Abstract
Summary
Age-specific intervention and assessment thresholds were developed for seven Latin American countries. The intervention threshold ranged from 1.2% (Ecuador) to 27.5% (Argentina) at the age of 50 and 90 years, respectively. In the Latin American countries, FRAX offers a substantial advance for the detection of subjects at high fracture risk.
Introduction
Intervention thresholds are proposed using the Fracture Risk Assessment (FRAX) tool. We recommended their use to calculate the ten-year probability of fragility fracture (FF) in both, men and women with or without the inclusion of bone mineral density (BMD). The purpose of this study is to compute FRAX-based intervention and BMD assessment thresholds for seven Latin American countries in men and women ≥ 40 years.
Methods
The intervention threshold (IT) was set at a 10-year probability of a major osteoporotic fracture (MOF) equivalent to a woman with a prior FF and a body mass index (BMI) equal to 25.0 kg/m2 without BMD or other clinical risk factors. The lower assessment threshold was set at a 10-year probability of a MOF in women with BMI equal to 25.0 kg/m2, no previous fracture and no clinical risk factors. The upper assessment threshold was set at 1.2 times the IT.
Results
For the seven LA countries, the age-specific IT varied from 1.5 to 27.5% in Argentina, 3.8 to 25.2% in Brazil, 1.6 up to 20.0% in Chile, 0.6 to 10.2% in Colombia, 0.9 up to 13.6% in Ecuador, 2.6 to 20.0% in Mexico, and 0.7 up to 22.0% in Venezuela at the age of 40 and 90 years, respectively.
Conclusions
In the LA countries, FRAX-based IT offers a substantial advance for the detection of men and women at high fracture risk, particularly in the elderly. The heterogeneity of IT between the LA countries indicates that country-specific FRAX models are appropriate rather than a global LA model.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a disease of concern from the perspective of public health due to its enormous economic and societal impact. Unfortunately, because of its silent nature, it is often not diagnosed until a fragility fracture (FF) has occurred. As a result, measuring the risk of having a FF has become important for the assessment of osteoporosis due to the well-established fracture risk reduction when lifestyle changes and pharmacological therapy are initiated before the fracture occurs [1, 2].
Several instruments are reported in the literature that measure the risk of fracture [3], but of these, only Fracture Risk Assessment (FRAX®) tool was designed to be implemented worldwide. The FRAX tool measures the 10-year probability of having a FF based in the local epidemiology of fracture and the risk of death of each country; this is supplemented with information from seven clinical risk factors, that together with age, and body mass index calculate the 10-year probability of either hip fracture alone or a major osteoporotic fracture (MOF) (forearm, hip, clinical spine, or humeral fracture). Clinical risk factors were identified through a series of meta-analyses, and the model was developed with and without the use of bone mineral density (BMD) in order to be of use in case finding in primary care where BMD is not available. This instrument was designed by the World Health Organization (WHO) Collaborating Centre for Metabolic Bone Diseases at Sheffield, United Kingdom (UK), and has become the most widely used instrument to evaluate the risk of a FF; models for 64 countries across the world are currently available [4].
In Latin America (LA), as in most regions in the world, the population is aging. Increments up to 280% in the population over 70 years of age from 2011 to 2015 have been estimated, and the prevalence of osteoporosis and FF is expected to rise in parallel [5].
Current estimates of annual rate for hip fractures in Argentina are as high as 488 per 100,000 for the population over 50 years; in Mexico, projections indicate a steep increase in the number of hip fractures from 20,725 in 2005 to 110,055 in 2050, an increase of 531% and, similar figures are estimated for Brazil. The Latin American Vertebral Osteoporosis Study (LAVOS) reported a 14% overall fracture rate for vertebral fractures in five countries (Argentina, Brazil, Colombia, Mexico, and Puerto Rico). The vertebral fracture prevalence rate reached as high as 38% in women 80 years and over. Therefore, with these data in mind, it is of the utmost importance to be able to accurately estimate the risk of fracture from both a clinical and a public health perspective in order to take action aimed at preventing FF [5,6,7].
Currently, FRAX is available in seven countries within the LA region (Argentina, Brazil, Colombia, Chile, Ecuador, Mexico, and Venezuela), but the lack of specific thresholds and cutoff points limits their use. The objective of the present study was to develop age-specific intervention thresholds for the LA countries where FRAX models are available to facilitate the use of this tool among clinicians.
Methods
The setting of intervention and assessment thresholds followed the methodology described for the case finding with FRAX by Kanis et al. [8] for the UK. The strategy was adopted by the National Osteoporosis Guideline Group (NOGG) [9], has been approved by the National Institute for Health and Care Excellence (NICE) in the UK [10] and was consistent with the clinical practice and guidelines for the diagnosis and treatment of osteoporosis in postmenopausal women published in 2013 by the Mexican National Health System under the coordination of the National Center of Excellence [11], and the recent Mexican guidelines for diagnosis and treatment at the primary care level [12] in which, a woman with a prior FF should be considered for treatment, as suggested by many international guidelines. Since the Argentinian and Colombian Guidelines adopted the same recommendations, we followed the same recommendations for the remaining countries with FRAX in the region since national guidelines have not been updated following the introduction of FRAX models for these countries (Brazil, Chile, Ecuador, and Venezuela).
The use of the NOGG strategy for primary care in the UK was chosen because it is easily adaptable to countries where the fracture and death risks vary, as is the case in LA [8, 13]. Additionally, the strategy is not solely dependent on BMD testing and the availability of densitometry in the LA region is suboptimal. The UK guidance for the identification of individuals at high fracture risk, developed by the NOGG, recommends that postmenopausal women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test. In women without a fragility fracture but other FRAX risk factors, the intervention threshold set by NOGG is at the age-specific fracture probability equivalent to women with a prior fragility fracture. The same intervention threshold is applied to men, since the effectiveness and cost-effectiveness of intervention in men is broadly similar to that in women for equivalent risk.
The NOGG management strategy considers two additional thresholds:
-
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold)
-
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold)
Fracture probabilities for a major osteoporotic fracture were calculated using the FRAX tool calibrated for the epidemiology and death of the seven LA countries (Argentina, Brazil, Chile, Colombia, Ecuador, Mexico, and Venezuela).
The intervention threshold in each country was the 10-year probability of osteoporotic fracture in a woman with a body mass index (BMI) equal to 25.0 kg/m2 and a previous fracture, without BMD and without other clinical risk factors; the lower assessment threshold was the age-specific fracture probability for a woman with BMI equal to 25.0 kg/m2, no previous fracture and no clinical risk factors. The upper assessment threshold was set at 1.2 times the intervention threshold. In this case, the risk of changing category from high risk to low risk or vice versa when adding BMD to the estimation of fracture probability is highest close to the threshold [14]. When individuals have a fracture probability that is 20% or more than the intervention threshold, almost no individuals are reclassified when probabilities are recomputed with the addition of BMD to FRAX. Thus, the risk of changing category from high risk to low risk or vice versa when adding BMD to the estimation of fracture probability is minimized [14].
Results
The 10-year fracture probabilities for the seven LA countries calculated using the country-specific FRAX models are shown in Table 1. In this case, the risk probabilities for the intervention thresholds are equivalent to a man or woman with previous fracture, no BMD, and no other clinical risk factors and computed from the ages of 40 to 90 years. In general, in all countries evaluated in the present analysis, the 10-year probability of MOF increased with age. Particularly, for Argentina, the probability rose with age, from 1.5% at the age of 40 years to 27.5% at the age of 90 years; whereas, for Mexico, women with previous fracture, but, no clinical risk factors, the probability of a major fracture increased from 2.6% at the age of 40 to 20.0% at the age of 85. Additionally, in Supplementary Figure 1, the fracture probability in men and women (≥ 50 years) with prior fracture is shown. The highest probabilities, from the age of 60–85, are in Argentina, while the lowest probabilities were observed in Ecuador.
Table 2 shows the 10-year probabilities for a MOF for the seven LA countries at the lower and upper assessment thresholds derived using FRAX. The highest risk probabilities for a major fracture were found in Argentina, while the lowest were found in Ecuador. Brazil, Chile, and Mexico had similar risk probabilities up to the age of 80 years. For example, a woman age 72 years in Argentina had a lower and upper assessment threshold of 8.5 and 18.8%, respectively; while, for Ecuador, the lower and upper assessment thresholds were 2.1 and 4.8%.
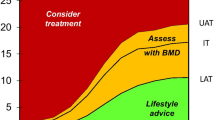
Figures 1 and 2 show intervention and assessment thresholds for the seven LA countries. For men or women with equal or higher fracture probabilities than the intervention threshold, treatment is recommended and conversely if the probability is lower than the intervention threshold; no intervention is recommended. The assessment thresholds are used if BMD testing with dual X-ray absorptiometry (DXA) is available. Where the fracture probability based on age, sex, and BMI plus clinical risk factors falls within the upper and lower threshold dual, the BMD result of the test is input to FRAX to recalculate the probabilities and make the final recommendations with the new estimates.
Lower and upper assessment threshold as set by FRAX-based 10-year probability (%) of a major osteoporotic fracture for the seven Latin American countries. The red area is where the treatment could be recommended, the orange area shows the limits of fracture probabilities for the assessment of BMD, and the green area is where treatment would not be recommended. The dotted line represents the intervention threshold
Discussion
In the present study, we have established the intervention and assessment thresholds for the seven LA countries for which FRAX models have been developed. As in other countries [15,16,17], and given that the effectiveness and cost-effectiveness of intervention in men are largely comparable to those in women for equivalent risk, we used the same intervention thresholds for men. For the seven LA countries, the intervention threshold was, as expected, age-specific and ranged from 1.2% (Ecuador) to 4.9% (Brazil) at the age of 50 years and from 10.2% (Colombia) to 27.5% (Argentina) at the age of 90 years. The large variation in intervention thresholds is consistent with the heterogeneity in fracture probabilities between countries [13] and indicates that country-specific thresholds are appropriate, rather than a generic LA threshold.
The utilization of thresholds, for all the seven LA countries, shown in Fig. 2 is summarized in Box 1 where facilities are available for the measurement of BMD at the femoral neck.
Box 1. Assessment of fracture risk with FRAX with limited access to BMD [18]
• Fracture risk should be assessed in postmenopausal women with one or more clinical risk factor where assessment would influence management.
• Women with a prior FF should be considered for treatment without the need for further risk assessment although BMD measurement may sometimes be appropriate, particularly in younger postmenopausal women.
• In women without a prior FF, the 10-year probabilities of a MOF (clinical spine, hip, forearm, or humerus) and hip fracture should be determined using FRAX without BMD.
• In the absence of other clinical considerations, men and women with probabilities below the lower assessment threshold can be reassured, and those with probabilities above the upper assessment threshold can be considered for treatment.
• Those with probabilities above the lower assessment threshold but below the upper assessment threshold can be considered for testing with BMD using DXA, and their fracture probability reassessed. Thereafter, women with probabilities above the intervention threshold should be considered for treatment.
The application of the guidance above depends on the availability of densitometry. Where facilities for BMD testing are wanting, FRAX can be used without BMD as summarized in Box 2.
Box 2. Assessment of fracture risk with FRAX without BMD [18]
• Fracture risk should be assessed in postmenopausal women with one or more clinical risk factor where assessment would influence management.
• Women with a prior FF should be considered for treatment without the need for further risk assessment.
• In men and in women without a prior FF, the 10-year probabilities of a MOF (clinical spine, hip, forearm, or humerus) and hip fracture should be determined using FRAX without BMD. In the absence of other clinical considerations, men and women with probabilities below the intervention threshold can be reassured.
• Treatment can be considered in those in whom fracture probabilities lie above the intervention threshold.
For the purposes of risk assessment, a characteristic of major importance is the ability of a technique to predict fractures, traditionally expressed as the increase in relative risk per standard deviation (SD) unit decrease in risk score—termed the gradient of risk. Whereas the gradient of risk of FRAX with BMD is higher than the use of BMD alone, the gradient of risk with FRAX without BMD is similar to the use of BMD alone to predict fractures [19].
Several agencies involved with guideline development have raised concerns about making treatment decisions in the absence of BMD [20, 21]. It is stated that there is no evidence from randomized control trials demonstrating a benefit of fracture reduction when FRAX scores are used for treatment decision making. The argument implies that the beneficial effects of treatment on fracture risk are restricted to patients with osteoporosis as judged by densitometry. Although not entirely true, the argument presupposes that high FRAX scores with or without BMD do not identify individuals with low BMD—a supposition that has for several years been shown to be ill-founded [15, 16, 22]. Moreover, analyses of randomized clinical trials have indicated that patients with high FRAX scores are responsive to a variety of interventions, including abaloparatide, alendronate, bazedoxifene, clodronate, denosumab, raloxifene, strontium ranelate, daily and weekly teriparatide [23] as well as a basket of interventions used by general practitioners in the UK [24]. Most of these were post hoc analyses but, in the case of denosumab, was a pre-planned analysis [25]. In addition, the “screening for prevention of fractures in older women” (SCOOP) study was a prospective randomized study that demonstrated efficacy for hip fracture in women selected on the basis of hip fracture probability assessed using FRAX [24]. These considerations indicate the validity of the use of FRAX with or without the incorporation of BMD.
Historically, BMD was the primary tool used for the assessment of osteoporosis, because of its strong predictive value for fracture risk [26]. The most commonly used intervention threshold is a T-score of − 2.5 SD. However, there are several weaknesses in the use of BMD to determine the intervention thresholds. First, any given T-score threshold has a different significance at different ages [27]. Additionally, whereas a T-score of −2.5 carries a greater than two-fold risk of fracture at the age of 50 years compared to women of the same age, with advancing age, the difference in the risk of fracture is markedly attenuated [27]. The explanation is that BMD in the general population decreases with age, so that at the age of 50 years, the relative risk of hip fracture in a woman at the threshold value of osteoporosis is high, whereas in the elderly, the relative risk is lower than 1.0 [27,28,29]. Moreover, the same T-score has a very different significance in different countries. In the case of LA, a T-score of − 2.5 in women at the age of 65 years, the 10-year probability of a major osteoporotic fracture ranges from 1.7% in Ecuador to 9.2% in Argentina. Importantly, FRAX allows the assessment of individuals in the absence of BMD testing; whereas, an individual assessed with an intervention threshold based on BMD alone could not qualify for treatment, for example, those patients with a prior fracture could not be eligible for treatment in the absence of a T-score − 2.5 SD [18]. Another issue concerns the reduced accessibility to densitometry in many LA countries. Thus, many clinical guidelines now recommend the use of FRAX to help primary care physicians identify postmenopausal women who may be candidates for treatment based on the level of fracture risk. These considerations suggest that BMD should not be used as the sole gateway to risk assessment; rather, BMD should be used as an adjunct to assessment the fracture risk.
There are some weaknesses in the intervention and assessment thresholds proposed in the present study. First, as noted by others [28, 30], the impact of intervention and assessment thresholds on BMD requests have not been investigated yet in the LA countries. Also, the cost-effectiveness of case finding and intervention in the LA countries as well as the budget impact of any modifications in refund policy is unknown. Notwithstanding these constraints, intervention based on fracture probability is more effective in identifying individuals at high risk and avoiding treatment of individuals at low risk, than those based on the utilization of BMD alone [31]. In other words, BMD measurement is not a precondition for assessment or treatment. Additionally, the use of FRAX model to calculate the intervention and assessment thresholds would be especially beneficial in some areas of the seven LA countries with restricted access to DXA. Lastly, it should be noted that the algorithms presented in this study are applicable only to the seven LA countries (Argentina, Brazil, Chile, Colombia, Ecuador, Mexico, and Venezuela); nevertheless, any other country where FRAX tool is available (in order that each FRAX is country specific) could compute the intervention and assessment thresholds.
In conclusion, as suggested in other populations, FRAX-based intervention threshold in these LA countries signifies a substantial advance in the detection of both men and women at high risk of fracture, certainly even more so than fixed T-score thresholds alone, particularly in the elderly. Additionally, FRAX intervention thresholds offer information that could be of use to clinicians and public health agencies to make reasonable treatment decisions.
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1–2):136. https://doi.org/10.1007/s11657-013-0136-1.
Kanis JA, Borgström F, Compston J, Dreinhöfer K, Nolte E, Jonsson L, Lems WF, McCloskey EV, Rizzoli R, Stenmark J (2013) SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos 8(1-2):144. https://doi.org/10.1007/s11657-013-0144-1
Rubin KH, Friis-Holmberg T, Hermann AP, Abrahamsen B, Brixen K (2013) Risk assessment tools to identify women with increased risk of osteoporotic fracture: complexity or simplicity? A systematic review. J Bone Miner Res 28(8):1701–1717. https://doi.org/10.1002/jbmr.1956
Kanis JA, Harvey NC, Cooper C, Johansson H, Odén A, McCloskey EV, Advisory Board of the National Osteoporosis Guideline Group (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos 11(1):25. https://doi.org/10.1007/s11657-016-0278-z
Zanchetta J, Campusano C, Muzzi B (2012) The Latin America regional audit. Epidemiology, costs and burden of osteoporosis in 2012. Report, International Osteoporosis Foundation
Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA (2011) Increasing age- and sex-specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int 22(8):2359–2364. https://doi.org/10.1007/s00198-010-1475-z
Clark P, Cons-Molina F, Deleze M, Ragi S, Haddock L, Zanchetta JR, Jaller JJ, Palermo L, Talavera JO, Messina DO, Morales-Torres J, Salmeron J, Navarrete A, Suarez E, Pérez CM, Cummings SR (2009) The prevalence of radiographic vertebral fractures in Latin American countries: the Latin American Vertebral Osteoporosis Study (LAVOS). Osteoporos Int 20(2):275–282. https://doi.org/10.1007/s00198-008-0657-4
Kanis JA, Closkey EV, Johansson H, Strom O, Borgstrom F, Oden A, National Osteoporosis Guideline Group (2008) Case finding for the management of osteoporosis with FRAX-assessment and intervention thresholds for the UK. Osteoporos Int 19(10):1395–1408. https://doi.org/10.1007/s00198-008-0712-1
Compston J, Cooper A, Cooper C, Francis R, Kanis JA, Marsh D, McCloskey EV, Reid DM, Selby P, Wilkins M, on behalf of the National Osteoporosis Guideline Group (NOGG) (2009) Guidelines for the diagnosis and management of osteoporosis in postmenopausal women and men from the age of 50 years in the UK. Maturitas 62(2):105–108. https://doi.org/10.1016/j.maturitas.2008.11.022
National Institute for Health and Care Excellence NICE Clinical Guideline 146 (2014) Osteoporosis: assessing the risk of fragility fracture. NICE UK. https://www.nice.org.uk/guidance/cg146, Accessed 18 May 2015
Salud. Diagnóstico y tratamiento de osteoporosis en mujeres posmenopaúsicas (2013) DOI:http://www.cenetec.salud.gob.mx/descargas/gpc/CatalogoMaestro/IMSS_673_13_Osteoporosisenpostmenopausia/673GER.pdf.
Secretaria de Salud (2017) Proyecto de Norma Oficial Mexicana PROY-NOM-049-SSA2–2017, para la prevención, detección, diagnóstico, tratamiento, control y vigilancia epidemiológica de la osteoporosis. Diario Oficial de la Federación. http://www.dof.gob.mx/nota_detalle.php?codigo=5496348&fecha=06/09/2017, Accessed 11 Sept 2017
Kanis JA, Odén A, EV MC, Johansson H, Wahl DA, Cooper C, IOF Working Group on Epidemiology and Quality of Life (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23(9):2239–2256. https://doi.org/10.1007/s00198-012-1964-3
Johansson H, Oden A, Johnell O, Jonsson B, de Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimization of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res 19(6):906–913. https://doi.org/10.1359/jbmr.2004.19.6.906
Johansson H, Kanis JA, Oden A, Compston J, McCloskey E (2012) A comparison of case-finding strategies in the UK for the management of hip fractures. Osteoporos Int 23(3):907–915. https://doi.org/10.1007/s00198-011-1864-y
Leslie WD, Majumdar SR, Lix LM, Johansson H, Oden A, McCloskey E, Kanis JA, Manitoba Bone Density Program (2012) Hip fracture probability with FRAX usually indicates densitometric osteoporosi: implications for clinical practice. Osteoporos Int 23(1):391–397. https://doi.org/10.1007/s00198-011-1592-3
Kanis JA, Adams J, Borgström F, Cooper C, Jönsson B, Preedy D, Selby P, Compston J (2008) The cost-effectiveness of alendronate in the management of osteoporosis. Bone 42(1):4–15. https://doi.org/10.1016/j.bone.2007.10.019
Kanis JA, EV MC, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. https://doi.org/10.1007/s00198-012-2074-y
Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Glüer C, Goltzman D, Hans D, Krieg MA, La Croix A, McCloskey E, Mellstrom D, Melton LJ 3rd, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18:1033–1046, 8, DOI: https://doi.org/10.1007/s00198-007-0343-y.
Qaseem A, Forciea MA, RM ML, Denberg TD, Clinical Guidelines Committee of the American College of Physicians (2017) Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med 166(11):818–839. https://doi.org/10.7326/M15-1361
Scottish Intercollegiate Guidelines Network (SIGN) (2015) Management of osteoporosis and the prevention of fragility fractures. Edinburgh: SIGN; 2015. SIGN publication. http://www.sign.ac.uk, 2015. Accessed 11 Sept 2017
Kanis JA, McCloskey E, Johansson H, Oden A, Leslie WD (2012) FRAXs with and without BMD. Calcif Tissue Int 90(1):1–13. https://doi.org/10.1007/s00223-011-9544-7
McCloskey EV, Johansson H, Oden A, Harvey NC, Jiang H, Modin S, Fitzpatrick L, Kanis JA (2017) The effect of abaloparatide-SC on fracture risk is independent of baseline FRAX fracture probability: a post hoc analysis of the ACTIVE Study. J Bone Miner Res 32(8):1625–1631. https://doi.org/10.1002/jbmr.3163
Shepstone L, Lenaghan E, Cooper C, Clarke S, Fordham R, Gittoes NJ, Harvey IM, Harvey NC, Heawood A, Holland R, Howe A, Kanis J, Marshall T, O'Neill TW, Peters TJ, Redmond NM, Torgerson DJ, McCloskey EV (2017) A randomized controlled trial of screening in the community to reduce fractures in older women—the SCOOP Study. Lancet, in press
McCloskey EV, Johansson H, Oden A, Austin M, Siris E, Wang A, Lewiecki EM, Lorenc R, Libanati C, Kanis JA (2012) Denosumab reduces the risk of all osteoporotic fractures in postmenopausal women, particularly in those with moderate to high fracture risk as assessed with FRAX®. J Bone Miner Res 27(7):1480–1486. https://doi.org/10.1002/jbmr.1606
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O'Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194, 7, DOI: https://doi.org/10.1359/JBMR.050304.
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27(5):585–590. https://doi.org/10.1016/S8756-3282(00)00381-1
Grigorie D, Sucaliuc A, Johansson H, Kanis JA, McCloskey E (2013) FRAX-based intervention and assessment thresholds for osteoporosis in Romania. Arch Osteoporos 8(1–2):164. https://doi.org/10.1007/s11657-013-0164-x
Kanis JA, Compston J, Cooper C, Harvey NC, Johansson H, Odén A, McCloskey EV (2016) SIGN guidelines for Scotland: BMD versus FRAX versus QFracture. Calcif Tissue Int 98(5):417–425. https://doi.org/10.1007/s00223-015-0092-4
Johansson H, Azizieh F, Al Ali N, Alessa T, Harvey NC, McCloskey E, Kanis JA (2017) FRAX vs. T-score-based intervention thresholds for osteoporosis. Osteoporos Int 28(11):3099–3105. https://doi.org/10.1007/s00198-017-4160-7
Kanis JA, McCloskey EV, Harvey NC, Johansson H, Leslie WD (2015) Intervention thresholds and the diagnosis of osteoporosis. J Bone Miner Res 30(10):1747–1753. https://doi.org/10.1002/jbmr.2531
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Electronic supplementary material
Supplementary figure 1
(DOCX 16 kb)
Rights and permissions
About this article
Cite this article
Clark, P., Denova-Gutiérrez, E., Zerbini, C. et al. FRAX-based intervention and assessment thresholds in seven Latin American countries. Osteoporos Int 29, 707–715 (2018). https://doi.org/10.1007/s00198-017-4341-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-017-4341-4