Abstract
Background
Laparoscopic Roux-en-Y gastric bypass (LRYGB) is a common, safe and effective bariatric procedure. Bleeding is a significant source of postoperative morbidity. We aimed to determine the incidence, outcomes, and predictors of postoperative bleeding after LRYGB.
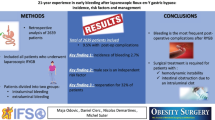
Methods
LRYGB patients included in the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 dataset were identified. Preoperative and intraoperative factors were tested for associations with bleeding using univariable and multivariable logistic regression analysis. Outcomes of length of stay, in-hospital mortality, 30-day mortality, discharge disposition, and 30-day complications among patients with and without clinically significant postoperative bleeding were compared using multivariable regression.
Results
In the 43,280 LRYGB patients included in this analysis, postoperative bleeding occurred in 652 (1.51%) patients. Of these, 165 (25.3%) underwent a re-operation and 97 (14.9%) underwent an unplanned endoscopy for ‘bleeding’. Postoperative bleeding was associated with a longer median postoperative length of stay (4 vs. 2 days), higher in-hospital mortality (1.23 vs. 0.04%), higher 30-day mortality (1.38 vs. 0.15%), discharge to an extended-care facility (3.88 vs. 0.6%), and higher rates of major complications (all P < 0.05). Independent predictors of postoperative bleeding included; a history of renal insufficiency (OR 2.55, 95% CI 1.43–4.52), preoperative therapeutic anticoagulation (OR 2.44, 95% CI 1.69–3.53), and revisional surgery (OR 1.45, 95% CI 1.06–1.97). Intraoperative associated factors included conversions (OR 3.37, 95% CI 1.42–7.97), and drain placement (OR 1.40, 95% CI 1.18–1.67). Robotic approaches resulted in independently lower postoperative bleeding rates (OR 0.50, 95% CI 0.32–0.77).
Conclusions
Postoperative bleeding occurs in 1.5% of patients undergoing a LRYGB and is associated with significantly increased morbidity and mortality. We have identified patient and operative factors that are independently associated with postoperative bleeding.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic Roux-en-Y Gastric Bypass (LRYGB) is a commonly performed weight-loss operation in the United States, with approximately 40,000 cases occurring annually [1, 2]. While often considered the “gold standard” bariatric operation and associated with significant, durable weight loss, it still has appreciable complications. Major complications occur in up to 12.4% of cases and mortality in up to 0.4% [3, 4]. Important early complications include leaks, obstruction, and hemorrhage [3,4,5,6].
Postoperative hemorrhage occurs in roughly 3% of patients and is associated with increases in re-operations, hospital length of stay, and mortality [7, 8]. It is theorized that surgical technique, patient illness severity, and specific preoperative comorbidities play a role in predisposing patients to postoperative hemorrhage. To our knowledge, there has been no comprehensive analysis of these predictors of postoperative bleeding after LRYGB. Since the incidence of postoperative bleeding complications is relatively low, only large multicenter analyses could adequately explore these associations. We aimed to determine the incidence, outcomes and predictors of postoperative bleeding after LRYGB using a large national dataset.
Methods
Data set
We analyzed data from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 Participant Use File (PUF) [9]. The MBSAQIP representing a collaboration between the American College of Surgeons and the American Society for Metabolic and Bariatric Surgery, is the largest bariatric specific clinical dataset in the United States. It contains information on all metabolic and bariatric procedures and interventions performed by participating centers. Over 200 variables are collected which include preoperative, intraoperative, and postoperative factors. Outcomes are measured over a 30-day postoperative period. The dataset contains information from over 160,000 patients from > 740 participating centers across the United States.
The MBSAQIP participant user file contains no identifying information on patients, hospitals or health care workers. It is Health Insurance Portability and Accountability Act (HIPAA) compliant and exempt from IRB review. All variables herein are as defined by the publicly available 2015 MBSAQIP PUF Variables and Definition Manual [9].
Patient selection and variables
We selected all patients that underwent a LRYGB (CPT code 43644). Patients at extremes of ages (< 10 or > 80 years), or who underwent mini gastric bypasses, gastric plications and natural orifice operations were excluded. We utilized demographic, preoperative, intraoperative and outcome information. Demographics included age, gender, ethnicity, and biometrics including the preoperative weight and body mass index (BMI). Preoperative variables included history of comorbid conditions, medication history, American Society of Anesthesiologists (ASA) score, information on prior relevant surgeries, and preoperative hematocrit and albumin levels. Intraoperative variables included operating times, approach, assistant level of training, conversions, and concurrent procedures (liver biopsy, hiatal hernia repair, laparoscopic cholecystectomy, and band removal). Outcomes included postoperative length of stay, in-hospital mortality, 30-day mortality, 30-day complications, discharge disposition, 30-day readmissions, and any unplanned procedure or intervention.
Postoperative bleeding (POB) was defined as any hemorrhagic event that required a blood transfusion within 72 h of operation or required a procedural intervention for “bleeding.” For the purposes of analysis, age was stratified by decile. BMI was categorized as < 35, 35–40, 40–50, 50–70, and > 70 kg/m2. Preoperative hematocrit was categorized as < 21, 21–30, 30–36, 36–45, and > 45%. Preoperative albumin was dichotomized by values above or below 3 g/dl.
Analysis
Categorical variables were reported as frequency and proportions. Means with standard deviations (SD) were calculated for continuous variables. Skewed continuous variables such as length of stay were summarized by medians and interquartile ranges. The frequency of patients requiring blood transfusions within 72 h and those requiring an operative, endoscopic or other intervention for ‘bleeding’ were summed to arrive at the frequency and proportion of those that suffered a postoperative bleeding. All preoperative and intraoperative variables were tested for associations with postoperative bleeding using the Chi-square test. Factors significant on univariate analysis and those that were clinically relevant were selected for the multivariable model. The variables ‘previous foregut/bariatric surgery’ was collinear with ‘revisional surgery’ and thus the previous foregut surgery variable was not used in the model. Multivariable logistic regression analysis was used to identify independent factors associated with postoperative bleeding events.
Outcomes of LOS, in-hospital mortality, 30-day mortality, discharge disposition, and 30-day complications were compared for patients that suffered a postoperative bleed (POB) versus those that did not using the chi-square test. Multivariate models were constructed to test for the independent association of POB with outcomes of 30-day mortality, postoperative length of stay, and any complication. Clinically relevant factors and those significant upon univariate analysis with the outcome were included in the final models. Multivariable logistic regression was used for the binary outcomes of mortality and complications while generalized linear modeling with log link was used for the length of postoperative stay outcome variable. All models were tested for fit using the Hosmer–Lemeshow goodness of fit [10]. Significance was determined at a two-sided P-value of 0.05 or less. All analyses were performed using STATA Version 13 (STATACorp, College Station, TX).
Results
A total of 43,280 patients undergoing a LRYGB were included in the analysis. The mean age was 45.4 years (SD ± 12 years). Eighty percent of patients were female and 77% reported being of White ethnicity. The mean BMI was 46.0 kg/m2 (SD ± 8.4 kg/m2). A total of 652 (1.51%) patients suffered a POB. Of these 165 (25.3%) underwent a re-operation and 97 (14.9%) underwent an unplanned endoscopic procedure. Patients received a mean 2.6 units of packed red blood cells (range of 1–13 units). Upon bivariate analysis between patients that did and did not suffer a POB, several significant differences were found. These are summarized in Table 1. Patients undergoing revisional surgery had a POB rate of 2.4%.
After multivariable logistic regression (Table 2) independent factors associated with postoperative bleeding included: history of deep vein thrombosis (OR 1.62, 95% CI 1.02–2.59), history of renal failure (OR 2.55, 95% CI 1.43–4.52), preoperative therapeutic anticoagulation (OR 2.44, 95% CI 1.69–3.53), conversion to an open procedure (OR 3.37, 95% CI 1.42–7.97), drain placement (OR 1.40, 95% CI 1.18–1.67), and revisional surgery (OR 1.45, 95% CI 1.06–1.97). If an attending non-bariatric surgeon was assisting in the procedure, the likelihood of POB was 40% lower than a resident assistant (OR 0.60, 95% CI 0.38–0.97). A robotic approach was also associated with a 50% lower likelihood of having a postoperative bleed (OR 0.50, 95% CI 0.32–0.77). BMI, age, sex, prolonged operations, concurrent procedures, and lower serum albumin levels < 3.0 g/dl were not independently associated with POB. The model was also adjusted for preoperative hematocrit levels and this factor was significant in the final model. Since our definition of POB is based on interventions performed for bleeding (transfusions and procedures), the association of hematocrit with bleeding most likely represents a threshold effect. Patients with lower hematocrit levels are more likely to reach a transfusion and intervention threshold after bleeding than patients with a higher preoperative hematocrit level.
Patients that suffered a POB were more likely to have adverse outcomes. Postoperative bleeding was associated with a longer median postoperative length of stay (4 vs. 2 days), higher in-hospital mortality (1.23 vs. 0.04%), higher 30-day mortality (1.38 vs. 0.15%), discharge to an extended-care facility (3.88 vs. 0.62%), and higher rates of major complications including acute renal failure (2.45 vs. 0.12%), cardiac arrest (1.38 vs. 0.06%), myocardial infraction (1.07 vs. 0.04%), pneumonia (1.84 vs. 0.41%), and pulmonary embolism (1.53 vs. 0.15%) (all P < 0.05) (Table 3). Upon multivariable analysis, significant independent associations were found between patients that suffered a postoperative bleed and postoperative complications (OR 5.4, 95% CI 4.26–6.86), length of stay (OR 2.3, 95% CI 2.24–2.42), and 30-day mortality (6.2, 95% CI 2.78–13.84). Subset analyses excluding patients with revisional surgery yielded similar results. The overall rate of POB was 1.42% with similarly adverse outcomes.
Discussion
At MBSAQIP participating centers, postoperative bleeding occurred in 1.5% of patients undergoing LRYGB and was associated with significantly increased morbidity and mortality. Postoperative bleeding was associated with a longer length of stay, higher in-hospital mortality, higher 30-day mortality, discharge to an extended-care facility, and higher rates of major complications. Furthermore, we found several independent factors associated with postoperative bleeding, including history of renal insufficiency, preoperative therapeutic anticoagulation, revisional surgery, conversion operations, and certain intraoperative factors. The 1.5% incidence of postoperative bleed is consistent with previous studies. Fesco et al. found a bleeding rate of 2.16% in their retrospective study of all bariatric operations at their institution [11]. Rondelli et al. found a bleeding rate of 1.0% within 30 days of undergoing LRYGB [12], similarly Heneghan et al. found a rate of 0.94% within 30 days of undergoing either laparoscopic or open RYGB [13].
Prior reports have demonstrated postoperative complications to have adverse sequelae for both the patient and the hospital. Fesco et al. found patients who developed postoperative bleeding stayed almost three times longer than the patients who had an uncomplicated postoperative course [11]. Dick et al. found a similar increase in mean length of stay in patients who developed postoperative bleeding, increased from a mean of 3 days to 4.8 [14]. Heneghan et al. also found that discharge was delayed more than 4 days in 87% of patients who experienced an early postoperative bleed and a mean length of hospital stay 11.43 days [13]. Similar to our findings, they found significant morbidity as a consequence of bleeding in 35% of patients, including respiratory complications, sepsis or infected hematomas, and systemic inflammatory response syndrome-induced multiple organ failure [13]. In a large study examining the etiologies and risk factors for readmission following bariatric surgery, Garg et al. found that readmission was highly associated with any in-hospital complication [15]. Specifically, 40.4% of patients with readmissions had experienced a complication at the initial hospital stay and 6.6% of all readmissions were due to hemorrhage. Moreover, patients with bleeding in the early postoperative period were almost three times more likely to be readmitted (1.3 vs. 3%, P < 0.001). Our results also demonstrate POB to be associated with a myriad of adverse outcomes. These are summarized in Table 3. Unlike prior smaller studies, we were able to assess several specific complications due to the large number of patients available in the dataset.
Not surprisingly, postoperative complications consume significant health care resources leading to increased cost of patient care. Vonlanthen et al. found that complications classified as grade IIIb (requiring surgical, endoscopic, or radiological intervention under general anesthesia) or higher led to a significant increase in costs compared to procedures without postoperative complications [16]. Specifically, the mean cost of RYGB in patients with any complication is increased by $9000 compared to patients without complications and by about $50,000 for more severe complications. Furthermore, the mean cost of a postoperative bleeding complication ranged from $7995 for grade I complications to $98,227 for grade IIIB and $149,582 for grade IV complications [16]. In our analysis, of the patients that bled, 25.3% underwent a re-operation and 14.9% underwent an unplanned endoscopy. Additionally, Ibrahim et al. in a study exploring the relationship of outcomes and cost after bariatric surgery found a strong correlation between hospitals identified as high-quality (having the lowest rates of serious complications), and lower Medicare payments [17]. They concluded that reducing complication rates following bariatric surgery may result in significant savings for payers and the healthcare system overall.
We found several risk factors for postoperative bleeding. Some of these factors, such as therapeutic anticoagulation, are modifiable. Other risk factors, such as renal insufficiency, may not be modifiable but patients may be medically optimized pre-operatively to potentially reduce the risk of postoperative bleeding. Chronic anticoagulation is a well-known risk factor for postoperative bleeding with any elective surgical procedure. A recent study on bariatric surgery patients on chronic anticoagulation showed that 12% of patients who underwent LRYGB developed early postoperative bleeding [18]. Furthermore, 12% of patients undergoing LRYGB required readmission within 30 days of surgery, approximately half of them admitted with postoperative bleeding [18]. Sharma et al. recommended careful surgical technique and tissue handling during surgery in patients on chronic anticoagulation, in addition to paying close attention to postoperative anticoagulation protocols to minimize bleeding [18].
While our study is not designed to assess it, other researchers have explored factors that could prevent postoperative bleeding after LRYGB. Silecchia et al. found that certain patient-related factors, such as liver disease, coagulopathy, hypertension, super-obesity, and revisional surgery, increase the risk of bleeding following LRGYB, while surgeon-related factors like no staple-line reinforcement and mechanical circular anastomosis also increased the bleeding risk [19]. The authors recommended the use of either a hand-sewn or linear cutting stapler technique for creation of anastomoses, and the use of staple-line buttress or application of glue to staple lines [19]. Dick et al. also recommend using staple line reinforcement devices to prevent early postoperative GI bleeding [14]. Several small studies have demonstrated a reduction in intraoperative and postoperative staple line bleeding with the use of buttressing [20, 21]. However, cost effectiveness studies of using this approach are still pending. Robotic-assisted RYGB is also associated with a lower incidence of postoperative bleed. The reasons for this finding are unclear and may be attributed to selection bias when choosing patients for robotic approaches, the use of staple line buttressing, and possibly more meticulous dissection and hemostasis with robot assisted surgery. This however warrants further study. Recent studies comparing robot-assisted gastric bypass operations to standard LRYGB have shown the robot to be more resource intensive and possibly associated with worse overall outcomes [22, 23].
Our analysis has several limitations which should be taken in to consideration. This is a retrospective analysis of prospectively collected data and thus we are only able to test variables that were present in the dataset. For example, the dosage and use or venous thromboembolism prophylaxis, or details on intraoperative technique, including management of staple lines, were unavailable for assessment. Cost data were also unavailable. Additionally, our definition of postoperative hemorrhage selects for major or clinically relevant bleeding events, patients with postoperative hemorrhage that did not result in any blood transfusion or intervention would not be identified by our methodology, so it is possible we are underestimating the true rate of postoperative bleeding events. Similarly, the risk factor analysis determines associations with clinically significant hemorrhage that required an intervention and discounts minor bleeding events. Also, we could not account for ‘thresholds’ for transfusion or intervention and these are likely to vary between providers. Since data on facility and surgeons are not available in the PUF, we are unable to account for clustering effects by facility or provider. It is also important to understand that we reveal and association of POB with adverse outcomes and this does not imply a causation. It is possible that high risk patients due to other factors are at a higher risk of morbidity and mortality and also happened to have higher POB rates. However, this is the largest study to date focusing on postoperative bleeding following LRYGB. With 43,280 patients and 652 POB events, we are able to use multivariable analysis to provide for meaningful conclusions.
In this large database study containing information from over 740 centers, the incidence of postoperative bleeding following LRYGB is substantial at 1.5%. It is associated with increased morbidity and mortality which would subsequently lead to higher health care costs. It is essential for providers to prevent early postoperative bleeding by recognizing high risk patients and optimizing them prior to surgery. The use of intraoperative hemostatic techniques to prevent postoperative hemorrhage may be beneficial but is still being studied. We identify several factors associated with bleeding events. Surgeons and policy makers can use these to inform further research or practice.
References
Livingston EH (2010) The incidence of bariatric surgery has plateaued in the U.S. Am J Surg 200:378–385
English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM (2018) American society for metabolic and bariatric surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 14:259–263
Rosenthal RJ, Szomstein S, Kennedy CI, Soto FC, Zundel N (2006) Laparoscopic surgery for morbid obesity: 1,001 consecutive bariatric operations performed at The Bariatric Institute, Cleveland Clinic Florida. Obes Surg 16:119–124
Zellmer JD, Mathiason MA, Kallies KJ, Kothari SN (2014) Is laparoscopic sleeve gastrectomy a lower risk bariatric procedure compared with laparoscopic Roux-en-Y gastric bypass? A meta-analysis. Am J Surg 208:903–910 (discussion 909–910)
Weiner RA, El-Sayes IA, Theodoridou S, Weiner SR, Scheffel O (2013) Early post-operative complications: incidence, management, and impact on length of hospital stay. A retrospective comparison between laparoscopic gastric bypass and sleeve gastrectomy. Obes Surg 23:2004–2012
Kligman MD, Thomas C, Saxe J (2003) Effect of the learning curve on the early outcomes of laparoscopic Roux-en-Y gastric bypass. Am Surg 69:304–309 (discussion 309–310)
Rabl C, Peeva S, Prado K, James AW, Rogers SJ, Posselt A, Campos GM (2011) Early and late abdominal bleeding after Roux-en-Y gastric bypass: sources and tailored therapeutic strategies. Obes Surg 21:413–420
Spaw AT, Husted JD (2005) Bleeding after laparoscopic gastric bypass: case report and literature review. Surg Obes Relat Dis 1:99–103
MBSAQIP MBSAQIP Participant Use Data File (PUF)
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–980
Fecso AB, Samuel T, Elnahas A, Sockalingam S, Jackson T, Quereshy F, Okrainec A (2018) Clinical indicators of postoperative bleeding in Bariatric Surgery. Surg Laparosc Endosc Percutan Tech 28:52–55
Rondelli F, Bugiantella W, Vedovati MC, Mariani E, Balzarotti Canger RC, Federici S, Guerra A, Boni M (2017) Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy: a retrospective multicenter comparison between early and long-term post-operative outcomes. Int J Surg 37:36–41
Heneghan HM, Meron-Eldar S, Yenumula P, Rogula T, Brethauer SA, Schauer PR (2012) Incidence and management of bleeding complications after gastric bypass surgery in the morbidly obese. Surg Obes Relat Dis 8:729–735
Dick A, Byrne TK, Baker M, Budak A, Morgan K (2010) Gastrointestinal bleeding after gastric bypass surgery: nuisance or catastrophe? Surg Obes Relat Dis 6:643–647
Garg T, Rosas U, Rivas H, Azagury D, Morton JM (2016) National prevalence, causes, and risk factors for bariatric surgery readmissions. Am J Surg 212:76–80
Vonlanthen R, Slankamenac K, Breitenstein S, Puhan MA, Muller MK, Hahnloser D, Hauri D, Graf R, Clavien PA (2011) The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg 254:907–913
Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB (2017) Hospital quality and medicare expenditures for bariatric surgery in the United States. Ann Surg 266:105–110
Sharma G, Hanipah ZN, Aminian A, Punchai S, Bucak E, Schauer PR, Brethauer SA (2018) Bariatric surgery in patients on chronic anticoagulation therapy. Obes Surg. https://doi.org/10.1007/s11695-018-3120-4
Silecchia G, Iossa A (2018) Complications of staple line and anastomoses following laparoscopic bariatric surgery. Ann Gastroenterol 31:56–64
Nguyen NT, Longoria M, Welbourne S, Sabio A, Wilson SE (2005) Glycolide copolymer staple-line reinforcement reduces staple site bleeding during laparoscopic gastric bypass: a prospective randomized trial. Arch Surg 140:773–778
Shikora SA, Kim JJ, Tarnoff ME (2003) Reinforcing gastric staple-lines with bovine pericardial strips may decrease the likelihood of gastric leak after laparoscopic Roux-en-Y gastric bypass. Obes Surg 13:37–44
Sharma G, Strong AT, Tu C, Brethauer SA, Schauer PR, Aminian A (2018) Robotic platform for gastric bypass is associated with more resource utilization: an analysis of MBSAQIP dataset. Surg Obes Relat Dis 14:304–310
Celio AC, Kasten KR, Schwoerer A, Pories WJ, Spaniolas K (2017) Perioperative safety of laparoscopic versus robotic gastric bypass: a propensity matched analysis of early experience. Surg Obes Relat Dis 13:1847–1852
Acknowledgements
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) the hospitals participating in the MBSAQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Syed Nabeel Zafar, Jessica Felton, Kaylie Miller, Eric S. Wise, and Mark Kligman have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Zafar, S.N., Miller, K., Felton, J. et al. Postoperative bleeding after laparoscopic Roux en Y gastric bypass: predictors and consequences. Surg Endosc 33, 272–280 (2019). https://doi.org/10.1007/s00464-018-6365-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6365-z