Abstract
Summary
Health status (HS) and influencing factors in HS were evaluated six and 12 months after hip fracture. One-third of the patients did not reach their pre-fracture HS within 1 year. HS before fracture and fall risk could, inter alia, be identified as influencing factors.
Purpose
From a patient’s perspective, regaining pre-fracture health status (HS) is one of the most important factors concerning the outcome after hip fracture. The aim of this study was to evaluate the HS and particularly to identify influencing factors in HS 6 and 12 months after hip fracture.
Methods
A total of 402 patients with hip fractures aged 60 years and older were included. HS was evaluated using the EQ-5D questionnaire pre-fracture and at 6 and 12 months after surgery. Multivariate regression analysis was performed to identify influencing factors in HS at 6 and 12 months. Afterwards, the results in the EQ-5D index were dichotomized into worse and equal/better results than before fracture, and a multivariate logistic regression analysis was performed for the dichotomized variables at 6 and 12 months.
Results
The EQ-5D index decreased from 0.71 before the fracture to 0.60 at 6 months (p < 0.001) and increased slightly to 0.63 at 12 months (p = 0.328). A high pre-fracture EQ-5D index was associated with not reaching the pre-fracture EQ-5D index, and a high Tinetti score at hospital discharge was associated with reaching the pre-fracture EQ-5D index at 6 and 12 months. A high ASA score was an influencing factor behind a lower EQ-5D index than before the fracture at 6 months.
Conclusions
Hip fractures constitute a deep and long-lasting drop in the patients’ HS. Early and intensive physiotherapy and individualized rehabilitation programmes regarding a patient’s living situation before the fracture seem to be essential to improve HS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fractures are one of the major health problems in the elderly population [1,2,3]. Besides their immense health economical relevance [4,5,6,7], hip fractures usually result in substantial consequences for each individual patient. The outcome after hip fracture is rather poor, with 18–33% mortality in the first year after the fracture [3, 8,9,10,11,12,13], 35–64% new nursing home admissions in previously non-institutionalized patients [12, 14] and 29–90% of the patients retaining permanent functional limitations [12, 14,15,16,17].
Besides those objective facts, another important aspect is the patient-based, subjective evaluation of the outcome, particularly with regard to the patients’ self-rated health status [18].
Previous studies report both health status (HS) and health-related quality of life (HRQOL) of the majority of patients recovering in the first 6 months after hip fracture, albeit not returning to the pre-fracture level [19,20,21,22,23,24,25,26]. Only a limited number of studies with partly inconclusive results have evaluated influencing factors in HS and HRQOL after hip fractures [16, 19, 27,28,29,30]. However, identifying influencing factors in HS would be essential to improve the patients’ quality of life after hip fracture.
The aim of this study therefore was to evaluate HS and particularly to identify influencing factors in HS 6 and 12 months after hip fracture.
Methods
Study design and patients
The current investigation is a secondary analysis of a prospective observational study including a total of 402 patients with hip fractures aged 60 years and older who were admitted to our university hospital for surgical fracture treatment [31]. The recruitment period was from 1 April 2009 to 30 September 2011. Institutional review board approval was obtained from the ethics committee (AZ 175/08). All of the patients provided written informed consent for participation in the study. Patients with malignancy-related fractures and polytrauma (ISS ≥ 16) were excluded [32].
Assessment of self-rated health status
Self-rated health status was evaluated using the EQ-5D-3L (three-level version) questionnaire. The EQ-5D questionnaire is a standardized measuring instrument of health status developed by the EuroQol Group [33]. It records the patient’s self-rated health with regard to five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression, with three levels of severity (1: no problems; 2: some or moderate problems; 3: extreme problems) for each of the five dimensions [34]. The responses to the five dimensions are then converted in a single summary index value (EQ-5D index) using a country-specific value set, which provides weights for each health state description according to the preferences of the general population of a country [35]. For this study, the German value set was applied [36]. The EQ-5D index score ranges from a maximum score of 1, indicating perfect health, to less than 0, indicating a health state worse than death (0 indicates a health state equivalent to death) [35].
The EQ-5D was assessed at the following times: pre-fracture (retrospectively evaluated at the day of admission to the hospital, regarding the last week before the fracture occurred), and at 6 and 12 months after surgery.
Additional patient data
Apart from socio-demographic patient data (age, sex), the type of fracture, operative procedure, American Society of Anesthesiologists (ASA) score (physical status classification; score ranging from 1 (healthy person) to 6 (brain-dead person)) [37], pre-fracture nursing care level and several geriatric scores were recorded: pre-fracture Charlson comorbidity index (CCI; score to assess comorbidity using a summary measure of 19 comorbid conditions weighted from 1 to 6 based on disease severity, total score ranging from 0 to 37) [38]; pre-fracture Barthel index (BI; score to measure performance in activities of daily living, score ranging from 0 (worst) to 100 points (optimal performance)) [39], preoperative Mini-Mental State Examination (MMSE; cognitive screening instrument, score ranging from 0 (worst) to 30 points (optimal performance)) [40], pre-fracture Geriatric Depression Scale (GDS; assessment tool to identify depression in elderly patients, score ranging from 0 (normal) to 30 points (severe depression)) [41], Tinetti test at hospital discharge (test to assess balance abilities and fall risk, score ranging from 0 (worst) to 28 points (optimal performance)) [42]. In addition, the time interval between hospital admission and surgery, the discharge type (geriatric rehabilitation, nursing home, home) and the occurrence of a postoperative delirium were recorded. All scores were recorded by a member of our study group (physician or specially trained medical student).
Data management and analysis
Data were collected in a FileMaker® database (FileMaker Inc., Santa Clara, CA, USA). Double entry was performed with a plausibility check to monitor for data quality. IBM SPSS Statistics 22 (Statistical Package for the Social Sciences, IBM Corporation, Armonk, NY, USA) was used for statistical analysis. The data were presented as frequencies and percentages for dichotomous variables, and as means and 95% confidence intervals for numerous parameters. For all tests, statistical significance was assumed at p < 0.05. Statistical analysis was performed in two steps.
In the first step, the scores in the EQ-5D index before the fracture and 6 and 12 months after surgery were calculated. Afterwards, a univariate analysis for the EQ-5D index at both 6 and 12 months after the surgery was executed with the following covariates: age, sex, fracture type, operative procedure, ASA score, pre-fracture nursing care level, pre-fracture CCI, pre-fracture BI, preoperative MMSE, preoperative GDS, Tinetti test at hospital discharge, time interval between hospital admission and surgery, discharge type (geriatric rehabilitation, nursing home, home), postoperative delirium and pre-fracture EQ-5D index. In the next step, a multivariate regression analysis with forward stepwise selection was performed for the EQ-5D index at both 6 and 12 months after the surgery, including all variables that were significant in the univariate analysis at 6 and 12 months after the surgery, respectively. Data were presented with standardized regression coefficients (β), non-standardized regression coefficients (B) and 95% confidence intervals of non-standardized regression coefficients.
Then, the results in the EQ-5D index after both 6 and 12 months were dichotomized into results which were worse and results which were equal to or better than the pre-fracture EQ-5D index. Afterwards, multivariate logistic regression analysis with forward stepwise selection was performed for the dichotomized variables at 6 and 12 months after the surgery. This analysis included the following co-variables: pre-fracture EQ-5D index, age, fracture type, operative procedure, pre-fracture BI, preoperative ASA score, pre-fracture CCI, preoperative MMSE, Tinetti test at hospital discharge and delirium. Data were presented with non-standardized regression coefficients (B), odds ratios (OR) and 95% confidence intervals of OR.
Results
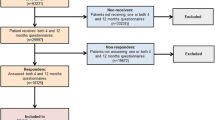
Of all 402 patients included in the study, 82 patients had died by the follow-up investigation 6 months after the fracture, and another 33 patients had died by the 12-month follow-up investigation. Additionally, 53 patients were lost to follow-up and another 100 patients had incomplete data concerning the EQ-5D or one of the other analysed scores at 6 months; 86 patients were lost to follow-up and another 63 patients had incomplete data at 12 months after the fracture. Ultimately, 167 and 150 patients could be included in the analysis at 6 and 12 months after the fracture, respectively (Fig. 1).
The mean age of the patients at the time of surgery was 81 years; 73% were female. Detailed patients’ characteristics are shown in Table 1. Table 2 compares characteristics of patients who were included in the analyses, patients who were lost to follow-up or had incomplete EQ-5D data and patients who died at 6 and 12 months, respectively.
The EQ-5D index decreased significantly from 0.71 (min, − 0.21; max, 1.0; SD, 0.29) on average before the fracture to 0.60 (min, − 0.21; max, 1.0; SD, 0.33) at 6 months (p = 0.000) and increased slightly to 0.63 (min, − 0.21; max, 1.0; SD, 0.34) at 12 months after the surgery (p = 0.328).
In univariate regression analysis for the EQ-5D index at 6 months after the surgery, age, pre-fracture BI, ASA score, pre-fracture CCI, fracture type, pre-fracture GDS, preoperative MMSE, pre-fracture nursing care level, Tinetti test at hospital discharge, operative procedure and postoperative delirium were significant influencing factors.
Multivariate analysis showed that Tinetti score at hospital discharge and pre-fracture BI score were independent positive influencing factors and that GDS score and ASA score were independent negative influencing factors for the EQ-5D index at 6 months after the surgery (Table 3).
In univariate regression analysis for the EQ-5D index at 12 months after the surgery, age, pre-fracture BI, ASA score, pre-fracture CCI, pre-fracture GDS, preoperative MMSE, Tinetti test at hospital discharge and postoperative delirium were significant influencing factors.
Tinetti score at hospital discharge, pre-fracture BI score and MMSE score were independent positive influencing factors for the EQ-5D index at 12 months after the surgery (Table 4).
At 6 months after the surgery, 40% of patients (n = 68) had a lower EQ-5D index than before the fracture, and 60% (n = 100) had an equal or better result than before; at the 12-month follow-up investigation, 31% (n = 49) had a lower EQ-5D index, and 69% (n = 110) had an equal or better result than before the fracture.
Logistic regression analysis showed that, at 6 months after the surgery, a high pre-fracture EQ-5D index and a high ASA score were independent influencing factors behind a lower EQ-5D index than before the fracture and a high Tinetti score at hospital discharge was an independent influencing factor behind an equal or higher EQ-5D index than before the fracture (Table 5). At 12 months, a high pre-fracture EQ-5D index was the only independent influencing factor behind a lower EQ-5D index, and a high Tinetti score was the only independent influencing factor behind an equal or higher EQ-5D index (Table 6).
Discussion
The purpose of this study was to evaluate self-rated health status, measured by using the EQ-5D questionnaire, and to identify influencing factors in the health status 6 and 12 months after hip fracture. The EQ-5D index had deteriorated significantly by the 6-month follow-up investigation and had improved again slightly 12 months after the fracture. Six and 12 months after the fracture, 40% and 31% of the patients, respectively, had a lower EQ-5D index than before the hip fracture. These results confirm the findings of previous studies that hip fractures constitute a deep and usually also long-lasting drop in the patients’ health status, with almost one-third not reaching the pre-fracture status within 1 year after the fracture.
A high score in the EQ-5D index before the fracture was associated with a higher risk of not reaching the pre-fracture EQ-5D index score at 6 and 12 months after the fracture, whereas a low risk of falling, measured using the Tinetti test, was associated with a higher probability of reaching the pre-fracture EQ-5D index score at 6 and 12 months after the fracture. Additionally, a bad general health status, measured by the ASA score, was found to be an independent influencing factor in not reaching the pre-fracture EQ-5D index score at 6 months, but not at 12 months after the fracture.
The EQ-5D values found at the different time-points in our study population (pre-fracture 0.71, 6 months 0.60, 12 months 0.63) are consistent with the results of other studies. Svedbom et al. report an EQ-5D index of 0.71 before the fracture, 0.54 at 4 months and 0.64 at 12 months after the fracture [43]. In a systematic review of health state utility values including 12 studies concerning hip fractures, Peasgood et al. report a pooled EQ-5D index of 0.76 before the fracture, 0.57 at 4 months and 0.6 at 12 months after the fracture [44].
Health status improved slightly in the period from 6 to 12 months after the fracture but, with an average score of 0.63, remained considerably below the average age-specific EQ-5D index of 0.84 in the German population aged 75 years and older [45]. On the one hand, these numbers demonstrate that hip fractures constitute a deep and long-lasting drop in the patients’ health status. On the other hand, it has to be considered that in our study population, with an average score of 0.71, the pre-fracture EQ-5D index was already below the age-appropriate reference value. This fact can be explained by the association of disability and frailty with a higher risk of falling and thus suffering a hip fracture. Similar findings were reported by Randell et al., who found a lower baseline HRQOL in hip fracture patients compared with a control group of osteoporosis patients without fracture [24] and by Borgström et al., who described a lower pre-fracture HRQOL in hip fracture patients (0.77) than in patients with vertebral fractures (0.88) [46].
Recent studies have shown that cognitive dysfunction [19, 30], comorbidities, higher ASA score [19, 27], postoperative pain [28] and low physical or psychosocial functioning before the fracture [16, 19, 29] are associated with a poorer health status after hip fracture. In agreement with these studies, we found that cognitive dysfunction is associated with a poorer health status 12 months after the fracture and that a bad general health status, measured by the ASA score, is associated with a poorer health status as well as higher odds of not reaching the pre-fracture health status 6 months after the fracture. Furthermore, we identified a high pre-fracture BI as an influencing factor behind a better health status 6 and 12 months after the fracture, which correlates with previous findings that, conversely, low physical functioning before the fracture is associated with a poorer health status after hip fracture.
An unexpected finding of our study was the fact that a high score in the EQ-5D index before the fracture was associated with a higher risk of not reaching the pre-fracture EQ-5D index at 6 and 12 months after the fracture. Conflicting with our results, previous studies have indicated that a low pre-fracture HS is associated with a poorer HS 3 months after hip fracture [29] and that higher scores of baseline HRQOL are associated with a lower probability of having reduced scores on the BI and Lawton scale 6 months after the fracture [16]. A possible explanation for this might be the fact that, first, patients with a better pre-fracture HS have higher demands on postoperative HS than patients with a poorer pre-fracture HS and, second, patients with a better pre-fracture HS were probably more active before the fracture and might not achieve their pre-fracture level of activity, whereas patients with restricted mobility already before the fracture might have better chances of recovering their pre-fracture level. The different results of the previous investigations might be explained by the shorter follow-up period in the study by Sylliaas et al. and by the fact that Vergara et al. measured the patients’ abilities to perform activities of daily living and not their HS at 6 months after the fracture. Functional abilities and self-reported HS might differ due to the fact that functional outcome and the patients’ perception of functioning can be different.
Regarding the results of this study and especially the fact that one-third of the surviving patients had not reached their pre-fracture health status within 1 year after the fracture, it seems essential to find ways to improve the outcome after hip fractures. A key point should be to address the variables which could be identified as independent influencing factors in this study. Pre-fracture EQ-5D index and general health status, which have been identified as influencing factors, are not influenceable, but can well be utilized to estimate the outcome/prognosis of a patient and to identify patients who are especially at risk of deteriorating after hip fractures. Developing special interventions and adjusted rehabilitation programmes for these risk groups regarding a patient’s individual living situation and HS before the fracture might help to improve the long-term HS of these patients.
In contrast, a lower fall risk, which could be identified as an independent positive influencing factor at 6 and 12 months after the fracture can be influenced in several ways. Early and intensive physiotherapy with gait training, training of balance and strength and geriatric rehabilitation programmes after hospital discharge seem to be crucial in this context. Previous studies support these findings by demonstrating that strength training is associated with a better health status in both short- and long-term follow-up [22, 47, 48]. Furthermore, reducing the fall risk is essential to prevent subsequent fractures, which occur in up to 35% of hip fracture patients and cause further deterioration of the health status [49].
Limitations
Our study has some limitations. First, pre-fracture BI, MMSE and GDS had to be evaluated retrospectively at the day of admission to the hospital, regarding the last week before the fracture occurred. Second, the patient collective is inhomogeneous with regard to fracture type and operative procedure. However, this could also be seen as a strength because it reflects the reality in everyday clinical practice and a high number of patients could be provided.
Another point that might weaken the quality of the statistical analyses is the fact that different subgroups were included in the analyses before, at 6 and 12 months after the fracture because some patients had died, were lost to follow-up or had incomplete data sets. Because of this reason, the different subgroups might not be representative for the entire sample.
Furthermore, only a limited number of variables could be included into the regression analysis in order not to decrease the quality of the statistical analysis. Therefore, it cannot be excluded that relevant variables have not been tested.
Another possible limitation is the fact that the study was conducted from 2009 until 2011. However, the surgical procedures and treatment algorithms in our hospital have not changed in the meantime.
Last, the question has to be raised of whether the EQ-5D index is the right assessment instrument with which to measure HS after hip fracture. The EQ-5D has some advantages. It is an established, validated and simple questionnaire. However, a possible weakness of the EQ-5D is its distributional properties. Several studies indicate that there is a ceiling effect especially for the EQ-5D-3L (three-level) version because the dimensions are limited to only three response choices per item [50,51,52,53]. Because of this ceiling effect, particularly less severe morbidity might not be reported [53]. On the other hand, Lutomski et al. found out that the EQ-5D has poor discriminative ability for healthy older persons due to ceiling effects, but adequate discriminative ability in older persons with major geriatric conditions [53]. As most hip fracture patients have major geriatric conditions, using the EQ-5D seems to be reasonable for our study population.
There are several assessment instruments for HS and HRQOL other than EQ-5D, such as the Short Form 36 (SF-36) and Short Form 12 (SF-12) health surveys; Assessment of Quality of Life (AQoL); and ICECAP-O (ICEpop CAPability measure for Older people), a measure of capability in elderly people. Some investigations have demonstrated that the EQ-5D index seems to be an adequate instrument for measuring the HS of hip fracture patients [54, 55].
Conclusion
In conclusion, the results of this prospective study confirm that hip fractures constitute a deep and usually also long-lasting drop in patients’ health status. A high pre-fracture EQ-5D index was associated with poorer chances of reaching pre-fracture health status, and a low risk of falling, measured by the Tinetti test, was associated with a higher health status 6 and 12 months after the fracture and with better chances of reaching pre-fracture health status.
In this context, early and intensive physiotherapy and the development of individualized rehabilitation programmes regarding a patient’s living situation before the fracture seem to be essential.
References
Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B (2011) Osteoporosis: burden, health care provision and opportunities in the EU: a report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 6:59–155
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C, Life IWGoEaQo (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Cheng SY, Levy AR, Lefaivre KA, Guy P, Kuramoto L, Sobolev B (2011) Geographic trends in incidence of hip fractures: a comprehensive literature review. Osteoporos Int 22:2575–2586
Singer A, Exuzides A, Spangler L, O'Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90:53–62
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res 22:465–475
Sahota O, Morgan N, Moran CG (2012) The direct cost of acute hip fracture care in care home residents in the UK. Osteoporos Int 23:917–920
Leal J, Gray AM, Prieto-Alhambra D, Arden NK, Cooper C, Javaid MK, Judge A, group Rs (2016) Impact of hip fracture on hospital care costs: a population-based study. Osteoporos Int 27:549–558
Keene GS, Parker MJ, Pryor GA (1993) Mortality and morbidity after hip fractures. BMJ 307:1248–1250
Vaseenon T, Luevitoonvechkij S, Wongtriratanachai P, Rojanasthien S (2010) Long-term mortality after osteoporotic hip fracture in Chiang Mai, Thailand. J Clin Densitom 13:63–67
Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF, Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP, Rosenthal GE, Wolinsky FD (2009) The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol 170:1290–1299
da Costa JA, Ribeiro A, Bogas M, Costa L, Varino C, Lucas R, Rodrigues A, Araújo D (2009) Mortality and functional impairment after hip fracture - a prospective study in a Portuguese population. Acta Reumatol Port 34:618–626
Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM (2006) Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma 20:172–178 discussion 179-180
Davidson CW, Merrilees MJ, Wilkinson TJ, McKie JS, Gilchrist NL (2001) Hip fracture mortality and morbidity--can we do better? N Z Med J 114:329–332
Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ (2002) Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc 50:1644–1650
Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE (1990) Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol 45:M101–M107
Vergara I, Vrotsou K, Orive M, Gonzalez N, Garcia S, Quintana JM (2014) Factors related to functional prognosis in elderly patients after accidental hip fractures: a prospective cohort study. BMC Geriatr 14:124
Bertram M, Norman R, Kemp L, Vos T (2011) Review of the long-term disability associated with hip fractures. Inj Prev 17:365–370
Ayers DC, Bozic KJ (2013) The importance of outcome measurement in orthopaedics. Clin Orthop Relat Res 471:3409–3411
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47:1369–1382
Peterson MG, Allegrante JP, Cornell CN, MacKenzie CR, Robbins L, Horton R, Ganz SB, Augurt A (2002) Measuring recovery after a hip fracture using the SF-36 and Cummings scales. Osteoporos Int 13:296–302
van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ (2001) Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res 390:232–243
Hagsten B, Svensson O, Gardulf A (2006) Health-related quality of life and self-reported ability concerning ADL and IADL after hip fracture: a randomized trial. Acta Orthop 77:114–119
Shyu YI, Chen MC, Liang J, Lu JF, Wu CC, Su JY (2004) Changes in quality of life among elderly patients with hip fracture in Taiwan. Osteoporos Int 15:95–102
Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA (2000) Deterioration in quality of life following hip fracture: a prospective study. Osteoporos Int 11:460–466
Tidermark J, Zethraeus N, Svensson O, Törnkvist H, Ponzer S (2002) Femoral neck fractures in the elderly: functional outcome and quality of life according to EuroQol. Qual Life Res 11:473–481
Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR (2012) Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. J Am Geriatr Soc 60:1268–1273
Chen LH, Liang J, Chen MC, Wu CC, Cheng HS, Wang HH, Shyu YL (2017) The relationship between preoperative American Society of Anesthesiologists Physical Status Classification scores and functional recovery following hip-fracture surgery. BMC Musculoskelet Disord 18:410
Shyu YI, Chen ML, Chen MC, Wu CC, Su JY (2009) Postoperative pain and its impact on quality of life for hip-fractured older people over 12 months after hospital discharge. J Clin Nurs 18:755–764
Sylliaas H, Thingstad P, Wyller TB, Helbostad J, Sletvold O, Bergland A (2012) Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disabil Rehabil 34:1225–1231
Sanz-Reig J, Lizaur-Utrilla A, Serna-Berna R (2012) Outcomes in nonagenarians after hemiarthroplasty for femoral neck fracture. A prospective matched cohort study. Hip Int 22:113–118
Buecking B, Struewer J, Waldermann A, Horstmann K, Schubert N, Balzer-Geldsetzer M, Dodel R, Bohl K, Ruchholtz S, Bliemel C (2014) What determines health-related quality of life in hip fracture patients at the end of acute care? A prospective observational study. Osteoporos Int 25:475–484
Baker SP, O'Neill B, Haddon W, Long WB (1974) The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 14:187–196
EuroQol Group (1990) EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
Gusi N, Olivares PR, Rajendram R (2010) The EQ-5D health-related quality of life questionnaire. In: Preedy VR, Watson RR (eds) Handbook of disease burdens and quality of life measures. Springer, New York, pp 87–99
Van Reenen M, Oppe M (2015) EQ-5D-3L User Guide. https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-3L_UserGuide_2015.pdf. Accessed 31 May 2019
Greiner W, Claes C, Busschbach JJ, von der Schulenburg JM (2005) Validating the EQ-5D with time trade off for the German population. Eur J Health Econ 6:124–130
Saklad M (1941) Grading of patients for surgical procedures. Anesthesiology 2:281–284
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Tinetti ME (1986) Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
Svedbom A, Borgström F, Hernlund E, Ström O, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Uusküla A, Lember M, Kallikorm R, Lesnyak O, McCloskey E, Ershova O, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jönsson B, Kanis JA (2018) Quality of life after hip, vertebral, and distal forearm fragility fractures measured using the EQ-5D-3L, EQ-VAS, and time-trade-off: results from the ICUROS. Qual Life Res 27:707–716
Peasgood T, Herrmann K, Kanis JA, Brazier JE (2009) An updated systematic review of Health State Utility Values for osteoporosis related conditions. Osteoporos Int 20:853–868
Janssen B, Szende A (2014) Population norms for the EQ-5D. In: Szende A, Janssen B, Cabases J (eds) Self-reported population health: an international perspective based on EQ-5D. Springer, New York, pp 19–30
Borgström F, Lekander I, Ivergård M, Ström O, Svedbom A, Alekna V, Bianchi ML, Clark P, Curiel MD, Dimai HP, Jürisson M, Kallikorm R, Lesnyak O, McCloskey E, Nassonov E, Sanders KM, Silverman S, Tamulaitiene M, Thomas T, Tosteson ANA, Jönsson B, Kanis JA (2013) The International Costs and Utilities Related to Osteoporotic Fractures Study (ICUROS)--quality of life during the first 4 months after fracture. Osteoporos Int 24:811–823
Zidén L, Frändin K, Kreuter M (2008) Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. Clin Rehabil 22:1019–1033
Allegrante JP, Peterson MG, Cornell CN et al (2007) Methodological challenges of multiple-component intervention: lessons learned from a randomized controlled trial of functional recovery after hip fracture. HSS J 3:63–70
Kanis JA, Johansson H, Odén A, Harvey NC, Gudnason V, Sanders KM, Sigurdsson G, Siggeirsdottir K, Fitzpatrick LA, Borgström F, McCloskey EV (2018) Characteristics of recurrent fractures. Osteoporos Int 29:1747–1757
Buchholz I, Janssen MF, Kohlmann T, Feng YS (2018) A systematic review of studies comparing the measurement properties of the three-level and five-level versions of the EQ-5D. Pharmacoeconomics 36:645–661
Bharmal M, Thomas J (2006) Comparing the EQ-5D and the SF-6D descriptive systems to assess their ceiling effects in the US general population. Value Health 9:262–271
Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, Swinburn P, Busschbach J (2013) Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 22:1717–1727
Lutomski JE, Krabbe PF, Bleijenberg N et al (2017) Measurement properties of the EQ-5D across four major geriatric conditions: findings from TOPICS-MDS. Health Qual Life Outcomes 15:45
Milte R, Crotty M, Miller MD, Whitehead C, Ratcliffe J (2018) Quality of life in older adults following a hip fracture: an empirical comparison of the ICECAP-O and the EQ-5D-3 L instruments. Health Qual Life Outcomes 16:173
Parsons N, Griffin XL, Achten J, Costa ML (2014) Outcome assessment after hip fracture: is EQ-5D the answer? Bone Joint Res 3:69–75
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional review board approval was obtained from the ethics committee (AZ 175/08). All of the patients provided written informed consent for participation in the study.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hack, J., Buecking, B., Aigner, R. et al. What are the influencing factors in self-rated health status after hip fracture? A prospective study on 402 patients. Arch Osteoporos 14, 92 (2019). https://doi.org/10.1007/s11657-019-0642-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-019-0642-x