Abstract
Background
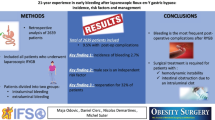
Early postoperative hemorrhage is an infrequent complication of both laparoscopic and open Roux-en-Y gastric bypass (RYGBP). The objective of our study is to review the incidence and management of this complication and identify contributing clinical and technical risk factors.
Methods
Over a 3-year period, 1,025 patients underwent RYGBP at our institution. The medical records of patients who required postoperative blood transfusions were reviewed for clinical presentation, diagnostic evaluation and management. These patients were matched for surgical approach (open vs. laparoscopic) in a 1:3 ratio and compared to a random group of patients who underwent RYGBP during the same time period.
Results
Thirty-three patients (3.2%) were diagnosed with postoperative hemorrhage, 17 (51.5%) of which were intraluminal. The incidence of hemorrhage was higher in the laparoscopic group (5.1% vs. 2.4%, p = 0.02). Comparing bleeders to nonbleeders, the average BMI, gender distribution, gastro-jejunostomy anastomotic technique (stapled vs. hand sewn) and the postoperative administration of ketorolac were not significantly different. The bleeding group was older (47.5 vs. 42.8, p = 0.02), had a longer hospital stay (4.9 vs. 3 days, p = 0.0001) and was more likely to have received low molecular weight heparin (LMWH) preoperatively (p = 0.03). Hemorrhage occurred earlier (13.8 vs. 25.9 h, p = 0.039) and was more severe (4.1 vs. 2.3 transfused blood units, p = 0.007) in the patients who required surgical reexploration (n = 9).
Conclusions
A laparoscopic approach and the preoperative administration of LMWH may increase the incidence of early hemorrhage after RYGBP. This complication frequently requires surgical reexploration and significantly prolongs the hospital stay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric bypass remains one of the main therapeutic options for morbid obesity. Among the potential complications of Roux-en-Y gastric bypass (RYGBP), early hemorrhage is relatively uncommon, with an incidence ranging from 0.6% to 4.4% [1–3]. Early hemorrhage usually occurs from the staple lines (gastro-jejunostomy, jejuno-jejunostomy, gastric pouch or gastric remnant staple lines), and could be intraluminal (gastrointestinal) or extraluminal (intraperitoneal). There have even been reports of early small bowel obstruction due to intraluminal hematomas [4]. The inaccessibility of the gastric remnant and the risks of early postoperative endoscopy make the diagnosis and treatment of early hemorrhage after RYGBP a challenging task.
Technical factors (laparoscopic vs. open approach, gastro-jejunostomy anastomosis technique) may affect the incidence of this complication. Certain studies have even reported a slightly higher early bleeding rate after a laparoscopic approach [2, 3]. In addition to the technical factors, the perioperative administration of certain drugs such as heparin products or ketorolac tromethamine (Toradol®, Roche Laboratories, Switzerland) may potentially influence the occurrence of this complication. In fact, although ketorolac has been found to be beneficial in the management of perioperative analgesia after gastric bypass surgery [5–8], some concerns have been raised in the surgical literature regarding its potential to increase the incidence of postoperative bleeding [9–11].
The objective of the study is to review the incidence and management of early postoperative hemorrhage after RYGBP at our institution and identify possible clinical and technical risk factors that may be associated with this complication.
Materials and Methods
We conducted a retrospective study in our 511-bed teaching hospital, designated as a Center of Excellence for obesity surgery by the American Society for Metabolic and Bariatric Surgery (ASMBS).
We reviewed all patients who underwent open or laparoscopic RYGBP over a 3-year period (January 1, 2003–December 31, 2005). RYGBP was performed by five different surgeons, one of which performed open procedures only. In all patients, a fully transected 30 cc gastric pouch was created on the lesser curvature using linear staplers (Ethicon Endo-Surgery, Cincinnati, OH, USA). Gastro-jejunostomies (GJ) were fashioned in an antecolic manner in the laparoscopic cases only, and every patient had a 10 mm flat Jackson-Pratt drain placed in the abdominal cavity to aid in the management of potential anastomotic leaks. No bovine pericardial staple-line reinforcements were used at our institution during the study period. The pharmacologic DVT prophylaxis protocol varied among the surgeons but consisted of one of the following: (1) 5,000 IU of subcutaneous heparin given 1 h before surgery followed by either 5,000 IU of heparin every 8 h or low molecular weight heparin (LMWH, enoxaparin, Lovenox®, Aventis, France) every 12 h, or (2) LMWH given 1 h before surgery and then twice daily. The individual dose of LMWH was 30 mg if given preoperatively, and varied in the postoperative period between 30 and 60 mg, depending on the BMI of the patient.
Patients who required blood transfusions (bleeding group) were evaluated for clinical presentation, diagnostic work-up and management. These patients were matched for surgical approach (open vs. laparoscopic) in a 1:3 ratio with a random group of patients who underwent RYGBP during the same time period without requiring any blood product transfusions (nonbleeding group). The two groups were assessed for the following parameters: demographics (age, gender, BMI), GJ anastomosis technique, (circular stapler vs. linear stapler vs. hand sewn anastomosis), perioperative utilization of anticoagulation prophylaxis medications (heparin or LMWH) and postoperative administration of ketorolac. The study was approved by the hospital’s Institutional Review Board. The Electronic Medical Records and the chart review were performed by one author only.
Parametric (Fisher’s exact, chi-square) and nonparametric (Wilcoxon Rank Sum) tests were used as appropriate; logistic regression analysis was used to estimate Odds Ratio. A type I error (alpha level) of 0.05 was considered significant. Numerical data are presented as mean ± standard deviation.
Results
A total of 1025 patients underwent RYGBP during the study period (678 open, 347 laparoscopic with 11 conversions). The average BMI of these patients was 51.5 ± 9.3, with a median BMI of 50 (range 35–90). Thirty-three patients (3.2%) were diagnosed with early postoperative hemorrhage. Considering the open group to include both patients who underwent an open RYGBP and those who were converted from a laparoscopic to an open approach, there was a significant difference in the incidence of bleeding among patients who underwent an open vs. a laparoscopic approach (16/689 = 2.4% vs. 17/336 = 5.1%, p = 0.02). The incidence of bleeding was not different among obese (35 ≤ BMI < 50) and superobese (BMI ≥ 50) patients (3.7% vs. 2.8%, p = 0.48).
Comparing bleeders and nonbleeders, the average BMI (range 37–74 and 38–75, respectively), gender distribution, gastro-jejunostomy anastomotic technique (linear vs. circular and handsewn p = 0.23; circular vs. linear and handsewn p = 0.18, handsewn vs. stapled p = 1.0) and the postoperative administration of ketorolac were not significantly different. The bleeding patients were older (47.5 ± 8.7 vs. 42.8 ± 10.8, p = 0.02) and had a longer hospital stay (4.9 ± 2.3 vs. 3 ± 1.1 days, p < 0.0001). They were 3.5 times more likely to have been over 45 years of age (95% CI 1.2 to 9.8) and 2.6 times more likely to have received LMWH preoperatively in comparison to subcutaneous heparin (95% CI 1.117 to 5.993; p = 0.03). In the bleeding group, a disproportionately larger number of patients who required blood transfusions postoperatively did not receive any single dose of pharmacologic DVT prophylaxis (LMWH or subcutaneous heparin; Table 1). The decision to hold anticoagulation was based upon concerns of intraoperative or immediate postoperative bleeding.
The most common presentation of early hemorrhage in our series consisted of the following triad: hematocrit drop, tachycardia and oliguria. Among the bleeders, 51% of the patients (n = 17) had evidence of intraluminal hemorrhage, and 49% (n = 16) intraperitoneal. The median time to presentation of bleeding was 20 h, with a mean time of 22.6 ± 14.7 h. Seven patients underwent eight diagnostic studies, including three EGDs (one of which found active bleeding at the gastro-jejunostomy), two tagged red blood cell scans (both were negative), and three CT scans of the abdomen (one documented a port site hernia and two revealed intraabdominal hematomas). Hemorrhage occurred earlier and was more severe in the patients who required surgical reexploration (N = 9, 27%; Table 2). The findings in the operating room included the following: active bleeding in four patients (three at the gastro-jejunostomy, one from the gastric remnant), four intraabdominal hematomas without active bleeding, and one incarcerated port site hernia with an associated abdominal wall hematoma.
Discussion
This study represents one of the largest series to describe early hemorrhage after RYGBP and the first comparative study of this size. We found an incidence of bleeding at our institution comparable to what is reported in the bariatric literature, particularly a higher incidence of bleeding after a laparoscopic approach [2, 3, 12, 13]. The higher incidence of this complication in laparoscopic cases has been attributed by some authors to the absence of oversewing of the staple lies and/or a more aggressive use of anti-thrombotics for DVT prophylaxis in the minimally invasive cases [14]. Our study however demonstrated an independent correlation between the preoperative administration of LMWH and the incidence of bleeding, since the control patients were matched for the surgical approach. We did not match the patients for their body mass index since there was no difference in the average BMI among the two groups, and no difference in the incidence of bleeding among obese and superobese patients. Although we found a significant decrease in the postoperative utilization of heparin products in the bleeding group, this was due to the fact that antithrombotics were discontinued in view of the hematocrit drop in this patient population. It is sometimes difficult to weight the risks of stopping anticoagulation in the face of postoperative hemorrhage with the risk of significant morbidity and mortality from venous thromboembolism. An inferior vena cava filter is an option in patients who bleed postoperatively and are at high risk from thromboembolism. A limitation of our study is the variation in the administrated dose of LMWH among the different surgeons. It is noteworthy to mention, however, that there still is no consensus on the appropriate dosage of LMWH in the morbidly obese patient. In a retrospective nonrandomized series by Paige et al. [15], the authors did not find any correlation between low molecular weight heparin, anti-Xa levels and the risk of bleeding.
In addition to heparin products, we sought to elucidate whether administering ketorolac could influence the incidence of bleeding. Ketorolac is an injectable nonsteroidal antiinflammatory drug that is often used as a transitional short-term analgesic to treat moderate pain and to decrease opioid use. There is a paucity of literature documenting the safety of using ketorolac after surgery, and the manufacturer even cautions against its use in patients who have a high risk of postoperative bleeding. However, we did not find in our series any significant correlation between the use of ketorolac and perioperative bleeding.
In addition to the surgical approach, this study has the advantage of including a variety of stapling techniques according to each surgeon’s preference. We did not find any impact of the type of stapler used, whether linear or circular. Interestingly though, we found that the patients who presented with early hemorrhage in our series were older. Although this has not been reported in the bariatric literature before, advanced age is a known risk factor for early bleeding after other surgical procedures, such as coronary artery bypass grafting [16]. Nevertheless, we cannot ascertain if age is an independent risk factor for bleeding in bariatric patients, as our finding could be due to a more diligent use of heparin products in the older population to prevent venous thromboembolism, or any other confounding variable that we did not account for.
Concerning the management of early hemorrhage after RYGBP, most authors agree that diagnostic studies are usually unnecessary, since the source of bleeding is almost always the staple lines [2, 14]. Only one imaging study in our series did modify the management of postoperative hemorrhage, and expedited surgical reintervention (a CT scan of the abdomen documenting an incarcerated, hemorrhaging port site hernia). Although we did not utilize any other therapeutic alternatives to surgery in our series, endoscopy has been shown to control acute bleeding from the gastro-jejunal staple line [14]. Furthermore, endoscopic management of bleeding from the jejuno-jejunostomy has also been described [17]. Surgical reexploration should still remain mandatory in cases of hemodynamic instability and/or failure of conservative management. Regarding the prevention of this complication, some published data describe the usage of bioabsorbable staple lines reinforcements or fibrin sealant to decrease its incidence, but these data lack power and convincing evidence to support their usage on a large scale [18, 19].
Another limitation of our study is that it is retrospective. We have introduced a selection bias by only including patients who required blood transfusions in the postoperative hemorrhage group and potentially excluding patients who may have bled significantly without requiring blood transfusions, based on the surgeons’ threshold for transfusions.
In conclusion, we found that advanced age, a laparoscopic approach and the preoperative administration of LMWH could increase the incidence of early hemorrhage after RYGBP. The patients’ BMI, administration of ketorolac and the gastrojejunostomy anastomosis technique did not seem to influence the incidence of this morbid complication, which frequently requires surgical reexploration and significantly prolongs the hospital stay.
References
Podnos YD, Jimenez JC, Wilson SE, et al. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg. 2003;138(9):957–61.
Nguyen NT, Rivers R, Wolfe BM. Early gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2003;13(1):62–5.
Mehran A, Szomstein S, Zundel N, Rosenthal R. Management of acute bleeding after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2003;13(6):842–7.
Awais O, Raftopoulos I, Luketich JD, Courcoulas A. Acute, complete proximal small bowel obstruction after laparoscopic gastric bypass due to intraluminal blood clot formation. Surg Obes Relat Dis. 2005;1(4):418–22; discussion 422–3.
Madan AK, Ternovits CA, Speck KE, Tichansky DS. Inpatient pain medication requirements after laparoscopic gastric bypass. Obes Surg. 2005;15(6):778–81.
Pellis T, Leykin Y, Albano G, et al. Perioperative management and monitoring of a super-obese patient. Obes Surg. 2004;14(10):1423–7.
Kamelgard JI, Kim KA, Atlas G. Combined preemptive and preventive analgesia in morbidly obese patients undergoing open gastric bypass: a pilot study. Surg Obes Relat Dis. 2005;1(1):12–6.
Govindarajan R, Ghosh B, Sathyamoorthy MK, et al. Efficacy of ketorolac in lieu of narcotics in the operative management of laparoscopic surgery for morbid obesity. Surg Obes Relat Dis. 2005;1(6):530–5; discussion 535–6.
Vuilleumier H, Halkic N. Ruptured subcapsular hematoma after laparoscopic cholecystectomy attributed to ketorolac-induced coagulopathy. Surg Endosc. 2003;17(4):659.
Erstad BL, Rappaport WD. Subcapsular hematoma after laparoscopic cholecystectomy, associated with ketorolac administration. Pharmacotherapy. 1994;14(5):613–5.
Sharma S, Chang DW, Koutz C, et al. Incidence of hematoma associated with ketorolac after TRAM flap breast reconstruction. Plast Reconstr Surg. 2001;107(2):352–5.
Oliak D, Ballantyne GH, Weber P, et al. Laparoscopic Roux-en-Y gastric bypass: defining the learning curve. Surg Endosc. 2003;17(3):405–8.
Schauer PR, Ikramuddin S, Gourash W, et al. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 2000;232(4):515–29.
Nguyen NT, Longoria M, Chalifoux S, Wilson SE. Gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2004;14(10):1308–12.
Paige JT, Gouda BP, Gaitor-Stampley V, et al. No correlation between anti-factor Xa levels, low-molecular-weight heparin, and bleeding after gastric bypass. Surg Obes Relat Dis. 2007;3(4):469–75.
Karthik S, Grayson AD, McCarron EE, et al. Reexploration for bleeding after coronary artery bypass surgery: risk factors, outcomes, and the effect of time delay. Ann Thorac Surg. 2004;78(2):527–34; discussion 534.
Moretto M, Mottin CC, Padoin AV, et al. Endoscopic management of bleeding after gastric bypass – a therapeutic alternative. Obes Surg. 2004;14(5):706.
Lee MG, Provost DA, Jones DB. Use of fibrin sealant in laparoscopic gastric bypass for the morbidly obese. Obes Surg. 2004;14(10):1321–6.
Miller KA, Pump A. Use of bioabsorbable staple reinforcement material in gastric bypass: a prospective randomized clinical trial. Surg Obes Relat Dis. 2007;3(4):417–21; discussion 422.
Acknowledgments
Authors would like to thank Jessie Moore APRN, John Courtney MBA, Jack Contessa PhD, and Dorota Kiwak (poster design for the New England Surgical Society meeting).
Conflicts of interest
None of the five authors has any conflict of interest, or any disclosure to mention.
Author information
Authors and Affiliations
Corresponding author
Additional information
Oral presentation and 1st prize winner, Bariatric surgery competition, CTACS meeting, November 2006.
Poster presentation at the New England Surgical Society meeting, September 2007.
Rights and permissions
About this article
Cite this article
Bakhos, C., Alkhoury, F., Kyriakides, T. et al. Early Postoperative Hemorrhage After Open and Laparoscopic Roux-En-Y Gastric Bypass. OBES SURG 19, 153–157 (2009). https://doi.org/10.1007/s11695-008-9580-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9580-1