Abstract
Summary
The vertebral trabecular bone has a complex three-dimensional (3D) microstructure, with inhomogeneous morphology. A thorough understanding of regional variations in the microstructural properties is crucial for evaluating age- and gender-related bone loss of the vertebra, and may help us to gain more insight into the mechanism of the occurrence of vertebral osteoporosis and the related fracture risks.
Introduction
The aim of this study was to identify regional differences in 3D microstructure of vertebral trabecular bone with age and gender, using micro-computed tomography (micro-CT) and scanning electron microscopy (SEM).
Methods
We used 56 fourth lumbar vertebral bodies from 28 women and men (57–98 years of age) cadaver donors. The subjects were chosen to give an even age and gender distribution. Both women and men were divided into three age groups, 62-, 77- and 92-year-old groups. Five cubic specimens were prepared from anterosuperior, anteroinferior, central, posterosuperior and posteroinferior regions at sagittal section. Bone specimens were examined by using micro-CT and SEM.
Results
Reduced bone volume (BV/TV), trabecular number (Tb.N) and connectivity density (Conn.D), and increased structure model index (SMI) were found between ages 62 and 77 years, and between ages 77 and 92 years. As compared with women, men had higher Tb.N in the 77-year-old group and higher Conn.D in the 62- and 77-year-old groups. The central and anterosuperior regions had lower BV/TV and Conn.D than their corresponding posteroinferior region. Increased resorbing surfaces, perforated or disconnected trabeculae and microcallus formations were found with age.
Conclusion
Vertebral trabeculae are microstructurally heterogeneous. Decreases in BV/TV and Conn.D with age are similar in women and men. Significant differences between women and men are observed at some microstructural parameters. Age-related vertebral trabecular bone loss may be caused by increased activity of resorption. These findings illustrate potential mechanisms underlying vertebral fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis and its associated bone fractures have become an increasingly important public health problem due to rapidly aging population [1]. It is important to identify the possible pathological mechanisms underlying bone fragility in old age. To this end, it is of interest to consider the age and gender differences in bone fracture rates in terms of sexual dimorphism in age-related skeletal changes. Human vertebral trabecular bone is one of the primary sites for age-related bone loss. Osteoporotic vertebral fractures are a serious health problem that can lead to disabling pain, kyphotic deformity and decreased quality of life [2]. The etiology of vertebral fractures remains obscure, despite the fact that they are the most common osteoporotic fracture. Moreover, they are associated with significant morbility and increased mortality.
Measurement of bone mineral density (BMD) has traditionally been used as a method for diagnosis of vertebral osteoporosis. However, this method does not fully account for the influence of changes in trabecular bone quality, such as three-dimensional (3D) microstructure, microdamage accumulation and mineralization, on the strength of the vertebra [3–6]. With the improvement in spatial resolution of 3D imaging systems, such as micro-computed tomography (micro-CT), it has become possible for unbiased 3D quantities of microstructural parameters, such as model-independent assessment of mean trabecular thickness (Tb.Th), trabecular number (Tb.N), trabecular separation (Tb.Sp), structure model index (SMI), connectivity density (Conn.D), degree of anisotropy (DA). All these parameters are related to changes with age and diseases [7–9]. With this newly developed technique, studies have been conducted to measure the changes of 3D microstructural parameters with age [7, 8]. For lumbar vertebral trabeculae, a thorough understanding of the regional variations in the microstructural properties is crucial for diagnosis and treatment of age-related degeneration, and may help us to gain more insight into the mechanism of the occurrence of vertebral osteoporosis and the related fracture risks [10, 11].
Regional vertebral microstructure has been examined using histological method [10–12] or micro-CT measurement [13–15]. It was reported that the anterior third of the vertebral body had a 20% lower bone volume (BV/TV), 16% fewer Tb.N and 28% greater Tb.Sp compared with the posterior third using histomorphometric method [11]. It was well accepted that there were pronounced age-related changes in human vertebral trabecular bone density and microstructure. The magnitude of these changes seemed to be dependent on regional location in the vertebral body. By using static histomorphometric method, Thomsen et al. [12] showed that BV/TV, Tb.N and Conn.D decreased significantly faster with age in the zone adjacent to the endplates than in the central zone. Both Tb.Th and Tb.Sp were higher in the central zone than in the sub-endplate zone. Recently, Gong et al. [13] analyzed vertebral trabecular microstructure of six cadavers using micro-CT measurement. They found that BV/TV and Tb.N decreased, while the anisotropic parameters increased significantly with age. Hulme et al. [15] analyzed the regional variations of vertebral bodies from 22 osteoporotic cadavers aged 63–80 years. They found that the posterior region of the vertebral body had greater BV/TV, more connections, reduced Tb.Sp and more plate-like isotropic structures than the corresponding anterior region. Significant heterogeneity also existed between superior and inferior regions. There are conflicting views about the gender-related differences of lumbar vertebral trabeculae. Some studies suggested that there were no gender-related differences of the vertebral trabecular bone morphometrically [5, 16]. Others showed that women had lower trabecular density [17, 18].
Micro-CT provides a tool for obtaining both 2D histomorphometric data and measurement of 3D connectivity. However, the detailed morphology of trabecular bone surfaces can not be identified by this method. Scanning electron microscopy (SEM) has proven effective in investigating the activity states of the bone surfaces [19, 20]. Our objective in this study was to confirm and extend these previous observations by estimating 3D microstructure, using micro-CT and SEM, from 56 cadaver donors to identify regional variations of vertebral trabecular bone with age and gender.
Materials and methods
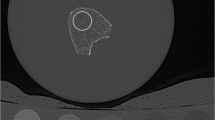
Fifty six fourth lumbar (L4) vertebral bodies were obtained during dissection in a gross anatomy course. We used 28 women (age range 57–98 years; mean age 77.4 ± 13.0 years) and 28 men (age range 57–98 years; mean age 77.6 ± 12.8 years). The subjects were chosen to give an even age and gender distribution. Both women and men were divided into three groups: 62-year (age range 57–68 years; N = 9), 77-year (age range 72–82 years; N = 9), and 92-year-old groups (age range 87–98 years; N = 10). Causes of death included cardiac failure, cerebral hemorrhage, pneumonia, multisystem organ failure and liver failure. Effects of these conditions on bone are various and were not controlled. The vertebral bodies were cleaned of soft connective tissue with a scalpel. They were checked with conventional histology, to rule out other bone diseases than osteopenia or osteoporosis. An 8-mm-thick sagittal section was cut close to the midline of the vertebral body using a water-cooled low-speed diamond saw (Buehler Isomet, Illinois, USA). Each section was divided into nine sectors (Fig. 1). Five cubes of 8 × 8 × 8 mm3 were prepared from anterosuperior (AS), anteroinferior (AI), central (C), posterosuperior (PS), posteroinferior (PI) sectors. The cortical shell and the endplate were not included in each bone specimen.
The trabecular bone microstructure was analyzed by using cone-beam X-ray micro-CT system (MCT-CB100MF, Hitachi Medical Corporation, Kashiwa, Japan) as described by Washimi et al. [21]. The bone specimens were scanned continuously with increments of 15 μm thickness for 512 slices with a tube voltage of 50 kV, tube current of 0.1 mA. The voxel size was 15 × 15 × 15 μm3.
After scanning, the micro-CT image data were transferred to a workstation and the microstructural parameters were calculated using 3D trabecular bone analysis software TRI/3D-BON (Ratoc System Engineering Co. Ltd., Tokyo, Japan). TRI/3D-BON builds 3D models from serial tomographic datasets for visualization and morphometric analysis as described by Joo et al. [22]. Briefly, the 3D images were segmented into voxels identified as bone and marrow. A histogram of the image gray scale values of a typical vertebral body is shown in Fig. 2a. A median filter was used to remove noise and a single threshold value was used to segment the images for all specimens. A sagittal section viewed from the lateral aspect of a typical vertebral body before segmenting is shown in Fig. 2b. The same section after segmentation is shown in Fig. 2c. The resulting image is the gray scale representation of the mineralized tissue. Subsequently, the isolated small particles in marrow space and the isolated small holes in bone were removed using a cluster-labeling algorithm [23]. The trabecular bone was then analyzed for microstructural indices. Bone volume (BV) was calculated using tetrahedrons corresponding to the enclosed volume of the triangulated surface [24]. Trabecular BV/TV was calculated with bone volume (BV) and total tissue volume (TV). Tb.Th, Tb.Sp and Tb.N were based on direct measures by a distance transformation method [25]. SMI is a parameter that quantified the characteristic form of a 3D described structure in terms of the number of plates and rods that compose the structure [25]. Conn.D is a topological parameter that estimates the number of trabecular connections per cubic millimeter [26]. DA defines the direction and magnitude of the preferred orientation of trabeculae and uses the ratio between the maximum and minimum radii of the mean intercept length ellipsoid [27]. All the above parameters were computed in 3D without model assumptions required for 2D-based analysis [28].
After micro-CT scanning, the trabecular bone specimens were cleaned with a fine jet of water to remove bone marrow. They were then treated with 5% sodium hypochlorite solution to remove residual marrow. The specimens were dehydrated in acetone and critical-point dried, mounted on stubs and coated with gold/palladium using an ion sputter. The vertebral trabeculae were examined with a scanning electron microscope (Hitachi S-3500 N SEM).
The trabecular resorbing surfaces, showing depressions or pits with bright scalloped edges, indicative of osteoclastic resorptions, have been described extensively [19, 20, 29]. In the present study, the percentage area occupied by the resorbing surface was estimated, by using an image measuring system (Finetec, Tokyo, Japan) as reported previously [29]. Measurements were carried out from all trabecular bone specimens examined at a magnification of 100 under the SEM.
All data are presented as mean ± SD. Statistical analysis was done using SPSS version 14 (Chicago, IL, USA). One-way analysis of variance (ANOVA) was used to compare the trabecular microstructural parameters overall in the three different age groups. Statistical analysis of differences between women and men of the same age group was made by Student’s t-test. Correlation between BV/TV, Conn.D and age for both women and men was studied by linear regression analysis. Regional variations of the microstructural parameters were examined using repeated-measures analysis of variance (ANOVA). Fisher’s protected least squares differences test was used for post hoc multiple comparisons. The same statistical analysis was performed for the percentage area of the trabecular bone resorbing surface. Differences were considered significant at p < 0.05.
Results
Table 1 shows the mean values of microstructural parameters in three age groups of women and men. As is evident, among three age groups, the 62-year-old group had the highest values of BV/TV and Tb.N for both women and men. BV/TV decreased by 11% and 12% (p < 0.05) between ages 62 and 77 years, between ages 77 and 92 years for women. The change pattern of Tb.N was quite similar with that of BV/TV. Consistently, Tb.Sp increased by about 9% (p < 0.05) between ages 62 and 77 years, between ages 77 and 92 years for women. The vertebral body displayed rod-like trabecular bone structure in the 92-year-old group. SMI increased by 10% and 7% between ages 62 and 77 years, between ages 77 and 92 years for women. Conn.D was the highest in the 62-year-old group, and it decreased by 20% and 22% between ages 62 and 77 years, between ages 77 and 92 years for women. The above microstructural parameters changed very similarly in women and men among three age groups. As compared with women, BV/TV, Tb.N and Conn.D had a tendency to be higher, while Tb.Sp and SMI had a tendency to be lower in men. Tb.N and Conn.D in the 77-year-old group were significantly higher (p < 0.05) in men than those of women (Table 1). We did not find any significant differences for Tb.Th and DA between women and men among three age groups. The lineal regression analysis showed that BV/TV and Conn.D decreased significantly with age for both women and men (Fig. 3a,b).
Table 2 shows the mean values of microstructural parameters in five different regions of vertebral body. The posteroinferior region had the highest BV/TV, Tb.N and Conn.D, and the lowest Tb.Sp. As compared with posteroinferior region, BV/TV, Tb.N and Conn.D were significantly low, while Tb.Sp was significantly high in the central and anterosuperior regions (p < 0.05). We did not find any significant differences among five regions with regard to Tb.Th, SMI and DA (Table 2).
Table 3 lists the mean values of microstructural parameters and their relative differences in women and men of three age groups. BV/TV in the anterior and posterior regions was decreased with age for both women and men. No significant difference was found for BV/TV in the central region among three age groups of both women and men. Tb.N had the tendency to decrease with age for all five regions. Tb.N in the 92-year-old group for both women and men was significantly low (p < 0.05). Tb.Sp and SMI increased with age. Conn.D was significantly decreased with age in all five regions. the In 77- and 92-year-old groups, Conn.D in the anterior, central and posterosuperior regions of men was significantly greater than that of women. Age-related change for Conn.D was the greatest among all microstructural parameters. Conn.D in all five regions was significantly decreased by about 20% between ages 66 and 77 years, and between ages 77 and 92 years (Table 3).
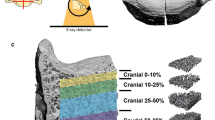
Figure 4 shows the typical 3D reconstructions of women vertebral trabecular bones at age 77 years. Images of the sample with BV/TV that were closest to the mean BV/TV were reconstructed in each group. The trabecular bone volume was higher in the posterosuperior and posteroinferior regions. There was a significant decline of trabeculae in the central and anterosuperior regions (Fig. 4).
Three-dimensional micro-CT image reconstructions in different regions of the vertebral body from a woman aged 78 years: anterosuperior (a), anteroinferior (b), central (c), posterosuperior (d), and posteroinferior (e) regions. The trabecular bone is higher in the posterosuperior and posteroinferior regions than that of the central and anterosuperior regions
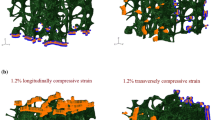
The SEM images showed that the vertical trabeculae were relatively thicker, while the horizontal ones were thinner (Fig. 5a). The characteristics of the resorbing surfaces (R) showed considerable variability at different ages both for women and men. These variations were related to the trabecular structural changes, such as thinning, perforation and disruption of the trabeculae, that occur with age. The size and shape of the resorbing surfaces varied from long, shallow, elongated furrows (Fig. 5b) to rounded deep lacunae (Fig. 5c). The amount of bone removed by the resorption varied from superficial skimming of surfaces to complete perforation or disconnection of the trabeculae (Fig. 5b,d). In some regions, the trabecular microcallus formation (MC) was observed, especially on the vertical trabeculae (Fig. 5d).
SEM photographs of the vertebral trabeculae from 89- (a, b), 90-(c), and 92-(d) year-old women. The vertical trabeculae are relatively thicker than the horizontal ones (a). The elongated shallow resorption furrows (b), rounded deep resorption lacunae (c) and the trabecular microcallus (d) are observed. R: resorbing surfaces; MC: microcallus
The percentage area of bone resorbing surface is shown in Table 4. Women had a tendency to have higher bone resorbing surfaces, but no significant differences were found between women and men. The percentage area of bone resorbing surface had a tendency to increase with age for both women and men. As compared with 62- and 77-year-old groups, the percentage area of bone resorbing surface was significantly high in the 92-year-old group for both women and men (Table 4). We did not find any significant differences for percentage area of bone resorbing surface among five regions of the vertebral body.
Discussion
In this study, we explored the age- and gender-specific regional differences of the trabecular bone microstructure in lumbar vertebral body. It is well accepted that age-related bone loss is an important factor leading to enhanced bone fragility and fracture risk in the elderly. Age-related changes of the trabecular bone included a decrease in BV/TV, Tb.N and Conn.D, an increase in Tb.Sp, a shift from plate-like trabeculae to rod-like structure [5, 13, 21, 30–36]. The results from our study are in line with these findings. According to our data, a 92-year-old person showed a decrease in BV/TV of about 20% in vertebral trabeculae as compared with a 62-year-old one. Similar to BV/TV, Tb.N and Conn.D also decreased in a line fashion. Consistently, Tb.Sp and SMI increased with age. We found no significantly age-related changes in Tb.Th and DA. The reduction of BV/TV with age is associated primarily with reduction in Tb.N and increases in Tb.Sp [5, 13, 30–36], which is in line with our findings. In the present study, we found that BV/TV decreased by 22% and 24%, Tb.N decreased by 16% and 19%, Tb.Sp increased by 18% and 19% from ages 62 to 92 years for women and men respectively (Table 1). There is considerable controversy with the age-related changes of Tb.Th. Some studies reported that there was a greater relative loss and thinning with age for all trabeculae [37–39], or horizontal trabeculae only [31, 32]. With the loss of horizontal trabeculae, the remaining vertical trabeculae tended to maintain their thickness and might even increase in thickness with age [5, 31]. Other studies indicated that there were no significant changes of Tb.Th with age [13, 40]. Our study showed that Tb.Th decreased by 10% from ages 62 to 92 years for both women and men, though there were no statistical significances with age. The reduced BV/TV due to decreases in Tb.N and increases in Tb.Sp, with or without thinning of Tb.Th, has formed the basis of the plausible hypothesis for age-related trabecular bone loss [40, 41].
The etiology of age-related bone loss remains unclear. This may occur by excessive resorption activity, with deeper cavities being formed by the osteoclasts, and/or insufficient formation of replacement bone tissue by the osteoblasts [30, 40, 42]. Our results showed that the percentage area of bone resorbing surface was significantly increased with age. Some trabeculae were completely perforated or disconnected. In some regions, trabecular microcallus formations were observed. These findings are consistent with the hypothesis that the bone resorption increases with age, and this accelerates the risk of fracture due to bone loss in the vertebrae [30]. Vertebral trabecular bone is lost principally through perforation of trabeculae rather than general thinning of trabeculae [31, 42, 43]. The loss of complete trabeculae results in a significantly greater deterioration in mechanical properties than an equivalent bone reduction where trabeculae are thinned but not lost altogether [8].
Vertebral trabecular bone has a complex 3D structure that consists of interconnecting plates and rods. An estimation of plate or rod characteristic of trabeculae can be determined by measuring SMI. This is important structural feature which impacts strongly on the mechanical properties of the trabeculae. Human vertebral trabecular bone has a more rod-like than plate-like structure and hence is likely to be more susceptible to bending and buckling failure than, for example, femoral head, which has a more plate-like structure [5]. There were few studies concerning age-related change for vertebral trabecular SMI. Stauber and Müller [5] stated that there was a slight increase of SMI with age in human vertebra. Ding et al. [8] analyzed age-related changes in proximal tibial trabeculae from 40 normal donors aged 16 to 85 years. It was found that SMI was the highest in the old age group as compared with young or middle age group. It seemed that human tibial trabecular bone structure changed with age from plate-like to somewhat more rod-like so as to form a combined plate-like and rod-like trabecular structure. Gong et al. [14] investigated microstructure of vertebral trabeculae from 6 donors. They suggested that vertebral bodies with the same age might belong to high-SMI or low-SMI group. The vertebrae with lower bone mass and poorer connectivity were liable to constitute high-SMI group, which was more susceptible to vertebral body wedge fracture. In the present study, we found that SMI increased from age 62 to 92 years by 18% and 20% respectively for women and men. A more rod-like structure of the trabecular bone is observed in the vertebral trabeculae with age and hence is likely to be more susceptible to bending and buckling failure modes.
Trabecular connectivity is a fundamental property of 3D networks, which has traditionally been measured by various surrogate 2D methods. Unbiased and model-free quantification of connectivity from 3D images is enabled by a topological approach [26]. Conn.D is important in the maintenance of bone strength. As bone volume decreases there is a corresponding decrease in Conn.D, possibly due to the loss of small interconnecting trabeculae with small initial diameter [15, 34]. Our data showed that Conn.D decreased by 37% from age 66 to 92 years (Table 1). The change in Conn.D with age in the vertebral body was almost identical for women and men. Similar result was reported previously using histomorphometric method [35]. How the trabecular connectivity changes under pathological condition remains to be obscure.
Several studies have reported no differences in vertebral BMD between women and men [36, 44]. Sigurdsson et al. [17], however, recently reported significantly lower trabecular density of lumbar spine and proximal femur in women between 67–69 years of age with QCT. A study by Bouxsein et al. [18] also using QCT, reported that both women and men exhibited a marked decline in trabecular compressive strength with age, the decline was greater in women than men. Recently, in a population-based cross-sectional study, effects of gender and age on bone microstructure of distal radius using high-resolution 3D pQCT were explored [45]. Decreases in trabecular BV/TV with age are similar in women and men. Compared with women, men had thicker trabeculae and had less microstructural damage with age [45]. Eckstein et al. [46] characterized bone microstructure, specifically gender differences, at multiple skeletal sites in 165 subjects aged 52 years and older using micro-CT technology. Significant gender differences were observed at the distal radius, femoral neck and femoral trochanter, but not at the iliac crest, calcaneus and lumbar vertebral body. Previously, no gender-related differences were found in vertebral trabeculae histomorphometrically [16]. Stauber and Müller [5] analyzed age-related changes in trabecular bone microstructures by global and local morphometry analysis. Age-related changes showed no gender but site differences.
Our study demonstrated that there were no significant gender differences for BV/TV. Men had higher BV/TV than women by 6% in the 62-year-old group and 3% only in the 92-year-old group (Table 1). The gender differences for BV/TV became smaller with aging. Clinical observation showed that women:men ratio of vertebral fracture in subjects ≥35 years of age was 2.4:1, while the ratio in subjects ≥85 years of age decreased to 1:0.92 [47]. In human lumbar vertebrae, trabeculae became thinner and finally vanished with aging, while the remaining trabeculae tended to maintain their thickness and might even increase in thickness. Due to loss of interconnecting trabeculae, the remaining trabeculae are more likely to buckle [5, 31]. However, there is no detailed information concerning the age-related change of the vertebral trabecular connectivity. Men displayed higher Conn.D than women (Table 1, 3). Why the gender-related difference occurs in the vertebral trabeculae, as well as the possible biomechanical or hormonal factors driving these changes is unknown at this point.
Vertebral trabeculae are not morphologically homogeneous. Banse et al. [48], using pQCT measurement, reported that BV/TV in the posterior region of lumbar vertebral body was 20% higher than that in the anterior one. Hulme et al. [15] found that the inferoposterior region had the highest BV/TV in vertebral body. Similar findings were observed in the present study. Our results showed that the central and anterosuperior regions of the vertebral body had the lowest BV/TV, Tb.N, Conn.D, and the highest Tb.Sp. The posteroinferior region had the highest BV/TV, Tb.N, Conn.D, and the lowest Tb.Sp for both women and men. BV/TV, Tb.N and Conn.D significantly decreased between ages 62 and 77 years, and between ages 77 and 92 years. SMI significantly increased between ages 62 and 77 years, and between ages 77 and 92 years. As compared with women, men had significantly higher Tb.N in the 77-year-old group, and higher Conn.D in the 62- and 77-year-old groups.
It was accepted that regional differences of vertebral body were dependent on age, with generally large differences in young, adult individuals and smaller or no differences in old individuals [12], which is in line with our findings. As compared with posteroinferior region, BV/TV in the central region was lower by 23% and 29%, respectively, for both women and men in the 62-year-old group, and this difference decreased to about 12% in the 92-year-old group (Table 3). The regional re-enforcement of trabecular bone is reflected in observed vertebral fracture location. Low energy compression fractures can occur in the anterior or posterosuperior regions of the vertebra, but rarely in the inferoposterior region [48, 49]. The posteroinferior endplate was found to be significantly stronger than the superior one [50]. One rationale for the regional inhomogeneity of BV/TV, higher in the posteroinferior region, is that the cortical shell of the posterosuperior region is reinforced by the posterior elements, relying less on the trabeculae for strength. However, the posteroinferior region of the cortical shell does not have reinforcement, lacking any posterior elements, and thus must rely on the trabecular core for strength [48]. The highest BV/TV in the posteroinferior region of vertebral body, and to a lesser extent a thickening of the posterior endplate, likely strengthens the inferior endplate resulting in a preferential failure of the superior endplate. The relationship between vertebral strength and structure is complex, involving contributions from the endplate, cortical shell, trabeculae and intervertebral disc health [10].
By using SEM, the trabecular resorption states are clearly visualized, which are important for bone architectural integrity, probably determining whether the bone quality is maintained or reduced [19, 20]. Vertebral trabecular bone is lost principally through perforation of trabeculae rather than general thinning of trabeculae [31]. It was possible to show that some perforated trabeculae were removed by osteoclasts. The trabecular connections were lost and continuity destroyed. If new bone formation does not adequately restore the lost tissue, the narrowed trabeculae will become tapered, free-ended, and unlikely ever to regain continuity [19, 20]. Trabecular microcallus formation was described previously in human vertebra [19, 20, 51]. Whether microcallus formations should be regarded as an indicator of poor architectural adaptation to prevailing strain or whether they are a sign of physiological repair mechanism is difficult to determine [19, 20, 51]. The interpretation of trabecular bone resorption by SEM is limited, because we have no accurate information of the resorption rates and the population dynamics of the osteoclasts that shaped the surface. We may blithely assume that large cells make larger holes in the bone, but standard histomorphometric studies give a poor interpretation of 3D isotropic resorption and the relationship of characterized osteoclasts to it.
The presented methodology differs from previous investigations in that the trabeculae were observed with micro-CT and SEM. Both methods allow direct assessment of the structure stereoscopically. To obtain microstructural parameters using micro-CT and SEM, the specimens are often not so large. In the present study, just five cubes of 8 × 8 × 8 mm3 of each vertebral body were used for microstructural analysis. This can only provide data for small localized bone volume, which may differ from that in other regions, and these data from such a small specimen can not be used to determine the overall bone strength or fracture risk. On the other hand, larger specimens can provide average structural and mechanical properties of a piece of bone, but may not reflect regional structural variations. In the present study, all specimens obtained from subjects aged 57 years or older and the number of specimens is limited (n = 56). Because of the limited availability of donors, we did not have the opportunity to get specimens from young individuals. With more cases from young individuals, we might offer a conclusion completely on regional variations in the microstructure of the human vertebral trabeculae with age and gender.
In conclusion, our study demonstrates that BV/TV, Tb.N and Conn.D decreased, while SMI increased significantly between ages 62 and 77 years, and between ages 77 and 92 years. As compared with women, men had higher Tb.N in the 77-year-old group, and higher Conn.D in the 62- and 77-year-old groups. The vertebral trabecular bone is microstructurally heterogeneous. These findings may be used to focus clinical CT analysis to specific trabecular regions to further improve fracture prediction for specific fracture modalities.
References
Ettinger MP (2003) Aging bone and osteoporosis: strategies for preventing fractures in the elderly. Arch Intern Med 163:2237–2246
Fechtenbaum J, Cropet C, Kolta S et al (2005) The severity of vertebral fractures and health-related quality of life in osteoporotic postmenopausal women. Osteoporos Int 16:2175–2179
Hui SL, Slemenda CW, Johnston CC Jr (1988) Age and bone mass as predictors of fracture in a prospective study. J Clin Invest 81:1804–1809
Burr DB, Forwood MR, Fyhrie DP et al (1997) Bone microdamage and skeletal fragility in osteoporotic and stress fractures. J Bone Miner Res 12:6–15
Stauber M, Müller R (2006) Age-related changes in trabecular bone microstructures: global and local morphometry. Osteoporos Int 17:616–626
Legrand E, Chappard D, Pascaretti C et al (2000) Trabecular bone microarchitecture, bone mineral density, and vertebral fractures in male osteoporosis. J Bone Miner Res 15:13–19
Ding M (2000) Age variations in the properties of human tibial trabecular bone and cartilage. Acta Orthop Scand Suppl 292:1–45
Ding M, Odgaard A, Linde F et al (2002) Age-related variations in the microstructure of human tibial cancellous bone. J Orthop Res 20:615–621
Kinney JH, Ladd AJ (1998) The relationship between three-dimensional connectivity and the elastic properties of trabecular bone. J Bone Miner Res 13:839–845
Hordon LD, Raisi M, Aaron JE et al (2000) Trabecular architecture in women and men of similar bone mass with and without vertebral fracture: I. Two-dimensional histology. Bone 27:271–276
Adams MA, Pollintine P, Tobias JH et al (2006) Intervertebral disc degeneration can predispose to anterior vertebral fractures in the thoracolumbar spine. J Bone Miner Res 21:1409–1416
Thomsen JS, Ebbesen EN, Mosekilde L (2002) Zone-dependent changes in human vertebral trabecular bone: clinical implications. Bone 30:664–669
Gong H, Zhang M, Yeung HY et al (2005) Regional variations in microstructural properties of vertebral trabeculae with aging. J Bone Miner Metab 23:174–180
Gong H, Zhang M, Qin L et al (2006) Regional variations in microstructural properties of vertebral trabeculae with structural groups. Spine 31:24–32
Hulme PA, Boyd SK, Ferguson SJ (2007) Regional variation in vertebral bone morphology and its contribution to vertebral fracture strength. Bone 41:946–957
Thomsen JS, Ebbesen EN, Mosekilde L (2002) Predicting human vertebral bone strength by vertebral static histomorphometry. Bone 30:502–508
Sigurdsson G, Aspelund T, Chang M et al (2006) Increasing sex difference in bone strength in old age: the Age, Gene/Environment Susceptibility-Reykjavik study (AGES-REYKJAVIK). Bone 39:644–651
Bouxsein ML, Melton LJ 3rd, Riggs BL et al (2006) Age- and sex-specific differences in the factor of risk for vertebral fracture: a population-based study using QCT. J Bone Miner Res 21:1475–1482
Jayasinghe JAP, Jones SJ, Boyde A (1993) Scanning electron microscopy of human lumbar vertebral bone surfaces. Virchows Arch A Pathol Anat 422:25–34
Mosekilde L (1993) Vertebral structure and strength in vivo and in vitro. Calcif Tissue Int 53(Suppl.):S121–S126
Washimi Y, Ito M, Morishima Y et al (2007) Effect of combined humanPTH(1–34) and calcitonin treatment in ovariectomized rats. Bone 41:786–793
Joo YI, Sone T, Fukunaga M et al (2003) Effects of endurance exercise on three-dimensional trabecular bone microarchitecture in young growing rats. Bone 33:485–493
Odgaard A, Gundersen HJ (1993) Quantification of connectivity in cancellous bone, with special emphasis on 3-D reconstructions. Bone 14:173–182
Lorensen WE, Cline HE (1987) Marching cubes: a high resolution 3D surface construction algorithm. Comput Graph 21:163–169
Hildebrand T, Rüegsegger P (1997) Quantification of bone microarchitecture with the structure model index. Comput Methods Biomech Biomed Engin 1:15–23
Odgaard A (1997) Three-dimensional methods for quantification of cancellous bone architecture. Bone 20:315–328
Harrigan TP, Mann RW (1984) Characterization of microstructural anisotropy in orthotropic materials using a second rank tensor. J Mater Sci 19:761–767
Hildebrand T, Laib A, Müller R et al (1999) Direct three-dimensional morphometric analysis of human cancellous bone: microstructural data from spine, femur, iliac crest, and calcaneus. J Bone Miner Res 14:1167–1174
Chen H, Shoumura S, Emura S (2004) Ultrastructural changes in bones of the senescence-accelerated mouse (SAMP6): a murine model for senile osteoporosis. Histol Histopathol 19:677–685
Mosekilde L (1989) Sex differences in age-related loss of vertebral trabecular bone mass and structure-biomechanical consequences. Bone 10:425–432
Thomsen JS, Ebbesen EN, Mosekilde LI (2002) Age-related differences between thinning of horizontal and vertical trabeculae in human lumbar bone as assessed by a new computerized method. Bone 31:136–142
Mosekilde L (1988) Age-related changes in vertebral trabecular bone architecture–assessed by a new method. Bone 9:247–250
Parfitt AM (1984) Age-related structural changes in trabecular and cortical bone: cellular mechanisms and biomechanical consequences. Calcif Tissue Int 36(Suppl 1):S123–S128
Grote HJ, Amling M, Vogel M et al (1995) Intervertebral variation in trabecular microarchitecture throughout the normal spine in relation to age. Bone 16:301–308
Thomsen JS, Ebbesen EN, Mosekilde L (2002) Static histomorphometry of human iliac crest and vertebral trabecular bone: a comparative study. Bone 30:267–274
Eckstein F, Fischbeck M, Kuhn V et al (2004) Determinants and heterogeneity of mechanical competence throughout the thoracolumbar spine of elderly women and men. Bone 35:364–374
Bergot C, Laval-Jeantet AM, Prêteux F et al (1988) Measurement of anisotropic vertebral trabecular bone loss during aging by quantitative image analysis. Calcif Tissue Res 43:143–149
McCalden RW, McGeough JA, Court-Brown CM (1997) Age-related changes in the compressive strength of cancellous bone. The relative importance of changes in density and trabecular architecture. J Bone Joint Surg Am 79:421–427
Weinstein RS, Hutson MS (1987) Decreased trabecular width and increased trabecular spacing contribute to bone loss with aging. Bone 8:137–142
Parfitt AM, Mathaws CHE, Villaneuva AR et al (1983) Relationship between surface, volume, and thickness of iliac trabecular bone in aging and in osteoporosis. Implications for the microanatomic and cellular mechanisms of bone loss. J Clin Invest 72:1396–1409
Riggs BL, Parfitt AM (2005) Drugs used to treat osteoporosis: the critical need for a uniform nomenclature based on their action on bone remodeling. J Bone Miner Res 20:177–184
McDonnell P, McHugh PE, O’Mahoney D (2007) Vertebral osteoporosis and trabecular bone quality. Ann Biomed Eng 35:170–189
Fyhrie DP, Lang SM, Hoshaw SJ et al (1995) Human vertebral cancellous bone surface distribution. Bone 17:287–291
Ebbesen EN, Thomsen JS, Beck-Nielsen H et al (1998) Vertebral bone density evaluated by dual-energy X-ray absorptiometry and quantitative computed tomography in vitro. Bone 23:283–290
Khosla S, Riggs BL, Atkinson EJ et al (2006) Effects of sex and age on bone microstructure at the ultradistal radius: a population-based noninvasive in vivo assessment. J Bone Miner Res 21:124–131
Eckstein F, Matsuura M, Kuhn V et al (2007) Sex differences of human trabecular bone microstructure in aging are site-dependent. J Bone Miner Res 22:817–824
Melton LJ 3rd (1995) Epidemiology of fractures. In: Riggs BL, Melton LJ (eds) Osteoporosis: etiology, diagnosis and management. 2nd ed. Lippicott-Raven, Philadelphia, pp 225–249
Banse X, Devogelaer JP, Munting E et al (2001) Inhomogeneity of human vertebral cancellous bone: systematic density and structure patterns inside the vertebral body. Bone 28:563–571
Silva MJ, Keaveny TM, Hayes WC (1998) Computed tomography-based finite element analysis predicts failure loads and fracture patterns for vertebral sections. J Orthop Res 16:300–308
Grant JP, Oxland TR, Dvorak MF (2001) Mapping the structural properties of the lumbosacral vertebral endplates. Spine 26:889–896
Hahn M, Vogel M, Amling M et al (1995) Microcallus formations of the cancellous bone: a quantitative analysis of the human spine. J Bone Mine Res 10:1410–1416
Acknowledgements
The authors thank Dr. Ken-ichi Tezuka, Department of Tissue and Organ Development, Gifu University Graduate School of Medicine, for providing micro-CT system used in this study.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, H., Shoumura, S., Emura, S. et al. Regional variations of vertebral trabecular bone microstructure with age and gender. Osteoporos Int 19, 1473–1483 (2008). https://doi.org/10.1007/s00198-008-0593-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0593-3