Abstract
Summary
Age-specific intervention and assessment thresholds based on FRAX® were developed for eight Eurasian countries participating in the EVA study (Armenia, Belarus, Georgia, Moldova, Kazakhstan, the Kyrgyz Republic, the Russian Federation, and Uzbekistan). The intervention thresholds (major osteoporotic fracture) ranged from 3.6 (Armenia and Georgia) to 12.3% (Uzbekistan) for people at age 50 years, and from 16 (Armenia) to 27% (Belarus) at the age of 90 years. These thresholds enable a substantial advance in the ease of detection of individuals at high fracture risk.
Introduction
The purpose of this study was to derive and compare FRAX-based intervention and BMD assessment thresholds for 8 Eurasian countries in the EVA study.
Methods
The intervention threshold (IT) was set at a 10-year probability of a major osteoporotic fracture (MOF), calculated without BMD, equivalent to a woman with a prior fragility fracture but no other clinical risk factors, and a body mass index (BMI) of 25.0 kg/m2. The lower assessment threshold was set at a 10-year probability of a MOF in women with BMI of 25.0 kg/m2, without previous fracture or other clinical risk factors. The upper assessment threshold was set at 1.2 times the IT.
Results
The age-specific intervention thresholds ranged from 3.6 (Armenia and Georgia) to 12.3% (Uzbekistan) for men and women at the age of 50 years and from 16 (Armenia) to 27% (Belarus) at the age of 90 years. The difference between countries was most evident at younger ages and become progressively less with advancing age.
Conclusions
For the 8 Eurasian countries, the newly established FRAX-based intervention thresholds provide an opportunity to improve the clinical detection of both men and women with a high risk of fracture and improve treatment rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis fracture risk assessment is being increasingly established as a critical part of clinical practice worldwide to enable access to a wide range of highly effective treatments which reduce fracture risk [1, 2]. The Fracture Risk Assessment (FRAX®) tool, launched in 2008 by the then WHO Collaborating Centre for Metabolic Bone Disease at the University of Sheffield (UK) [3], has become the most widely used algorithm for assessing this risk [4]. Within FRAX, each country/territory model is based on local fracture epidemiology and risk of death; fracture risks, like death risks, are taken from national sources where possible and, if not, from regional sources. Seven clinical risk factors incorporated into the FRAX tool, along with age and body mass index (BMI), allow clinicians to calculate the 10-year probability of either a hip fracture alone or a major osteoporotic fracture (MOF; distal forearm, hip, clinical spine, or proximal humeral fracture). The model can be used with or without femoral neck bone mineral density (BMD), which is important in settings, both in primary and secondary care, where such measurement may not be readily available.
The Multicenter Multinational population-based Study in Eurasian Countries (EVA study or ЭBA, in Russian) aimed to provide epidemiological information on fracture incidence for selected Eurasian countries so that FRAX models could be created. Authentic FRAX models were developed for Armenia [5], Belarus [6], Kazakhstan [7], Moldova [8], Russia [9], and Uzbekistan [10]. In addition, surrogate FRAX models were developed for Georgia [11] (based on epidemiology of hip fracture in Armenia) and the Kyrgyz Republic [12] (based on Kazakhstan hip fracture rates). The FRAX models indicated that the lifetime hip fracture risk in people at the age of 50 years was highest in Uzbekistan (14.7 and 8.7% for women and men, respectively) and in Kazakhstan (12.6 and 6% for women and men, respectively) [7, 10]. The lowest lifetime hip fracture probability was observed in Armenia (5.9% for women and 2.4% for men) [5]. However, the lack of specific assessment and intervention thresholds limits the current use of the FRAX tool in clinical practice in these countries.
The aim of the present study was to develop FRAX assessment and intervention thresholds for Armenia, Belarus, Georgia, Moldova, Kazakhstan, the Kyrgyz Republic, the Russian Federation, and Uzbekistan in order to enhance clinical management through the wider use of the FRAX tool to appropriately identify high risk and increase access to licensed treatments.
Methods
The setting of intervention and assessment thresholds followed the methodology described first for the UK [13] and subsequently adopted by the National Osteoporosis Guideline Group (NOGG) [14] and endorsed by the National Institute for Health and Care Excellence (NICE) [15]. The premise within the method is summarized briefly; in postmenopausal women with a prior fragility fracture, treatment should be considered without necessarily the need for a BMD test. Thus, if patients with a prior fragile fracture require a long-term intervention to prevent the next fracture, individuals without a fracture but with a similar risk value calculated by FRAX should also be eligible for preventive medical care.
Accordingly, the intervention threshold in the present study was defined as a 10-year probability of osteoporotic fracture, calculated without knowledge of femoral neck BMD, in a woman with a previous fracture and a body mass index (BMI) of 25.0 kg/m2 without other clinical risk factors [13]. The threshold probabilities were country- and age-specific. The threshold level for men had the same value since the efficacy and cost-effectiveness of intervention in men is broadly similar to that in women for an equivalent risk [16, 17]. This definition of an intervention threshold value is consistent with the current guidelines for the diagnosis and treatment of osteoporosis in postmenopausal women published in 2017 by the Russian Osteoporosis Association (RAO) [18].
The NOGG osteoporosis management strategy considers two additional thresholds that were adopted for each of the eight countries of interest:
-
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold). This was set as the age-specific fracture probability for a woman with BMI of 25.0 kg/m2, no previous fracture, and no clinical risk factors.
-
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold). The upper assessment threshold was accepted as 1.2 times the intervention threshold. In this case, very few individuals are reclassified when probabilities are recomputed with the addition of BMD to FRAX, so that the risk of changing the category from high risk to low risk or vice versa when adding BMD to the estimation is minimized [19].
The original FRAX tools created within the framework of the epidemiologic project EVA for 8 Eurasian countries were used as the primary sources to calculate 10-year probabilities of major osteoporotic fracture at the assessment and intervention thresholds.
Results
Ten-year fracture probabilities of a major osteoporotic fracture in a woman with a previous fracture, a body mass index of 25.0 kg/m2, and no other clinical risk factors calculated using the country-specific FRAX models are shown in Table 1. As expected, values for the intervention threshold generally increased with age but plateaued or even decreased at the highest of ages. The most marked (earliest) inflection point was seen in Uzbekistan where fracture probabilities decreased from the age of 75 years and the latest was for Moldova at the age of 85 years. At the age of 40 years, the lowest probabilities were seen for Armenia, Georgia, and Belarus; intermediate values for Moldova and Uzbekistan; and the highest probabilities for Kazakhstan, Kyrgyzstan, and Russia. Overall, there was approximately a fourfold range of probabilities (2.6 to 10.7%). The incremental increase with age varied between countries, and at the age of 90 years, there was a less than twofold range of probabilities (15.6 to 26.9%).
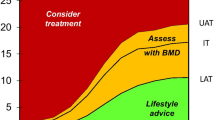
Figure 1 shows the 10-year probabilities of a MOF for the 8 Eurasian countries with additionally the lower and upper assessment thresholds obtained using FRAX.
Lower (LAT) and upper assessment threshold (UAT) as set by FRAX-based 10-year probability (%) of a major osteoporotic fracture for the 8 Eurasian countries. The red area indicates that treatment could be recommended, and the green area indicates probabilities where treatment may not be recommended. The amber area between LAT and UAT shows the limits of fracture probabilities where the assessment of BMD is recommended where available. The line within the amber area represents the intervention threshold (IT)
For men or women with equal or higher fracture probabilities than the upper assessment threshold (red area), treatment is recommended in all cases without the necessity for a BMD test. Conversely, if the probability is below the lower assessment threshold (green area) neither BMD assessment nor intervention is recommended. Those individuals whose probabilities lie between the upper and lower assessment threshold (amber area) can be recommended for testing with BMD where dual X-ray absorptiometry (DXA) is available and the femoral neck BMD result input into FRAX, and the probabilities recalculated.
Discussion
In the present study, we describe age-dependent intervention and assessment thresholds for Armenia, Belarus, Georgia, Moldova, Kazakhstan, the Kyrgyz Republic, the Russian Federation, and Uzbekistan based on the FRAX models developed in the EVA study. The large variation in intervention thresholds is consistent with the heterogeneity in fracture probabilities [20] and indicates that country-specific thresholds are appropriate, rather than a generic Eurasian threshold. These country-specific thresholds can be used as clinical decision tools for prescribing diagnostics or long-term interventions in women and men.
Historically, BMD has been the primary tool used for the assessment of osteoporosis, because of its strong predictive value for fracture risk [21]. The most commonly used intervention threshold is a T score of − 2.5 SD. However, there are several weaknesses in the use of BMD to determine the intervention thresholds [22]. First, any given T score threshold has a different significance at different ages. Additionally, whereas a T score of − 2.5 carries a greater than twofold risk of fracture at the age of 50 years compared to women of the same age, with advancing age, the difference in the risk of fracture is markedly attenuated [23]. Moreover, the same T score has a very different significance in different countries. In the case of Eurasia, a T score of − 2.5 in women at the age of 65 years is equivalent to the 10-year probability of a major osteoporotic fracture that ranges from 4.8 in Belarus to 18% in Uzbekistan. These limitations have led to the development of risk engines to determine fracture risk of which FRAX is the most widely used [4]. FRAX also has the advantage in that it can be used in the absence of BMD where such facilities are scarce or unavailable [24]. The availability of DXA devices in all 8 countries is low ranging from 0.16 per 1 million population in Uzbekistan and the Kyrgyz Republic to 4.8 per 1 million population in Armenia. The availability of DXA scans is further limited with their high costs [25]. Thus, recommendation to use FRAX threshold is appropriate either to be used in the first level of care for referral or directly for the treatment in high-risk cases.
There have been several approaches to the development of intervention thresholds using FRAX. Many guidelines have adopted FRAX within pre-existing guidance. In the USA, for example, the gateway to treatment includes either a prior fracture (hip or spine fracture) or a BMD T score of ≤ − 2.5 SD [26] irrespective of FRAX. FRAX is reserved for individuals in whom the T score is in the osteopenic range and treatment recommended if the probability of a major fracture or hip fracture lies at 20% or more or 3% or more, respectively. Similarly, in Japan, the use of FRAX is reserved for individuals without a prior fracture and a BMD that lies between a T score of − 1.8 and − 2.77 SD and treatment recommended if the probability of a major fracture is 15% or more [27].
Notably, the decision that treatment can be indicated in the presence of a prior fracture is encompassed within many other guidelines but has additionally been used to derive age-dependent thresholds for use in those without prior fracture. This approach, adopted in many countries particularly in Europe and Latin America [4, 28, 29], was first applied by the NOGG in the UK [13, 14, 30]. Briefly, the NOGG guidance ‘translated’ the preceding Royal College of Physicians (RCP) guideline [14] which indicated that women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test for the purpose of making the treatment decision [4]. The translational logic used was that if a woman with a prior fragility fracture be eligible for treatment, then a woman with the same fracture probability but, in the absence of a previous fracture, should also be eligible. For this reason, the intervention threshold in women without a prior fracture at any given age was set at the age-specific fracture probability equivalent to women with a prior fragility fracture of average BMI [13] and, therefore, rose with age (see Fig. 1). In other words, the intervention threshold was set at the age-dependent ‘fracture threshold.’
Irrespective of the approach to intervention thresholds, the present study indicates that these should be country-specific because of the differences in fracture risk and mortality between countries [20]. The increase in fracture probabilities at younger ages is largely attributable to the fracture hazard whereas the plateau in probability with advanced age is a result of the competing effect of mortality. The marked heterogeneity in both characteristics between countries indicates the need for country-specific assessment and intervention thresholds. Although intervention thresholds differ between countries, this does not necessarily mean that the number of patients eligible for treatment will differ. Differences will depend more on the demographic characteristics of the population at risk and the prevalence of the various clinical risk factors.
The limitation of our study was the need to use surrogate FRAX models for two countries in which no data to build FRAX were available (Georgia and Kyrgyz Republic).
In conclusion, for 8 countries of the Eurasia region, Armenia, Belarus, Georgia, Moldova, Kazakhstan, the Kyrgyz Republic, the Russian Federation, and Uzbekistan, the newly established FRAX-based thresholds are a substantial step forward in the detection of both men and women with a high risk of a fracture. Obvious heterogeneity of the intervention thresholds in individuals of different ages and among the countries indicates that country-specific FRAX-based thresholds are appropriate. It will be important that thresholds be incorporated into the national clinical guidelines for each country to facilitate treatment decisions in primary and secondary care. Additionally, FRAX intervention thresholds offer information that could be of use to clinicians and public health agencies to develop treatment strategies.
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8(1–2):136. https://doi.org/10.1007/s11657-013-0136-1
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L, Lems WF, McCloskey EV, Rizzoli R, Stenmark J (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8(1–2):144. https://doi.org/10.1007/s11657-013-0144-1
Kanis JA, on behalf of the World Health Organization Scientific Group (2007) Assessment of osteoporosis at the primary health-care level. Technical Report. World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield. https://www.sheffield.ac.uk/FRAX/reference.aspx. Accessed 12 Feb 2021
Kanis JA, Harvey NC, Cyrus Cooper C, Johansson H, Odén A, McCloskey EV, the Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX. A report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25. https://doi.org/10.1007/s11657-016-0278-z.
Lesnyak O, Sahakyan S, Zakroyeva A, Bilezikian JP, Hutchings N, Galstyan R, Lebedev A, Johansson H, Harvey NC, McCloskey E, Kanis JA (2017) Epidemiology of fractures in Armenia: Development of a country-specific FRAX model and comparison to its surrogate. Arch Osteoporos 12(1):98. https://doi.org/10.1007/s11657-017-0392-6
Ramanau H, Chernyanin I, Rudenka E, Lesnyak O, Zakroyeva A, Bilezikian JP, Johansson H, Harvey NC, McCloskey EV, Kanis JA (2018) Epidemiology of hip fracture in Belarus: development of a country-specific FRAX model and its comparison to neighboring country models. Arch Osteoporos 13:42. https://doi.org/10.1007/s11657-018-0454-4
Issayeva S, Lesnyak O, Zakroyeva A, Issayeva B, Dilmanova D, Johansson H, Harvey NC, McCloskey E, Kanis JA (2020) Epidemiology of osteoporotic fractures in the Republic of Kazakhstan and the development of country specific FRAX model. Arch Osteoporos 15(1):30. https://doi.org/10.1007/s11657-020-0701-3
Zakroyeva A, Lesnyak O, Cazac V, Groppa L, Russu E, Chislari L, Rotaru L, Johansson H, Harvey NC, McCloskey E, Kanis JA (2020) Epidemiology of osteoporotic fracture in Moldova and development of a country specific FRAX model. Arch Osteoporos 15:13. https://doi.org/10.1007/s11657-019-0669-z
Lesnyak O, Ershova O, Belova K, Gladkova E, Sinitsina O, Ganert O, Romanova M, Khodirev V, Johansson H, McCloskey E, Kanis JA (2012) Epidemiology of fracture in the Russian Federation and the development of a FRAX model. Arch Osteoporos 7:67–73. https://doi.org/10.1007/s11657-012-0082-3
Lesnyak O, Ismailov S, Shakirova M, Alikhanova N, Zakroyeva A, Abboskhujaeva L, Johansson H, Harvey NC, McCloskey E, Kanis JA (2020) Epidemiology of hip fracture and the development of a FRAX model for Uzbekistan. Arch Osteoporos 15(1):119. https://doi.org/10.1007/s11657-020-00792-7
Giorgadze E, Tsagareli M, Lomidze M, Sulikashvili T, Jeiranashvili N, Uridia N.(2019) Recommendations by Georgian association of skeletal metabolic diseases on the initiation of treatment with use of age-dependent intervention threshold based on FRAX in patients with osteoporosis. Georgian Med News: Jun (291). 89–93
Lesnyak O., Zakroyeva A., Lobanchenko O., Johansson H., Liu E., Lorentzon M., Harvey N.C.,6, McCloskey E., Kanis J. A (2020) A surrogate FRAX model for the Kyrgyz Republic. Arch Osteoporos 6;15(1):68. https://doi.org/10.1007/s11657-020-00743-2.
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A and the National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX® - Assessment and intervention thresholds for the UK. Osteoporos Int 19:1395–1408. https://doi.org/10.1007/s00198-008-0712-1
Compston J, Cooper A, Cooper C et al (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62:105–108. https://doi.org/10.1016/j.maturitas.2008.11.022
National Institute for Health and Care Excellence (2014) NICE clinical guideline 146. Osteoporosis: assessing the risk of fragility fracture. London, UK. https://www.nice.org.uk/guidance/cg146, Accessed 11 February 2021
Kanis JA, Brazier JE, Stevenson M, Calvert NW, Lloyd JM (2002) Treatment of established osteoporosis: a systematic review and cost-utility analysis. Health Technol Assess 6(29):1–146. https://doi.org/10.3310/hta6290
Kanis JA, Johnell O, Oden A, Borgstrom F, Johansson H, De Laet C, Jönsson B (2005) Intervention thresholds for osteoporosis in men and women: a study based on data from Sweden. Osteoporos Int 16(1):6–14. https://doi.org/10.1007/s00198-004-1623-4
Melnichenko GA, Belaya ZhE, Rozhinskaya LYa, Toroptsova NV, Alekseeva LI, Biryukova EV, Grebennikova TA, Dzeranova LK, Dreval' AV, Zagorodniy NV, Il'yin AV, Kryukova IV, Lesnyak OM, Mamedova EO, Nikitinskaya OA, Pigarova EA, Rodionova SS, Skripnikova IA, Tarbaeva NV, Farba LYa, Tsoriev TT, Chernova TO, Yureneva SV, Yakushevskaya OV, Dedov II. Russian clinical guidelines on the diagnostics, treatment, and prevention of osteoporosis. Probl Endocrinol. 2017;63(6):392–426. https://doi.org/10.14341/probl2017636392-426
Johansson H, Oden A, Johnell O, Jonsson B, De Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimization of BMD measurements to identify high risk groups for treatment – a test analysis. J Bone Miner Res 19:906–913. https://doi.org/10.1359/jbmr.2004.19.6.906
Kanis JA, Odén A, EV MC, Johansson H, Wahl DA, Cooper C, IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256. https://doi.org/10.1007/s00198-012-1964-3
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194. https://doi.org/10.1359/JBMR.050304
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30:1747–1753. https://doi.org/10.1002/jbmr.2531
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27(5):585–590. https://doi.org/10.1016/s8756-3282(00)00381-1
Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD (2012) FRAX® with and without BMD. Calcif Tissue Int 90:1–13. https://doi.org/10.1007/s00223-011-9544-7
Lesnyak O, Bilezikian JP, Zakroyeva A et al (2020) Report on the Audit on Burden of Osteoporosis in Eight Countries of the Eurasian Region: Armenia, Belarus, Georgia, Moldova, Kazakhstan, the Kyrgyz Republic, the Russian Federation, and Uzbekistan. Arch Osteoporos 15:175. https://doi.org/10.1007/s11657-020-00836-y
Cosman F, de Beur SJ, LeBoff MS et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. https://doi.org/10.1007/s00198-014-2794-2(ErratumOsteoporosInt2015;26:2045-7doi:10.1007/s00198-015-3037-x)
Orimo H, Nakamura T, Hosoi T et al (2012) Japanese 2011 Guidelines for prevention and treatment of osteoporosis— executive summary. A report of the committee for developing guidelines for prevention and treatment of osteoporosis: Japan Osteoporosis Society, Japanese Society for Bone and Mineral Research, and Japan Osteoporosis Foundation. Arch Osteoporos 7:3–20. https://doi.org/10.1007/s11657-012-0109-9
Kanis JA, Cooper C, Rizzoli R, Reginster JY; European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). Osteoporos Int. 2019 Jan;30(1):3–44. https://doi.org/10.1007/s00198-018-4704-5.
Clark P., Denova-Gutiérrez E., Zerbini C. Sanchez A., Messina O., Jaller J.J. Campusano C., Orces C. H. Riera G. Johansson H., Kanis J. A. (2017) FRAX-based intervention and assessment thresholds in seven Latin American countries. Osteoporos Int. 23.Dec 2017 https://doi.org/10.1007/s00198-017-4341-4
Compston J, Cooper A, Cooper C et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43. https://doi.org/10.1007/s11657-017-0324-5
Acknowledgements
The EVA project was supported by the International Osteoporosis Foundation (Epidemiology and quality of life working group). Servier, however, is acknowledged in helping with organization of the EVA project, ‘Epidemiology of osteoporotic fractures in Eurasian counties’ study (EVA or ЭBA, in Russian), of which this paper is one of the outcomes. The authors thank the research teams in our countries, whose activity and perseverance led to the successful implementation of the EVA project. We express our special gratitude to Dr S Sahakyan, Dr H Ramanau, Professor B Issayeva, Dr S Issayeva, and Professor O Ershova for their practical contribution to this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or compatible ethical standards.
Conflict of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lesnyak, O., Zakroyeva, A., Babalyan, V. et al. FRAX-based intervention thresholds in eight Eurasian countries: Armenia, Belarus, Georgia, Kazakhstan, the Kyrgyz Republic, Moldova, the Russian Federation, and Uzbekistan. Arch Osteoporos 16, 87 (2021). https://doi.org/10.1007/s11657-021-00962-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-021-00962-1