Abstract
Introduction
Imminent fracture risk, or fractures within 2 years of an initial fracture, is a pressing issue worldwide. Hong Kong is a city with one of the longest life expectancies. The concern of fragility fractures and the imminent risk of a subsequent fracture is becoming a top priority. The objective of this study was to present the epidemiology of incident fragility fractures of all public acute hospitals and the imminent risk of a subsequent fracture in Hong Kong.
Methodology
This was a retrospective population-based analysis. Patient records from all acute hospitals in Hong Kong from 1 January 2004 to 31 December 2018 were retrieved for patients ≥ 50 years of age with hip, distal radius, or proximal humerus fractures. Secondary fractures and falls were identified in the subsequent 5 years. Post hoc analysis in recent 2013–2018 period was performed. Overall survival (re-fracture incidence) on age subgroups using Kaplan survival analysis and variables was compared using the log-rank test. Cox proportional hazard regressions, obtaining the hazard ratios (HR) and their respective 95% confidence intervals (CI), were used.
Results
There is an overall increasing trend of fragility fractures (hip, distal radius, proximal humerus) from 5596 in 2004 to 8465 in 2018. The average cumulative imminent risk of fractures from recent 5 years is 3.87% at 1 year and 6.50% at 2 years. 49.5% of the patients with a secondary fracture occurred within 2 years since the initial major fragility fracture. Post hoc analysis in recent 2013–2018 period (N = 7039) showed male patients were 1.21 times more likely to have further fractures with time (HR = 1.21 (1.02, 1.45), p = 0.03) compared with female patients. Patients over age 95 were 2.01 times higher than patients of age under 75 to have further fracture over time.
Conclusions
Following an initial fracture, prompt treatment strategies should be adopted to avoid imminent risk of fractures. This window of opportunity in the first 2 years is a golden period to treat osteoporosis and prevent falls. Our post hoc analysis has shown that male patients and patients older than 95 are at even higher risk. Clinicians and allied healthcare professionals should be alert on these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Imminent fracture risk, or fractures within 2 years of an initial fracture, is a pressing issue worldwide [1, 2]. In fact, a recent study from the Swedish database has shown that the cumulative subsequent fracture incidence at 12 months was 7.1% and at 24 months was 12.0% [3]. Johansson et al. also showed that at 1 year after a major osteoporotic fracture, the risk of a second fracture was 2.7-fold higher than population risk compared with 1.4-fold at 10 years [2]. These findings highlight the importance of early intervention after an initial fracture with dedicated and coordinated services. Currently, an estimated 200 million people are affected by osteoporosis and the lifetime fracture risk reaches up to 40% [4, 5]. With the aging population, the incidence of fragility fractures is expected to increase yearly, posing a significant healthcare burden to our society. In fact, 9 million osteoporotic fractures occurred worldwide in year 2000 [6], but a large healthcare gap still exists leading to imminent risk of further fractures. In a previous study of 905 women and 337 men with an initial fracture, it was shown that 41% of women and 52% of men had an imminent fracture within 2 years [7]. It has also been reported that secondary fractures cost 1.6–6.2 times higher with costs ranging from USD 3844 to USD 27,730 compared with those without a prior fracture [8]. This implies the healthcare costs of a secondary fracture are mainly concentrated during this window period. It is therefore important to increase awareness and enhance international network alliances to further improve current public and health policies.
Hong Kong is a city with one of the longest life expectancies worldwide. In 2017, the life expectancy for males is 81.9 years of age and for females 87.6 years of age, increasing steadily [9]. The concern of fragility fractures and the imminent risk of a subsequent fracture is becoming a top priority. The current cost of a single hip fracture in Hong Kong is USD 8831.9, with projected direct cost of USD 84.7 million in total in 2018 [10]. It is well established that the single most predictive factor of a secondary fracture is a previous one [1]. Apart from osteoporosis, evidence has also shown that patients with fragility fractures often have low muscle mass and function as well, which has been postulated as a cause of further falls [11]. Major pitfalls in the healthcare system include low rates of bone mineral density (BMD) testing, low drug initiation, poor drug compliance, and low follow-up rates leading to falls and fractures. Therefore, establishment of Fracture Liaison Services (FLS) to improve patient outcomes has been adopted in many countries [12], but is still not yet available in many hospitals. Thus, the rate of imminent fractures remains high currently. In a recent study in the USA, it was shown that among 337,561 women, cumulative risk of subsequent fractures was 10% and 18% at 1 and 2 years, respectively [13].
The risk of a secondary fracture decreases over time [2], and therefore capturing imminent fractures in the first 2 years provides a window of opportunity in preventing a large number of secondary fractures. It is well known that osteoporotic fractures lead to high morbidity and mortality [14] and therefore a call-to-action worldwide is needed to stop further risk. Currently, there is a lack of published data in Asian cities on imminent risk of fractures. Presenting the imminent fracture risk in regions with long life expectancies and in Asia would prove to be important in strengthening the knowledge of this global threat. It is also crucial for representative parties internationally to share and provide treatment goals and strategies for our patients.
The objective of this study was to present the epidemiology of incident fractures and the imminent risk of a subsequent fracture in Hong Kong. This is the first study representing imminent fracture data from a Chinese population.
Methods
Study design
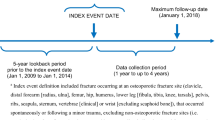
This was a retrospective population-based analysis. Patient records from all acute hospitals in Hong Kong from 1 January 2004 to 31 December 2018 were retrieved from the Hospital Authority Clinical Data Analysis and Reporting System (CDARS, Hospital Authority, Hong Kong) [15, 16]. Patients ≥ 50 years of age with hip, distal radius, or proximal humerus fractures (major osteoporotic fractures) were identified using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for hip fracture (820.02, 820.3, 820.8, 820.9, 820.12, 820.20, 820.22, 820.32), proximal humerus fracture (812.02, 812.03, 812.09, 812.12, 812.13, 812.19), and distal radius fracture (13.41, 813.42, 813.44, 813.52, 813.54). Patients with motor vehicle accident or pathological fractures were excluded. In Hong Kong, hip, distal radius, and proximal humerus fractures are well captured in the database. The public hospital system in Hong Kong uses the Clinical Management System (CMS) and the diagnosis is entered. This allows retrieval of all records through the CDARS regardless of in-patient or out-patient [15, 16], and more than 90% of the Hong Kong population is captured [17]. The positive predictive value (PPV) in using ICD-9 does for CDARS database search has also been shown to be 100% for fracture hip, wrist, and humerus [17]. However, although 98% of hip fractures are admitted to public hospitals instead of private hospitals and captured [10], there is currently no available data on the sensitivity and completeness in capturing all distal radius and proximal humerus fractures in Hong Kong.
Vertebral fractures were not retrieved initially because it is well documented that approximately two-thirds are not diagnosed and therefore, diagnostic coding would strongly underestimate the prevalence and thereby be inaccurate [18, 19]. Incident fracture, mean age, gender, and length of stay in acute hospital were recorded for 15 years (2004 to 2018). Secondary fractures and falls and deaths of patients were further identified from each year from 2004 to 2013 (follow-up of 5 years each year) projecting up to 5 years using the Hospital Authority CDARS. A 5-year follow-up is used as it is a common time-point in fracture studies [20]. Imminent fractures were defined as the first 2 years. To eliminate risk of double counting, secondary fracture was excluded if it was at the same site as the initial fracture [2]. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used in preparation of this manuscript.
Data analysis
Descriptive statistics were presented in numbers and percentages. Secondary fractures and falls and deaths of patients were identified from each year from 2004 to 2013 (follow-up of 5 years each year) to better represent the average imminent fracture risk over 10 years. The more recent data over 5 from 2008 to 2013 was also calculated. Post hoc analysis of imminent fracture risk in Hong Kong was performed in year 2013 as it is the most recent 5 years (since fracture in 2013, and follow-up to 2018) and is therefore most representative of recent data. We determined and compared the overall survival (re-fracture incidence) on age subgroups using the Kaplan–Meier product-limit method and variables were compared using the log-rank test. Cox proportional hazard regressions, obtaining the hazard ratios (HR) and their respective 95% confidence intervals (CI), were used to show the strength of estimated relative risk, which were applied to model the relationship between potential covariates (sex and age groups) and fracture incidence. Comparisons of percentage cumulative fractured rates happened between the 1st and 2nd year and 3rd to 5th years were performed after stratifying for age groups. p value of < 0.05 was regarded as statistical significance.
Results
Incidence of fragility fractures, characteristics, and length of hospital stay from 2004 to 2018
There is an overall increasing trend of fragility fractures (hip, distal radius, proximal humerus) from 5596 in 2004 to 8465 in 2018 (Fig. 1and Table 2). Hip fractures have the highest incidence for fragility fractures in Hong Kong, with 4002 in 2004 to 5241 in 2018. The mean age is 81.4 ± 9.0 years old, with a female to male ratio of 2:1. The average length of hospital stay is 15.5 days. The mean age of distal radius fractures is 67.6 ± 11.9 years old, which is earliest to occur. The female to male ratio is 3:1, and average length of hospital stay is 3.7 days. Proximal humerus fractures occur at a mean age of 73.5 ± 11.7 years old, with a female to male ratio of 3.7:1. The average length of hospital stay is 5.7 days (refer to Table 1).
Mortality of fragility fracture patients from 2004 to 2013
The mortality of fragility fracture patients from 2004 to 2013 at 1 year on average is 401 and at 2 years 357. The absolute number has a steady increasing trend over the years due to the increase in fragility fracture incidence. An average mortality of 6.3% of all fragility fracture patients occurs each year after an initial fracture (refer to Table 6). Hip fractures on average had an 8.49%, 15.8%, and 34.8% cumulative mortality rate at 1, 2, and 5 years, respectively. Distal radius on average had a 1.80%, 3.96%, and 10.6% cumulative mortality rate at 1, 2, and 5 years, respectively. Proximal humerus on average had a 4.56%, 9.90%, and 17.4% cumulative mortality rate at 1, 2, and 5 years, respectively (refer to Table 9 and 10).
Imminent risk of fractures and falls
The average cumulative imminent risk of fractures from 2004 to 2013 at 1 year is 3.41% and at 2 years is 5.77%. This amounts to an average of 325 imminent fractures in 2 years. In the more recent 2009–2013, the average cumulative imminent risk of fractures at 1 year is 3.87% and at 2 years is 6.50%. Projecting to year 2018 with an incidence of 8465 fragility fractures, imminent fractures would reach 550 in 2 years (Table 2). Cumulative secondary fractures at the 3rd, 4th, and 5th years from 2004 to 2013 are 7.67%, 9.57%, and 11.1%, respectively. This amounts to an average of 258 secondary fractures from the 3rd to 5th years. The results show that an average of 55% of secondary fractures occurs in the first 2 years in a 5-year period (refer to Table 11). Corresponding to the imminent risk of fractures, mean fall rates from 2004 to 2013 at 1 year are 3.61% and at 2 years is 6.60%. At the 3rd, 4th, and 5th years, cumulative fall rates are 9.27%, 11.79%, and 13.97%, respectively (refer to Table 12).
Post hoc analysis of imminent risk of fractures during period of 2013–2018
A total of 4891 of the 7039 patients were female (69.5%). Four hundred twenty-six (57.0%) of the patients with a secondary fracture occurred within 2 years since the initial major fragility fracture. The overall Kaplan–Meier survival curve is shown in Fig. 2. Subgroup analyses on age and sex groups are graphically represented in Figs. 3 and 4, respectively (Table 6, 7, and 8). Both show statistical significance. Upon stratification, the cumulative secondary fractures in the first 2 years were significantly higher compared with the 3rd to 5th year after the initial fracture in all age groups, 85–94 and ≥ 95 (p < 0.01) (Tables 3 and 4). The largest difference was observed in the age group ≥ 95 (79.2% in the first 2 years vs. 20.8% in the 3rd to 5th years). Mortality is shown in Table 5. Using sex (ref: female) and age groups (ref: age < 75), we show that male patients were 1.21 times more likely to have further fractures with time (HR = 1.21 (1.02, 1.45), p = 0.03) compared with female patients. Patients over age 95 were 2.01 times higher than patients of age under 75 to have further fracture over time (Table 6). Age group- and sex-specific analyses showed statistical significances in both male age over 95 (HR = 8.04 (1.06, 61.03)) and female patients age 85–94 (HR = 1.29 (1.01, 1.64), p = 0.04)), and over 95 (HR = 2.25 (1.38, 3.66), p < 0.01)), when both compared with “age < 75” group (Table 7). When controlling for sex, patients over age 95 were 2.15 times more likely to have second fracture compared with patients younger than 75 (HR = 2.15 (1.36, 3.42), p < 0.01) (Table 8).
Discussion
The risk of an imminent fracture after an initial fracture is a major threat in our aging population. Our results show nearly half of all patients with secondary fractures occurring in the first 2 years. Resources should be allocated to prevent the high risk to save healthcare costs. Our results concur with other studies on imminent fractures in the USA, Sweden, and Iceland as secondary fractures significantly decrease after the first 2 years [2, 3, 13]. Compared with the study in the USA and Sweden, the risk of imminent fractures is lower in Hong Kong and Iceland. The differences seen would likely correlate with the demographics and general health status of patients in different countries. Furthermore, in countries including the USA, insurance coverage may allow follow-ups with increased detection of secondary fractures including vertebral compression fractures. However, all studies are consistent in highlighting the importance of intervening rapidly after a fragility fracture. Although Hong Kong is a small city, it has one of the longest life expectancies worldwide and the risk of imminent fractures is still substantial. At an imminent fracture rate of 6.50% at 2 years based on the average in years 2009–2013, costs of secondary fractures are a major burden. A systematic review and meta-regression analysis have shown that the estimated cost for a single hip fracture is USD 10,075 for index hospitalization, and health and social care costs at 1 year are USD 43,669 [21]. Furthermore, secondary fractures have higher costs ranging from USD 3844 to USD 27,730 compared with those without a prior fracture [8]. The excess costs are due to hospital admissions, long-term care, and outpatient visits [8] that may result from further complications. With the majority of secondary fractures in the first 2 years, decreasing imminent fractures should be a national priority.
Despite the strong evidence and need to prevent imminent fractures, there remains a large healthcare gap. Our recent study showed that only 23% of hip patients in Hong Kong are prescribed with anti-osteoporotic medications, excluding calcium and vitamin D supplements [22]. In the USA, Canada, and UK, only 9–50% of patients proceed for bone health assessment after a fragility fracture [23]. Systematic reviews have shown that the prevention of secondary fractures with Fracture Liaison Services to be cost-effective [24]. In fact, a recent meta-analysis of 74 studies showed that Fracture Liaison Service programs improved outcomes of fracture patients with significant increase in BMD assessment (48.0% vs 23.5%), treatment initiation (38.0% vs 17.2%), compliance (57.0% vs 34.1%), secondary fracture (6.4% vs 13.4%), and mortality (10.4% vs 15.8%) (Tables 9, 10, 11, and 12) [12].
Given the high risk in the first 2 years for imminent fractures, a call-to-action with international alliances should be made. Expert groups and stakeholders should have consensus and guidelines in the allocation of resources and treatment in managing imminent risk of fractures in an effective manner. Although FLS appear to be a promising solution, only 10–25% of public hospitals in Hong Kong have the existing service [25]. Likewise, only 9–20% of fragility fracture patients actually get treated for osteoporosis [26, 27]. Despite the evidence, difficulties in setting up FLS, lack of resources, and expertise in certain hospitals have still not been addressed. Recently, several organizations including the Fragility Fracture Network (FFN), the European Geriatric Medicine Society (EuGMS), the European Federation of National Associations of Orthopaedics and Traumatology (EFFORT), the International Collaboration of Orthopaedic Nursing (ICON), the International Geriatric Fracture Society (IGFS), and the International Osteoporosis Foundation (IOF) have stated the importance of acute multidisciplinary care for fragility fracture patients, rapid secondary prevention, and ongoing post-acute care [28]. However, given the current low treatment rates, it is still important to continue spreading the awareness of this imminent threat to our society.
The strengths of this study are that it includes public hospital data from the whole of Hong Kong, reflecting the situation across all territories in the city, thus reducing selection bias. To the knowledge of the authors, this is also the first study with data of imminent fractures from Asia. Furthermore, the locations of imminent fractures are also shown to further elaborate the epidemiological data. We have identified male patients to have further fractures with time (HR = 1.21 (1.02, 1.45), p = 0.03). Patients over age 95 were also 2.01 times higher than patients of age under 75 to have further fracture over time.
Falls are the major cause of fractures [29]. Our data suggests the rates of falls are similar to the fractures especially in the first 2 years of imminent risk of fractures. Effective fall prevention and programs are therefore an essential step. Multidisciplinary approach with physiotherapists and occupational therapists is important and exercise programs have been shown to be successful [30]. More importantly, recent studies have shown a high prevalence of sarcopenia in patients with fragility fractures [11, 31]. Sarcopenia is an age-related decline in muscle mass and function [32] and studies have postulated the occurrence of the condition due to the loss of muscle bulk during in-patient periods [11]. Our previous systematic review further showed that the prevalence of sarcopenia in elderly patients with fragility fracture is high, especially in men [11]. This corresponds to the current observation of male patients more likely to have a secondary fracture with time. Further studies investigating an imminent risk of sarcopenia after a fracture should be conducted. As sarcopenia is associated with an increased risk of falls, it should therefore be treated promptly. Exercise and nutrition should be optimized after a fragility fracture with Fracture Liaison Services.
The limitations of the study include that the study was retrospective data. Vertebral fractures for initial fractures were not collected due to the fact that it is well documented that approximately two-thirds are not diagnosed and therefore diagnostic coding would strongly underestimate the prevalence and thereby be inaccurate [18, 19]. Furthermore, fracture patients may have gone to the private setting, which would not be captured. In fact, although 98% of hip fractures are admitted to public hospitals instead of private hospitals [10], there is currently no available data on the sensitivity and completeness in capturing distal radius and proximal humerus fractures in Hong Kong. With the lower incidence of distal radius and proximal humerus fractures in this study compared with other epidemiological studies [33, 34], it is suggestive that the current data source is unable to detect the majority of these 2 fractures, thereby underestimating the overall incidence of major osteoporotic fractures in Hong Kong. Mortality can also be a factor of underestimating the actual total number of re-fractures. Medical risk factors of patients were not analyzed in this study as the purpose was solely to identify the number of secondary fractures and the significance of imminent fractures. Patient loss to follow-up is also a limitation as the CDARS database does provide this data.
In conclusion, following an initial fracture, prompt treatment strategies should be adopted to avoid imminent risk of fractures. This window of opportunity in the first 2 years is a golden period to treat osteoporosis and prevent falls. This would not only save costs but also decrease morbidity and mortality for the patients. Furthermore, our post hoc analysis has shown that male patients and patients older than 95 are at even higher risk. Clinicians and allied healthcare professionals should be alert on these patients.
References
Roux C, Briot K (2017) Imminent fracture risk. Osteoporos Int 28(6):1765–1769
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780
Banefelt J, Akesson KE, Spangeus A, Ljunggren O, Karlsson L, Strom O et al (2019) Risk of imminent fracture following a previous fracture in a Swedish database study. Osteoporos Int 30(3):601–609
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis: now and the future. Lancet. 377(9773):1276–1287
Sozen T, Ozisik L, Basaran NC (2017) An overview and management of osteoporosis. Eur J Rheumatol 4(1):46–56
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17(12):1726–1733
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 297(4):387–394
Weaver J, Sajjan S, Lewiecki EM, Harris ST, Marvos P (2017) Prevalence and cost of subsequent fractures among U.S. patients with an incident fracture. J Manag Care Spec Pharm 23(4):461–471
Centre for Health Protection DoH, The Government of the Hong Kong Special Administrative Region. Life expectancy at birth (male and female), 1971 - 2017 2019 [Available from: https://www.chp.gov.hk/en/statistics/data/10/27/111.html
Cheung MY, Ho AW, Wong SH (2018) Post-fracture care gap: a retrospective population-based analysis of Hong Kong from 2009 to 2012. Hong Kong Med J 24(6):579–583
Wong RMY, Wong H, Zhang N, Chow SKH, Chau WW, Wang J, Chim YN, Leung KS, Cheung WH (2019) The relationship between sarcopenia and fragility fracture-a systematic review. Osteoporos Int 30(3):541–553
Wu CH, Tu ST, Chang YF, Chan DC, Chien JT, Lin CH, Singh S, Dasari M, Chen JF, Tsai KS (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone. 111:92–100
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, Curtis JR (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30(1):79–92
Wong RMY, Choy MHV, Li MCM, Leung KS, S KHC, Cheung WH et al (2018) A systematic review of current osteoporotic metaphyseal fracture animal models. Bone Joint Res 7(1):6–11
Cheung NT, Fung KW, Wong KC, Cheung A, Cheung J, Ho W, Cheung C, Shung E, Fung V, Fung H (2001) Medical informatics--the state of the art in the Hospital Authority. Int J Med Inform 62(2–3):113–119
Fung V, Cheung NT, Ho E, Cheung C, Chan H, Tsang K, Cheung J, Ho W, Lau M, Hung V, Wong A, Tong A, Wong WN, Sek A (2007) Building a womb-to-tomb health record in Hong Kong--an application of information architecture. Stud Health Technol Inform 129(Pt 1):474–477
Sing CW, Woo YC, Lee ACH, Lam JKY, Chu JKP, Wong ICK, Cheung CL (2017) Validity of major osteoporotic fracture diagnosis codes in the Clinical Data Analysis and Reporting System in Hong Kong. Pharmacoepidemiol Drug Saf 26(8):973–976
Kendler DL, Bauer DC, Davison KS, Dian L, Hanley DA, Harris ST et al (2016) Vertebral fractures: clinical importance and management. Am J Med 129(2):221–e1–10
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20(7):1216–1222
Handoll HH, Keding A, Corbacho B, Brealey SD, Hewitt C, Rangan A (2017) Five-year follow-up results of the PROFHER trial comparing operative and non-operative treatment of adults with a displaced fracture of the proximal humerus. Bone Joint J 99-B(3):383–392
Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, Leal J (2017) Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int 28(10):2791–2800
Leung KS, Yuen WF, Ngai WK, Lam CY, Lau TW, Lee KB et al (2017) How well are we managing fragility hip fractures? A narrative report on the review with the attempt to set up a Fragility Fracture Registry in Hong Kong. Hong Kong Med J 23(3):264–271
Walters S, Khan T, Ong T, Sahota O (2017) Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging 12:117–127
Wu CH, Kao IJ, Hung WC, Lin SC, Liu HC, Hsieh MH, Bagga S, Achra M, Cheng TT, Yang RS (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 29(6):1227–1242
International Osteoporosis Foundation.2013 Epidemiology, costs, and burden of osteoporosis in Hong Kong The Asia Pacific Regional Audit.
Boudou L, Gerbay B, Chopin F, Ollagnier E, Collet P, Thomas T (2011) Management of osteoporosis in fracture liaison service associated with long-term adherence to treatment. Osteoporos Int 22(7):2099–2106
Bonanni S, Sorensen AA, Dubin J, Drees B (2017) The role of the Fracture Liaison Service in osteoporosis care. Mo Med 114(4):295–298
Dreinhofer KE, Mitchell PJ, Begue T, Cooper C, Costa ML, Falaschi P et al (2018) A global call to action to improve the care of people with fragility fractures. Injury. 49(8):1393–1397
Berry SD, Miller RR (2008) Falls: epidemiology, pathophysiology, and relationship to fracture. Curr Osteoporos Rep 6(4):149–154
Sherrington C, Tiedemann A (2015) Physiotherapy in the prevention of falls in older people. Aust J Phys 61(2):54–60
Steihaug OM, Gjesdal CG, Bogen B, Kristoffersen MH, Lien G, Ranhoff AH (2017) Sarcopenia in patients with hip fracture: a multicenter cross-sectional study. PLoS One 12(9):e0184780
Hong W, Cheng Q, Zhu X, Zhu H, Li H, Zhang X, Zheng S, du Y, Tang W, Xue S, Ye Z (2015) Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS One 10(9):e0138102
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet. 359(9319):1761–1767
Kim SH, Szabo RM, Marder RA (2012) Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res 64(3):407–414
Funding
This study was financially supported by the Knowledge Transfer Fund 2019, the Chinese University of Hong Kong (Re: KPF19HKLF14).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wong, R.M.Y., Ho, W.T., Wai, L.S. et al. Fragility fractures and imminent fracture risk in Hong Kong: one of the cities with longest life expectancies. Arch Osteoporos 14, 104 (2019). https://doi.org/10.1007/s11657-019-0648-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0648-4