Abstract
Patients (n = 8) with uncomplicated mild traumatic brain injury (mTBI) underwent serial assessments (4) with diffusion tensor imaging (DTI) and neuropsychological testing within the first 8 days post-injury. Using a multi-case study design, we examined changes in brain parenchyma (via DTI-derived fractional anisotropy [FA], apparent diffusion coefficient [ADC], axial diffusivity [AD] and radial diffusivity [RD] in the left cingulum bundle) and in memory performance (via Hopkins Verbal Learning Test-Revised). Qualitative inspection of the results indicated that memory performance was transiently affected in most participants over the course of the week, with performance most negatively impacted on the second assessment (days 3–4 or 97–144 h post-injury), and then returning to within normal limits by 8 days post-injury. Alternatively, FA and other DTI metrics showed a more complex pattern, with the trajectory of some participants changing more prominently than others. For example, FA transiently increased in some participants over the study period, but the pattern was heterogeneous. Memory performance appeared to mirror changes in FA in certain cases, supporting a pathophysiological basis to memory impairment following mTBI. However, the pattern and the degree of symmetry between FA and memory performance was complex and did not always correspond. Serial imaging over the semi-acute recovery period may be important in reconciling conflicting findings in mTBI utilizing memory and/or DTI. Serial use of imaging modalities including DTI may aid understanding of underlying pathophysiological changes in the semi-acute post-injury period. Should a consistent pattern emerge that allows identification of patients at-risk for acute and/or persistent symptoms, such knowledge could guide development of therapeutic targets in mTBI and in understanding the most effective administration time window for these agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 1.7 million new traumatic brain injuries (TBI) are reported annually in recent years in the United States, with an estimated 75 % of these classified as mild TBI (mTBI) (Faul et al. 2010). Physiological, cognitive and psychiatric symptoms following mTBI have been well documented in some patients with mTBI and concussion, including headaches, sensitivity to light or noises, fatigue, emotional changes and decreased attention, memory, and information processing speed. However, despite the prevalence of mTBI, the degree and persistence of these post-concussive symptoms has been a source of some controversy, as has the relation of these symptoms to any underlying physiologic or parenchymal change in the brain.
Computed tomography (CT) and magnetic resonance imaging (MRI) have been somewhat helpful in the acute diagnosis and prognosis of patients with mild TBI when findings are present (often termed “complicated mild” TBI). However, these conventional imaging techniques are considered to have limited sensitivity in mTBI or concussion, and are frequently unrevealing regardless of clinical presentation. Therefore, there has been substantial recent interest in utilizing advanced imaging methods such as diffusion tensor imaging (DTI) which may be more sensitive to the detection of mTBI-related alterations in brain structure. Several studies have suggested a promising role for DTI as a biomarker of injury at all ranges of severity (Huisman et al. 2004; Sidaros et al. 2008; Perlbarg et al. 2009; Warner et al. 2010; Zappala et al. 2012; Bigler and Bazarian 2010), including mTBI (Mac Donald et al. 2011; Davenport et al. 2012; Ling et al. 2012; Rutgers et al. 2008; Wilde et al. 2008; Niogi et al. 2008a, b; Lipton et al. 2008). However, other studies have not found group differences in groups of subjects with mild TBI using DTI (Levin et al. 2010; Lange et al. 2011).
DTI has been used to probe the integrity of white matter in specific brain areas through common DTI-derived metrics such as fractional anisotropy (FA) and apparent diffusion coefficient (ADC; also referred to as mean diffusivity or MD), axial diffusivity (AD), and radial diffusivity (RD) (Huisman et al. 2004; Alexander et al. 2007). FA has been shown to be related to fiber directionality in white matter as well as anisotropic diffusion, or the tendency of water molecules to move preferentially in parallel (rather than perpendicular) to barriers to free diffusion such as fibers or axons. A high degree of anisotropic diffusion has been shown to be related to homogeneity in fiber orientation, increased fiber density or axonal diameter, and the ratio of intracellular/extracellular space. In the context of semi-acute mTBI, increased FA has also been implicated as a marker for inflammation or cytotoxic edema (Bazarian et al. 2007; Wilde et al. 2008; Mayer et al. 2010; Ling et al. 2012). FA is one of the most commonly reported metric in studies of TBI, though ADC, AD and RD have also been utilized as these metrics are reported to have differential sensitivity to forms of pathology such as inflammation, edema, axonal degeneration, etc. For a full review of DTI in mild TBI, please refer to Shenton et al. (2012), this issue.
Memory functioning has been considered a primary deficit in TBI generally (Bigler 2008), but the results of studies in mTBI regarding persistent memory impairment have again been mixed, with some studies suggesting persistent impairment in memory functioning (McCauley et al. 2005, 2008; Ponsford et al. 2011; King and Kirwilliam 2011), and others finding no difference in comparison to a control cohort (McCrea et al. 2009; Mayer et al. 2010). While memory deficits have traditionally been ascribed to pathology in temporal lobe structures in more severe TBI, other brain regions, such as the cingulate have also been implicated in memory functioning.
The purpose of this study was to capitalize on a unique dataset of uncomplicated mTBI patients who underwent serial DTI and neuropsychological testing within the first 8 days post-injury. Using a multi-case study design, we examined changes in brain parenchyma (via DTI metrics derived in the left cingulum bundle) and in memory performance (using a verbal list-learning task). We hypothesized that alterations would be observed in both DTI metrics and memory performance over the course of the first week post-injury, and that there would be evidence for brain-behavior relations, at least in a subset of participants. The left cingulum bundle was selected as the imaging structure of interest for three primary reasons. First, this structure has demonstrated vulnerability to injury in other studies of TBI using DTI (Bigler et al. 2010; McCauley et al. 2011; Wilde et al. 2010, 2011; Wang et al. 2011), including mTBI (Wu et al. 2010; Niogi et al. 2008a). Additionally, the left cingulum bundle has been associated with verbal memory functioning (Kaneda and Osaka 2008; Wu et al. 2010). Finally, DTI measurement of this structure has been shown to be quite reproducible both between and within raters on quantitative tractography. It also is well-suited for serial measurement since it can be easily identified in multiple imaging planes, and despite changes in head position between scans.
Methods and materials
Participants
This research protocol was approved by the Institutional Review Board of the Baylor College of Medicine and other affiliated institutions involved in this project. Informed consent was obtained from each participant; enrollment through consent of a legally authorized representative was not necessary as all participants had emerged from post-traumatic amnesia (PTA) at the time of screening and enrollment as determined by the administration of the Galveston Orientation and Amnesia Test (GOAT; Levin et al. 1979) with a score of 76 or higher. In the current report, we included data collected as part of a larger study, but restrict this report to only those participants who 1) had useable DTI data at each time point (with the exception of one participant where there were technical difficulties with the DTI on two occasions), 2) whose performance was considered reliable (e.g., out of PTA at the time of testing, no compelling concerns regarding adequate effort on cognitive testing), and 3) who sustained injury in conjunction with a high-velocity mechanism of injury (i.e., motor vehicle crash or all-terrain vehicle accident). The TBI group discussed in this manuscript was composed of 8 participants (5 males and 3 females) between the ages of 18 and 40 years (mean = 24.8 ± 7.5) with a mean of 13 ± 1.9 years of education who sustained “uncomplicated” mTBI as defined by a lowest postresuscitation Glasgow Coma Scale (GCS) score (Teasdale and Jennett 1974) of 13-15. A single participant had a GCS score which very briefly dropped to 12, which is considered a TBI of moderate severity by some definitions. All participants were recruited less than 48 h post-mTBI from consecutive admissions to emergency rooms at three American College of Surgeons Level-I trauma centers in Houston, Texas. The mean Injury Severity Score (ISS) from the Abbreviated Injury Scale (AIS; Committee on Injury Scaling 1998) score for individuals with mTBI was 2.5 ± 1.1 (range 1–6) and the modified ISS (m-ISS; the standard ISS score not including the head region) was 1.0 ± 0.8. The mean loss of consciousness (LOC) based on self-report or report of a reliable witness was 14.1 ± 12.6 min (range 1–30), and the mean duration of PTA, based on medical records and self-report was 55.0 ± 46.8 min (range 0–150). In accordance with our inclusion criteria, no participant was enrolled who had intracranial abnormalities on his or her initial CT scan performed within the emergency department. Other inclusion criteria for entry into the study included having a LOC no greater than 30 min, an AIS < 3 for any body region, and an Injury Severity Scale (ISS) ≤ 12. Exclusion criteria for the study included 1) lack of fluency in English (due to the unavailability of a Spanish version of the memory test used in this study), 2) AIS score greater than 3 for any body region or total ISS score greater than 27 including body parts other than head, 3) acute severe intoxication as determined by clinician and/or laboratory measures at time of examination in the emergency department, 4) previous hospitalization for head injury, 5) pregnancy when screened prior to brain imaging, 6) pre-existing neurologic disorder associated with cerebral dysfunction and/or cognitive deficit (e.g., cerebral palsy, mental retardation, epilepsy, etc.), 7) pre-existing severe psychiatric disorder (e.g., bipolar disorder, schizophrenia), 8) contraindications to undergoing MRI, including metallic implant or marked agitation, and 9) inability to provide fully informed consent. Detailed information for demographic and injury characteristics for each participant is presented in Table 1.
Participants were assessed on four occasions over the first week post-injury using the following time intervals: 1) days 1–2 (0–48 h), 2) days 3–4 (49–96 h), 3) days 5–6 (97–144 h) and 4) days 7–8 (145–192 h). Imaging and administration of the memory test were performed within a 2 h block of time. Study personnel administering the memory measure were blinded to the results of imaging analysis, and those involved in the imaging analysis did not have access to the memory performance data at the time of analysis.
Imaging protocols
All participants underwent MRI without sedation on the same Philips 3.0 Tesla Achieva scanner. Regular quality assurance testing was performed including American College of Radiology (ACR) phantom testing, and no concerns with quality assurance were noted through the course of the study.
The absence of intracranial abnormalities was established via initial day-of-injury CT scanning done as part of standard clinical management. Moreover, these scans were re-reviewed by a second board-certified neuroradiologist on our study to confirm the absence of findings. At the time of the initial DTI acquisition, a T1-weighted sequence, a gradient recalled echo (GRE) sequence, and a fluid attenuated inversion recovery (FLAIR) were also performed and reviewed for evidence of intracranial abnormalities. No additional trauma-related intracranial abnormalities were detected on these sequences.
DTI parameters included an axial single-shot spin-echo echo-planar imaging sequence with 30 diffusion-encoding directions; 256-mm field of view (FOV); acquisition voxel size, 2 × 2 × 2 mm3; repetition time (TR), 11526.0 ms; echo time (TE), 51 ms, sensitivity encoding (SENSE) reduction factor of 2, two B factors with 0 s/mm2, low B, and 1000 s/mm2, high B), with two acquisitions to average the signal of the two DTI scans in order to ensure better signal-to-noise ratio. Acquisitions consisted of 70 slices. A SENSE 8-channel head coil was used.
Image processing
A multiple region of interest (ROI) approach to DTI tractography was applied. Using the sagittal plane, the posterior slice was identified as the one just anterior to the splenium of the corpus callosum. Transposing the view to the coronal plane, all visible aspects of the cingulum bundle were included in the first ROI. The anterior slice was again selected using the sagittal plane as the slice immediately posterior to the genu of the corpus callosum. In the coronal plane, the cingulum bundle was again identified and used as the second ROI. Automated tractography was applied utilizing these two ROIs to determine the tract, and FA, ADC, AD and RD of the tract were generated. DTI metrics were calculated as the average of all points identified along the cingulum bundle.
All DTI data was analyzed twice by a single rater to establish intra-rater reliability using intra-class correlational coefficients (ICCs). A subset of the images was analyzed by two raters to establish inter-rater reliability. ICCs for all measurements were above 0.95.
Cognitive testing
Given the need for a memory measure with sufficient multiple equivalent forms for this study design, the Hopkins Verbal Learning Test-Revised (HVLT-R; Frey 2003) was selected. The HVLT-R is a word list memory test which includes three learning trials followed 25 min later by free recall and recognition trials. The order of the equivalent versions of the HVLT-R was counterbalanced by participant through a prepared randomization schedule to prevent confounding test occasion with test version. In this report, total recall (age-corrected T-score) was the variable of interest. Delayed free recall was not included as a variable of interest given its comparative restriction in range attenuating its sensitivity.
Results
The small sample size prevents a meaningful parametric analysis, but the uniqueness of the sample provides an opportunity to descriptively characterize performance over the first week following mTBI. As demonstrated in Fig. 1, at the lowest ebb of memory performance, 7 of the 8 participants had age-corrected T-scores that declined to at least one standard deviation below either their initial assessment level, or at the peak of their recovery. While admittedly this is not a particularly sophisticated method of determining significant change in a single patient (Ker et al. 2008), it is a rule-of-thumb method often used in clinical practice. Additionally, changes in cognitive performance following mTBI have frequently been reported as subtle when found (Lange et al. 2009; Stapert et al. 2006), complicating the selection of the most appropriate method to determine significant change over time. The normal range of functioning is depicted in Fig. 1 with dashed lines indicating one standard deviation about the mean age-corrected T-score of 50. It should be noted that 5 of the 8 had scores within normal limits at their initial assessment and all but 1 participant rebounded to this average level of performance by the end of the first week. If memory impairment was defined as a score of 1.5 standard deviations or more below the mean, as is commonly used in studies of mTBI (McCauley et al. 2008), and mild cognitive impairment (Petersen 2004), 3 participants (38 %) met this criterion at Day 1–2, 5 (63 %) at Day 3–4, 3 (38 %) at Day 5–6, and none at Day 7–8. As a more stringent test of the decrease in memory performance, the reliable change index (RCI; Jacobsen and Truax 1991) was calculated based on normative data obtained from 1 week test-retest intervals reported by Benedict et al. (Benedict et al. 1998). Using this procedure, 5 of 8 (63 %) of the participants had differences in raw scores between Day 1–2 until their lowest performance that exceeded the RCI. This result is particularly interesting because reliable change (i.e., a decline in this case) was found in spite of practice effects that may have accrued potentially offsetting this decline.
Line graph depicting the performance of each participant over the four assessment occasions within 8 days post-injury on the Hopkins Verbal Learning Test – Revised. Scores are presented as age-corrected T-scores with a mean of 50 and a standard deviation of 10. A standard deviation above and below the mean is represented with a dotted line
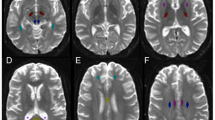
As can be seen in Fig. 2a, acute increases in FA of the left cingulum bundle occurred at varying time points during the first week. Similar increases in FA during the semi-acute phase post-mTBI have been reported (Wilde et al. 2008; Mayer et al. 2010; Bazarian et al. 2007; Ling et al. 2012). This variation in pattern of FA increases may reflect the heterogeneity of each participant’s injury even though the general mechanism was similar in each case (i.e., rapid acceleration/deceleration in a motor vehicle crash). Comparison of the trajectories of ADC, AD and RD measures for each participant (see Fig. 2b–d) further highlights the complex nature of change as measured by DTI as there is considerable difference in the patterns between each metric, at least from a qualitative perspective. Some of these metrics indicate more prominent change within each individual, but the pattern of change is complicated and varies by the metric used.
To illustrate potential connection between alterations in DTI metrics and verbal memory performance, two participants from our sample were selected. Relevant clinical history is detailed below in the vignettes.
Vignette 1
Participant 001 is 25 year-old male with a high school diploma, employed as a construction worker at the time of injury. This man was involved in a motor vehicle crash at highway speeds, in which he struck his head on the windshield. He was restrained. He suffered lacerations to his head and face and also injured his shoulder; the AIS score was 3. Paramedics measured his initial GCS score as 15, and LOC for a period of approximately 5 min was reported. Participant 001 also reported a significant duration of PTA—2.5 h. In terms of post-concussive symptoms, the patient primarily reported impaired memory and decreased processing speed. He reported that these persisted somewhat through the first week after injury but resolved after 1 month (though the patient began reporting significant sleep impairment at this time). This individual was not involved in litigation and returned to work 1 month after the injury.
Vignette 2
Participant 005 is an 18 year-old female senior in high school (11 years of education). She is a student and unemployed. She was involved in a motor vehicle crash when the car she was riding in hydroplaned at approximately 55 miles per hour. She was a restrained passenger, but leaned over to restrain the driver (who was not wearing a seat belt) and so struck her head on the windshield. Paramedics noted the windshield was broken where this young lady’s head made impact, and recorded her initial GCS to be 14 (she did not spontaneously open her eyes). The AIS score was 2. This individual reportedly lost consciousness for 25 min following the impact and family members reported post-traumatic amnesia lasting 60 min. At her first evaluation, this patient reported intense headaches, dizziness and nausea, hypersomnia, emotional changes such as increased irritability and depression, decreased processing speed, poor memory, sensitivity to light and sound, and increased anxiety. These symptoms persisted for months after the injury. She did not return to school until 3 months post-injury. This individual was also not involved in litigation.
As can be seen in Fig. 3a, participant 001 reached a local minimum on memory performance at about 65 h postinjury and later recovered to within the normal range by 166 h. At these same time points, there was a local peak in the FA at about 65 h and a sharp decline following (Fig. 3b). In contrast to this relatively “early” pattern of declining memory performance and a mirror pattern of increasing FA, participant 005 demonstrated a “late” developing pattern. Here, memory performance reached a local minimum at about 124 h while FA gradually increased reaching a local peak at that same time point followed by some resolution on both measures.
a–b Panel a shows the performance of two participants (001 in black and 005 in blue) on the Hopkins Verbal Learning Test – Revised. Time post-injury is indicated on the abscissa. Both participants demonstrate a notable decrease in performance followed by an increase, though this occurs earlier for 001 than for 005. Panel b illustrates the measurement of fractional anisotropy (FA) in these two participants. Comparison of FA with the HVLT-R total recall age-corrected T-score reveals a mirror pattern of these two variables for each participant
Discussion
This study represents the first prospective serial examination of DTI in the left cingulum bundle and memory utilizing four assessments over the first week post-injury in a small sample of uncomplicated mild TBI participants. Our intention was to explore the trajectory of change for both DTI metrics and memory performance in a subset of study participants who were injured as a result of relatively high-velocity motor vehicle crashes (MVC). Qualitative inspection of the results indicates that performance on verbal list-learning was transiently affected in the majority of participants, with performance most negatively impacted on the second testing occasion (days 3–4 or 97–144 h post-injury), and then returning to within normal limits. On the other hand, FA in the left cingulum bundle showed a more complex pattern, with the trajectory of changes in some participants changing more prominently than in others. Memory performance did appear to mirror changes in FA in the cases highlighted in the vignettes, but the pattern and the degree of symmetry between FA and memory did not necessarily correspond in all cases.
It is widely assumed that many patients with mTBI or concussion may exhibit transient symptoms that spontaneously and apparently completely resolve within 2–14 days post-injury from sports-related concussions (Covassin et al. 2010; Iverson et al. 2006; Sim et al. 2008; McCrea et al. 2003; Thomas et al. 2011; Iverson 2005) and up to 3 months following other mechanisms of injury (Kwok et al. 2008) though a subset of patients may exhibit persistent post-concussive symptoms beyond 3 months post-injury (McCauley et al. 2001, 2005, 2008; Ruff et al. 1996; Lannsjo et al. 2009; Sterr et al. 2006; King and Kirwilliam 2011). The results of this preliminary study are consistent in pattern with a previous investigation of memory functioning following mTBI that also used the HVLT-R (Bruce and Echemendia 2003) and suggest that the disturbance in memory performance may indeed be short-lived in some patients, though we emphasize that this examination was limited to 8 days post-injury, and cannot address the trajectory of memory performance beyond that time. In addition to various neurologic factors inherent in the heterogeneity of TBI, we acknowledge that factors such as sleep disruption, pain, pain medication use, and stress could potentially also be contributory to small declines in memory performance during the semi-acute recovery interval.
Similarly, the changes in DTI-related metrics indicate some perturbation of microstructure in the semi-acute recovery interval, though these do not appear to be consistent in nature or degree across the sample presented in this study. Unfortunately, current limitations of DTI include the lack of normative data and inconsistencies in the specifics of acquisition and analysis which preclude direct comparison of the results across studies (see Hunter et al. 2012 for further detail). Therefore, at this time, we do not have sufficient information to determine whether the degree of FA (or other DTI metric) alteration detected in this study reflects any clinically meaningful change. While we carefully examined the inter- and intra-rater reliability of DTI measurements reported in this study, the degree of expected error in serial measurement in DTI remains incompletely determined. Patterns of DTI change may differ in other brain regions and using additional forms of DTI analysis, and this warrants further investigation. We also acknowledge that there remain substantial gaps in what we currently know about the specificity of each DTI metric in measurement of underlying neuropathology in mTBI, or how competing pathological influences in mTBI (e.g., inflammation versus direct axonal pathology) may differentially affect each metric. Clearly, this is a complex issue that requires further study. Finally, we acknowledge that the profile pattern and consistency may be different for report of other post-concussive symptoms or for other cognitive abilities such as processing speed, executive functioning, prospective memory, and other measures of outcome, and these will be the focus of future studies.
While we have included four assessments over a week, our knowledge of the exact nature, degree, and time course of disturbance in the recovery curves is still incomplete. For example, it is possible that our design may still have missed transient but more extreme disturbances in some participants that were not apparent because of the specific timing of their evaluations. Nevertheless, this study highlights the presence of fluctuations that occur over the first week following injury. It is possible that such fluctuations in both cognitive performance and DTI-derived metrics contribute to the seemingly conflicting results that have been found in other studies of mTBI. For example, some studies have failed to find differences between mTBI patient groups and controls using DTI, and those that do report differences have failed to reach a consensus regarding the direction of DTI-related changes and the degree to which these may be related to cognition.
We emphasize that the sample of patients in this report generally presented with a history of LOC and significant PTA, but no intracranial abnormalities on CT or MRI. The patterns of memory performance and DTI metrics presented in this report may differ for patients with greater or lesser injury severity or with focal lesions. Additionally, we intentionally restricted our analyses to motor vehicle crashes. Despite including only participants with injuries resulting from a seemingly homogeneous mechanism of injury, each case likely has its own unique features in the precise mechanism and site(s) of injury. We acknowledge that the pattern of memory and DTI-related changes may differ for patients with milder mTBI or TBI resulting from differing injury mechanisms (e.g., low-velocity injury, sport-related injury, blast-related injury). Finally, we acknowledge that there may be other injury- and host-related factors that must be considered in recovery from mTBI (e.g., age, gender, genetic and constitutional contributors, pre-existing emotional disturbances, brain reserve, etc.) and the interplay between injury and these other factors remains a complex issue.
The sample size is a shortcoming of this investigation, but the uniqueness of sequential scanning and cognitively assessing patients with mTBI over the first 8 days post-injury provides important insights into the fluctuation of DTI metrics in conjunction with neurocognitive functioning in the first week post-injury. Because of these limitations, our findings are preliminary, and we provide mostly descriptive observations; further investigation in a larger sample studied over a longer post-acute time frame is warranted.
DTI has some inherent limitations (see Shenton et al. 2012), and we emphasize that DTI provides information about structural alterations rather than direct functional consequences of mTBI or concussion, which may be better assessed by other advanced imaging modalities. At present, our knowledge about what specific DTI metrics reveal about underlying pathophysiology remains incomplete and requires additional study. We selected the left cingulum, a region that is less prone to measurement error and is readily identifiable using DTI methods, and which is also considered vulnerable to injury and relevant to memory functioning. Whether similar DTI fluctuations occur in other critical brain structures essential to short-term memory functioning and that may be disrupted by mTBI is not known and should also be investigated. There are also issues regarding the short re-test intervals for memory assessment. Although potential practice effects accruing from frequent exposure to the same memory procedure could not have been controlled effectively (if at all), practice effect due to repeated exposure to the same stimuli was controlled for with the use of multiple equivalent (alternate) forms. Based on a study by Benedict and Zgaljardic (1998), raw scores were nearly identical using a two week test-retest interval and alternate forms; similar data regarding alternate form equivalence and reliability coefficients were reported using a 1 week interval by Benedict et al. (1998); however, no data could be located involving the approximately two-day interval used in the present study and therefore, the level of practice effects using alternate forms remains unknown.
Conclusions
The current investigation shows that DTI and neurocognitive changes post mTBI occur in concert in some patients with semi-acute elevations of FA and other metrics and corresponding decreases in performance on memory testing followed by normalization of both measures by the end of the 8-day examination. However, this relation is complex. While there was some consistency in the shape and time of the trajectory of decreased memory performance generally occurring at the second assessment, the DTI-related changes were far less consistent, and the relation between memory performance and FA was also inconsistent. This investigation is the first to document temporally consistent fluctuations this semi-acute time frame in both performance on a memory task and FA in two cases, supporting a pathophysiological basis to short-term memory impairment in mTBI in these individuals. Detailed serial imaging over the semi-acute recovery period may be important in better reconciling some of the conflicting findings in mild TBI utilizing memory and/or DTI. The serial use of imaging modalities such as DTI may also allow a better understanding of the underlying pathophysiological changes in the semi-acute post-injury period. Should a consistent pattern emerge that allows identification of patients at-risk for acute and/or persistent symptoms, such knowledge would be critical in guiding development of therapeutic targets in mTBI and in understanding the time window when agents are likely to be most effective.
References
Alexander, A. L., Lee, J. E., Lazar, M., & Field, A. S. (2007). Diffusion tensor imaging of the brain. Neurotherapeutics, 4(3), 316–329.
Bazarian, J. J., Zhong, J., Blyth, B., Zhu, T., Kavcic, V., & Peterson, D. (2007). Diffusion tensor imaging detects clinically important axonal damage after mild traumatic brain injury: a pilot study. [Research Support, N.I.H., ExtramuralResearch Support, Non-U.S. Gov't]. Journal of Neurotrauma, 24(9), 1447–1459. doi:10.1089/neu.2007.0241.
Benedict, R. H., Schretlen, D., Groninger, L., & Brandt, J. (1998). Hopkins verbal learning test – revised: normative data and analysis of inter-form and test-retest reliability. Clinical Neuropsychology, 12(1), 43–55.
Benedict, R. H., & Zgaljardic, D. J. (1998). Practice effects during repeated administrations of memory tests with and without alternate forms. [Clinical Trial]. Journal of Clinical and Experimental Neuropsychology, 20(3), 339–352. doi:10.1076/jcen.20.3.339.822.
Bigler, E. D. (2008). Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. Journal of the International Neuropsychological Society, 14(1), 1–22. doi:10.1017/S135561770808017X.
Bigler, E. D., & Bazarian, J. J. (2010). Diffusion tensor imaging: a biomarker for mild traumatic brain injury? [Comment Editorial]. Neurology, 74(8), 626–627. doi:10.1212/WNL.0b013e3181d3e43a.
Bigler, E. D., McCauley, S. R., Wu, T. C., Yallampalli, R., Shah, S., MacLeod, M., et al. (2010). The temporal stem in traumatic brain injury: preliminary findings. [Comparative Study In Vitro Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Brain Imaging Behav, 4(3–4), 270–282. doi:10.1007/s11682-010-9105-0.
Bruce, J. M., & Echemendia, R. J. (2003). Delayed-onset deficits in verbal encoding strategies among patients with mild traumatic brain injury. [Research Support, Non-U.S. Gov't]. Neuropsychology, 17(4), 622–629. doi:10.1037/0894-4105.17.4.622.
Committee on Injury Scaling. (1998). Abbreviated Injury Scale. Arlington Heights: Association for the Advancement of Automotive Medicine.
Covassin, T., Elbin, R. J., & Nakayama, Y. (2010). Tracking neurocognitive performance following concussion in high school athletes. [Research Support, Non-U.S. Gov't]. The Physician and Sportsmedicine, 38(4), 87–93. doi:10.3810/psm.2010.12.1830.
Davenport, N. D., Lim, K. O., Armstrong, M. T., & Sponheim, S. R. (2012). Diffuse and spatially variable white matter disruptions are associated with blast-related mild traumatic brain injury. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.]. Neuroimage, 59(3), 2017–2024. doi:10.1016/j.neuroimage.2011.10.050.
Faul, M., Xu, L., Wald, M. M., & Coronado, V. G. (2010). Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control.
Frey, L. C. (2003). Epidemiology of posttraumatic epilepsy: a critical review. Epilepsia, 44(Suppl 10), 11–17.
Huisman, T. A., Schwamm, L. H., Schaefer, P. W., Koroshetz, W. J., Shetty-Alva, N., Ozsunar, Y., et al. (2004). Diffusion tensor imaging as potential biomarker of white matter injury in diffuse axonal injury. [Research Support, U.S. Gov't, P.H.S.]. AJNR Am J Neuroradiol, 25(3), 370–376.
Hunter, J. V., Wilde, E. A., Tong, K. A., & Holshouser, B. A. (2012). Emerging imaging tools for use with traumatic brain injury research. [Research Support, N.I.H., Extramural Research Support, U.S. Gov't, Non-P.H.S.]. Journal of Neurotrauma, 29(4), 654–671, doi:10.1089/neu.2011.1906.
Iverson, G. L. (2005). Outcome from mild traumatic brain injury. Current Opinion in Psychiatry, 18(3), 301–317. doi:10.1097/01.yco.0000165601.29047.ae.
Iverson, G. L., Brooks, B. L., Collins, M. W., & Lovell, M. R. (2006). Tracking neuropsychological recovery following concussion in sport. Brain Injury: [BI], 20(3), 245–252. doi:10.1080/02699050500487910.
Jacobsen, N. S., & Truax, P. (1991). Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19.
Kaneda, M., & Osaka, N. (2008). Role of anterior cingulate cortex during semantic coding in verbal working memory. [Research Support, Non-U.S. Gov't]. Neurosci Lett, 436(1), 57–61. doi:10.1016/j.neulet.2008.02.069.
Ker, K., Perel, P., Blackhall, K., & Roberts, I. (2008). How effective are some common treatments for traumatic brain injury? BMJ, 337, a865.
King, N. S., & Kirwilliam, S. (2011). Permanent post-concussion symptoms after mild head injury. Brain Injury: [BI], 25(5), 462–470. doi:10.3109/02699052.2011.558042.
Kwok, F. Y., Lee, T. M., Leung, C. H., & Poon, W. S. (2008). Changes of cognitive functioning following mild traumatic brain injury over a 3-month period. [Multicenter Study Research Support, Non-U.S. Gov't]. Brain Injury: [BI], 22(10), 740–751. doi:10.1080/02699050802336989.
Lange, R. T., Iverson, G. L., Brubacher, J. R., Madler, B., & Heran, M. K. (2011). Diffusion tensor imaging findings are not strongly associated with postconcussional disorder 2 months following mild traumatic brain injury. The Journal of Head Trauma Rehabilitation. doi:10.1097/HTR.0b013e318217f0ad.
Lange, R. T., Iverson, G. L., & Franzen, M. D. (2009). Neuropsychological functioning following complicated vs. uncomplicated mild traumatic brain injury. Brain Injury: [BI], 23(2), 83–91. doi:10.1080/02699050802635281.
Lannsjo, M., af Geijerstam, J. L., Johansson, U., Bring, J., & Borg, J. (2009). Prevalence and structure of symptoms at 3 months after mild traumatic brain injury in a national cohort. [Multicenter Study Research Support, Non-U.S. Gov't]. Brain Injury: [BI], 23(3), 213–219. doi:10.1080/02699050902748356.
Levin, H. S., O'Donnell, V. M., & Grossman, R. G. (1979). The Galveston Orientation and Amnesia Test. A practical scale to assess cognition after head injury. Journal of Nervous and Mental Disease, 167(11), 675–684.
Levin, H. S., Wilde, E., Troyanskaya, M., Petersen, N. J., Scheibel, R., Newsome, M., et al. (2010). Diffusion tensor imaging of mild to moderate blast-related traumatic brain injury and its sequelae. Journal of Neurotrauma, 27(4), 683–694. doi:10.1089/neu.2009.1073.
Ling, J. M., Pena, A., Yeo, R. A., Merideth, F. L., Klimaj, S., Gasparovic, C., et al. (2012). Biomarkers of increased diffusion anisotropy in semi-acute mild traumatic brain injury: a longitudinal perspective. Brain, 135(Pt 4), 1281–1292. doi:10.1093/brain/aws073.
Lipton, M. L., Gellella, E., Lo, C., Gold, T., Ardekani, B. A., Shifteh, K., et al. (2008). Multifocal white matter ultrastructural abnormalities in mild traumatic brain injury with cognitive disability: a voxel-wise analysis of diffusion tensor imaging. Journal of Neurotrauma, 25(11), 1335–1342. doi:10.1089/neu.2008.0547.
Mac Donald, C. L., Johnson, A. M., Cooper, D., Nelson, E. C., Werner, N. J., Shimony, J. S., et al. (2011). Detection of blast-related traumatic brain injury in U.S. military personnel. [Research Support, N.I.H., Extramural Research Support, U.S. Gov't, Non-P.H.S.]. N Engl J Med, 364(22), 2091–2100. doi:10.1056/NEJMoa1008069.
Mayer, A. R., Ling, J., Mannell, M. V., Gasparovic, C., Phillips, J. P., Doezema, D., et al. (2010). A prospective diffusion tensor imaging study in mild traumatic brain injury. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Neurology, 74(8), 643–650. doi:10.1212/WNL.0b013e3181d0ccdd.
McCauley, S. R., Boake, C., Levin, H. S., Contant, C. F., & Song, J. X. (2001). Postconcussional disorder following mild to moderate traumatic brain injury: anxiety, depression, and social support as risk factors and comorbidities. [Comparative Study Research Support, U.S. Gov't, P.H.S.]. Journal of Clinical and Experimental Neuropsychology, 23(6), 792–808.
McCauley, S. R., Boake, C., Pedroza, C., Brown, S. A., Levin, H. S., Goodman, H. S., et al. (2005). Postconcussional disorder: Are the DSM-IV criteria an improvement over the ICD-10? [Comparative Study Research Support, U.S. Gov't, P.H.S.]. The Journal of Nervous and Mental Disease, 193(8), 540–550.
McCauley, S. R., Boake, C., Pedroza, C., Brown, S. A., Levin, H. S., Goodman, H. S., et al. (2008). Correlates of persistent postconcussional disorder: DSM-IV criteria versus ICD-10. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. J Clin Exp Neuropsychol, 30(3), 360–379. doi:10.1080/13803390701416635.
McCauley, S. R., Wilde, E. A., Bigler, E. D., Chu, Z., Yallampalli, R., Oni, M. B., et al. (2011). Diffusion tensor imaging of incentive effects in prospective memory after pediatric traumatic brain injury. [Research Support, N.I.H., Extramural]. Journal of Neurotrauma, 28(4), 503–516. doi:10.1089/neu.2010.1555.
McCrea, M., Guskiewicz, K. M., Marshall, S. W., Barr, W., Randolph, C., Cantu, R. C., et al. (2003). Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. [Research Support, Non-U.S. Gov't]. JAMA: the Journal of the American Medical Association, 290(19), 2556–2563. doi:10.1001/jama.290.19.2556.
McCrea, M., Iverson, G. L., McAllister, T. W., Hammeke, T. A., Powell, M. R., Barr, W. B., et al. (2009). An integrated review of recovery after mild traumatic brain injury (MTBI): implications for clinical management. [Review]. Clin Neuropsychol, 23(8), 1368–1390. doi:10.1080/13854040903074652.
Niogi, S. N., Mukherjee, P., Ghajar, J., Johnson, C., Kolster, R. A., Sarkar, R., et al. (2008a). Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. [Research Support, Non-U.S. Gov't]. AJNR Am J Neuroradiol, 29(5), 967–973. doi:10.3174/ajnr.A0970.
Niogi, S. N., Mukherjee, P., Ghajar, J., Johnson, C. E., Kolster, R., Lee, H., et al. (2008b). Structural dissociation of attentional control and memory in adults with and without mild traumatic brain injury. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.]. Brain, 131(Pt 12), 3209–3221. doi:10.1093/brain/awn247.
Perlbarg, V., Puybasset, L., Tollard, E., Lehericy, S., Benali, H., & Galanaud, D. (2009). Relation between brain lesion location and clinical outcome in patients with severe traumatic brain injury: a diffusion tensor imaging study using voxel-based approaches. Human Brain Mapping, 30(12), 3924–3933. doi:10.1002/hbm.20817.
Petersen, R. C. (2004). Mild cognitive impairment as a diagnostic entity. [Research Support, U.S. Gov't, P.H.S. Review]. Journal of Internal Medicine, 256(3), 183–194. doi:10.1111/j.1365-2796.2004.01388.x.
Ponsford, J., Cameron, P., Fitzgerald, M., Grant, M., & Mikocka-Walus, A. (2011). Long term outcomes after uncomplicated mild traumatic brain injury: a comparison with trauma controls. Journal of Neurotrauma. doi:10.1089/neu.2010.1516.
Ruff, R. M., Camenzuli, L., & Mueller, J. (1996). Miserable minority: emotional risk factors that influence the outcome of a mild traumatic brain injury. [Case Reports]. Brain Injury: [BI], 10(8), 551–565.
Rutgers, D. R., Toulgoat, F., Cazejust, J., Fillard, P., Lasjaunias, P., & Ducreux, D. (2008). White matter abnormalities in mild traumatic brain injury: a diffusion tensor imaging study. [Comparative Study Research Support, Non-U.S. Gov't]. AJNR Am J Neuroradiol, 29(3), 514–519. doi:10.3174/ajnr.A0856.
Shenton, M. E., Hamoda, H. M., Schneiderman, J. S., Bouix, S., Pasternak, O., Rathi, Y., et al. (2012). A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging and Behavior. doi:10.1007/s11682-012-9156-5.
Sidaros, A., Engberg, A. W., Sidaros, K., Liptrot, M. G., Herning, M., Petersen, P., et al. (2008). Diffusion tensor imaging during recovery from severe traumatic brain injury and relation to clinical outcome: a longitudinal study. [Research Support, Non-U.S. Gov't]. Brain, 131(Pt 2), 559–572. doi:10.1093/brain/awm294.
Sim, A., Terryberry-Spohr, L., & Wilson, K. R. (2008). Prolonged recovery of memory functioning after mild traumatic brain injury in adolescent athletes. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.]. Journal of Neurosurgery, 108(3), 511–516. doi:10.3171/JNS/2008/108/3/0511.
Stapert, S., Houx, P., de Kruijk, J., Ponds, R., & Jolles, J. (2006). Neurocognitive fitness in the sub-acute stage after mild TBI: the effect of age. Brain Injury: [BI], 20(2), 161–165. doi:10.1080/02699050500442949.
Sterr, A., Herron, K. A., Hayward, C., & Montaldi, D. (2006). Are mild head injuries as mild as we think? Neurobehavioral concomitants of chronic post-concussion syndrome. [Research Support, Non-U.S. Gov't]. BMC Neurology, 6, 7. doi:10.1186/1471-2377-6-7.
Teasdale, G., & Jennett, B. (1974). Assessment of coma and impaired consciousness. A pratical scale. Lancet, 13(7872), 81–84.
Thomas, D. G., Collins, M. W., Saladino, R. A., Frank, V., Raab, J., & Zuckerbraun, N. S. (2011). Identifying neurocognitive deficits in adolescents following concussion. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 18(3), 246–254. doi:10.1111/j.1553-2712.2011.01015.x.
Wang, J. Y., Bakhadirov, K., Abdi, H., Devous, M. D., Sr., Marquez de la Plata, C. D., Moore, C., et al. (2011). Longitudinal changes of structural connectivity in traumatic axonal injury. [Comparative Study Research Support, N.I.H., Extramural Research Support, U.S. Gov't, Non-P.H.S.]. Neurology, 77(9), 818–826. doi:10.1212/WNL.0b013e31822c61d7.
Warner, M. A., Marquez de la Plata, C., Spence, J., Wang, J. Y., Harper, C., Moore, C., et al. (2010). Assessing spatial relationships between axonal integrity, regional brain volumes, and neuropsychological outcomes after traumatic axonal injury. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.]. Journal of Neurotrauma, 27(12), 2121–2130. doi:10.1089/neu.2010.1429.
Wilde, E. A., McCauley, S. R., Hunter, J. V., Bigler, E. D., Chu, Z., Wang, Z. J., et al. (2008). Diffusion tensor imaging of acute mild traumatic brain injury in adolescents. Neurology, 70(12), 948–955. doi:10.1212/01.wnl.0000305961.68029.54.
Wilde, E. A., Newsome, M. R., Bigler, E. D., Pertab, J., Merkley, T. L., Hanten, G., et al. (2011). Brain imaging correlates of verbal working memory in children following traumatic brain injury. [Research Support, N.I.H., Extramural]. Int J Psychophysiol, 82(1), 86–96. doi:10.1016/j.ijpsycho.2011.04.006.
Wilde, E. A., Ramos, M. A., Yallampalli, R., Bigler, E. D., McCauley, S. R., Chu, Z., et al. (2010). Diffusion tensor imaging of the cingulum bundle in children after traumatic brain injury. Developmental Neuropsychology, 35(3), 333–351. doi:10.1080/87565641003696940.
Wu, T. C., Wilde, E. A., Bigler, E. D., Yallampalli, R., McCauley, S. R., Troyanskaya, M., et al. (2010). Evaluating the relationship between memory functioning and cingulum bundles in acute mild traumatic brain injury using diffusion tensor imaging. Journal of Neurotrauma, 27(2), 303–307. doi:10.1089/neu.2009.1110.
Zappala, G., Thiebaut de Schotten, M., & Eslinger, P. J. (2012). Traumatic brain injury and the frontal lobes: what can we gain with diffusion tensor imaging? [Research Support, Non-U.S. Gov't]. Cortex, 48(2), 156–165. doi:10.1016/j.cortex.2011.06.020.
Acknowledgements
This work was supported by the National Institute of Neurological Disorders and Stroke grant 1R03NS069943-01 (“Diffusion Tensor Imaging of Acute and Subacute Mild TBI”; Wilde and McCauley, Co-PIs). We gratefully acknowledge the contribution of Ponnada Narayana, Ph.D. and Vipulkumar S. Patel in implementation and execution of the imaging sequences. We would also like to thank Melisa L. Frisby, MSN, Reni Varghese, and Hector M. Garza for their support and assistance in patient recruitment. We thank the participants and their families for their participation in this research. Finally, we wish to thank the anonymous reviewers of this manuscript for their thoughtful insights and suggestions. None of the authors have any financial or other relationship(s) that could be construed as a conflict of interest with respect to the content of this manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Elisabeth A. Wilde and Stephen R. McCauley contributed equally to this work and wish to be considered co-first authors.
This project was supported by grant number 1R03NS069943-01 from the National Institute of Neurological Disorders and Stroke. Portions of this study were presented at the 29th annual meeting of the National Neurotrauma Symposium, Ft. Lauderdale, Florida, June, 2011.
Rights and permissions
About this article
Cite this article
Wilde, E.A., McCauley, S.R., Barnes, A. et al. Serial measurement of memory and diffusion tensor imaging changes within the first week following uncomplicated mild traumatic brain injury. Brain Imaging and Behavior 6, 319–328 (2012). https://doi.org/10.1007/s11682-012-9174-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-012-9174-3