Abstract
Major Depressive Disorder (MDD) is recognized to be heterogeneous in terms of brain structure abnormality findings across studies, which might reflect previously unstudied traits that confer variability to neuroimaging measurements. The purpose of this study was to examine the relationships between different types of trait impulsivity and MDD diagnosis on adolescent brain structure. We predicted that adolescents with depression who were high on trait impulsivity would have more abnormal cortical structure than depressed patients or non-MDD who were low on impulsivity. We recruited 58 subjects, including 29 adolescents (ages 12–19) with a primary DSM-IV diagnosis of MDD and a history of suicide attempt and 29 demographically-matched healthy control participants. Our GLM-based analyses sought to describe differences in the linear relationships between cortical thickness and impulsivity trait levels. As hypothesized, we found significant moderation effects in rostral middle frontal gyrus and right paracentral lobule cortical thickness for different subscales of the Barratt Impulsiveness Scale. However, although these brain-behavior relationships differed between diagnostic study groups, they were not simple additive effects as we had predicted. For the middle frontal gyrus, non-MDD participants showed a strong positive association between cortical thickness and BIS-11 Motor scores, while MDD-diagnosed participants showed a negative association. For Non-Planning Impulsiveness, paracentral lobule cortical thickness was observed with greater impulsivity in MDD, but no association was found for controls. In conclusion, the findings confirm that dimensions of impulsivity have discrete neural correlates, and show that relationships between impulsivity and brain structure are expressed differently in adolescents with MDD compared to non-MDD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Major Depressive Disorder (MDD) is a disabling condition characterized by mood impairment, cognitive and social dysfunction, and poor quality of life (Kessler et al. 2003). The heterogenous symptom presentation of MDD has been linked to dysfunction in several brain systems, most notably regions in the lateral and medial surface of the frontal lobes, parts of temporal lobes, and several subcortical structures (Abe et al. 2010; Fallucca et al. 2011). In MDD-diagnosed children and adolescents, there are brain volume abnormalities in several frontal lobe regions, including lateral prefrontal, orbitofrontal and anterior cingulate cortex, as well as in medial temporal lobe structures and striatum (Hulvershorn et al. 2011). Many studies have sought to characterize the relationship between such structural abnormalities and depression symptomatology severity (Hulvershorn et al. 2011; Marrus et al. 2015), associated cognitive dysfunction (Nakano et al. 2014), or similarly informative biomarkers of the disorder (Papmeyer et al. 2015). However, there has been notable inconsistency in brain volume findings in MDD at all ages, with studies of the same region alternatively often finding greater, lesser, or no difference in volumes of the same regions across different studies.
Some researchers have focused on specific aspects of abnormal brain structure in hopes of more clearly disentangling the complex relationships between symptom presentation and neuroimaging-measured abnormalities. One methodological focus involves surface-based measurements of cortical thickness and surface area. These two indices contribute to volumetric measurements in different ways. Analysis of regional cortical thickness and surface area are increasingly being viewed as an important means for understanding the relationship among genetic influences, brain structure, and brain function in psychiatric disorders (Winkler et al. 2010). There are relatively few cortical thickness studies of pediatric MDD. Early onset MDD affects the trajectory of cortical maturation (Luby et al. 2016) and early life cortical thickness abnormalities are an MDD risk factor (Papmeyer et al. 2015; Peterson et al. 2009) that predicts MDD onset (Foland-Ross et al. 2015a, b) or MDD-associated problems in emotional or social functioning (Holmes et al. 2012). However, both pediatric and adult MDD cortical thickness studies (van Eijndhoven et al. 2013) are inconsistent with regard to which specific brain regions are abnormal, or even whether or not those abnormalities involve greater or lesser brain structure in MDD. In younger MDD-diagnosed children, studies typically found reduced prefrontal cortical thickness children (Marrus et al. 2015; Fallucca et al. 2011; Pannekoek et al. 2014). In contrast, studies of slightly older pediatric MDD-diagnosed groups have found regions with greater prefrontal cortical thickness (Reynolds et al. 2014; Ducharme et al. 2014).
Such inconsistencies across studies could reflect the systematic impact of various unexamined sampling characteristics. A useful strategy to begin disentangling such influences is to focus on specific MDD subgroups to determine the extent to which cortical thickness differs along a particular dimension of neurobiologically-linked behavior. One particularly important problem relevant to MDD is impulsivity. However, study of impulsivity-related neurobiological abnormalities is not straightforward. Impulsivity is conceptualized as a collection of several different stable, traitlike dimensions of behavior (Bari and Robbins 2013). Two of the most studied constructs are “rash impulsivity” (usually conceptualized as failures of control over cognition or motor behavior) and “reward sensitivity” (heightened responsiveness to rewarding or punishing influences). The former has been linked to dorsal striatum and its neural network connections with different prefrontal cortex regions (Leshem and Glicksohn 2012), while the latter is associated with the function of ventral striatum, amygdala and inter-connected cortical regions (Dawe et al. 2004; Dawe and Loxton 2004; Stephens et al. 2010).
These two forms of impulsivity are relevant to MDD, though perhaps in different ways. First, there is an extensive literature conceptualizing reward sensitivity-related neurobiological abnormalities as liabilities for depression (Luking et al. 2016; Russo and Nestler 2013; Telzer 2016), with evidence that different theoretical aspects of reward sensitivity predict mood disorder symptoms and severity (Gruber et al. 2013; Van Meter and Youngstrom 2015). In other words, reward sensitivity might be an endophenotype of the MDD diagnosis itself, i.e., something present in varying degrees in most but perhaps not all MDD-diagnosed patients. In contrast, despite some meta-analytic evidence for an association between rash impulsivity and the MDD diagnosis (Saddichha and Scheutz 2014), rash impulsivity is not often considered important to neurobiological models of depression. However, it is a leading risk factor for self-harm for the most clinically severe MDD-diagnosed patients. In a review of 90 studies, Brezo and colleagues concluded elevated levels of many different types of impulsive personality features could be found in persons from diverse backgrounds who attempted suicide (Brezo et al. 2006). Suicide is highly prevalent in adolescents with MDD (Perroud et al. 2011; Sahoo Saddichha and Scheutz 2014) and is particularly problematic when self-harm is impulsive or unpredictable. Impulsive personality traits have been found to be one of the important predictors of high-risk suicidal behavior, contributing to both high mortality and disability of children and adolescents with MDD (Beghi et al. 2013; Brezo et al. 2006; Giegling et al. 2009; Gvion and Apter 2011). In sum, prior research suggests that both of these distinct impulsivity traits are relevant to MDD and/or impulsive suicide. Although it is logical to expect both traits to be strongly expressed in clinically-severe MDD, there presently is no clear understanding of how these factors might relate to brain structure abnormalities found in such clinical samples.
Emerging research in healthy, non-clinical populations has found both rash impulsivity and reward sensitivity traits have unique associations with individual differences in cortical thickness or surface area (Schilling et al. 2013, 2012; Kaag et al. 2014; Churchwell and Yurgelun-Todd 2013; Bernhardt et al. 2014; Drobetz et al. 2014). No study has examined the link between cortical thickness or surface area and traits of rash impulsivity or reward sensitivity in suicidally-depressed adolescents. The purpose of this study was to examine the interaction of MDD diagnosis and trait impulsivity levels in hopes of providing insight into abnormal neurobiological processes that underlie increased high risk MDD behavior. We predicted that adolescents with depression who were high on trait impulsivity would have more abnormal cortical structure than depressed patients or non-MDD who were low on impulsivity. Because prior studies have found rash impulsiveness predicted greater cortical thickness and surface area in insula and lower thickness in left superior and mid-lateral, and orbital prefrontal regions (Schilling et al. 2013, 2012) in non-clinical adolescents and adults (Kaag et al. 2014; Churchwell and Yurgelun-Todd 2013), we predicted that any MDD vs non-MDD group differences in the relationship between cortical structure and impulsivity would be found these regions. Fewer studies have examined the brain structure correlates of reward sensitivity or comparable reward-related traits, but some evidence has been reported that points to greater surface area in lateral prefrontal and anterior cingulate and lesser cortical thickness in anterior cingulate predicting preference for immediate rewards (Bernhardt et al. 2014; Drobetz et al. 2014). Collectively, cingulate, orbitofrontal cortex, and lateral prefrontal cortex are brain regions most consistently linked to different types of impulsivity in non-MDD groups. These are regions that have been particularly variable across different prior studies of brain structure in MDD. Moreover, we predicted these differences would generally be additive. In other words, any brain region implicated in both trait impulsivity and MDD would show the greatest cortical thickness deficits.
Methods
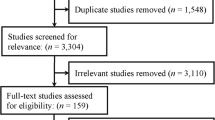
Participants
A total of 58 adolescents were recruited for the study. Participants included 29 adolescents (ages 12–19) with a primary DSM-IV diagnosis of MDD and a history of suicide attempt. MDD subjects were referred by physicians at The Institute of Living and were obtained through community via word of mouth, internet and newspaper advertisements. Exclusion criteria for patients in the study included: head injury sufficient to have caused >30 min lost consciousness; past or current central nervous system disease (e.g. stroke, MS, epilepsy or any repeated seizure history, tumor) or brain lesion identified on structural MR scan; Axis I DSM-IV lifetime history of psychotic disorder, Tourette’s disorder, Pervasive Developmental Disorder (e.g., Autistic disorder, PDD NOS, etc.); current alcohol or substance dependence; hypertension or juvenile-onset diabetes (e.g., current treatment with antihypertensives or insulin); current pregnancy as confirmed by urinalysis; IQ estimate < 80; left handedness; previous/ongoing ECT; previous failed clinical trial of any antidepressant medication; report of psychotic illness in first degree relative. Potential participants also were excluded if they were claustrophobic or if they had metal in their body that were interfere with scanning or pose a safety risk. At the time of the MRI scan, 14 of 29 MDD participants were pharmacological treatment-naïve. The others were receiving SSRI treatment, including 4 patients taking Prozac (10–80 mg), 6 patients taking Zoloft (25–100 mg), 5 Celexa (20–40 mg), 5 Lexapro (10–20 mg), 1 Wellbutrin 100 mg. Four adolescents had a history of inpatient hospitalizations.
We also recruited 29 demographically-matched healthy control participants using community advertisements. Control and experimental subgroup participants did not significantly differ by sex, race, or IQ. All participants (and a parent/legal guardian if under age 18) provided written informed consent prior to the start of the study in accordance with the procedures approved by the Institutional Review Board at Hartford Hospital.
Clinical characterization
All participants were evaluated using The KSADS-PL semi-structured clinical interview (Kaufman et al. 1997) to confirm MDD diagnoses and identify any psychiatric comorbidities (patients) or to confirm absence of DSM-IV disorders (controls). The majority of the MDD study group (17 of 29, or 59 %) had a comorbid psychiatric disorder, mostly anxiety (i.e., PTSD, Social Phobia, Panic Disorder, or Generalized Anxiety Disorder). However, none of the MDD patients currently met criteria for substance dependence. Clinical severity was further quantified using the Beck Depression Inventory II (BDI-II; (Beck et al. 1988)), the Multidimensional Anxiety Scale for Children (MASC; (March et al. 1997)), the Reynolds’ Suicidal Ideation Questionnaire (SIQ and SIQ-JR depending on age; (Reynolds et al. 2014), and Suicide Intent Scale SIS; (Beck et al. 1974).
We used two personality questionnaires to quantify impulsivity. First, we used the Barratt Impulsivity Scale (Patton et al. 1995), which has been widely-used in impulsivity research for last 50 years. Impulsivity is differentiated on the BIS-11 by three subscales. The Motor scale comprises items that reflect acting without thinking. The Non-Planning scale measures an orientation focused on the immediate present that fails to consider future effects. The Attentional scale includes items measuring poor concentration/attentiveness with those reflecting cognitive instability. To measure sensitivity to reward, we used Torrubia et al.’s Sensitivity to Reward Sensitivity to Punishment questionnaire SPSRQ; (Torrubia et al. 2001). This instrument quantifies whether a person is highly motivated by opportunities to receive rewards, or alternatively to avoid punishment. Because the SPSRQ made Sensitivity to Punishment scores readily available, these data were included in study analyses as well for exploration.
Table 1 describes demographic, IQ, and impulsivity trait scores for the study groups. MDD and non-MDD study groups did not differ by age, sex or IQ when tested by two-sample t or chi-square tests. As planned, MDD participants had higher depression scores. Anxiety scores also were elevated as is commonly found in a MDD samples (Cummings et al. 2014). Also, trait impulsivity measures were higher in the MDD group. These group differences in BIS-11 and SPSRQ scores were similar to previously published studies (Piko and Pinczés 2014), mitigating the possibility that MDD self-report of impulsivity might have been inflated due to negative self-perception in the MDD group (Brewin et al. 1992). Because a large proportion of the MDD participants were taking antidepressant medications at the time of the study, medicated MDD characteristics were compared to unmedicated MDD participants. There were no significant demographic or impulsivity trait differences between medication-defined subgroups.
Structural MRI
High resolution, isotropic T1-weighted 3D MPRAGE images were acquired from all participants to confirm normal gross brain structure and rule out pathology using a Siemens 3 T Allegra MRI machine at the Olin Neuropsychiatry Research Center at The Institute of Living/Hartford Hospital (TR/TE/TI = 2300/2.74/900 ms, flip angle = 8°, FOV = 176 × 256 mm, matrix = 176 × 256 × 176, voxel size = 1 × 1 × 1 mm, pixel bandwidth = 190 Hz; 7:09 min).
Cortical thickness analysis
We prepared brain structure images for cortical reconstruction by correction of the estimated MRI bias-field using SPM software (http://www.fil.ion.ucl.ac.uk/), followed by noise reduction using FSL SUSAN filtering software (http://www.fmrib.ox.ac.uk/). We then performed anatomical reconstruction of the cortical surfaces using the FreeSurfer image analysis suite (v5.0; http://surfer.nmr.mgh.harvard.edu/). FreeSurfer surface-based cortical reconstruction and analysis has been described previously (Dale et al. 1999; Fischl et al. 1999). The reconstruction estimated the white surface (comprised of the gray/white matter interface) and the pial surface (comprised of the gray matter/cerebrospinal fluid interface) via two-dimensional mesh of triangular elements comprised of >100,000 vertices per hemisphere. The estimated white and pial surfaces were manually corrected for inconsistencies by visual inspection and addition of control points where necessary to aid gray and white matter differentiation. Typically, only the temporal poles required manual edits to improve reconstructed surface accuracy. Cortical thickness at each vertex was calculated by measuring the shortest distance between the white and pial surfaces at that vertex (Han et al. 2006). Estimated total intracranial volume for each subject also was obtained for use as a covariate in all hypothesis-testing.
Hypothesis-testing analyses
Although several analysis approaches could be used to test whether MDD-diagnosed adolescents brain-behavior relationships showed greater evidence for abnormality, we elected to use a general linear model (GLM) approach. GLM allowed us to parameterize the strength of association between impulsivity trait and cortical thickness for each study group, then contrast them via statistical interaction. Significant interactions could reflect either exaggerated relationships in MDD (e.g., when a normal brain-behavior association showed a steeper slope), or denote a completely different relationship (e.g., when the brain-behavior relationships were opposite in MDD versus non-MDD). For each type of brain structure measurement (cortical thickness or surface area), we performed five separate FreeSurfer qdec GLM analyses (i.e., one each for BIS-11 Attentional, Motor, or Non-Planning subscale scores or Sensitivity to Reward and Sensitivity to Punishment scores). For each model, we assessed whether or not there was a significant interactions of diagnosis (MDD versus non-MDD) × impulsivity trait. The dependent measure in all analyses was either cortical thickness or surface area across the whole brain. All GLMs included age and intracranial volume (ICV) as covariates of no interest. All models were tested using vertex-based based qdec analysis. To safeguard against false positives, we applied Monte Carlo permutation testing for multiple comparison correction (p < .05), which corrects across vertices in each entire hemisphere. In addition, the statistical significance of clusters detected by Monte Carlo methods were adjusted using a Holm-Bonferroni method (Holm 1979). Peak vertex results within each cluster were reported with reference to the Desikan-Killiany atlas (Desikan et al. 2006) for anatomical localization. To aid interpretation, significant results were converted to Cohen’s d effect size estimates (GLM effect of interest / residual standard deviation) by averaging all vertex d values within significant clusters.
Although examining the effect of current antidepressant status was not the focus of this study, it was important to ensure that medication usage was unrelated to any associations between brain structure and impulsivity. Therefore, we also conducted supplemental analyses of MDD subgroups brain structure. We also compared the MDD and non-MDD study groups to determine if MDD brain structure abnormalities might be characteristically different from those reported in prior research.
Results
As hypothesized, a significant Diagnosis × BIS-11 Motor Impulsiveness interaction was found for cortical thickness in the anterior part of left rostral middle frontal region (xyz = −21, 52.9, −2) (Fig. 1a). In this region, non-MDD participants showed a strong positive association between cortical thickness and BIS-11 Motor scores. In contrast, MDD participants showed a negative association. For BIS-11 Non-Planning Impulsiveness, a significant interaction emerged for right paracentral lobule (xyz = 19.4, 26.3, 50.8). In this region, greater cortical thickness was observed with greater impulsivity in MDD, but no association was found for controls. These significant effects are depicted in Fig. 1 and Table 2.
No hypothesized interaction effects were found for Sensitivity to Reward SPSRQ scores. However, we observed significant differences between the MDD and non-MDD groups that survived the Monte Carlo whole brain significance-correction thresholds in the relationship of Sensitivity to Punishment and cortical thickness in left supramarginal (xyz = −35.5, −34.2, 35.2) and left precuneus (xyz = −8.2, −68.8, 46) regions. These results are listed in Table 2 and depicted in Supplemental Figure 1.
Additional Holm-Bonferroni experimentwise corrections for multiple tests confirmed all p values reported in Table 1 ranged from 0.04 to.016.
There were no significant interaction effects found for surface area for any analysis. Supplemental analyses of cortical thickness comparing medicated versus unmedicated MDD participants failed to find any differences that survived corrections for multiple comparisons. The supplemental analysis comparing MDD to non-MDD found many of the same MDD abnormalities as reported in prior studies, albeit at liberal p < .05 uncorrected statistical thresholds, supporting the idea that our MDD-diagnosed adolescents were generally representative of the population. Because we did not have a priori hypotheses for this comparison and for consideration of space limitations, specific results were not tabulated but can be made available upon request to the authors.
Discussion
This study examined for the first time whether the relationship between cortical thickness and impulsivity traits differed in adolescents with and without Major Depressive Disorder. As hypothesized, we found a significant moderation effect in several different cortical regions depending on which personality trait was considered. Interaction plots of these effects revealed they typically were not simple additive effects as we had predicted. In other words, the presence of both high impulsivity trait levels and MDD typically was not always linked to the lowest (or greatest) cortical thickness measurements in those brain regions. Rather, impulsivity-brain structure relationships typically differed in nature in each study group. For example, for the left rostral middle frontal, left supramarginal, and left precuneus study findings, any positive linear association in one study group was observed as a negative association in the other. For the right paracentral region, there was no discernable relationship between cortical thickness and impulsivity in non-MDD, but greater thickness in MDD was linked to higher Non-Planning Impulsiveness levels. Instead, the findings illustrate that within adolescence, whatever neurobiological differences that underlie and presumably give rise to MDD somehow result in altered brain-behavior relationships in these regions. On a purely practical level, this suggests that studies seeking to understand brain structure abnormalities in MDD or other clinical disorders should more carefully consider disorder-associated factors like impulsivity to the same degree as they recognize other, more commonly-recognized potential confounds like age or intracranial volume. Otherwise, there is a risk of introducing error into MDD case-control group comparisons in all but perhaps the very largest samples.
The conceptual and neurobiological implications of having different impulsivity-brain structure relationships in MDD and non-MDD groups can be clarified somewhat by examining the functional correlates of the brain regions we identified. For instance, our analyses found that anterior left rostral middle frontal cortex cortical thickness was linked to BIS-11-measured forms of impulsivity. Not only is lateral prefrontal cortex function robustly associated with impulsivity in numerous prior reports (Aron et al. 2014; Bari and Robbins 2013), at least one previous study also specifically found a positive relationship between left lateral prefrontal and Motor Impulsiveness in typically-developing participants (Schilling et al. 2012). This bolsters confidence in this finding. Although there is a well-known association of mid-dorsolateral or caudal prefrontal cortex with supervisory or “executive” forms of cognition, the region we detected was in a more anterior part of the rostral middle frontal gyrus region. This region is engaged during performance of numerous tasks involving higher-order cognition (e.g., attention shifting, memory encoding and retrieval, contextual processing, etc. (Donaldson et al. 2001; King et al. 2005; Huang et al. 2012). It also has been linked to impulsivity. Rubia et al. found girls had better inhibitory capacity than boys on a stop-signal reaction time task, which was linked to greater activation in this region (Rubia et al. 2013). Not only is self-reported impulsivity linked to activation of this area on temporal choice experimental paradigms (Hinvest et al. 2011), Diekhof et al. found that counter-acting an impulse to act in order to be rewarded changed functional connectivity between this region and nucleus accumbens (Diekhof et al. 2012). Moreover, in another study, MDD-diagnosed participants were found to have diminished functional connectivity within a neural circuit that included this region bilaterally, as well as lateral parietal cortex, the temporal-occipital junction and precentral gyrus – regions involved with attention and working memory function (Veer et al. 2010). Collectively, a growing body of research has linked this specific region to various forms of impulsive behavior. Therefore, this seems to be a meaningful neural correlate of impulsive-MDD adolescents. Our supplemental comparison of MDD versus non-MDD showed that this effect was found in a region with decreased MDD cortical thickness. In other words, in non-MDD greater left rostral middle cortical thickness was linked to higher impulsivity, perhaps reflecting maturational delays in the normal synaptic pruning and volume loss seen in this region across adolescence. In contrast, for MDD who showed overall lower thickness, higher impulsivity was linked to even thinner left rostral middle frontal cortex, suggesting an early-emerging traitlike marker.
The second study finding was that the most impulsive MDD-diagnosed adolescents also had greater cortical thickness in right paracentral lobule, consistent with greater paracentral MDD thickness in at least one prior MDD study (Peng et al. 2015) and with several studies that found evidence for increased cortical thickness (Mackin et al. 2013; Peng et al. 2015; Qiu et al. 2014) or volume (Kim et al. 2013) in some adolescent MDD brain regions. The paracentral lobule is a brain region traditionally recognized to be part of both sensory and motor systems representing lower extremities and elimination functions. However, recent studies have begun to describe its role in cognitive functions relevant to either MDD or impulsivity. It is engaged during interpretation of sensory information such as emotion perception (Radua et al. 2010). Other evidence suggests that effect might be most relevant to MDD-specific neurobiological abnormalities. For example, a recent pilot study specifically found greater paracentral lobule activation to negatively-valenced pictures as part of a network of regions involved in emotion processing in female MDD patients with histories of significant stressful events in the 6 months prior to assessment (Li et al. 2015). The relevance of paracentral lobule to impulsivity is suggested by recent findings showing greater functional connectivity in neural circuits known to be engaged not only for cognitive control in patients with late-life depression, but also in numerous motor system regions (Kenny et al. 2010). Such a profile might be expected for a correlate of BIS Non-Planning impulsiveness that measures a specific type of behavior marked by a lack of careful, controlled, reflective thinking about behavior before acting. While this possibility is intriguing, the functional interpretation of greater paracentral lobule thickness in impulsive-MDD requires additional explication. Future MDD studies might explore the role of paracentral lobule as a possible functional correlate of action planning and reflection using fMRI. Such research should keep the association with impulsivity found here in mind for its sampling, approach and data interpretation.
Our analyses found no differences between MDD-diagnosed and non-MDD adolescents in the relationship between cortical thickness and reward sensitivity for any brain region. We also found no statistical interaction for surface area measurements. However, we unexpectedly found that depressed adolescents had an abnormal relationship between cortical thickness in left supramarginal and left precuneus areas and scores on the Sensitivity to Punishment subscale. Because these were not hypothesized effects, we do not offer conclusions, but rather point out some prior associations that suggest this relationship is worth future consideration. These two regions typically are not considered key nodes in neural networks that selectively respond to punishment (e.g., posterior mid-cingulate/posterior cingulate, premotor cortex, parahippocampal gyrus, inferior/middle temporal gyri, periaqueductal grey) or regions that respond to either reward or punishment (e.g., mid-cingulate, amygdala/hippocampus, thalamus) (Hayes et al. 2014). However, it is interesting that the results of both animal (Leathers and Olson 2012, 2013) and human (Kahnt and Tobler 2013) studies suggest lateral intraparietal regions contribute to punishment processing by encoding stimulus salience and thereby enhancing attention, particularly in complex environments when both appetitive and aversive stimuli are available. Alternatively, these associations might reflect the role of parietal lobe and precuneus in self-referential information processing (Platek et al. 2008; Kircher et al. 2000, 2002). Midline cortical structures including precuneus contribute to being self-aware (Kjaer et al. 2002; Keenan et al. 2003). Other research showed increased activity in precuneus and dorsomedial prefrontal cortex compared to a resting state baseline during viewing of social interactions (Iacoboni et al. 2004). In that study, both feelings of sympathy and judged mitigation of punishment were reflected in precuneus activation levels. Although speculative, these associations suggest greater cortical thickness in these regions might be a structural correlate of abnormal processing of the relevance of punishment to the self in MDD. Such ideas require additional study to formally test. However, this unexpected finding is not directly relevant to impulsivity traits as typically conceptualized. Also, subsequent research might find this interaction is actually driven by one or more MDD-related factors. For example, left supramarginal gyrus cortex has been found to be thinner in medication-naïve pediatric MDD in a previous report (Fallucca et al. 2011), as well as in our current sample in our supplemental analyses. Lower supramarginal gray matter also has been linked to suicidal behavior in patients with psychotic disorders (Giakoumatos et al. 2013), raising the possibility this effect is more related to suicidality than punishment per se.
In conclusion, we have identified two brain regions whose relationship between cortical thickness and “rash impulsivity” differ between MDD and non-MDD adolescent groups. This study shows that impulsivity traits believed important to some of the most high risk behavior in MDD has distinct neural correlates. Although our interest in MDD impulsive suicide prompted the study question and we have linked these abnormalities to suicidal depression through our sampling focus, we could not test whether these abnormalities predict suicide because we did not have a non-suicidal MDD comparison group. Also, caution should be used before inferring that the cortical thickness patterns described here might be the cause of either impulsivity or MDD. Cortical thickness represents the endpoint of numerous influences, both environmental and genetic (Hulvershorn et al. 2011; Winkler et al. 2010; Evans 2013; Alexander-Bloch et al. 2013). This study does show that simple, additive models of neurobiological impairment can only explain some of the different brain-behavior relationships with impulsivity in MDD. Although our use of age and ICV as statistical covariates made it possible to characterize the relationships among study factors without having to explain a complicated maturational context, it also remains possible that these relationships change in meaningful ways across adolescent development. Evaluating any 3-way interaction between MDD diagnosis, impulsivity, and age is better suited to a prospective longitudinal study that uses a larger sample than we examined in this study. The findings are not likely related to any effects of antidepressant use on brain structure. Although prior studies have found greater grey matter volume in MDD patients treated with antidepressants (e.g., in ventral midline prefrontal cortex regions), none of the impulsivity-related brain structure differences found in the current study overlapped with these prior findings (Bora et al. 2012; Hamilton et al. 2008; Lorenzetti et al. 2009). More recently, the ENIGMA Mood Disorders working group failed to find any medication-related cortical thickness differences in adolescents taking antidepressants (Schmaal et al. 2016).
Future research should build upon these findings to directly explore the neurobiological basis of impulsive suicide, carefully controlling for effects of comorbidity (e.g., anxiety), medications, and other factors known to be linked to suicide. Finally, although our use of stringent “whole brain” correction for multiple comparisons was appropriate for confidence in the novel findings, it might have not revealed meaningful, equally interesting interaction effects in other brain regions. Therefore, these results are not intended to be comprehensive or definitive, but rather to provoke more careful thinking about how cognitive or personality factors might complicate our search for the causes of common psychiatric disorders, and how the neurobiology of impulsivity and MDD interact in patients with high risk behavior.
References
Abe, O., Yamasue, H., Kasai, K., Yamada, H., Aoki, S., Inoue, H., et al. (2010). Voxel-based analyses of gray/white matter volume and diffusion tensor data in major depression. Psychiatry Research, 181(1), 64–70. doi:10.1016/j.pscychresns.2009.07.007.
Alexander-Bloch, A., Giedd, J. N., & Bullmore, E. (2013). Imaging structural co-variance between human brain regions. Nature Reviews. Neuroscience, 14(5), 322–336. doi:10.1038/nrn3465.
Aron, A. R., Robbins, T. W., & Poldrack, R. A. (2014). Inhibition and the right inferior frontal cortex: one decade on. Trends in Cognitive Sciences, 18(4), 177–185. doi:10.1016/j.tics.2013.12.003.
Bari, A., & Robbins, T. W. (2013). Inhibition and impulsivity: behavioral and neural basis of response control. Progress in Neurobiology, 108, 44–79. doi:10.1016/j.pneurobio.2013.06.005.
Beck, A., Schuyler, D., & Herman, J. (1974). Development of suicidal intent scales. In A. Beck, H. Resnik, & D. J. Lettieri (Eds.), The prediction of suicide (pp. 45–56). Bowie: Charles.
Beck, A., Steer, R. A., & Carbin, M. G. (1988). Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. doi:10.1016/0272-7358(88)90050-5.
Beghi, M., Rosenbaum, J. F., Cerri, C., & Cornaggia, C. M. (2013). Risk factors for fatal and nonfatal repetition of suicide attempts: a literature review. Neuropsychiatric Disease and Treatment, 9, 1725–1736. doi:10.2147/ndt.s40213.
Bernhardt, B. C., Smallwood, J., Tusche, A., Ruby, F. J., Engen, H. G., Steinbeis, N., et al. (2014). Medial prefrontal and anterior cingulate cortical thickness predicts shared individual differences in self-generated thought and temporal discounting. NeuroImage, 90, 290–297. doi:10.1016/j.neuroimage.2013.12.040.
Bora, E., Harrison, B. J., Davey, C. G., Yucel, M., & Pantelis, C. (2012). Meta-analysis of volumetric abnormalities in cortico-striatal-pallidal-thalamic circuits in major depressive disorder. Psychological Medicine, 42(4), 671–681. doi:10.1017/S0033291711001668.
Brewin, C. R., Smith, A. J., Power, M., & Furnham, A. (1992). State and trait differences in depressive self-perceptions. Behaviour Research and Therapy, 30(5), 555–557. doi:10.1016/0005-7967(92)90042-F.
Brezo, J., Paris, J., & Turecki, G. (2006). Personality traits as correlates of suicidal ideation, suicide attempts, and suicide completions: a systematic review. Acta Psychiatrica Scandinavica, 113(3), 180–206. doi:10.1111/j.1600-0447.2005.00702.x.
Churchwell, J. C., & Yurgelun-Todd, D. A. (2013). Age-related changes in insula cortical thickness and impulsivity: significance for emotional development and decision-making. Developmental Cognitive Neuroscience, 6, 80–86. doi:10.1016/j.dcn.2013.07.001.
Cummings, C. M., Caporino, N. E., & Kendall, P. C. (2014). Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin, 140(3), 816–845. doi:10.1037/a0034733.
Dale, A. M., Fischl, B., & Sereno, M. I. (1999). Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage, 9(2), 179–194. doi:10.1006/nimg.1998.0395.
Dawe, S., & Loxton, N. J. (2004). The role of impulsivity in the development of substance use and eating disorders. Neuroscience and Biobehavioral Reviews, 28(3), 343–351. doi:10.1016/j.neubiorev.2004.03.007.
Dawe, S., Gullo, M. J., & Loxton, N. J. (2004). Reward drive and rash impulsiveness as dimensions of impulsivity: implications for substance misuse. Addictive Behaviors, 29(7), 1389–1405. doi:10.1016/j.addbeh.2004.06.004.
Desikan, R. S., Segonne, F., Fischl, B., Quinn, B. T., Dickerson, B. C., Blacker, D., et al. (2006). An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage, 31(3), 968–980. doi:10.1016/j.neuroimage.2006.01.021.
Diekhof, E. K., Keil, M., Obst, K. U., Henseler, I., Dechent, P., Falkai, P., et al. (2012). A functional neuroimaging study assessing gender differences in the neural mechanisms underlying the ability to resist impulsive desires. Brain Research, 1473, 63–77.
Donaldson, D. I., Petersen, S. E., & Buckner, R. L. (2001). Dissociating memory retrieval processes using fMRI: evidence that priming does not support recognition memory. Neuron, 31(6), 1047–1059. doi:10.1016/S0896-6273(01)00429-9.
Drobetz, R., Hanggi, J., Maercker, A., Kaufmann, K., Jancke, L., & Forstmeier, S. (2014). Structural brain correlates of delay of gratification in the elderly. Behavioral Neuroscience, 128(2), 134–145. doi:10.1037/a0036208.
Ducharme, S., Albaugh, M. D., Hudziak, J. J., Botteron, K. N., Nguyen, T. V., Truong, C., et al. (2014). Anxious/depressed symptoms are linked to right ventromedial prefrontal cortical thickness maturation in healthy children and young adults. Cerebral Cortex, 24(11), 2941–2950. doi:10.1093/cercor/bht151.
Evans, A. C. (2013). Networks of anatomical covariance. NeuroImage, 80, 489–504. doi:10.1016/j.neuroimage.2013.05.054.
Fallucca, E., MacMaster, F. P., Haddad, J., Easter, P., Dick, R., May, G., et al. (2011). Distinguishing between major depressive disorder and obsessive-compulsive disorder in children by measuring regional cortical thickness. Archives of General Psychiatry, 68(5), 527–533.
Fischl, B., Sereno, M. I., & Dale, A. M. (1999). Cortical surface-based analysis. II: inflation, flattening, and a surface-based coordinate system. NeuroImage, 9(2), 195–207. doi:10.1006/nimg.1998.0396.
Foland-Ross, L. C., Gilbert, B. L., Joormann, J., & Gotlib, I. H. (2015a). Neural markers of familial risk for depression: an investigation of cortical thickness abnormalities in healthy adolescent daughters of mothers with recurrent depression. Journal of Abnormal Psychology, 124, 476–485 US: American Psychological Association.
Foland-Ross, L. C., Sacchet, M. D., Prasad, G., Gilbert, B., Thompson, P. M., & Gotlib, I. H. (2015b). Cortical thickness predicts the first onset of major depression in adolescence. International Journal of Developmental Neuroscience, 46, 125–131. doi:10.1016/j.ijdevneu.2015.07.007.
Giakoumatos, C. I., Tandon, N., Shah, J., Mathew, I. T., Brady, R. O., Clementz, B. A., et al. (2013). Are structural brain abnormalities associated with suicidal behavior in patients with psychotic disorders? Journal of Psychiatric Research, 47(10), 1389–1395. doi:10.1016/j.jpsychires.2013.06.011.
Giegling, I., Olgiati, P., Hartmann, A. M., Calati, R., Moller, H. J., Rujescu, D., et al. (2009). Personality and attempted suicide. Analysis of anger, aggression and impulsivity. Journal of Psychiatric Research, 43(16), 1262–1271. doi:10.1016/j.jpsychires.2009.04.013.
Gruber, J., Gilbert, K. E., Youngstrom, E., Youngstrom, J. K., Feeny, N. C., & Findling, R. L. (2013). Reward dysregulation and mood symptoms in an adolescent outpatient sample. Journal of Abnormal Child Psychology, 41(7), 1053–1065. doi:10.1007/s10802-013-9746-8.
Gvion, Y., & Apter, A. (2011). Aggression, impulsivity, and suicide behavior: a review of the literature. Archives of Suicide Research, 15(2), 93–112. doi:10.1080/13811118.2011.565265.
Hamilton, J. P., Siemer, M., & Gotlib, I. H. (2008). Amygdala volume in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Molecular Psychiatry, 13(11), 993–1000. doi:10.1038/mp.2008.57.
Han, X., Jovicich, J., Salat, D., van der Kouwe, A., Quinn, B., Czanner, S., et al. (2006). Reliability of MRI-derived measurements of human cerebral cortical thickness: the effects of field strength, scanner upgrade and manufacturer. NeuroImage, 32(1), 180–194. doi:10.1016/j.neuroimage.2006.02.051.
Hayes, D. J., Duncan, N. W., Xu, J., & Northoff, G. (2014). A comparison of neural responses to appetitive and aversive stimuli in humans and other mammals. Neuroscience & Biobehavioral Reviews, 45, 350–368. doi:10.1016/j.neubiorev.2014.06.018.
Hinvest, N. S., Elliott, R., McKie, S., & Anderson, I. M. (2011). Neural correlates of choice behavior related to impulsivity and venturesomeness. Neuropsychologia, 49(9), 2311–2320.
Holm, S. (1979). A simple sequential rejective method procedure. Scandinavian Journal of Statistics, 6, 65–70.
Holmes, A. J., Lee, P. H., Hollinshead, M. O., Bakst, L., Roffman, J. L., Smoller, J. W., et al. (2012). Individual differences in amygdala-medial prefrontal anatomy link negative affect, impaired social functioning, and polygenic depression risk. The Journal of Neuroscience, 32(50), 18087–18100. doi:10.1523/JNEUROSCI.2531-12.2012.
Huang, S., Belliveau, J. W., Tengshe, C., & Ahveninen, J. (2012). Brain networks of novelty-driven involuntary and cued voluntary auditory attention shifting. PloS One, 7(8), e44062.
Hulvershorn, L. A., Cullen, K., & Anand, A. (2011). Toward dysfunctional connectivity: a review of neuroimaging findings in pediatric major depressive disorder. Brain Imaging and Behavior, 5(4), 307–328. doi:10.1007/s11682-011-9134-3.
Iacoboni, M., Lieberman, M. D., Knowlton, B. J., Molnar-Szakacs, I., Moritz, M., Throop, C. J., et al. (2004). Watching social interactions produces dorsomedial prefrontal and medial parietal BOLD fMRI signal increases compared to a resting baseline. NeuroImage, 21(3), 1167–1173. doi:10.1016/j.neuroimage.2003.11.013.
Kaag, A. M., Crunelle, C. L., van Wingen, G., Homberg, J., van den Brink, W., & Reneman, L. (2014). Relationship between trait impulsivity and cortical volume, thickness and surface area in male cocaine users and non-drug using controls. Drug and Alcohol Dependence, 144, 210–217. doi:10.1016/j.drugalcdep.2014.09.016.
Kahnt, T., & Tobler, P. N. (2013). Salience signals in the right temporoparietal junction facilitate value-based decisions. The Journal of Neuroscience, 33(3), 863–869. doi:10.1523/jneurosci.3531-12.2013.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36(7), 980–988. doi:10.1097/00004583-199707000-00021.
Keenan, J. P., Gallup, G. C., & Falk, D. (2003). The face in the mirror: The search for the origins of consciousness. New York: HarperCollins Publishers.
Kenny, E. R., O'Brien, J. T., Cousins, D. A., Richardson, J., Thomas, A. J., Firbank, M. J., et al. (2010). Functional connectivity in late-life depression using resting-state functional magnetic resonance imaging. The American Journal of Geriatric Psychiatry, 18(7), 643–651. doi:10.1097/JGP.0b013e3181cabd0e.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K. R., et al. (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289(23), 3095–3105.
Kim, B., Kim, M. K., Yoo, E., Lee, J. Y., Choe, A. Y., Yook, K. H., et al. (2013). Comparison of panic disorder with and without comorbid major depression by using brain structural magnetic resonance imaging. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 43, 188–196. doi:10.1016/j.pnpbp.2012.12.022.
King, J. A., Hartley, T., Spiers, H. J., Maguire, E. A., & Burgess, N. (2005). Anterior prefrontal involvement in episodic retrieval reflects contextual interference. NeuroImage, 28(1), 256–267. doi:10.1016/j.neuroimage.2005.05.057.
Kircher, T. T., Senior, C., Phillips, M. L., Benson, P. J., Bullmore, E. T., Brammer, M., et al. (2000). Towards a functional neuroanatomy of self processing: effects of faces and words. Brain Research. Cognitive Brain Research, 10(1–2), 133–144.
Kircher, T. T., Brammer, M., Bullmore, E., Simmons, A., Bartels, M., & David, A. S. (2002). The neural correlates of intentional and incidental self processing. Neuropsychologia, 40(6), 683–692. doi:10.1016/S0028-3932(01)00138-5.
Kjaer, T. W., Nowak, M., & Lou, H. C. (2002). Reflective self-awareness and conscious states: PET evidence for a common midline parietofrontal core. NeuroImage, 17(2), 1080–1086. doi:10.1006/nimg.2002.1230.
Leathers, M. L., & Olson, C. R. (2012). In monkeys making value-based decisions, LIP neurons encode cue salience and not action value. Science, 338(6103), 132–135.
Leathers, M. L., & Olson, C. R. (2013). Response to comment on “In monkeys making value-based decisions, LIP neurons encode cue salience and not action value”. Science, 340(6131), 430. doi:10.1126/science.1233367.
Leshem, R., & Glicksohn, J. (2012). A critical look at the relationship between impulsivity and decision-making in adolescents: are they related or separate factors? Developmental Neuropsychology, 37(8), 712–731. doi:10.1080/87565641.2012.718815.
Li, G., Ma, X., Bian, H., Sun, X., Zhai, N., Yao, M., et al. (2015). A pilot fMRI study of the effect of stressful factors on the onset of depression in female patients. Brain Imaging and Behavior. doi:10.1007/s11682-015-9382-8.
Lorenzetti, V., Allen, N. B., Fornito, A., & Yucel, M. (2009). Structural brain abnormalities in major depressive disorder: a selective review of recent MRI studies. Journal of Affective Disorders, 117(1–2), 1–17. doi:10.1016/j.jad.2008.11.021.
Luby, J. L., Belden, A. C., Jackson, J. J., Lessov-Schlaggar, C. N., Harms, M. P., Tillman, R., et al. (2016). Early childhood depression and alterations in the trajectory of gray matter maturation in middle childhood and early adolescence. JAMA Psychiatry, 73(1), 31–38. doi:10.1001/jamapsychiatry.2015.2356.
Luking, K. R., Pagliaccio, D., Luby, J. L., & Barch, D. M. (2016). Reward processing and risk for depression across development. Trends in Cognitive Sciences, 20(6), 456–468. doi:10.1016/j.tics.2016.04.002.
Mackin, R. S., Tosun, D., Mueller, S. G., Lee, J. Y., Insel, P., Schuff, N., et al. (2013). Patterns of reduced cortical thickness in late-life depression and relationship to psychotherapeutic response. The American Journal of Geriatric Psychiatry, 21(8), 794–802. doi:10.1016/j.jagp.2013.01.013.
March, J. S., Parker, J. D. A., Sullivan, K., Stallings, P., & Conners, C. K. (1997). The multidimensional anxiety scale for children (MASC): factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4), 554–565. doi:10.1097/00004583-199704000-00019.
Marrus, N., Belden, A., Nishino, T., Handler, T., Ratnanather, J. T., Miller, M., et al. (2015). Ventromedial prefrontal cortex thinning in preschool-onset depression. Journal of Affective Disorders, 180, 79–86. doi:10.1016/j.jad.2015.03.033.
Nakano, M., Matsuo, K., Nakashima, M., Matsubara, T., Harada, K., Egashira, K., et al. (2014). Gray matter volume and rapid decision-making in major depressive disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 48, 51–56. doi:10.1016/j.pnpbp.2013.09.011.
Pannekoek, J. N., van der Werff, S. J. A., van den Bulk, B. G., van Lang, N. D. J., Rombouts, S. A. R. B., van Buchem, M. A., et al. (2014). Reduced anterior cingulate gray matter volume in treatment-naïve clinically depressed adolescents. NeuroImage: Clinical, 4, 336–342. doi:10.1016/j.nicl.2014.01.007.
Papmeyer, M., Giles, S., Sussmann, J. E., Kielty, S., Stewart, T., Lawrie, S. M., et al. (2015). Cortical thickness in individuals at high familial risk of mood disorders as they develop major depressive disorder. Biological Psychiatry, 78(1), 58–66. doi:10.1016/j.biopsych.2014.10.018.
Patton, J. H., Stanford, M. S., & Barratt, E. S. (1995). Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology, 51(6), 768–774.
Peng, D., Shi, F., Li, G., Fralick, D., Shen, T., Qiu, M., et al. (2015). Surface vulnerability of cerebral cortex to major depressive disorder. PloS One, 10(3), e0120704. doi:10.1371/journal.pone.0120704.
Perroud, N., Baud, P., Mouthon, D., Courtet, P., & Malafosse, A. (2011). Impulsivity, aggression and suicidal behavior in unipolar and bipolar disorders. Journal of Affective Disorders, 134(1–3), 112–118. doi:10.1016/j.jad.2011.05.048.
Peterson, B. S., Warner, V., Bansal, R., Zhu, H., Hao, X., Liu, J., et al. (2009). Cortical thinning in persons at increased familial risk for major depression. Proceedings of the National Academy of Sciences of the United States of America, 106(15), 6273–6278. doi:10.1073/pnas.0805311106.
Piko, B. F., & Pinczés, T. (2014). Impulsivity, depression and aggression among adolescents. Personality and Individual Differences, 69, 33–37. doi:10.1016/j.paid.2014.05.008.
Platek, S. M., Wathne, K., Tierney, N. G., & Thomson, J. W. (2008). Neural correlates of self-face recognition: an effect-location meta-analysis. Brain Research, 1232, 173–184.
Qiu, L., Lui, S., Kuang, W., Huang, X., Li, J., Li, J., et al. (2014). Regional increases of cortical thickness in untreated, first-episode major depressive disorder. Translational Psychiatry, 4, e378. doi:10.1038/tp.2014.18.
Radua, J., Phillips, M. L., Russell, T., Lawrence, N., Marshall, N., Kalidindi, S., et al. (2010). Neural response to specific components of fearful faces in healthy and schizophrenic adults. NeuroImage, 49(1), 939–946. doi:10.1016/j.neuroimage.2009.08.030.
Reynolds, S., Carrey, N., Jaworska, N., Langevin, L. M., Yang, X.-R., & MacMaster, F. P. (2014). Cortical thickness in youth with major depressive disorder. BMC Psychiatry, 14(1), 83.
Rubia, K., Lim, L., Ecker, C., Halari, R., Giampietro, V., Simmons, A., et al. (2013). Effects of age and gender on neural networks of motor response inhibition: from adolescence to mid-adulthood. NeuroImage, 83, 690–703.
Russo, S. J., & Nestler, E. J. (2013). The brain reward circuitry in mood disorders. Nature Reviews. Neuroscience, 14(9), 609–625. doi:10.1038/nrn3381.
Saddichha, S., & Scheutz, C. (2014). Impulsivity in remitted depression: a meta-analytic review. Asian Journal of Psychiatry, 9, 13–16.
Schilling, C., Kuhn, S., Romanowski, A., Schubert, F., Kathmann, N., & Gallinat, J. (2012). Cortical thickness correlates with impulsiveness in healthy adults. NeuroImage, 59(1), 824–830. doi:10.1016/j.neuroimage.2011.07.058.
Schilling, C., Kuhn, S., Paus, T., Romanowski, A., Banaschewski, T., Barbot, A., et al. (2013). Cortical thickness of superior frontal cortex predicts impulsiveness and perceptual reasoning in adolescence. Molecular Psychiatry, 18(5), 624–630. doi:10.1038/mp.2012.56.
Schmaal, L., Hibar, D. P., Samann, P. G., Hall, G. B., Baune, B. T., Jahanshad, N., et al. (2016). Cortical abnormalities in adults and adolescents with major depression based on brain scans from 20 cohorts worldwide in the ENIGMA major depressive disorder working group. Molecular Psychiatry. doi:10.1038/mp.2016.60.
Stephens, D. N., Duka, T., Crombag, H. S., Cunningham, C. L., Heilig, M., & Crabbe, J. C. (2010). Reward sensitivity: issues of measurement, and achieving consilience between human and animal phenotypes. Addiction Biology, 15(2), 145–168. doi:10.1111/j.1369-1600.2009.00193.x.
Telzer, E. H. (2016). Dopaminergic reward sensitivity can promote adolescent health: a new perspective on the mechanism of ventral striatum activation. Developmental Cognitive Neuroscience, 17, 57–67. doi:10.1016/j.dcn.2015.10.010.
Torrubia, R., Ávila, C., Moltó, J., & Caseras, X. (2001). The Sensitivity to Punishment and Sensitivity to Reward Questionnaire (SPSRQ) as a measure of Gray's anxiety and impulsivity dimensions. Personality and Individual Differences, 31(6), 837–862. doi:10.1016/S0191-8869(00)00183-5.
van Eijndhoven, P., van Wingen, G., Katzenbauer, M., Groen, W., Tepest, R., Fernández, G., et al. (2013). Paralimbic cortical thickness in first-episode depression: evidence for trait-related differences in mood regulation. American Journal of Psychiatry, 170(12), 1477–1486. doi:10.1176/appi.ajp.2013.12121504.
Van Meter, A. R., & Youngstrom, E. A. (2015). A tale of two diatheses: temperament, BIS, and BAS as risk factors for mood disorder. Journal of Affective Disorders, 180, 170–178. doi:10.1016/j.jad.2015.03.053.
Veer, I. M., Beckmann, C. F., van Tol, M.-J., Ferrarini, L., Milles, J., Veltman, D. J., et al. (2010). Whole brain resting-state analysis reveals decreased functional connectivity in major depression. Frontiers in Systems Neuroscience, 4, 41. doi:10.3389/fnsys.2010.00041.
Winkler, A. M., Kochunov, P., Blangero, J., Almasy, L., Zilles, K., Fox, P. T., et al. (2010). Cortical thickness or grey matter volume? The importance of selecting the phenotype for imaging genetics studies. NeuroImage, 53(3), 1135–1146.
Acknowledgments
This study was funded by a grant from the American Foundation for Suicide Prevention. Special thanks go to the research staff who helped collect the data for the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Fradkin and Stevens and Ms. Bessette and Mr. Khadka declare that none of them have a conflict of interest in the research described in this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of Hartford Hospital’s institutional review board (IRB), and met standards described in the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. As most participants were legal minors, informed assent was accompanied by parental permission using procedures approved by the institutional IRB. This article does not contain any studies with animals performed by any of the authors.
Electronic supplementary material
Supplemental Figure 1
Regions showing significant difference in correlation between sensitivity to punishment and cortical thickness in depressed vs. healthy controls. (GIF 617 kb)
Rights and permissions
About this article
Cite this article
Fradkin, Y., Khadka, S., Bessette, K.L. et al. The relationship of impulsivity and cortical thickness in depressed and non-depressed adolescents. Brain Imaging and Behavior 11, 1515–1525 (2017). https://doi.org/10.1007/s11682-016-9612-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9612-8