients examined in this study presented an average loss of 66.1% of excess weight, which represents a satisfactory loss in bariatric surgery [4, 36].
The mostly used formulas in bariatric surgery for calculating the ideal weight are: the average weight listed in the Metropolitan Life Insurance Company’s table [27], calculation based on BMI of 25 kg/m2 [37]. The 25 kg/m2 BMI reflects an ideal weight higher than the one presented by previous methods. This study based the ideal weight calculation on the average provided by the Metropolitan Life Insurance Company’s table [27], as presented in the methodology. Sugerman et al. [37], who used the same methodology for calculating ideal weight, showed an excess weight loss of 67 ± 18% in patients with 12 months after surgery. In the population analyzed in this study, among patients with more than 12 months of postsurgery time (n = 42), we found 68 ± 18% of excess weight loss, i.e., a loss similar to Sugerman’s results [37]. Christou et al. [38] who also used the same methodology for calculating ideal weight, found 67.1% of excess weight loss in patients with 30 months of postsurgery time.
Usually, studies discuss the postsurgery weight loss in patients with less or more than 12 months of postsurgery time aiming to analyze weight loss in the highest speed period, which is the first year after the surgery, apart from the second year on, when patients lose weight more slowly or have already achieved a healthy weight. In this study, results assessed according to this period also presented comparable results. The AMWL among patients with less than 12 months of postsurgery time was higher than the AMWL among those with 12 months or more of postsurgery time. However, the PEWL variable does not present properly the individual differences in the rhythm of weight loss. The PEWL calculated in this study, despite being an average of weight loss in relation to total months after the operation, now considers the time (in months) in which weight loss occurred. Thus, AMWL seems to be a useful sensitive indicator, for evaluating the magnitude of weight loss in the postoperation period of each patient. From this variable, it was possible to observe that AMWL is more accelerated in the first 12 months after surgery (8.6 ± 2.0%), decreasing to an average of 4.0 ± 1.5% after that period. Other studies [39–42] corroborate these results, once that after the first year of more substantial weight loss, there is a reduction or stabilization in weight loss. This difference in the rhythm of weight loss is due to an increase of food intake and reduction of body weight. As a result, the calorie intake per body weight kilogram reaches values that favor a decrease in the weight loss speed. There is higher food intake among patients with more than 12 months of postsurgery time since they have developed more capability to consume foods. AMWL in this study correlated well to variables that show the difference of food intake between those two groups.
The results of food intake in this population remained a little above other studies. In other studies with patients who underwent the same surgery with the same technique, researchers observed an intake of 890 ± 407 kcal 6 months after the operation and 1,100 ± 426 kcal by the end of 1 year [28, 39]. On patients with 2 years after surgery, Wardé-Kamar et al. [43] found intake of 1,800 kcal/day.
In food intake studies, in general, the type of tool has influence on the food inquiry. Such types of study are affected by various measurement biases [44, 45]. In the case of this research, the difference found in relation to other studies may be attributed to the evaluation method of food intake. The studies of Andersen et al. [46] and Blake [47] used the 1-day food record for nutritional calculations. Brown [48] used a 3-day food record. Other studies [28, 39, 43] used 24-h food recall. Food records, which take into account three or more days of food intake, need more collection time and require patients to be literate, but represent better the intrapersonal variability, thus being more indicated for the study on food-intake pattern [44, 45].
We found in this study a negative correlation between calorie intake (kcal/day) and AMWL. Patients who have consumed less calories have lost more weight. It was also observed that the highest lipid and carbohydrate intake was related to a lesser weight loss. This study suggests that the intake of a high glycemic load favors higher calorie intake and also lesser weight loss. A study by Roberts [49] suggested that high GL meals favor an increase of 29% in calorie intake when compared to low glycemic-load meals.
According to the Canadian Diabetes Association (CDA) [48], low glycemic-load meals are composed by foods with a glycemic index below 55; medium glycemic-load meals contain glycemic-index values ranging between 56 and 69, and high glycemic-load meals are composed by foods with GI above 70. Calories in the menu proceeding from proteins (%PTN) correlate negatively to the GL. That is, the higher the percentage of proteins in the menu, the lesser the GL and the higher the AMWL.
There was a positive correlation between grams of carbohydrate consumed and the average GL. That was expected since GL is calculated based on the quantity of carbohydrate in meals. In relation to AMWL, the highest consumption of carbohydrate in grams was correlated to a lesser AMWL. This fact may be associated to the GL, since when carbohydrate in a meal is increased, so is the GL, consequently.
It is important to underscore that in the methodology for calculating the average GL of meals, only the GL of foods which are important source of carbohydrate is calculated. Foods such as meat, butter, eggs, oil, and chicken are not accounted into the GL of meals. Nevertheless, the metabolic impact of consuming a high-GI food—such as white bread—alone, and its impact when consumed with a high-protein food or one which is a source of diet fat—such as fried eggs or bread with butter—is not the same, for we know that fat and protein slow down the gastric emptying process, which is likely to reduce the GL of such kind of meal. This is not analyzed in the calculation of the GL of meals, pursuant to criteria established to date.
We found a negative correlation between AMWL and the number of meals. The higher the number of meals, the lower the AMWL. We also found a significant positive correlation between number of meals and daily calorie intake. An increase in the number of meals favors higher calorie intake and lesser weight loss.
We have not found an association between number of meals and GL of meals. The definition of “satiety,” as per Blundell and Burley [49], Hsu et al. [40], and Gerstein et al. [5], includes two terms with different meanings. The term “satiety” means absence of appetite between meals, thus contributing for a lesser number of meals, and the term “satiation” means a sensation of satisfaction which contributes for the patient to stop eating during the meal. This study indicated a possible relation of the GL to “satiation,” and not to “satiety.” Low GL meals have contributed for a sensation of satiation which may have contributed for a lesser calorie intake, but there was no relation to satiety (lesser number of meals).
There was no correlation of fibers to GL. The low average quantity consumed by the patients may be one of the reasons of this lack of correlation. The mechanic restriction in the gastric pouch is one of the factors that makes it difficult to increase the quantity of fibers in the diet. On the other hand, fiber composition data of tables are usually limited and this may also have contributed for the low fiber values consumed by patients.
In the multiple linear regression analysis, it was observed that the GL of meals and the quantity of carbohydrate in grams have great influence over the weight loss of these patients, thus being held accountable for 63% of the AMWL in this population. It was observed that the AMWL decreases 1.5 percentage points for every 10-unit increment on GL, and that it decreases 0.1 percentage point for every 1-carbohydrate-gram increment on the diet.
An important bias in this study is that the researcher is also the nutritionist who follows up the group of patients. Such fact may have altered the answers of patients. They may have increased the protein content of meals for knowing that such habit is important for their nutritional state, and they may also have omitted the consumption of sweets, alcohol, and other highly caloric foods with no nutritional value.
Conclusion
The study suggested that the usage of meal GL calculation and management of the quantity of daily consumed carbohydrate may be useful tools in the nutritional follow-up of patients who underwent bariatric surgery (RYGB). We found that these two variables are held accountable for 63% of the AMWL. For every 10-unit decrement in the GL, there is an increase of two percentage points in the monthly weight loss. A higher quantity of daily calories proceeding form proteins was also related to higher weight loss. A higher quantity of proteins is also associated to a lesser-glycemic-load meal, whereas an increase in the diet’s quantity of carbohydrate correlates to a higher glycemic load. Thus, in addition to the nutritional characteristics already addressed currently in the diet guidance of these patients—such as daily kilocalories, proteins, lipids, vitamins, minerals, fibers, diet fractionation—the glycemic load of meals and the quantity of daily consumed carbohydrate are diet characteristics that may be of help to lesser calorie intake and adequate weight loss.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric review. JAMA. 2004;292:1725–37.
Mognol P, Chosidow D, Marmuse JP. Laparoscopic conversion of laparoscopic gastric banding to Roux-en-Y Gastric Bypass: a review of seventy patients. Obes Surg. 2004;14:1349–53.
Sugerman HJ, et al. Gastric bypass for treating severe obesity. Am J Clin Nutr Bethesda. Apr 2000;55(2):108–13.
Brolin RE. Bariatric surgery and long-term control of morbid obesity. JAMA. 2002;288:2793–6.
Gerstein DE, Woodward-Lopez G, Evans AE, et al. Clarifying concepts about macronutriets’ effect on satiation and saciety. J Am Diet Assoc. 2004;104:1151–3.
Flanagan L Jr. Understanding the function of the small gastric pouch. In: Deitel M, Cowan GSM, editors. Update: surgery for morbidly obese patient. Toronto: FD Communications Inc.; 2000. p. 147–60.
Kristensen ST. Social and cultural aspects perspectives on hunger, appetite and satiety. Eur J Clin Nutr. 2000;54(6):473–8.
Cummings DE, Overduin J, Foster-Schubert K. Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab. 2004;89(6):2608–15.
Fruhbeck G, Diez-Caballero A, Gil MJ, et al. The decrease in plasma ghrelin concentrations following bariatric surgery depends on the functional integrity of the fundus. Obes Surg. 2004;14:606–12.
Kral J. Surgical treatment of obesity. Nat Clin Pract. 2007;3(8):574–83.
Cummings DE, Weigle DS, Frayo RS, et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–30.
Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, et al. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001;86(10):4753–8.
Cummings DE, et al. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001;50:1714–9.
Hanusch-Enserer U, Cauza E, Brabant G, et al. Plasma ghrelin in obesity before and after weight loss after laparoscopic adjustable gastric banding. J Clin Endocrinol Metab. 2004;89:3352–8.
Stoeckli R, Chanda R, Langer I, et al. Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res. 2004;12:346–50.
Tso P, Liu M. Ingested fat and satiety. Physiol Behav. 2004;81:275–87.
Morínigo R, et al. Glucagon-like Peptide-1, Peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2006;91(5):1735–40.
Korner J, Bessler M, Cirilo LJ, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90(1):359–65.
Jenkins DJ, Wolever TM, Taylor RH, et al. Glycemic Index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr. 1981;34:362–6.
Ludwig DS. Dietary glycemic index and obesity. J Nutr. 2000;130:280s–3s.
Roberts SB. High-glycemic index foods, hunger and obesity: is there a connection? Nutr Rev. 2000;8:163–9.
Pawlak DB, Ebbeling CB, Ludwig DS. Should obese patient be counseled to follow a low-glycaemic index diet? Yes. Obes Rev. 2002;3:235–43.
Foster-Power K, Holt SH, Brand-Miller JC. International table of glycemic index and glycemic load values. Am J Clin Nutr. 2002;76:5–56.
Ebbeling CB, Ludwing DS. Treating obesity in youth: should dietary glycemic load be a consideration? Adv Pediatr. 2001;48:179–212.
Gordon CC, Chumlea WC, Roche AF. Stature, recumbent length and weight. In: Lohman TG, Roche AF, Martorell R, editors. Anthropometrics standarlization reference manual. Champaign, IL: Human Kinetics; 1988. p. 3–8.
World Health Organization. Physical status: the use and interpretation of anthropometry. Geneva: WHO; 1995.
Metropolitan Height and Weight Tables 1983. Metropolitan Life Foundation, Statistical Bulletin 1959.
Moize V, Geliebter A, Gluck. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13:23–8.
Cottan DR, Atkinson J, Anderson A, et al. A case-controlled matched-pair cohort study of laparoscopic Roux-en-Y Gastric Bypass and lap-band® patients in a single US center with three-year follow-up. Obes Surg. 2006;16:534–40.
Botelho CZ, Viana RPT, Fli MF, et al. Registro Fotográfico para inquéritos Dietéticos utensílios e porções. Goiânia: UFG; 1996. p. 21–63.
Nutrisurvey. Available at http://www.nutrisurvey.de/. Accessed in December 2002.
Pinheiro ABV, Lacerda EMA, Benzecry EH, et al. Tabela para Avaliação de Consumo Alimentar em Medidas Caseiras. São Paulo: Atheneu; 2000.
Ludwig D. The glycemic index physiological mechanism relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287:2414–23.
FAO/WHO. Expert consultation on carbohydrates in human nutrition. Geneva; 1998.
Woodward BG. The surgical experience. In: A complete guide to obesity surgery. 1st ed. Traffor Publishing.
Balsiger BM, Murr MM, Poggio JL, et al. Bariatric surgery. Med Clin North Am. 2000;84:477–89.
Sugerman HJ, Londrey GL, Kellum JM, et al. Weight loss with vertical banded gastroplasty and Roux-Y gastric bypass for morbid obesity in selective versus random assignment. Am J Surg. 1989;157:93–102.
Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidily and health care use in morbidly obese patient. Ann Surg. 2004;240:416–24.
Brolin RE, Robertson LB, Kenler HA, Cody RP. Weight loss and dietary intake aftervertical banded gastroplasty and Roux-en-Y gastric bypass. Ann Surg. 1994;220.
Hsu GLK, Benoti PN, Dwyer, et al. Nonsurgical factors that influence the outcome of bariatric surgery: a review. Psychosom Med. 1998;60:338–46.
Brolin RE. Gastric bypass. In: Sugerman HJ, editor. The surgical clinics of North America. Obesity surgery. Vol. 81. Pennsylvania: Saunders Company; 2001. p. 1077–95.
Stocker DJ. Management of bariatric surgery patient. Endocrinol Metab Clin N Am. 2003;32:437–57.
Wardé-Kamar J, Rogers M, Flancbaum, et al. Calorie intake and meal patterns up to 4 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2004;14:1070–90.
Banegas JR. Diretrizes para la elaboracion de estúdios poblaciones de alimentacion y nutricion; 1994.
O’Neil PM. Assessing dietary intake in management of obesity. Obes Res. 2001;9(5):361–6.
Andersen T, et al. Pouch volume stoma diameter and clinical outcome after gastroplasty for morbid obesity. Scand Gastroenterol. 1984;19:643–9.
Blake M, et al. Assessment of nutrient in association with weight loss after gastric restrictive procedures for morbid obesity. Aust NZJ Surg. 1991;61:195–9.
Canadian Diabetes Association. Available at www.diabetes.ca. Accessed in January 2006.
Blundell JE, Burley VJ. Satiation, satiety and the action of fibre on food intake. Int J Obes. 1997; Suppl 1:9–25.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faria, S.L., Faria, O.P., Lopes, T.C. et al. Relation Between Carbohydrate Intake and Weight Loss After Bariatric Surgery. OBES SURG 19, 708–716 (2009). https://doi.org/10.1007/s11695-008-9583-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9583-y