Abstract
Summary
The distribution of bone tissue within the vertebra can modulate vertebral strength independently of average density and may change with age and disc degeneration. Our results show that the age-associated decrease in bone density is spatially non-uniform and associated with disc health, suggesting a mechanistic interplay between disc and vertebra.
Purpose
While the decline of bone mineral density (BMD) in the aging spine is well established, the extent to which age influences BMD distribution within the vertebra is less clear. Measures of regional BMD (rBMD) may improve predictions of vertebral strength and suggest how vertebrae might adapt with intervertebral disc degeneration. Thus, we aimed to assess how rBMD values were associated with age, sex, and disc height loss (DHL).
Methods
We measured rBMD in the L3 vertebra of 377 participants from the Framingham Heart Study (41–83 years, 181 M/196 F). Integral (Int.BMD) and trabecular BMD (Tb.BMD) were measured from QCT images. rBMD ratios (anterior/posterior, superior/mid-transverse, inferior/mid-transverse, and central/outer) were calculated from the centrum. A radiologist assigned a DHL severity score to adjacent intervertebral discs (L2–L3 and L3–L4).
Results
Int.BMD and Tb.BMD were both associated with age, though the decrease across age was greater in women (Int.BMD, − 2.6 mg/cm3 per year; Tb.BMD, − 2.6 mg/cm3 per year) than men (Int.BMD, − 0.5 mg/cm3 per year; Tb.BMD, − 1.2 mg/cm3 per year). The central/outer (− 0.027/decade) and superior/mid-transverse (− 0.018/decade) rBMD ratios were negatively associated with age, with similar trends in men and women. Higher Int.BMD or Tb.BMD was associated with increased odds of DHL after adjusting for age and sex. Low central/outer ratio and high anterior/poster and superior/mid-transverse ratios were also associated with increased odds of DHL.
Conclusions
Our results indicate that the distribution of bone within the L3 vertebra is different across age, but not between sexes, and is associated with disc degeneration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Aging increases the risk of musculoskeletal disorders in the spine, such as osteoporosis [1], vertebral fractures [2], herniated discs [3], and non-specific back pain [4]. Age-related changes widely observed in vertebral bone and intervertebral disc (IVD) are key factors in many of these cases. Loss of vertebral bone mineral density (BMD) with age [1, 5,6,7,8,9,10,11,12], for example, has been correlated with declines in vertebral bone strength and stiffness [9]. Lower BMD [6] and faster loss [1, 10] of BMD with age have been implicated in the increased risk of incident fractures in older women compared to older men [2, 13]. Degenerative changes in the aging IVD, including a loss of nuclear material and intradiscal pressure [14], are associated with vertebral joint dysfunction, instability, and pain [15].
The spatial resolution of computed tomography (CT) permits regional decomposition of BMD measures within the trabecular centrum, enabling study of the role of a heterogeneous distribution of bone mineral within the vertebral body [16, 17]. The ability of the vertebrae to avoid fracture may be critically linked to this distribution. A relatively high density of bone in the posterior versus the anterior vertebral body, for example, may provide high vertebral strength under compression [17] and thereby reduce the risk of fracture. Ex vivo evidence suggests that the distribution of BMD within the centrum changes with age, with a preferential loss of bone in the sub-endplate [5, 8] and central [8] regions in older adults. Yet, such cadaveric studies typically are challenged with limited sample numbers, increasing the risk of sample bias to an elderly population and reducing the power necessary to explore potential covariates. Thus, a better understanding of the pattern of bone loss in the vertebra is needed to provide a fuller insight into the age-related increase in risk of fracture.
Regional measures of bone mineral density (rBMD) may also shed light on how the vertebrae adapt to altered loading conditions accompanying IVD aging and degeneration [11]. Indeed, studies have observed an increase in BMD [18] and trabecular number and thickness [19] within the vertebra in the presence of disc degeneration, potentially reflecting the altered loading of bone with adjacent disc degeneration. During disc degeneration, the nucleus pulposus becomes more fibrous and less hydrated [20] resulting in a disc height loss (DHL) [21], a greater amount of force transmission through the neural arches [22], and an uneven decline in the compressive stress within the disc [23]. These changes could explain why the spatial distribution of bone tissue in the vertebral body may differ in the presence of disc degeneration, with higher and lower amounts of bone in the anterior and central regions, respectively, with advanced disc degeneration [19]. Yet, it remains to be seen how these aspects of disc degeneration interact with age- and sex-associated alterations [10] in the distribution of bone tissue in the vertebral body.
The relationship between IVD degeneration and the spatial distribution of bone tissue has only been observed in a limited number of studies on cadaveric spine segments, not in a large in vivo cohort where additional covariates of age and sex can be assessed. Here, we performed a cross-sectional study of 377 participants across four decades of life from the Framingham Heart Study [24]. We aimed to examine the age- and sex-dependent differences in the regional distribution of vertebral trabecular bone density. We hypothesized: (1) the central/outer rBMD ratio would present a similar decrease with age in women and men, and (2) individuals with higher central/outer and lower anterior/posterior rBMD ratios would have greater risk of degeneration of the adjacent IVDs.
Methods
Subject demographics
Our study includes 377 participants (181 M/196 F), 41 to 83 years old, selected using sex- and age-stratified random samplings from the community-based offspring and third generation cohorts of the Framingham Heart Study Multidetector Computed Tomography (MDCT). Detailed methods of recruitment and data collection have previously been published [10]. As part of a study of kyphosis and spinal degeneration, MDCT cohort members had CT images evaluated for vertebral fracture and disc height lost [25]. For the present study, inclusion criteria required participants to be fracture-free at all vertebral levels and have the L3 vertebra and adjacent discs fully visible within the quantitative computed tomography (QCT) scans. All participants signed written informed consent before enrollment and examination. Our study was approved by the Institutional Review Board at Boston University Medical Center.
Image collection and processing
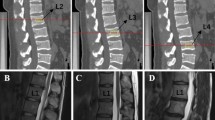
QCT scans were acquired using an eight-slice multidetector CT scanner (GE Lightspeed Ultra/Plus, General Electric Medical Systems, Waukesha, WI, USA). Details of the imaging protocol have been published previously [10, 26]. Abdominal QCT scans were collected using a nominal in-plane pixel size of 0.68 × 0.68 mm, a slice thickness of 2.5 mm, tube voltage of 120 kVp, tube current 120/400 mA (for participants ≤ 200/> 200 lb. body weight, respectively), gantry rotation of 500 ms, and a data collection diameter of 500 mm. From these scans, the cortical and trabecular bone of the L3 vertebral body were separately contoured using Canny edge detection [27] on each axial slice (Fig. 1). Schmorl’s nodes and osteophytes were both included in the trabecular and cortical contours, respectively. Further details on contouring can be found in the Supplemental Information. A calibration phantom with hydroxyapatite regions (Image Analysis, Columbia, KY, USA) was used to linearly translate pixel intensity to equivalent mineral density, and vertebral bodies were analyzed for measures of integral BMD (Int.BMD, mg/cm3, inclusive of endplate and cortical bone) and trabecular BMD (Tb.BMD, mg/cm3, exclusive of endplate and cortical bone).
Axial slice of an example QCT image of the L3 vertebra with contours of the cortical (black) and trabecular (red) bone used to calculate Int.BMD and Tb.BMD, respectively: The QCT image was then subdivided into 27 regions, the superior-most nine of which are shown by the black grid in (A), and the rBMD was calculated for each of the seven regions shown (B)
Regional values of volumetric BMD (rBMD) were then calculated from semi-automatically defined subregions of the trabecular contour. For this process, the L3 vertebra was first aligned in the sagittal plane. The first slice and last slice of the vertebral body were then manually selected. Slices with partial views of the endplate were included in this range if the visible bone was primarily trabecular and the regions of cortical bone within the slice were continuous. The most lateral, anterior, and posterior points on the cortical shell of the vertebral body were manually selected. These points were then used together with the trabecular contour to define 27 subregions of the vertebral body (three layers of nine subregions) (Fig. 1; further details can be found in the Supplemental Information). These subdivisions were combined to calculate the rBMD for each of the following regions: anterior, posterior, superior, mid-transverse, inferior, central, and outer (Fig. 1). Anterior, posterior, central, and outer regions included all three layers of the vertebral body. As individual rBMD values were highly intercorrelated (Supplemental Information), we used four ratios of rBMD values (anterior/posterior, central/outer, superior/mid-transverse, and inferior/mid-transverse), rather than the individual rBMD values, to capture the distribution of bone within the centrum.
CT imaging assessments of disc height loss were performed using a Myrian platform (Version 1.12, Intrasense SA). A single trained musculoskeletal radiologist (MJ) assessed DHL of levels L2–L3 and L3–L4 on sagittal reformat reconstructions, using standardized, validated methods together with an atlas based on Videman’s grading system. The Videman’s grading system is a visual assessment of a reduction in disc height relative to the height of the disc immediately superior (reference disc): 0 = normal (disc height greater than height of disc immediately superior), 1 = mild (disc height equal to height of disc immediately superior), 2 = moderate (disc height less than height of disc immediately superior), and 3 = severe (vertebral endplates almost in contact) [25, 28, 29]. To evaluate reliability, the reader assessed DHL for 30 individuals on two separate occasions approximately 6 months apart. Intraclass correlation coefficients for intra-reader reliability were 0.80 to 1.00.
Statistical analyses
Linear regression models assessed the association of BMD (Int.BMD, Tb.BMD, and rBMD ratios) with age and sex and evaluated age by sex interaction. Generalized estimating equations (GEE) were applied to account for potential correlation among observations within age-sex stratification clusters. If a significant age by sex interaction was found, then a linear regression model assessing the association between age and BMD was run separately in women and men.
We used conditional logistic regression to assess the association between the age- and sex-adjusted rBMD ratios (independent variable) and DHL score (dependent variable). Three dichotomous comparisons of DHL scores were defined: no DHL (score = 0 at both the L2/L3 and L3/L4 levels; N = 180) vs. mild-to-severe DHL (“DHL1+,” score = 1, 2, or 3 at either the L2/L3 or L3/L4 level; N = 197); no DHL vs. moderate-to-severe DHL (“DHL2+,” score = 2 or 3; N = 103), and no DHL vs. severe DHL (“DHL3,” score = 3; N = 13). Regression models were analyzed both with and without adjustment for height and weight to correct for potential confounding. The significance level for p values was 0.05.
Results
Study sample
Mean age was 61 in both women and men. Men were heavier and taller than women, with a mean (SD) weight of 87.6 (15.6) kg versus 72.0 (13.8) kg and a height of 1.8 (0.07) m versus 1.6 (0.07) m, respectively (Table 1).
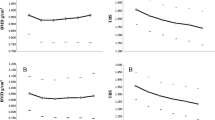
Age- and sex-related changes in vertebral bone
Integral and trabecular BMD measures of the L3 vertebrae were age- and sex-dependent. Women had a greater bone loss with age than men for both integral (women: β (SE) = − 2.6 (0.5) mg/cm3 per year; men: − 0.5 (0.2) mg/cm3 per year; interaction p < 0.01) and trabecular BMD (women: β (SE) = − 2.6 (0.4) mg/cm3 per year; men: − 1.2 (0.1) mg/cm3 per year; interaction p < 0.01) (Fig. 2).
The distribution of bone within the centrum, as measured by the rBMD ratios, was also associated with age and sex. Men had a lower central/outer ratio than women (age-adjusted mean (SD) of − 1.0 (7.9) % for men and 0.9 (10.3) % for women; p < 0.01), though this difference between sexes did not remain significant after accounting for height and weight (p = 0.96). Further, the central/outer (β (SE) = − 2.7 (0.6) × 10−3 per year, p < 0.01) and superior/mid-transverse (β (SE) = − 1.8 (0.5) × 10−3 per year, p < 0.01) ratios were negatively associated with age (Fig. 3). Unless otherwise noted, the inclusion of height and weight did not alter the results of the models.
Association (beta coefficient) between age and ratios of rBMD in the L3 vertebra. The central/outer, and superior/mid-transverse ratios declined with age similarly between men and women (interaction p = 0.83 for central/outer and interaction p = 0.31 for superior/mid-transverse). The anterior/posterior and inferior/mid-transverse ratios were not associated with age
Relationship between vertebral bone density and disc height loss
Increased risk of DHL was associated with increases in Int.BMD and Tb.BMD after adjusting for age and sex (Table 2). Similarly, an increase in age- and sex-adjusted anterior/posterior and superior/mid-transverse ratios were associated with greater risk of DHL. Conversely, a decrease in central/outer ratio was associated with increased odds of DHL. No other rBMD ratios were associated with DHL (all p values greater than 0.06). As there were only a few cases of severe DHL (N = 13), the confidence intervals for associations between bone metrics and severe DHL were wide (Table 2).
Discussion
While declines in density have been widely observed within the aging vertebra, age-related changes in the intra-vertebral distribution of density have been under-studied in large cohorts. Our cross-sectional study observed 377 individuals sampled from across four decades of life to determine if the distribution of rBMD within the vertebra changes with age and sex, and if the distribution is associated with degeneration of the adjacent IVDs. The results confirm prior studies reporting that BMD declines within the L3 vertebra more quickly in women than in men [10]. In addition, we found that the age-associated decline is non-uniform in both sexes, most notably with a decline in the central/outer and superior/mid-transverse rBMD ratios. After adjusting for age, a low central/outer ratio and high anterior/posterior and superior/mid-transverse ratios were associated with increased odds of DHL, a marker of disc degeneration. Thus, the relative distribution of bone density within the L3 vertebra is different across age, but not between sexes, and is associated with disc degeneration.
Average measures of BMD within the vertebral body are frequently used as predictors of vertebral strength [16, 30] and risk of fracture [16]. Previous studies of the aging vertebra have observed declines in BMD of approximately 1–2.5 mg/cm3 per year [1, 6, 7, 10] and declines in bone volume fraction of 0.1–0.3% per year at the lumbar level [5, 8, 12, 31]. We observed similar rates of loss of 1.6 (95% CI = 0.8–2.3) mg/cm3 and 1.9 (1.3–2.4) mg/cm3 per year in Int.BMD and Tb.BMD in this study, which are in good agreement with the reported values.
The effect of age on BMD is seemingly different between men and women. Int.BMD has previously been shown to be lower and to decrease twice as quickly with age in women than men [9, 10], aligning with previous observations of a rise in prevalent and incident vertebral deformities and fractures in women compared to men after the age of 50 [13, 32]. Our data suggest a fivefold more rapid decline of Int.BMD in women than men, which is higher than previously reported. This discrepancy could in part be due to higher values of Int.BMD in older men in our study (~ 200 mg/cm3) compared to the previous study (~ 180 mg/cm3) [10]. Interestingly, we found that the rate of decline in Tb.BMD was only 2.5 times quicker in women than men. While the rates of decrease across age are similar for Int.BMD and Tb.BMD in women (~ 2.6 mg/cm3 per year), losses of Int.BMD across age were lower than Tb.BMD in men. Further, we found a lower central/outer rBMD ratio in men than women before adjusting for height and weight. These findings support an observation that peripheral bone (defined as the cortical shell and all of the trabecular compartment within 1 mm of the outer boundary of the shell) might be better preserved in men with age [10]. Another study on the Framingham Heart Study cohort similarly reported that the strength of the trabecular centrum decreases with age for both sexes, but the strength of the peripheral compartment (defined as the outer 2 mm of the vertebral body) decreases only in women [9]. Together, this evidence suggests that women may lose more cortical and peripheral trabecular BMD than men with age and that this loss may in part explain the discrepancies between sexes in the prevalence of vertebral fractures in older age.
However, despite their widespread use as predictors of fracture, neither areal nor integral BMD alone can fully predict vertebral strength [30, 33] or fracture risk [34]. Models incorporating the distribution of BMD can improve upon these predictions [35]. While spatial heterogeneity in the distribution of bone within the vertebral centrum has been known for decades [36], the effect of age on this distribution is not well established [8, 11, 31, 37]. Primarily using a limited number of cadaveric specimens, prior studies have identified preferential loss of bone, and associated changes in microarchitecture, in the sub-endplate [37] and central [11] regions of the vertebrae with age. These studies, however, were limited to either a single sagittal plane [37] or to a restricted population of middle-age men [11]. Our study establishes that these observations of an age-associated decline in the superior/mid-transverse and central/outer rBMD ratios hold in a large in vivo cohort across four decades of life. While men and women differed in the rates of change in Int.BMD and Tb.BMD, the pattern of bone loss (i.e., the age-associated changes in rBMD ratios) within the centrum might be conserved across sex.
IVD degeneration has been associated with higher age-adjusted vertebral BMD [18] and bone volume fraction [19]. The role of IVD health on the regional distribution of bone, however, has been less well investigated despite the general recognition that vital biochemical and biomechanical interactions between disc and bone contribute substantially to spine health. In this study, we found that the central/outer ratio was associated with mild-to-severe and moderate-to-severe DHL. This observation in our population-based cohort supports previous observations of bone loss [11, 19] and strength reduction [38] in the central region of cadaveric specimens with disc degeneration. For cases of greater DHL, we found associations with the anterior/posterior ratio (for DHL2+ and DHL3) and the superior/mid-transverse ratio (for DHL3) supporting observations of increased bone volume fraction in the superior and anterior regions in cadaveric samples with severe disc degeneration [19].
Altered loading conditions on the vertebral bone in the presence of disc degeneration may stimulate bone remodeling, offering one possible explanation for altered bone distributions with DHL. The shift in BMD between central and outer regions, for instance, mirrors the shift in pressure with disc degeneration from the nucleus pulposus to the posterior annulus fibrosus [39]. This relationship suggests a decline in force would be accompanied with a reduction in the underlying bone. The link between the age- and sex-adjusted anterior/posterior ratio and DHL, however, is less clear as the changes in compressive forces in the anterior disc with degeneration are posture-dependent [22]. Thus, establishing a direct relationship between the altered forces following IVD degeneration and BMD distribution would require careful consideration of the multitude of complex loading cases seen during activities of daily living. Further, a cross-sectional study, such as the one presented here, cannot resolve the temporal sequence of changes in regional density and IVD, preventing a test of a causal link between IVD degeneration and bone remodeling.
Large, controlled trials have shown the efficacy of osteoporosis medications, such as biophosphonates, teriparatide, abaloparatide, and denosumab, on reducing the risk of fractures in osteoporotic patients by increasing the vertebral BMD [40]. Our results and others [17] suggest that the distribution of BMD within the vertebrae may hold vital information about vertebral strength during aging. It is not currently known, however, if any osteoporosis therapies affect the BMD distribution. Understanding the natural aging progression of BMD distribution in both sexes is the first step to this end. While we did not exclude individuals who were on medication for osteoporosis from our study (N = 29), an examination of the effect of treatment on bone distribution is outside the scope of this study.
The prevalence of bony abnormalities of the vertebra, such as Schmorl’s nodes, osteophytes, and sclerotic bone (reactive bone formation), increase with age and may artificially elevate the BMD measurement [41]. These abnormalities may lead to an underdiagnosis of osteoporosis [41], but their impact on vertebral strength and fracture are not well documented. We included individuals with such abnormalities in this study and they were flagged and scored for the severity and location of the abnormality. The low occurrence of sclerotic bone in particular (N = 29) precluded a thorough statistical analysis of the effect of abnormalities on BMD metrics. A post hoc analysis, however, revealed that while the presence and severity of osteophytes and sclerotic bone were associated with increased Int.BMD and Tb.BMD, consistent with Tenne et al. [41], their inclusion did not alter the observed relationships between rBMD ratios, age, sex, and disc health.
The use of CT in our study limited our evaluation of the aging IVD to disc height loss. While DHL is a hallmark of disc degeneration [21], the measure may not be sensitive enough to capture the subtle changes associated with early disc degeneration. Magnetic resonance imaging may provide a more nuanced examination of in vivo disc health by enabling assessment of annulus tears, disc height, herniation, and hydration. Pfirrmann’s method [42] and Modic changes [43], in particular, have been correlated with histopathologic deviations and are strongly associated with back pain and disc degeneration. Concurrent studies of changes in vertebral bone via CT and IVD tissue quality via MRI across age may then provide additional insight into the interplay between these two tissues, though would be costly and time-consuming for large population studies.
In summary, we discovered similar patterns of rBMD changes in both sexes, with greater differences across age in the density of the central and superior regions compared to the outer and mid-transverse regions, respectively. After adjusting for age, a decrease in the central/outer ratio and increases in anterior/posterior and superior/mid-transverse rBMD ratios were associated with increased risk of disc height loss. Further studies might explore whether there is a causal link between IVD degeneration and the BMD distribution in the hopes of leading to interventions to slow these deleterious changes and reduce the incidents of musculoskeletal disorders in the spine.
References
Riggs BL, Wahner HW, Dunn WL, Mazess RB, Offord KP, Melton LJ 3rd (1981) Differential changes in bone mineral density of the appendicular and axial skeleton with aging: relationship to spinal osteoporosis. J Clin Invest 67:328–335. https://doi.org/10.1172/JCI110039
Cooper C, Atkinson EJ, O’Fallon MW, Melton JL (2009) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 7:221–227. https://doi.org/10.1002/jbmr.5650070214
Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg 72:403–408
Waxman R, Tennant A, Helliwell P (2000) A prospective follow-up study of low back pain in the community. Spine (Phila Pa 1976) 25:2085–2090
Thomsen JS, Ebbesen EN, Mosekilde LI (2002) Static histomorphometry of human iliac crest and vertebral trabecular bone: a comparative study. Bone 30:267–274
Ebbesen EN, Thomsen JS, Beck-Nielsen H, Nepper-Rasmussen HJ, Mosekilde L (1999) Age- and gender-related differences in vertebral bone mass, density, and strength. J Bone Miner Res 14:1394–1403. https://doi.org/10.1359/jbmr.1999.14.8.1394
Riggs BL, Melton LJ, Robb RA et al (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954. https://doi.org/10.1359/jbmr.040916
Chen H, Shoumura S, Emura S, Bunai Y (2008) Regional variations of vertebral trabecular bone microstructure with age and gender. Osteoporos Int 19:1473–1483. https://doi.org/10.1007/s00198-008-0593-3
Christiansen BA, Kopperdahl DL, Kiel DP, Keaveny TM, Bouxsein ML (2011) Mechanical contributions of the cortical and trabecular compartments contribute to differences in age-related changes in vertebral body strength in men and women assessed by QCT-based finite element analysis. J Bone Miner Res 26:974–983. https://doi.org/10.1002/jbmr.287
Samelson EJ, Christiansen BA, Demissie S, Broe KE, Louie-Gao Q, Cupples LA, Roberts BJ, Manoharam R, D'Agostino J, Lang T, Kiel DP, Bouxsein ML (2012) QCT measures of bone strength at the thoracic and lumbar spine: the Framingham study. J Bone Miner Res 27:654–663. https://doi.org/10.1002/jbmr.1482
Wang Y, Owoc JS, Boyd SK, Videman T, Battié MC (2013) Regional variations in trabecular architecture of the lumbar vertebra: associations with age, disc degeneration and disc space narrowing. Bone 56:249–254. https://doi.org/10.1016/j.bone.2013.06.022
Grote HJ, Amling M, Vogel M, Hahn M, Pösl M, Delling G (1995) Intervertebral variation in trabecular microarchitecture throughout the normal spine in relation to age. Bone 16:301–308. https://doi.org/10.1016/8756-3282(94)00042-5
Davies KM, Stegman MR, Heaney RP, Recker RR (1996) Prevalence and severity of vertebral fracture: the Saunders county bone quality study. Osteoporos Int 6:160–165. https://doi.org/10.1007/BF01623941
Boos N, Weissbach S, Rohrbach H, Weiler C, Spratt KF, Nerlich AG (2002) Classification of age-related changes in lumbar intervertebral discs: 2002 Volvo award in basic science. Spine (Phila Pa 1976) 27:2631–2644. https://doi.org/10.1097/01.BRS.0000035304.27153.5B
Osti O, Vernon-Roberts B, Moore R, Fraser R (1992) Annular tears and disc degeneration in the lumbar spine. A post-mortem study of 135 discs. Bone Joint J 74–B:678–682
Cody DD, Goldstein SA, Flynn MJ, Brown EB (1991) Correlations between vertebral regional bone mineral density (rBMD) and whole bone fracture load. Spine (Phila Pa 1976) 16:146–154
Hussein AI, Jackman TM, Morgan SR, Barest GD, Morgan EF (2013) The intravertebral distribution of bone density: correspondence to intervertebral disc health and implications for vertebral strength. Osteoporos Int 24:3021–3030. https://doi.org/10.1007/s00198-013-2417-3
Livshits G, Ermakov S, Popham M, MacGregor AJ, Sambrook PN, Spector TD, Williams FMK (2010) Evidence that bone mineral density plays a role in degenerative disc disease: the UK Twin Spine study. Ann Rheum Dis 69:2102–2106. https://doi.org/10.1136/ard.2010.131441
Simpson EK, Parkinson IH, Manthey B, Fazzalari NL (2001) Intervertebral disc disorganization is related to trabecular bone architecture in the lumbar spine. J Bone Miner Res 16:681–687. https://doi.org/10.1359/jbmr.2001.16.4.681
Prescher A (1998) Anatomy and pathology of the aging spine. Eur J Radiol 27:181–195. https://doi.org/10.1016/S0720-048X(97)00165-4
Lane NE, Nevitt MC, Genant HK, Hochberg MC (1993) Reliability of new indices of radiographic osteoarthritis of the hand and hip and lumbar disc degeneration. J Rheumatol 20:1911–1918
Pollintine P, Dolan P, Tobias JH, Adams MA (2004) Intervertebral disc degeneration can lead to “stress-shielding” of the anterior vertebral body: a cause of osteoporotic vertebral fracture? Spine (Phila Pa 1976) 29:774–782
Adams MA, McNally DS, Dolan P (1996) “Stress” distributions inside intervertebral discs. Bone Joint J 78–B:965–972
Splansky GL, Corey D, Yang Q, Atwood LD, Cupples LA, Benjamin EJ, D'Agostino RB, Fox CS, Larson MG, Murabito JM, O'Donnell CJ, Vasan RS, Wolf PA, Levy D (2007) The third generation cohort of the National Heart, Lung, and Blood Institute’s Framingham Heart Study: design, recruitment, and initial examination. Am J Epidemiol 165:1328–1335. https://doi.org/10.1093/aje/kwm021
Yau MS, Demissie S, Zhou Y, Anderson DE, Lorbergs AL, Kiel DP, Allaire BT, Yang L, Cupples LA, Travison TG, Bouxsein ML, Karasik D, Samelson EJ (2016) Heritability of thoracic spine curvature and genetic correlations with other spine traits: the Framingham study. J Bone Miner Res 31:2077–2084. https://doi.org/10.1002/jbmr.2925
Hoffmann U, Massaro JM, Fox CS, Manders E, O’Donnell CJ (2008) Defining normal distributions of coronary artery calcium in women and men (from the Framingham Heart study). Am J Cardiol 102:1136–1141.e1. https://doi.org/10.1016/j.amjcard.2008.06.038
Canny J (1986) A computational approach to edge detection. IEEE Trans Pattern Anal Mach Intell PAMI-8:679–698. https://doi.org/10.1109/TPAMI.1986.4767851
Videman T, Battié MC, Ripatti S, Gill K, Manninen H, Kaprio J (2006) Determinants of the progression in lumbar degeneration. Spine (Phila Pa 1976) 31:671–678. https://doi.org/10.1097/01.brs.0000202558.86309.ea
Suri P, Hunter DJ, Rainville J, Guermazi A, Katz JN (2012) Quantitative assessment of abdominal aortic calcification and associations with lumbar intervertebral disc height loss: the Framingham study. Spine J 12:315–323. https://doi.org/10.1016/j.spinee.2012.03.033
Cheng XG, Nicholson PHF, Boonen S, Lowet G, Brys P, Aerssens J, van der Perre G, Dequeker J (1997) Prediction of vertebral strength in vitro by spinal bone densitometry and calcaneal ultrasound. J Bone Miner Res 12:1721–1728. https://doi.org/10.1359/jbmr.1997.12.10.1721
Gong H, Zhang M, Yeung HY, Qin L (2005) Regional variations in microstructural properties of vertebral trabeculae with aging. J Bone Miner Metab 23:174–180. https://doi.org/10.1007/s00774-004-0557-4
Samelson EJ, Hannan MT, Zhang Y, Genant HK, Felson DT, Kiel DP (2006) Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham study. J Bone Miner Res 21:1207–1214. https://doi.org/10.1359/jbmr.060513
Bjarnason K, Hassager C, Svendsen OL, Stang H, Christiansen C (1996) Anteroposterior and lateral spinal DXA for the assessment of vertebral body strength: comparison with hip and forearm measurement. Osteoporos Int 6:37–42. https://doi.org/10.1007/BF01626536
Kanis J, Johnell O, Oden A et al (2002) Ten-year risk of osteoporotic fracture and the effect of risk factors on screening strategies. Bone 30:251–258. https://doi.org/10.1016/S8756-3282(01)00653-6
Bouxsein ML, Seeman E (2009) Quantifying the material and structural determinants of bone strength. Best Pract Res Clin Rheumatol 23:741–753. https://doi.org/10.1016/j.berh.2009.09.008
Keller T, Moeljanto E, Main J, Spengler D (1992) Distribution and orientation of bone in the human lumbar vertebral centrum. J Spinal Disord 5:60–74
Thomsen J, Ebbesen E, Mosekilde L (2002) Zone-dependent changes in human vertebral trabecular bone: clinical implications. Bone 30:664–669. https://doi.org/10.1016/S8756-3282(02)00686-5
Keller TS, Hansson TH, Abram AC et al (1989) Regional variations in the compressive properties of lumbar vertebral trabeculae: effects of disc degeneration. Spine (Phila Pa 1976) 14:1012–1019
Homminga J, Aquarius R, Bulsink VE, Jansen CTJ, Verdonschot N (2012) Can vertebral density changes be explained by intervertebral disc degeneration? Med Eng Phys 34:453–458. https://doi.org/10.1016/j.medengphy.2011.08.003
Whitaker M, Guo J, Kehoe T, Benson G (2012) Bisphosphonates for osteoporosis — where do we go from here? N Engl J Med 366:2048–2051. https://doi.org/10.1056/NEJMp1202619
Tenne M, McGuigan F, Besjakov J, Gerdhem P, Åkesson K (2013) Degenerative changes at the lumbar spine—implications for bone mineral density measurement in elderly women. Osteoporos Int 24:1419–1428. https://doi.org/10.1007/s00198-012-2048-0
Pfirrmann CA, Metzdorf A, Zanetti M et al (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 26:1873–1878. https://doi.org/10.1097/00007632-200109010-00011
Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166:193–199. https://doi.org/10.1148/radiology.166.1.3336678
Funding
This study received funding from the National Institute of Health (R01AR054620, R01AR053986, and R01AG041658) and support from the Framingham Heart Study (NIH/NHLBI Contract HHSN268201500001I).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ali Guermazi is the President of Boston Imaging Core Lab, LLC. He is a Consultant to MerckSerono, GE, TissueGene, OrthoTrophix, AstraZeneca, Pfizer, and Sanofi.
Ethics statement
All participants signed written informed consent before enrollment and examination. Our study was approved by the Institutional Review Board at Boston University Medical Center.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Kaiser, J., Allaire, B., Fein, P.M. et al. Correspondence between bone mineral density and intervertebral disc degeneration across age and sex. Arch Osteoporos 13, 123 (2018). https://doi.org/10.1007/s11657-018-0538-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0538-1