Abstract
Previous work suggests that the ability to selectively attend to and resolve conflicting information may be the most enduring cognitive deficit following mild traumatic brain injury (mTBI). The current study used fMRI to evaluate potential differences in hemodynamic activation in 22 mTBI patients and 22 carefully matched healthy controls (HC) during a multimodal selective attention task (numeric Stroop). Behavioral data indicated faster reaction times for congruent versus incongruent trials and for stimuli presented at 0.66 compared to 0.33 Hz across both groups, with minimal differences in behavioral performance across the groups. Similarly, there were no group-wise differences in functional activation within lateral and medial prefrontal cortex during the execution of cognitive control (incongruent versus congruent trials). In contrast, within-group comparisons indicated robust patterns of attention-related modulations (ARM) within the bilateral dorsolateral prefrontal cortex and bilateral visual streams for HC but not mTBI patients. In addition, mTBI patients failed to exhibit task-induced deactivation within the default-mode network (DMN) under conditions of higher attentional load. In summary, in spite of near normal behavioral performance, current results suggest within-group abnormalities during both the top-down allocation of visual attention and in regulating the DMN during the semi-acute stage of mTBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With more than one million new cases each year, mild traumatic brain injury (mTBI) is a major health concern (Bigler 2008). Mild TBI is defined as any transient neurologic dysfunction resulting from a biomechanical force (Giza and Hovda 2001). It is associated with subtle cognitive deficits within the first few weeks of injury that typically resolve spontaneously within 3 to 6 months (Belanger et al. 2007; Bigler 2008; Iverson 2005). In addition to cognitive deficits, other symptoms include an inability to concentrate, dizziness, fatigue, headache, irritability, visual disturbances, and light sensitivity (Bryant and Harvey 1998). Despite these prominent cognitive and clinical symptoms during the semi-acute phase, standard neuroimaging modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) are usually negative (Bigler 2001; Hofman et al. 2001), prompting interest in functional neuroimaging as a means to further evaluate this condition.
The ability to selectively attend to and resolve conflicting information (i.e., cognitive control) has been reported to be an enduring cognitive deficit in mTBI (Halterman et al. 2006). Top-down cognitive control is critical for effective day-to-day functioning, as humans are constantly bombarded by congruent and incongruent information from multiple sensory modalities (e.g., visual and auditory). When multisensory information is spatially and/or temporally congruent, performance efficiency may be enhanced (Dhamala et al. 2007; Eimer et al. 2002; Spence et al. 2004). However, cognitive performance may be hampered if one sensory modality contains task-relevant but conflicting information (Johnson and Zatorre 2005; Mayer et al. 2009). Prior neuroimaging studies have indicated that the dorsal medial frontal cortex (dMFC), dorsolateral prefrontal cortex (DLPFC), anterior insula/ventrolateral prefrontal cortex (VLPFC), and inferior parietal lobes are all commonly activated during cognitive control experiments (Banich et al. 2000; Hester et al. 2004; Braver et al. 2003; Ridderinkhof et al. 2004; Roberts and Hall 2008; van Veen et al. 2001). In addition, the differential allocation of attentional resources directly affects neuronal responses for multisensory events, otherwise known as attention-related modulations (ARM). Specifically, the most widely reported ARM involves an enhanced neuronal response (i.e., increase in response amplitude) for identical stimuli within sensory and heteromodal cortices dependent on the allocation of attention (Johnson and Zatorre 2005; Liu et al. 2003; Mayer et al. 2009; Talsma et al. 2006; Woodruff et al. 1996).
To date, only a handful of studies have examined semi-acutely injured (less than 1 month post-injury) mTBI patients using functional magnetic resonance imaging (fMRI) (Lovell et al. 2007; Mayer et al. 2009; McAllister et al. 1999; McAllister et al. 2001; Slobounov et al. 2010; Smits et al. 2009). The distinction between sub-acute and chronic phases of mTBI is critical given that clinical symptoms are expected to resolve for the majority of mTBI patients (Belanger et al. 2007), and hence, samples comprised of chronically symptomatic patients likely represent a special population. McAllister and colleagues were the first to report differential activity in the right DLPFC and lateral parietal regions for mTBI patients compared to controls, dependent on processing loads during a working memory task (McAllister et al. 1999; McAllister et al. 2001). Although it was notable that task performance between the groups was equivalent, results from both of these studies suggest that processing resources may be limited in mTBI patients as tasks increase in difficulty.
Other work demonstrates that increased hemodynamic activation during a working memory task is associated with recovery time in semi-acutely injured patients (Lovell et al. 2007). Similarly, a more recent study reported a correlation between self-report measures of symptom severity and increased activation within the working memory network (e.g., dorsolateral and ventrolateral PFC), as well as a correlation between self-reported symptomatology and hyperactivation outside of the traditional network (Smits et al. 2009). Semi-acutely injured athletes also exhibit hyperactivation in the fronto-parietal network and right hippocampus during a spatial navigation task (Slobounov et al. 2010). In contrast, we recently reported hypoactivation within the fronto-parietal reorienting network and sub-cortical structures during an auditory attention task (Mayer et al. 2009), as well as abnormalities in functional connectivity between and within the default-mode network (DMN) and task-related network (Mayer et al. 2011a). These findings suggested that neuropsychiatric deficits may arise in part from abnormalities between neuronal networks mediating attention to external (frontoparietal networks) versus internal (DMN) events.
Therefore, the current study used fMRI to evaluate neuronal activation following mTBI during a multimodal Stroop task, using both auditory and visual stimuli as well as task-induced deactivations. We hypothesized that mTBI patients would exhibit normal performance on our multimodal cognitive control task, but would be characterized by hyperactivation within the cognitive control network (dMFC, DLPFC and inferior parietal lobules) during more demanding task conditions (i.e., incongruent stimuli at higher frequencies). In addition, we predicted that mTBI subjects would not exhibit ARM, suggesting a neuronal deficiency in the ability to allocate top-down attentional control (Mayer et al. 2009).
Methods
Participants
Twenty-four patients with mTBI and twenty-four gender, age and education matched controls were recruited as part of an ongoing longitudinal study. One male patient was identified as an outlier on head motion parameters (greater than 3 standard deviations over two parameters) and one male patient performed poorly on the fMRI task (below chance performance on two or more conditions) and both were excluded (along with their matched controls) from further analyses. There were no significant differences between the final groups (p > 0.10) on any of these major demographic variables or for hand preference as assessed by the Edinburgh Handedness Inventory (Oldfield 1971).
All mTBI patients suffered a closed head injury with a self-reported alteration in mental status. Additional inclusion criteria, based on the American Congress of Rehabilitory Medicine, included a Glasgow Coma Score of 13-15 upon initial presentation in the emergency room, loss of consciousness (if experienced) restricted to 30 minutes in duration and post-traumatic amnesia limited to a 24 h period. Sixteen of twenty-two mTBI patients had a CT scan at the time of their emergency room visit (determined by treating physician), and 2 of the CT scans were deemed to contain trauma-related pathology (two small subdural bleeds and one punctate subarachnoid hemorrhage) by a non-blinded neuroradiologist. Mild TBI participants and controls were not enrolled in the study if there was a history of neurological disease, alcohol or other drug abuse, psychiatric disorder, prior closed head injuries with more than 5 min loss of consciousness, learning disorder, or Attention Deficit Hyperactivity Disorder.
Patients and healthy controls underwent the same task procedures. Patients were assessed with neuropsychological (mean day post-injury = 11.48 +/- 4.64) and neuroimaging (mean day post-injury = 11.90 +/- 5.42) measures within 21 days of injury (Table 1). One mTBI patient did not complete the full neuropsychological battery within 21 days of injury (neuropsychological data missing). At the time of assessment, five of the mTBI participants were being prescribed medications for pain and other conditions associated with injury (e.g., Vicodin, Oxycontin, Percocet and Fioricet). Informed consent was obtained per institutional guidelines of the University of New Mexico. In addition to the multimodal Stroop task, all participants completed an auditory orienting task (Mayer et al. 2009) as well as a resting state scan during fMRI acquisition (Mayer et al. 2010a).
Neuropsychological assessment
Composite indices were calculated for attention, memory, working memory, processing speed, and executive function. Emotional status and somatic and cognitive complaints were also assessed (see Mayer et al. 2009 for details). The Wechsler Test of Adult Reading (WTAR) was used to provide an estimate of overall pre-morbid intellectual functioning and the Test of Memory and Malingering (TOMM) was administered to assess effort. Univariate tests were conducted to compare estimates of effort and pre-morbid intelligence, whereas multivariate tests were used to compare composite indices given the known correlation amongst neuropsychological tests.
Task
Participants rested supine in the scanner with their head secured by a forehead strap, with additional foam padding to limit head motion within the head coil. Presentation software (Neurobehavioral Systems) was used for stimulus presentation, synchronization of stimulus events with the MRI scanner and recording of response times and accuracy data. A non-ferrous key-press device was positioned directly under the subject’s right hand to record responses. During the selective attention task (numeric Stroop), multimodal (visual and auditory) congruent or incongruent numeric stimuli (targets) were simultaneously presented at either a low (0.33 Hz) or a high (0.66 Hz) frequency over a ten-second block (Fig. 1). For each block, the stream of target numbers (one, two, or three; exemplary visual angle = 9.73°) was preceded by a cue word (exemplary visual angle = 7.69°) “HEAR”, “LOOK” or “NONE.” If the cue word was “HEAR,” participants were instructed to respond (via button press) to the target stimuli presented aurally and ignore the number that was simultaneously presented visually on the screen in that block. If the cue was “LOOK,” visually presented stimuli were the targets (ignore auditory). An additional passive condition (cue word NONE) was included, in which participants were instructed not to respond to the targets. There was a 1325 ms delay between the presentation of the cue and the presentation of the first set of target numbers to maximize attentional focus.
This figure presents a diagrammatic representation of the task, exemplified by the auditory incongruent condition. Participants were asked to respond via button press (R) to a target number (one, two, or three) in one modality while ignoring congruent or incongruent stimuli in the opposite modality. Multimodal cue words (175 ms duration) indicated the modality for focused attention (e.g., “HEAR”) and were presented prior to targets (200 ms duration). The inter-block interval (IBI) varied randomly and the inter-trial interval (ITI) within each block was determined by the rate of stimulation (0.33 Hz or 0.66 Hz)
Within each block, three or six trials of the same condition were presented for the low and high frequency, respectively. Cues (175 ms duration) and targets (200 ms durtation) were always presented below the fixation cross. The inter-block interval was varied between 8, 10 and 12 s to decrease temporal expectations and permit modeling of the baseline response (visual fixation plus baseline gradient noise). There were a total of 432 trials presented across six separate imaging runs.
As response time data has a tendency towards positive skew, the median reaction time was selected as a more representative measure of central tendency for each subject and each trial-type. Two 2 × 2 × 2 [Group (mTBI vs. HC) x Condition (Congruent vs. Incongruent) x Frequency (0.33 Hz vs. 0.66 Hz)] mixed-measures ANOVAs were conducted on auditory and visual selective attention conditions to assess behavioral performance under conditions of auditory compared to visual selective attention.
MR imaging
A high resolution 5-echo multi-echo MPRAGE T1 sequence [TR (repetition time) = 2.53 s, 7○ flip angle, number of excitations (NEX) = 1, slice thickness = 1 mm, FOV (field of view) = 256 mm, resolution = 256 × 256] and T2 [echo time = 77.0 ms, TR = 1.55 s, flip angle 152°, NEX = 1, slice thickness = 1.5 mm, FOV = 220 mm, matrix = 192 × 192, voxel size = 1.15 × 1.15 × 1.5 mm3] anatomic images were collected on a 3 Tesla Siemens Trio scanner. Echo-planar images (EPI) were collected using a single-shot, gradient-echo echoplanar pulse sequence [TR = 2000 ms; TE = 29 ms; flip angle = 75○ ; FOV = 240 mm; matrix size = 64 × 64]. A total of six different fMRI runs were required to collect all relevant task data. The first image of each run was eliminated to account for T1 equilibrium effects, resulting in a total of 966 images for the final analyses. Thirty-three contiguous sagittal 3.5-mm thick slices with a gap factor of 1.05 mm were selected to provide whole-brain coverage (voxel size: 3.75 × 3.75 × 4.55 mm).
Image processing and statistical analyses
Functional images were generated using Analysis of Functional NeuroImages (AFNI) software package (Cox 1996). Time series images were spatially registered in two- and three-dimensional space to the second EPI image of the first run to reduce the effects of head motion, and were temporally interpolated to the first slice to account for differences in slice acquisition. Two MANOVAs were conducted to examine group differences in motion parameters. A voxel-wise deconvolution analysis was then performed to generate a single hemodynamic response function (HRF) for each trial-type, which was derived relative to the baseline state (visual fixation plus baseline gradient noise) and based on the first 22 s post-stimulus onset. Error trials were also modelled separately for each trial-type with additional regressors based on individual participant performance (Mayer et al. 2011b). An estimation of percent signal change for correct trials was then calculated for each condition by summing the beta coefficients for the images occurring 6–14 s post-cue onset (peak of the hemodynamic response function) and dividing by the average model intercept (β0) across the individual runs. The percent signal change maps were then converted to a 1 mm3 standard stereotaxic coordinate space (Talairach and Tournoux 1988) and spatially blurred using a 6 mm Gaussian full-width half-maximum filter.
Two voxel-wise, 2 × 2 × 2 [Group (mTBI vs. HC) x Condition (Congruent vs. Incongruent) x Frequency (0.33 Hz vs. 0.66 Hz)] mixed-measures ANOVAs were then performed on the spatially normalized percent signal change measure for the auditory and visual modality separately based on our a priori predictions. In addition, 2 × 2 × 2 [Modality (Auditory vs. Visual) x Condition (Congruent vs. Incongruent) x Frequency (0.33 Hz vs. 0.66 Hz)] repeated-measures ANOVAs were also performed to examine the effects of ARMs within each of the subject groups. All voxel-wise results were corrected for false positives at p < 0.05 (z > 2.6) using Gaussian Random Fields theory as implemented in FSL (http://www.fmrib.ox.ac.uk/fsl/feat5/programs.html).
Results
Neuropsychological and clinical measures
Results of all major neuropsychological and clinical indices are presented in Table 2. Independent samples t-tests were initially conducted to determine group differences in effort (TOMM) and estimates of premorbid levels of intelligence (WTAR). There were no significant differences in levels of effort or in estimated premorbid intellectual functioning (p > 0.10). A MANOVA was performed to investigate group differences in emotional functioning and extent of somatic and cognitive complaints. The multivariate effect of group was significant for the MANOVA (F3,39 = 9.24, p < 0.001). The univariate test results indicated that mTBI patients reported more cognitive (F1,41. = 8.73; p < 0.01) and somatic (F1,41 = 23.51; p < 0.001) complaints than controls. Significant differences were also found for the emotionality index (F1,41 = 12.01, p < 0.002; mTBI > HC), with controls exhibiting decreased levels of depression and anxiety relative to patients.
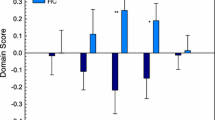
A MANOVA was performed to investigate group differences in composite neuropsychological scores. The multivariate effect of group was not significant for the MANOVA (p > 0.10), although moderate effect sizes were observed across several cognitive domains (Table 2).
Complex selective attention task: behavioral data
Behavioral accuracy for both groups was very high and approached ceiling (mTBI: 96.50 % ± 3.71 %; HC: 96.60 % ± 3.48 %), suggesting that participants had little difficulty in understanding the task. Given this low variability across participants, accuracy data was not subjected to further analyses.
Individual participants’ median reaction time (RT) for correct trials was used for all behavioral analysis. For the auditory modality (Fig. 2a), results from the ANOVA indicated significant main effects of both condition (F1,42 = 51.93, p < 0.001) and frequency (F1,42 =120.16, p < 0.001), with participants responding more quickly to congruent (mean = 561.44 +/- 77.53) compared to incongruent (mean = 637.01 +/- 92.69) trials, as well as to higher (0.66 Hz; mean = 559.81 +/- 67.69) relative to lower (0.33 Hz; mean = 638.64 +/- 93.49) frequency trials.
Graphs A and B depict reaction time (RT) in milliseconds (ms) for the auditory (Panel a) and visual (Panel b) attention conditions. Frequency of stimulation is presented on the X‐axis (0.33 Hz or 0.66 Hz) and bars represent mild traumatic brain injury (mTBI; dark grey and black bars) and healthy controls (HC; light grey bars) data for both the congruent (Con) and incongruent (Inc) conditions. Asterisks indicate trend differences between groups. Error bars correspond to the standard error of mean
The condition x frequency x group interaction term was also significant (F1,42 = 4.80, p < 0.05). To determine the significance of this three-way interaction, two 2 × 2 (condition x group) repeated-measures ANOVAs were conducted separately for each of the two primary frequencies. Similar to the omnibus model, the main effects of condition were present at both 0.33 and 0.66 Hz (p < 0.05). However, a significant condition x group interaction was also present in the more demanding 0.66 Hz condition (F1,42 = 5.04, p < 0.05), with simple effect testing indicating that patients’ (618.75 +/- 88.62) reaction times were marginally slower than HC (573.28 +/- 72.64) for the incongruent stimuli (t1,42 = 1.86, p = 0.07), with no differential effects for congruent trials (p > 0.10).
Within the visual modality (Fig. 2b), the main effects of condition (F1,42 = 45.71, p < 0.001) and frequency (F1,42 = 83.84, p < 0.001) were also significant, with participants responding more quickly to congruent (mean = 530.93 ± 77.76) compared to incongruent (mean = 577.52 ± 77.73) trials, as well as to high (0.66 Hz; mean = 524.29 ± 68.28) compared to low (0.33 Hz; mean = 584.16 ± 85.60) frequency trials. The condition by frequency interaction was also significant (F1,42 = .4.36, p < 0.05), with simple effect tests indicating that the difference between incongruent and congruent trials was significantly greater for the low frequency (t1,43 = -2.11, p < 0.05) compared to high frequency (0.33 Hz mean = 57.50 +/- 66.91; 0.66 Hz mean = 35.68 +/- 44.25) trials. No other main effects or interaction effects approached significance (p > 0.10).
MRI structural imaging data
T1- and T2-weighted MRI images were reviewed by a neuroradiologist blinded to patient diagnosis. Only one patient (negative CT scan) was found to have a lesion (right centrum semiovale) that may have been secondary to trauma. Therefore, there were a total of 3/22 (two CT and one MRI) patients with visible lesions using conventional neuroimaging techniques.
Motion parameter analyses
Two MANOVAs were performed to examine potential group differences in head motion across all 6 motion parameters (3 translational and 3 rotational) derived from the rigid body correction. Although the group effect was not significant for the translational or rotational MANOVAs (p > 0.10), univariate measures suggested marginally increased motion for the mTBI group (roll: F1,42 = 4.59; p < 0.05; yaw: F1,42 = 2.90; p = 0.096; displacement in right-left axis: F1,42 = 2.96 p = 0.093; displacement in the superior-inferior axis: F1,42 = 2.88 p = 0.097).
Between-group analyses
Similar to our behavioral results, two 2 × 2 × 2 [Group (mTBI vs. HC) x Condition (Congruent vs. Incongruent) x Frequency (0.33 Hz vs. 0.66 Hz)] mixed-measures ANOVAs were conducted to assess differences in functional activation to the auditory and visual selective attention conditions. Results for the auditory selective attention condition indicated that neither the main effect of group, the Group x Condition interaction nor the Group x Frequency interaction were significant. The main effects of frequency and condition are discussed in the within-subjects analyses section below.
For the visual selective attention condition, results indicated that the main effect of group was not significant. However, a significant group x condition x frequency interaction was observed within the bilateral thalamus. This three-way interaction was followed up with two 2 × 2 mixed design ANOVAs, with results indicating that the group x condition interaction effect was only significant at low frequency (F1, 42 = 14.71; p < 0.001) but not at high frequency (p > 0.10) trials. To follow up the significant two-way interaction effect, simple t-tests indicated that activation was significantly greater (t1,21 = -2.99, p < 0.01) for the HCs in the incongruent (mean = 0.38 ± 0.33) relative to the congruent trials (mean = 0.25 ± 0.35). In contrast, the mTBI patients showed the opposite pattern (t1,21 = 2.54, p < 0.05; incongruent: 0.24 ± 0.29; congruent: 0.38 ± 0.40).
A significant group x frequency interaction was also observed within the left primary and secondary visual cortex (Brodmann areas (BAs) 18, 19, 37), including the cuneus, lingual gyrus and middle occipital gyrus, extending into the parahippocampal and fusiform gyri (Fig. 3). Simple effects testing for this left visual cortex ROI indicated that whereas the HC did not exhibit any differences in activation between the 0.33 Hz and 0.66 Hz conditions (p > 0.10), activation was significantly greater (t1,21 = 5.74, p < 0.001) for mTBI patients in the 0.66 Hz (mean = 0.12 ± 0.26) relative to the 0.33 Hz trials (mean = -0.03 ± 0.29). In addition, the Group x Condition interaction was also significant within a region that included the caudate, periventricular white matter and other tissues that are highly susceptible to partial voluming effects. Given the lack of physiological basis for the blood-oxygen level dependent (BOLD) signal in this region, this cluster was deemed to be an artifact (false positive) and was not subjected to further analyses.
This figure presents the region of the left visual cortex (L Vis) that exhibited a significant Group x Frequency interaction when the visual modality was the focus of attention. The magnitudes of z-scores are represented by either red or yellow coloring. Locations of the sagittal (X) and axial (Z) slices are given according to the Talairach atlas. Percent signal change (PSC) values for the region are presented for both healthy controls (HC; light grey bars) and mild traumatic brain injury patients (mTBI; dark grey and black bars) at 0.33 Hz and 0.66 Hz. Error bars correspond to the standard error of mean
Within-group analyses
Two 2 × 2 × 2 ANOVAs were conducted to examine the main effects of condition, frequency, and modality within each of the mTBI and HC samples. Both groups demonstrated similar areas of increased activation during the incongruent trials relative to the congruent trials (main effect of condition), primarily localized to the left hemisphere (Online Resource 1). Common areas of increased activation for incongruent trials across both HC and mTBI patients included the left pre-supplementary motor area (pre-SMA; BA 6), DLPFC (BA 9), bilateral medial frontal gyrus (BA 32), left anterior insula/VLPFC (BAs 13/44/45/46), left posterior superior temporal sulcus (BAs 22/21) and left inferior parietal lobe (BA 39). In addition, HC also showed greater activation for incongruent trials within the right anterior insula (BA 13), bilateral striatum, bilateral thalamus and bilateral cerebellum.
Both groups also exhibited a similar pattern of hemodynamic activity as a result of increasing stimulus frequency (Fig. 4). Specifically, increased activation was observed in the bilateral primary and secondary auditory cortex (BAs 13/41/22/21), bilateral pre-motor cortex (BAs 6/9), left sensorimotor cortex (BAs 4/2/3), bilateral supplementary motor area (BA 6) extending into the anterior cingulate gyrus (BA 24), left inferior (BA 40) and superior (BA 7) parietal lobules, left striatum, left pulvinar nucleus of the thalamus, and bilateral cerebellum when the stimuli were presented at 0.66 Hz compared to 0.33 Hz. In the primary and secondary visual cortex (BAs 17, 18, 19, 37), mTBI patients exhibited bilateral activation whereas activation was more left-lateralized for the HC group. In contrast, there were marked differences across the two groups in terms of task-induced deactivations. Specifically, whereas HC exhibited a robust pattern of task-induced deactivation for the greater stimulus frequency within the anterior midline (BAs 9/32), posterior midline (BAs 5/7/18/31), right postcentral gyrus (BAs 3/4) and left medial temporal lobes, mTBI patients showed a much smaller area of deactivation within the right postcentral gyrus (BAs 3/4).
This figure presents regions showing differential activation between low (0.33 Hz) and high (0.66 Hz) frequency trials for healthy controls (HC: Panel a) and mild traumatic brain injury patients (mTBI: Panel b) during within-group comparisons. Results indicated increased activation during high frequency (blue/cyan coloring) trials for both groups within the bilateral primary and secondary auditory cortex (AUD), visual cortex (VIS), bilateral supplemental motor area (SMA), and bilateral sensorimotor cortex (S-MOT). In contrast, only HC demonstrated significantly greater deactivation for high compared to low frequency (red/yellow coloring) trials within the left medial temporal lobes (L MTL), bilateral medial frontal lobes (MFC), and bilateral posterior cingulate gyrus (PCC). The magnitudes of z-scores are color-coded and the locations of sagittal (X) and axial (Z) slices are given according to the Talairach atlas. Percent signal change (PSC) values for selected areas are presented in Panel c for both the mild traumatic brain injury (mTBI; dark grey and black bars) and healthy controls (HC; light grey bars) at both frequencies of stimulation (0.33 Hz and 0.66 Hz). Importantly, PSC for regions of interest were determined solely based on the unique areas of deactivation from the healthy control statistical parametric maps (Panel a red/yellow colored regions). Error bars correspond to the standard error of mean
Finally, there were large differences between the two groups in terms of attention-related modulations (ARM; Fig. 5), assessed through the main effect of modality. Similar to our previous study (Mayer et al. 2009), HC exhibited increased activation when attending to the visual stimuli and ignoring auditory stimuli within the bilateral “what” (temporal lateral occipital areas; BAs 18/19/37) and “where” (superior parietal lobule, precuneus and cuneus; bilateral BAs 19/7 and right BA 39) pathways of the visual cortex, bilateral DLPFC (BAs 8/9/46/45), bilateral pre-SMA (BA 6), left VLPFC (BAs 45/47), and bilateral cerebellum. In contrast, mTBI patients did not exhibit any evidence of ARM within the visual condition, providing preliminary evidence of a lack of top-down attentional control in neuronal systems. For both groups, there were no areas of increased activation for attending to the auditory stimuli while ignoring visual distractors.
This figure presents regions exhibiting greater activation for the attend visual (Vis; blue/cyan coloring) compared to attend auditory (Aud) conditions during the within-group comparisons for healthy controls (HC: Panel a) and mild traumatic brain injury patients (mTBI: Panel b). Areas of increased activation for HC during the attend visual condition included the bilateral prefrontal cortex (PFC), “what” (lateral temporal-occipital cortex; LTO) and “where” (precuneus/cuneus; PrCu) pathways, which were absent for mTBI. The magnitudes of significant z-scores are color-coded and the locations of sagittal (X) and axial (Z) slices are given according to the Talairach atlas. Percent signal change (PSC) values for selected areas are presented in Panel c for both mTBI (dark grey and black bars) and HC (light grey bars) based on selected regions from Panel a (HC group only). Error bars correspond to the standard error of mean
Discussion
Selectively attending to information from one sensory modality while ignoring another is critical for everyday functioning, and impairments in selective attention are proposed to be one of the more enduring behavioral deficits following mTBI (Halterman et al. 2006). The current study explicitly examined this selective attention hypothesis in a sample of predominantly non-complicated mTBI patients using neuropsychological, behavioral and neuroimaging parameters. Although mTBI patients exhibited a trend for increased reaction times during more rapidly presented incongruent auditory stimuli, few differences emerged in terms of between-group differences in neuronal activation. The longer delay in assessment (i.e., weeks versus days) for the current versus previous studies (Halterman et al. 2006) may potentially explain the differences in findings on measures of selective attention. However, within-group comparisons indicated that mTBI failed to both deactivate the DMN during conditions of higher attentional load and failed to exhibit attention-related modulations (ARM) during top-down visual attention.
As expected, semi-acutely injured mTBI patients self-reported significantly increased subjective cognitive, somatic and emotional symptoms on several measures relative to a carefully matched cohort of healthy controls. Consistent with previous meta-analyses (Belanger and Vanderploeg 2005; Belanger et al. 2005; Schretlen and Shapiro 2003), current results indicated subtle deficits (i.e., moderate effect sizes) across several domains of cognitive functioning objectively measured with traditional neuropsychological testing. However, objective neuropsychological deficits did not reach conventional levels of significance, perhaps as a result of our relatively small sample size and longer delay in terms of assessment time during the sub-acute stage (McCrea et al. 2003). Similarly, only subtle cognitive deficits (i.e., a trend) were observed during a multimodal selective attention task, and only for the “attend” auditory condition during the more rapid presentation of incongruent stimuli. Collectively, current findings provide evidence of both subjective and subtle objective (trend and moderate effect sizes) neurobehavioral deficits (trend and moderate effect sizes) during the first few weeks of mTBI (Belanger et al. 2007; Bigler 2008; Iverson 2005).
The primary objective of the current study was to investigate putative neurophysiological differences between patients and controls given that traditional neuroimaging measures (CT, T1 and T2 scans) were only sensitive to pathology in a handful of patients. As noted in the introduction, previous neuroimaging studies have reported a mixed pattern of both hypo- and hyperactivation in mTBI across a variety of different tasks in mTBI patients (Lovell et al. 2007; Mayer et al. 2009; McAllister et al. 1999; McAllister et al. 2001; Slobounov et al. 2010; Smits et al. 2009). Similarly, findings of both hyperactivation (Scheibel et al. 2007) and hypoactivation (Soeda et al. 2005) have been reported in more severely injured TBI patients within the lateral and medial prefrontal cortex during cognitive control tasks. In contrast, there were minimal between-group differences during the direct comparisons of hemodynamic activity for incongruent compared to congruent trials following mTBI in the current study. Moreover, within-group comparisons suggested similar activation of both the dMFC and lateral prefrontal cortex during incongruent relative to congruent trials, regions previously implicated in studies of cognitive control (Carter and van Veen 2007; Kerns et al. 2004).
In contrast, within-group comparisons indicated that healthy controls exhibited increased activation within the pulvinar nucleus of the thalamus and cerebellum during incongruent trials compared to congruent trials whereas this activity was absent in mTBI patients. A failure to activate the thalamus and cerebellum is similar to our previous studies of auditory orienting, in which both pediatric (Yang et al. 2012) and adult (Mayer et al. 2009) mTBI showed a similar pattern of hypoactivation within similar structures. In addition, within-group comparisons also indicated large differences in attention-related modulations (ARM) during the semi-acute stages of mTBI. Specifically, in contrast to HC, mTBI failed to exhibit ARM within the bilateral DLPFC, the “what” visual pathway and the “where” visual pathways when attention was allocated to the visual modality (i.e., ignore auditory). Previous studies of multimodal selective attention in healthy controls have also demonstrated that ARM are more robust during the allocation of multisensory visual (ignore auditory) relative to auditory (ignore visual) attention (Degerman et al. 2007; Johnson et al., 2005; Mayer et al. 2009). Although the exact role of ARM are unclear, enhancing the neural response for attended stimuli and suppressing the response for ignored stimuli may minimize the contribution of cross-modal distracters (Baier et al. 2006; Weissman et al. 2004). Therefore, the lack of an enhanced neural response for mTBI subjects may indicate a neurophysiological basis for the attentional problems that are so frequently reported during the semi-acute stage of the disorder.
The physiological basis for the blood-oxygen level dependent signal is the change in blood flow, blood volume and ratio of deoxyhemoglobin to oxyhemoglobin during activation relative to baseline states (Raichle and Mintun 2006), the latter of which is typically defined as unconstrained passive mental activity and spontaneous neuronal firings (Fox and Raichle 2007). In the current study, mTBI patients demonstrated a relative lack of deactivation within the bilateral anterior medial frontal cortex, bilateral posterior cingulate gyrus and left medial temporal lobe during states of increased cognitive demands (higher stimulation frequencies). In early neuroimaging studies, a similar network of task-induced deactivations was consistently (i.e., regardless of the nature of the task) observed using both PET (Shulman et al. 1997) and fMRI studies (Binder et al. 1999), which was later formalized as the default-mode network (DMN; Raichle, et al. 2001). Previous work has also indicated a close spatial relationship between the central hubs of the DMN during more formal network analyses (independent component analyses and seed-based techniques) relative to task-induced deactivations (Mannell et al. 2010).
The DMN has been related to introspection, self-referential thought, and mind wandering (Kelley et al. 2002; Mason et al. 2007; Raichle et al. 2001) and is disrupted in a number of different neuropsychiatric disorders (Broyd et al. 2009; Mannell et al. 2010). The magnitude of task-induced deactivations has been shown to vary as a function of task difficulty (Greicius and Menon 2004; McKiernan, et al. 2003), suggesting the lack of DMN deactivation in the mTBI group may be indicative of a failure to disengage from internal states. This in turn may result in a state of increased cognitive distractibility, as DMN activity has been shown to predict errors during cognitive control tasks (Eichele et al. 2008). The lack of task-induced deactivation within the DMN is also consistent with previous work by our group and others using more formal network analyses (Johnson et al. 2012; Mayer et al. 2011a), suggesting that the putative balance between the DMN and cortical attentional networks is partially disrupted following mTBI.
The lack of expected attention-related modulations (activations) and task-induced deactivation observed in the mTBI patients may therefore be the result of cognitive deficits or may directly result from impaired neuronal function, impaired neural control of microvessels, direct damage to the vascular system, metabolic disruptions, or a combination of all of the above following mTBI (Barkhoudarian et al. 2011). For example, increased Virchow-Robin spaces and hemosiderin depositions are frequently observed following mTBI (Inglese et al. 2005; Bigler 2004), and animal models indicate reduction in capillary number and diameter at different levels of injury severity (Park et al. 2009). At present, it would be overly speculative to determine the relative contributions of these different physiological mechanisms as they pertain to our finding. Moreover, the current study design is unable to distinguish whether differences in activation contribute to the subtle cognitive difficulties that are frequently observed during the semi-acute stage of mTBI or are secondary to these same impairments. Finally, other non-specific factors such as differences in head motion, pain or fatigue also contribute to differences in hemodynamic activation. Nonetheless, if current findings can be replicated, it would suggest that newer neuroimaging techniques may provide important information regarding underlying pathophysiology that is not available with conventional imaging techniques (Belanger et al. 2007; Bigler 2008).
There are several limitations to the current study. First, our anatomical imaging battery did not include more advanced scans such as susceptibility weighted imaging, which may have been more sensitive for detecting small hemorrhagic lesions. Second, there are multiple medical (e.g., pain, fatigue, and headache) and medication (pain relievers) related issues that are associated with studying mTBI patients during the semi-acute injury phase. These non-specific conditions have been shown to affect neurobehavioral functioning (Hutchison et al. 2011) and medications may directly alter the properties of the hemodynamic response. This introduces a potential confound, as it would not be feasible to eliminate patients with secondary injuries and pain from any unselected study and derive a representative sample. Thus, future studies should consider including orthopedic injuries as a potential mechanism for controlling for non-specific effects. Finally, we did not have adequate power to examine the effects of lesions on hemodynamic activity. Patients with positive structural scans (complicated mTBI) may experience increased symptoms and worse prognoses relative to patients without lesions (Iverson 2006; Lange et al. 2009), but the effects of focal lesions on more diffuse injuries are only beginning to be evaluated.
In conclusion, current results demonstrate minimal (i.e., a trend) behavioral deficits in multi-modal selective attention during the semi-acute phase of mTBI. Within-group comparisons of hemodynamic activity indicated that mTBI patients failed to both exhibit expected ARM in visual and heteromodal cortical areas, as well as failed to show expected task-induced deactivation of the default-mode network during higher attentional loads (i.e., high frequency conditions) in the absence of significant group differences. Future fMRI studies should determine whether these behavioral and functional deficits normalize in conjunction with recovery, which is expected to spontaneously occur in the majority of mTBI patients (Belanger et al. 2007; Bigler 2008; Iverson 2005). For example, activation within the frontal and parietal lobes has been shown to normalize as a function of recovery in more severely injured populations (Kim et al. 2009; Sanchez-Carrion et al. 2008). Observations of recovery within ARM or task-induced deactivations would provide additional evidence that these disruptions may serve as biomarkers of mTBI, although current findings indicate that they may not be sensitive enough for robust classification.
References
Baier, B., Kleinschmidt, A., & Muller, N. G. (2006). Cross-modal processing in early visual and auditory cortices depends on expected statistical relationship of multisensory information. Journal of Neuroscience, 26, 12260–12265.
Banich, M. T., Milham, M. P., Atchley, R. A., Cohen, N. J., Webb, A., Wszalek, T., et al. (2000). Prefrontal regions play a predominant role in imposing an attentional 'set': evidence from fMRI. Brain Research. Cognitive Brain Research, 10, 1–9.
Barkhoudarian, G., Hovda, D. A., & Giza, C. C. (2011). The molecular pathophysiology of concussive brain injury. Clinics in Sports Medicine, 30, 33–48.
Belanger, H. G., & Vanderploeg, R. D. (2005). The neuropsychological impact of sports-related concussion: a meta-analysis. Journal of International Neuropsychological Society, 11, 345–357.
Belanger, H. G., Curtiss, G., Demery, J. A., Lebowitz, B. K., & Vanderploeg, R. D. (2005). Factors moderating neuropsychological outcomes following mild traumatic brain injury: a meta-analysis. Journal of International Neuropsychological Society, 11, 215–227.
Belanger, H. G., Vanderploeg, R. D., Curtiss, G., & Warden, D. L. (2007). Recent neuroimaging techniques in mild traumatic brain injury. The Journal of Neuropsychiatry and Clinical Neurosciences, 19, 5–20.
Bigler, E. D. (2001). Quantitative magnetic resonance imaging in traumatic brain injury. The Journal of Head Trauma Rehabilitation, 16, 117–134.
Bigler, E. D. (2004). Neuropsychological results and neuropathological findings at autopsy in a case of mild traumatic brain injury. Journal of International Neuropsychological Society, 10, 794–806.
Bigler, E. D. (2008). Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. Journal of International Neuropsychological Society, 14, 1–22.
Binder, J. R., Frost, J. A., Hammeke, T. A., Bellgowan, P. S., Rao, S. M., & Cox, R. W. (1999). Conceptual processing during the conscious resting state. A functional MRI study. Journal of Cognitive Neuroscience, 11, 80–95.
Braver, T. S., Reynolds, J. R., & Donaldson, D. I. (2003). Neural mechanisms of transient and sustained cognitive control during task switching. Neuron, 39, 713–726.
Broyd, S. J., Demanuele, C., Debener, S., Helps, S. K., James, C. J., & Sonuga-Barke, E. J. (2009). Default-mode brain dysfunction in mental disorders: a systematic review. Neuroscience and Biobehavioral Reviews, 33, 279–296.
Bryant, R. A., & Harvey, A. G. (1998). Relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. The American Journal of Psychiatry, 155, 625–629.
Carter, C. S., & van Veen, V. (2007). Anterior cingulate cortex and conflict detection: an update of theory and data. Cognitive, Affective, & Behavioral Neuroscience, 7, 367–379.
Cox, R. W. (1996). AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research, 29, 162–173.
Degerman, A., Rinne, T., Pekkola, J., Autti, T., Jaaskelainen, I. P., Sams, M., et al. (2007). Human brain activity associated with audiovisual perception and attention. NeuroImage, 34, 1683–1691.
Dhamala, M., Assisi, C. G., Jirsa, V. K., Steinberg, F. L., & Kelso, J. A. (2007). Multisensory integration for timing engages different brain networks. NeuroImage, 34, 764–773.
Eichele, T., Debener, S., Calhoun, V. D., Specht, K., Engel, A. K., Hugdahl, K., et al. (2008). Prediction of human errors by maladaptive changes in event-related brain networks. Proceedings of the National Academy of Sciences of the United States of America, 105, 6173–6178.
Eimer, M., van Velzen, J., & Driver, J. (2002). Cross-modal interactions between audition, touch, and vision in endogenous spatial attention: ERP evidence on preparatory states and sensory modulations. Journal of Cognitive Neuroscience, 14, 254–271.
Fox, M. D., & Raichle, M. E. (2007). Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nature Reviews. Neuroscience, 8, 700–711.
Giza, C. C., & Hovda, D. A. (2001). The neurometabolic cascade of concussion. Journal of Athletic Training, 36, 228–235.
Greicius, M. D., & Menon, V. (2004). Default-mode activity during a passive sensory task: uncoupled from deactivation but impacting activation. Journal of Cognitive Neuroscience, 16, 1484–1492
Halterman, C. I., Langan, J., Drew, A., Rodriguez, E., Osternig, L. R., Chou, L. S., et al. (2006). Tracking the recovery of visuospatial attention deficits in mild traumatic brain injury. Brain, 129, 747–753.
Hester, R., Fassbender, C., & Garavan, H. (2004). Individual differences in error processing: a review and reanalysis of three event-related fMRI studies using the GO/NOGO task. Cerebral Cortex, 14, 986–994.
Hofman, P. A., Stapert, S. Z., van Kroonenburgh, M. J., Jolles, J., de Kruijk, J., & Wilmink, J. T. (2001). MR imaging, single-photon emission CT, and neurocognitive performance after mild traumatic brain injury. AJNR. American Journal of Neuroradiology, 22, 441–449.
Hutchison, M., Comper, P., Mainwaring, L., & Richards, D. (2011). The influence of musculoskeletal injury on cognition: implications for concussion research. The American Journal of Sports Medicine, 39, 2331–2337.
Inglese, M., Makani, S., Johnson, G., Cohen, B. A., Silver, J. A., Gonen, O., et al. (2005). Diffuse axonal injury in mild traumatic brain injury: a diffusion tensor imaging study. Journal of Neurosurgery, 103, 298–303.
Iverson, G. L. (2005). Outcome from mild traumatic brain injury. Current Opinion in Psychiatry, 18, 301–317.
Iverson, G. L. (2006). Complicated vs uncomplicated mild traumatic brain injury: acute neuropsychological outcome. Brain Injury, 20, 1335–1344.
Johnson, J. A., & Zatorre, R. J. (2005). Attention to simultaneous unrelated auditory and visual events: behavioral and neural correlates. Cerebral Cortex, 15, 1609–1620.
Johnson, B., Zhang, K., Gay, M., Horovitz, S., Hallett, M., Sebastianelli, W., et al. (2012). Alteration of brain default network in subacute phase of injury in concussed individuals: resting-state fMRI study. NeuroImage, 59, 511–518.
Kelley, W. M., Macrae, C. N., Wyland, C. L., Caglar, S., Inati, S., & Heatherton, T. F. (2002). Finding the self? An event-related fMRI study. Journal of Cognitive Neuroscience, 14, 785–794.
Kerns, J. G., Cohen, J. D., MacDonald, A. W., III, Cho, R. Y., Stenger, V. A., & Carter, C. S. (2004). Anterior cingulate conflict monitoring and adjustments in control. Science, 303, 1023–1026.
Kim, Y. H., Yoo, W. K., Ko, M. H., Park, C. H., Sung, T. K., & Na, D. L. (2009). Plasticity of the attentional network after brain injury and cognitive rehabilitation. Neurorehabilitation and Neural Repair, 23, 468–477.
Lange, R. T., Iverson, G. L., & Franzen, M. D. (2009). Neuropsychological functioning following complicated vs. uncomplicated mild traumatic brain injury. Brain Injury, 23, 83–91.
Liu, T., Slotnick, S. D., Serences, J. T., & Yantis, S. (2003). Cortical mechanisms of feature-based attentional control. Cerebral Cortex, 13, 1334–1343.
Lovell, M. R., Pardini, J. E., Welling, J., Collins, M. W., Bakal, J., Lazar, N., et al. (2007). Functional brain abnormalities are related to clinical recovery and time to return-to-play in athletes. Neurosurgery, 61, 352–359.
McKiernan, K. A., Kaufman, J. N., Kucera-Thompson, J., & Binder, J. R. (2003). A parametric manipulation of factors affecting task-induced deactivation in functional neuroimaging. Journal of Cognitive Neuroscience, 15, 394–408.
Mannell, M. V., Franco, A. R., Calhoun, V. D., Canive, J. M., Thoma, R. J., & Mayer, A. R. (2010). Resting state and task-induced deactivation: a methodological comparison in patients with schizophrenia and healthy controls. Human Brain Mapping, 31, 424–437.
Mason, M. F., Norton, M. I., Van Horn, J. D., Wegner, D. M., Grafton, S. T., & Macrae, C. N. (2007). Wandering minds: the default network and stimulus-independent thought. Science, 315, 393–395.
Mayer, A. R., Franco, A. R., Canive, J., & Harrington, D. L. (2009). The effects of stimulus modality and frequency of stimulus presentation on cross-modal distraction. Cerebral Cortex, 19, 993–1007.
Mayer, A. R., Ling, J., Mannell, M. V., Gasparovic, C., Phillips, J. P., Doezema, D., et al. (2010). A prospective diffusion tensor imaging study in mild traumatic brain injury. Neurology, 74, 643–650.
Mayer, A. R., Mannell, M. V., Ling, J., Gasparovic, C., & Yeo, R. A. (2011). Functional connectivity in mild traumatic brain injury. Human Brain Mapping, 32, 1825–1835.
Mayer, A. R., Teshiba, T. M., Franco, A. R., Ling, J., Shane, M. S., Stephen, J. M., et al. (2011b). Modeling conflict and error in the medial frontal cortex. Human Brain Mapping.
McAllister, T. W., Saykin, A. J., Flashman, L. A., Sparling, M. B., Johnson, S. C., Guerin, S. J., et al. (1999). Brain activation during working memory 1 month after mild traumatic brain injury: a functional MRI study. Neurology, 53, 1300–1308.
McAllister, T. W., Sparling, M. B., Flashman, L. A., Guerin, S. J., Mamourian, A. C., & Saykin, A. J. (2001). Differential working memory load effects after mild traumatic brain injury. NeuroImage, 14, 1004–1012.
McCrea, M., Guskiewicz, K. M., Marshall, S. W., Barr, W., Randolph, C., Cantu, R. C., et al. (2003). Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA: The Journal of the American Medical Association, 290, 2556–2563.
Oldfield, R. C. (1971). The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia, 9, 97–113.
Park, E., Bell, J. D., Siddiq, I. P., & Baker, A. J. (2009). An analysis of regional microvascular loss and recovery following two grades of fluid percussion trauma: a role for hypoxia-inducible factors in traumatic brain injury. Journal of Cerebral Blood Flow and Metabolism, 29, 575–584.
Raichle, M. E., & Mintun, M. A. (2006). Brain work and brain imaging. Annual Review of Neuroscience, 29, 449–476.
Raichle, M. E., MacLeod, A. M., Snyder, A. Z., Powers, W. J., Gusnard, D. A., & Shulman, G. L. (2001). A default mode of brain function. Proceedings of the National Academy of Sciences of the United States of America, 98, 676–682.
Ridderinkhof, K. R., Ullsperger, M., Crone, E. A., & Nieuwenhuis, S. (2004). The role of the medial frontal cortex in cognitive control. Science, 306, 443–447.
Roberts, K. L., & Hall, D. A. (2008). Examining a supramodal network for conflict processing: a systematic review and novel functional magnetic resonance imaging data for related visual and auditory stroop tasks. Journal of Cognitive Neuroscience, 20, 1063–1078.
Sanchez-Carrion, R., Gomez, P. V., Junque, C., Fernandez-Espejo, D., Falcon, C., Bargallo, N., et al. (2008). Frontal hypoactivation on functional magnetic resonance imaging in working memory after severe diffuse traumatic brain injury. Journal of Neurotrauma, 25, 479–494.
Scheibel, R. S., Newsome, M. R., Steinberg, J. L., Pearson, D. A., Rauch, R. A., Mao, H., et al. (2007). Altered brain activation during cognitive control in patients with moderate to severe traumatic brain injury. Neurorehabilitation and Neural Repair, 21, 36–45.
Schretlen, D. J., & Shapiro, A. M. (2003). A quantitative review of the effects of traumatic brain injury on cognitive functioning. International Review of Psychiatry, 15, 341–349.
Shulman, G. L., Corbetta, M., Buckner, R. L., Raichle, M. E., Fiez, J. A., Miezin, F. M., et al. (1997). Top-down modulation of early sensory cortex. Cerebral Cortex, 7, 193–206.
Slobounov, S. M., Zhang, K., Pennell, D., Ray, W., Johnson, B., & Sebastianelli, W. (2010). Functional abnormalities in normally appearing athletes following mild traumatic brain injury: a functional MRI study. Experimental Brain Research, 202, 341–354.
Smits, M., Dippel, D. W., Houston, G. C., Wielopolski, P. A., Koudstaal, P. J., Hunink, M. G., et al. (2009). Postconcussion syndrome after minor head injury: brain activation of working memory and attention. Human Brain Mapping, 30, 2789–2803.
Soeda, A., Nakashima, T., Okumura, A., Kuwata, K., Shinoda, J., & Iwama, T. (2005). Cognitive impairment after traumatic brain injury: a functional magnetic resonance imaging study using the Stroop task. Neuroradiology, 47, 501–506.
Spence, C., Pavani, F., & Driver, J. (2004). Spatial constraints on visual-tactile cross-modal distractor congruency effects. Cognitive, Affective, & Behavioral Neuroscience, 4, 148–169.
Talairach, J., & Tournoux, P. (1988). Co-planar steriotaxic atlas of the human brain. New York: Thieme.
Talsma, D., Kok, A., & Ridderinkhof, K. R. (2006). Selective attention to spatial and non-spatial visual stimuli is affected differentially by age: effects on event-related brain potentials and performance data. International Journal of Psychophysiology, 62, 249–261.
van Veen, V., Cohen, J. D., Botvinick, M. M., Stenger, V. A., & Carter, C. S. (2001). Anterior cingulate cortex, conflict monitoring, and levels of processing. NeuroImage, 14, 1302–1308.
Weissman, D. H., Warner, L. M., & Woldorff, M. G. (2004). The neural mechanisms for minimizing cross-modal distraction. Journal of Neuroscience, 24, 10941–10949.
Woodruff, P. W., Benson, R. R., Bandettini, P. A., Kwong, K. K., Howard, R. J., Talavage, T., et al. (1996). Modulation of auditory and visual cortex by selective attention is modality-dependent. NeuroReport, 7, 1909–1913.
Yang, Z., Yeo, R., Pena, A., Ling, J., Klimaj, S., Campbell, R., et al. (2012). A fMRI Study of Auditory Orienting and Inhibition of Return in Pediatric Mild Traumatic Brain Injury. Journal of Neurotrauma.
Acknowledgements
Special thanks to Diana South, George Malloy and Cathy Smith for assistance with data collection, to Reyaad Hayek, M.D. for review of anatomical images, and to Gayle Pohl and her students for generous contributions to help fund this study.
Funding
This work was supported by the National Institutes of Health [R24-HD050836, R21-NS064464-01A1 and 3 R21 NS064464-01 S1 to A.M.].
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Esm 1
(DOC 1110 kb)
Rights and permissions
About this article
Cite this article
Mayer, A.R., Yang, Z., Yeo, R.A. et al. A functional MRI study of multimodal selective attention following mild traumatic brain injury. Brain Imaging and Behavior 6, 343–354 (2012). https://doi.org/10.1007/s11682-012-9178-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-012-9178-z