Abstract
Purpose
Among others, the German National Prevention Conference recently recommended the provision of preventive options for elderly to maintain their independent living. Because a home safety assessment and modification program (HSM) has shown to be effective in avoiding falls and risk of falling in elderly, the aim of this analysis was to evaluate the cost-effectiveness of HSM in patients aged ≥ 80 years who receive non-institutionalized long-term care.
Methods
In order to reflect quality-adjusted life years (QALYs) and costs resulting from HSM, a Markov-model with a time horizon of 20 years was performed from the perspective of the German statutory health insurance (SHI) and statutory long-term care insurance (LCI). The model assumed that HSM reduces fall-related hip fractures in accordance with the reduction of the rate of falls. Data was obtained from public databases and from various literature searches. The robustness of the results was assessed in deterministic and probabilistic sensitivity analyses.
Results
In women, the incremental cost-effectiveness ratio of HSM compared to no prevention was €9580 per QALY, while in men, it was €57,589. For the German SHI/LCI, in total, the provision of HSM to patients ≥ 80 years who receive non-institutionalized long-term care would result in annual costs of €7.7 million. The results were robust in several sensitivity analyses.
Conclusions
Provided that the rate of falls is a valid surrogate endpoint for the rate of fall-related hip fractures, HSM could be a promising approach for investments in preventive options targeting the reduction of fall-related fractures in elderly women.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Falls are associated with an increased risk of mortality and morbidity and are the most important risk factor in an elderly person for suffering a fracture [1]. In addition, fall-related fractures, particularly osteoporotic hip fractures, result in high socioeconomic costs. In Germany, the number of osteoporosis-attributable hip fractures was 55,000 in 2010 and is expected to increase to 92,000 fractures in the year 2030 [2].
There are several preventive options for reducing the risk of fractures, targeting either at strengthening bone density by bone-stimulating drugs (i.e., bisphosphonates) or, at reducing the number of falls by non-medical interventions (e.g., visual aids, multiple-component group exercise or home safety adaptions). Because the effectiveness of these opportunities differ according to the subgroup provided [3], a specific preventive intervention should be offered to those who are assumed to benefit most.
In Germany, in 2015, the parliament passed a law to strengthen health promotion and preventive health care, named the Preventive Health Care Act. According to this law, the health insurance and long-term insurance funds will be investing over €500 million for health promotion and prevention within the next years. The main focus, thereby, will be on health promotion in life settings [4]. Based on recommendations of the German National Prevention-Conference, the Statutory Health Insurance (SHI) should offer—among others—preventive measures that allow elderly people to maintain their independent living and, to resist a required demand for long-term care. Thus, preventive measures should also be offered to elderly who are in need of long-term care but still able to stay at home [4].
The home environment has been implicated in many fall-related injuries in older persons. Home environments may be affected by potential hazards, and many older people attribute their falls to trips or slips inside the home or immediate home surroundings. In addition, the relationship between an older person’s physical abilities and the exposure to environmental stressors appears to be risk-predictive as taking risks or impulsivity may further increase the risk of falls [5].
Home hazard reduction reduced the rate of falls and the risk of falling if targeted at older people with a history of falls and mobility limitations [3]. The effectiveness may depend on the provision of concomitant training for improving transfer abilities and other strategies for effecting behavioral change [5].
Because falls carry a risk of injury, an intervention which reduces the number of times a person falls, has clinical, public health, and economic relevance. The home environment has been implicated in more than one third of all falls or injurious fall events in older persons [6]. Thus, a modification of the home environment can specifically be used for reducing the fall risk of elderly people. Several economic studies have evaluated the cost-effectiveness of fall prevention in nursing home settings, whilst only few studies addressed preventive measures for elderly in the home environment. The aim of this modeling study was to evaluate the cost-effectiveness of a home safety assessment and modification program (HSM) in German elderly people prescribed for outpatient long-term care compared to no intervention.
Methods
In order to reflect the clinical and monetary consequences of hip fractures for non-institutionalized elderly people aged ≥ 80, a Markov model with a time horizon of 20 years and a cycle length of 6 months was developed in TreeAge Pro© (TreeAge Software, Williamstown, Massachusetts). In accordance with many clinical studies which have evaluated the efficacy of HSM, the model starts at the age of 80. It stops at the age of 100 because for Germany there are no survival data beyond that age. The health benefit was estimated in terms of quality-adjusted life-years (QALYs). We performed different literature searches in the PubMed database aimed at data on efficacy, costs of care, event rates, and utilities (which should be based either on the time trade off or the standard gamble method). If more than one source was available, data reflecting the German context more appropriate was preferred. Before inclusion into the model, clinical experts were asked for the suitability of data. As the risk of hip fractures of non-institutionalized elderly people is increased in the subgroup of patients receiving outpatient care (compared to non-institutionalized elderly people without care), the analysis was targeted to this subgroup [7]. To assess the cost-effectiveness of an HSM, incremental cost-effectiveness ratios (ICERs) were calculated from the combined perspective of the statutory health insurance (SHI) and long-term care insurance (LCI).
Model design
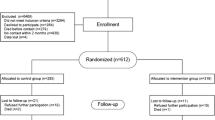
A Markov model with 6 health states was developed. In the model, a cohort of non-institutionalized men and women recently assigned to outpatient long-term care starts in the state “healthy.” Patients either remain in this state or suffer a “hip fracture.” Other fractures were not taken into account because the treatment of hip fractures is more costly and the reduction in health-related quality of life (HRQoL) due to hip fractures more severe compared to other fractures [8]. In addition, for non-hip-fractures, there is a lack of data in this subgroup. After a hip fracture, patients move to a “post-fracture” state (due to a persistent reduction in HRQoL), the “nursing home” state, or they remain in this state as a result of a re-fracture. For Germany, data on nursing home admissions due to hip fractures was available only for a period of 6 months after fracture [9]. Therefore, rates of delayed nursing home admissions more than 6 months after fracture were assumed to be equal between the intervention and control group and, a transition from the state “post-fracture” to the state “nursing home” not modeled. A transition from the state “healthy” to “nursing home” was not modeled because for this analysis only hip-fracture-related nursing home admissions are relevant. In addition, there is no evidence for a reduction of admissions as a result of HSM without suffering a fracture. Patients admitted to a nursing home were assumed to stay there with or without subsequent fractures until they die. To take into account the costs and reduced HRQoL for patients who suffered a re-fracture within their nursing home stay, an own fracture state “re-fracture in nursing home” was modeled (Fig. 1).
Intervention
For the avoidance of falls in a non-institutional environment several preventive options are available. HSM was chosen because it was found to reduce the rate of falls and risk of falling and, can be easily offered to immobile patients without incurring stressful efforts and costs of transport. HSM was assumed to include a home visit—provided by a multidisciplinary team immediately after non-institutionalized long-term care was prescribed—and 2 follow-up visits.
The multidisciplinary team initially assesses the environment of the patient with respect to potential environmental hazards and prescribes technical aids according to the patient’s need. In two further home visits, patients are informed about the possible fall risk in their home, they are given advice on possible changes of the home environment, any necessary home modifications are facilitated and, participants are instructed in the use of technical and mobility aids.
Data
Clinical input data
Incidence of hip fractures was based on a large retrospective routine data set of German elderly assigned to non-institutionalized home care [10]. Fracture rates included the ICD-code S72 (about 90% hip fractures) and were adjusted for age, sex, and fractures unrelated to falls [11]. According to a Danish registry study, in the model, the risk of a re-fracture was increased almost 12-fold in the month following the first hip fracture and gradually decreases within 20 years [12]. In addition, for re-fractures, the model reflects the increased likelihood of a re-fracture for patients in nursing homes compared to those still receiving non-institutionalized home care. Both risk increases were included by applying corresponding rate ratios.
The rates of hip fracture-related nursing home admissions (ICD-code S72) were obtained from a retrospective routine data set of community-dwelling elderly Germans who suffered a femoral fracture [9].
According to German routine data on mortality of care-dependent people, the model considered the difference in mortality in case of outpatient or inpatient long-term care [13]. It was assumed that excess mortality due to a hip fracture does not differ between patients with homecare and nursing home residents [14] (Table 1).
Based on a meta-analysis of 3 randomized controlled trials (RCTs) HSM-approaches—which were homogeneous in terms of content and personnel—have shown to be effective in reducing rate of falls [Rate ratio (RaR) = 0.62, 95% CI 0.50–0.77] of non-institutionalized elderly who were at higher risk of falling [3]. The studies included in the meta-analysis evaluated HSM-elements provided by a physiotherapist and public health worker/occupational therapist. The meta-analysis was based on 851 patients and showed no heterogeneity. Applying this RaR to the rate of hip fractures we assumed that reducing the rate of falls results in a reduction of fall-related hip fractures to the same degree. The full intervention effect was assumed to last for 6 months. Beyond this period, we assumed a linear decrease of the risk reduction over 2.5 years (5 cycles). In addition, the effect was not applied in case of a nursing home admission as the intervention referred to the non-institutionalized setting.
Health-related quality of life
In order to reflect the HRQoL of patients receiving outpatient care, we used the mean utility value of Swiss non-institutionalized individuals with moderate or severe problems in the 5 dimensions of the EQ-5D [15]. The utility values of nursing home residents refer to a German study based on the EQ-5D [16], while the decreased utility due to a hip fracture was obtained from a systematic review [17]. In order to combine utilities, reference case multipliers based on EQ-5D pooled data were used.
Costs
In accordance with the intervention profile used for the German randomized-controlled Home Intervention Team (HIT)-trial [18]—which was included in the meta-analysis—home visits were assumed to be made jointly by a physiotherapist and an occupational therapist. The costs of these home visits were based on the reimbursement agreement between the associations of health care insurers and health care providers [19]. The resource use of technical aids was also calculated in accordance with the German RCT [18]. Corresponding prices were mainly obtained from German databases. Adherence was considered in the cost calculation by taking into account the percentage of technical aids being implemented after the recommendation. The costs of a geriatric assessment were not calculated because they had already been included in the preliminary assessment for non-institutionalized long-term care. In contrast, additional costs of administration were included.
The treatment costs of a hip fracture include hospital costs, outpatient costs, and rehabilitation costs. In order to calculate the reimbursement for hospital treatment, the webgrouper of the DRG Research Group was used [20]. Surgical procedures were extracted by using OPS codes from a retrospective analysis of SHI data (S72.0–S.72.2) [21]. The cost of rehabilitation relied on the overall days spent in an inpatient follow-up rehabilitation [22]. It was assumed that 45% of hip fracture patients received rehabilitation with 27 days length of stay on average [23, 24].
Costs of additional long-term care due to a hip fracture were calculated according to the level of care (I–III) in the population of non-institutionalized elderly who receive outpatient long-term care [25]. All costs were calculated with respect to the occurrence of dementia, and whether they receive benefits in cash or in kind. The costs for nursing home residents refer to costs of full inpatient care. To incorporate the additional amount of long-term care due to a hip fracture, we assumed that after a hip fracture the share of long-term care recipients in care level I is reduced by 36% while the shares in levels II and III are increased by 14% and 22% [21] (Table 2).
All co-payments by the patients were extracted due to the SHI perspective. To reflect the continuous timing of transitions between the health states, a half-cycle correction was conducted. Costs and benefits were discounted by 3% annually [35]. If costs referred to past years, they were inflated according to the German Consumer Price Index [36]. (For further details on costs’ calculation, see supplemental Tables A1-A4).
Sensitivity analysis and model validation
In order to test the robustness of the results, deterministic and probabilistic sensitivity analyses were performed for the following parameters: incidence of hip and re-fractures, hospital admission rate, mortality, effectiveness, costs of HSM (e.g., decreasing costs by individual contracts with physiotherapists and occupational therapist), utilities, discount rate and, the inclusion of costs of added life years. In addition, the intervention effect was assumed to decline more or less rapidly. Where standard errors were not available from the literature a coefficient of variation of 0.4 (costs and utilities) or 0.2 (mortality) was used to vary parameters for deterministic sensitivity analysis [34].
To assess how a simultaneous variation of parameters affects the results, we carried out a Monte Carlo simulation with 10,000 iterations. Transition probabilities and utilities were assumed to follow a beta distribution while costs were assumed to be gamma distributed. Effectiveness was varied using a normal distribution obtained from the logarithm of the RaR. We transformed cost-effectiveness ratios in net monetary benefits and cost-effectiveness acceptability curves for different values (€0–€100,000) of a willingness to pay (WTP).
In addition, we performed three structural sensitivity analyses: including (i) admissions to nursing home unrelated to hip fracture [37] (see supplemental Table A5 and Figure A1), (ii) two additional health states for reflecting the clinical and economic consequences of vertebral fractures [2, 38] (see supplemental Table A6 and Figure A2), and (iii) a different modeling of excess mortality after hip fracture by taking into account that this excess mortality is only partly due to the fracture itself and, therefore excluding the share attributable to co-morbidity [39] (see supplemental Table A7).
To validate the model, technical accuracy was checked regarding medical plausibility, data entry and potential programming errors (internal validation). For external validation, we assessed the extent to which other models for HSM to prevent falls came to different conclusions (cross validation).
Budget impact analysis
A budget impact analysis was conducted in order to assess the expected annual cost burden on SHI and LCI related to HSM. The incremental costs of a patient who is offered the program were multiplied by the number of elderly community-dwellers between 80 and 85 years of age assigned to a care level [25].
Results
In the base-case, HSM provided to non-institutionalized men aged ≥ 80 years resulted in an ICER of €57,589 per QALY. In women at the same age, the ICER was €9580 per QALY (Table 3).
In the univariate deterministic sensitivity analyses (supplement, Figures A3 and A4), a change of the variables for clinical efficacy, costs of HSM and utilities had the largest effect on the result. Compared to no intervention, assuming a higher efficacy of HSM or, a decrease of the costs of HSM by 40% resulted in a dominance of HSM in women. In men, HSM being less costly was the only variation resulting in an ICER of below €30,000 per QALY.
Including the costs of treatment for additional life years, the ICER would increase by 60% in women and by 10% in men. For a linear decrease of the risk reduction over 1 year (base-case 3), in women, the ICER would increase to €38,523 per QALY (men: €110,214), while a slower effect decrease over 5 years would result in an ICER of €330 per QALY (men: €41,378).
Based on the probabilistic sensitivity analysis, in women, the probability of cost-effectiveness is higher than 54% at a WTP of €0 and almost 95% at a WTP of €20,000. In contrast, the probability of cost-effectiveness in men is 38% at a WTP of €20,000 and reaches 90% at a WTP of €50,000 (Fig. 2).
If admissions to nursing homes unrelated to hip fractures were considered [structural sensitivity analysis (i)], the ICER increases by about €4000 for women (men: €5000). In contrast, including vertebral fractures [structural sensitivity analysis (ii)] would make HSM more cost-effective and even dominant in women (compared to no HSM). The alternative modeling of excess mortality [structural sensitivity analysis (iii)] results in an ICER of about €7500 in women and €64,000 in men (supplement, Table A8).
The budget impact analysis indicated that the adoption of HSM for care-dependent community-dwellers aged ≥ 80 years would cost €7.7 million for the SHI/LCI.
By applying different methods for validation, which resulted in minor changes of the model assumptions, the final model was considered to be valid.
Discussion
This modeling study is the first analysis which evaluated the cost-effectiveness of a community-based HSM for elderly people receiving long-term care in Germany. From the SHI/LCI-perspective, in women aged ≥ 80 years investments in the improvement of home safety results in costs of almost €9600 per QALY compared to no intervention, while in men the cost-effectiveness ratio was six times higher. Because in Germany the majority of long-term care recipients are women, overall, the implementation of HSM targeting all care dependent community-dwellers aged ≥ 80 years may result in annual costs of €7.7 million. Assuming a societal perspective, we would expect similar results, mainly due to the patients increased age which makes aspects of productivity losses negligible. However, the inclusion of costs and effects of family care givers by applying a societal perspective could further improve the cost-effectiveness of HSM.
Targeting HSM to impaired elderly patients with reduced quality of life would result in only marginal gains in QALYs. According to the data used for the model, a hip fracture can be avoided in 1.4% of women and 0.8% of men, whereas admissions to nursing homes can be avoided in less than 0.5% of both men and women.
Strengths of the analysis
The model which was focused on hip fractures as the most fatal and costly consequence of a fall has several strengths. Except for the proportion of fall-related hip fractures (including re-fractures) and, a fracture-related reduction of quality of life, the evidence used for the analysis can be considered as representative for the German health care system. Admissions to German nursing homes due to hip fractures were considered and, transition probabilities were based on large samples of both institutionalized and non-institutionalized German patients in need of long-term care [9, 10, 13].
Furthermore, the majority of data on costs was obtained from a German real-world setting with a high level of detail. Moreover, estimates of the intervention costs were based on a German RCT [18] with specific information about the prescribed technical aids and the related compliance. Because in Germany the prices of technical aids are hardly regulated and differed widely (e.g., the costs of a shower seat vary between €67 and €2608), we calculated medians based on the German Technical Aids Register of the health insurance companies [28].
In addition to different deterministic and probabilistic sensitivity analyses, three structural sensitivity analyses were performed for scrutinizing basic assumptions of our model conceptualization. In these analyses, the inclusion of vertebral fractures, a more precise consideration of excess mortality and, an additional model transition for admissions to nursing home unrelated to hip fracture was assessed.
Limitations
Our analysis has several limitations which might have influenced the results. First, in balancing the results of our analysis decision makers may express concerns due to the lack of strong clinical evidence for HSM. RCTs were underpowered to detect a change in injuries, particularly hip fractures that occurred specifically as a result of an environmental hazard in the home [3]. Therefore, we used the rate of falls as a proxy to calculate the number of fractures which might attract a considerable amount of criticism because of the potential overestimation of cost-effectiveness. Increasing the relative risk of falls (either to reflect a lower reduction of the number of falls by providing HSM or to question the assumption of equal rate ratios for falls and fractures), more than triples the cost-effectiveness ratio in women and almost doubles it in men.
In order to ensure sufficient statistical power, clinical trials which evaluated interventions for preventing falls often chose the number of fallers or the rate of falls as a surrogate for fall-related fractures. A surrogate endpoint is considered useful if it meets important standards for accuracy, precision and reliability [40]. In order to predict fractures in the frail elderly, several epidemiological studies have shown plausibility and a significant association between falls and fractures [41,40,41,44]. A further prerequisite for the quality of a surrogate endpoint is its response to treatment when compared to the patient-relevant outcome. For the rate of falls, clinical trials have demonstrated that the number of falls and injuries (including moderate injuries such as cuts or abrasions) changes consistently in response to fall-prevention, which may explain a substantial proportion of the anti-fracture efficacy [45].
Second, our analysis was targeted to German non-institutionalized elderly people receiving outpatient care, a population assumed to have an increased risk of fracture [7]. However, the subjects of the clinical studies applied for the model were previous fallers, people with poor vision, or elderly who were short-term admitted to a geriatric clinic for different reasons [3]. Because the representativeness of these study samples with the model cohort is uncertain (e.g., bedridden patients do not benefit from HSM), the intervention might be less effective. Moreover, as the trials of the meta-analysis specifically excluded older people who were cognitively impaired, had Parkinson’s disease or already suffered a stroke, the results of our analysis may not be applicable to these groups of people at risk.
Third, due to a lack of valid data, the model could not incorporate potential increases in HRQoL due to a patient’s improved sense of security. Additionally, the avoidance of fractures other than hip or, injuries without a fracture resulting from environmental changes was not modeled. Assuming the availability of appropriate data, the consideration of these aspects would have further decreased the cost-effectiveness ratio (as indicated by a structural sensitivity analysis including vertebral fractures).
Fourth, it was assumed that the treatment effect linearly diminishes after 6 months due to increasing frailty and dementia of the target population. However, a longer lasting treatment effect might also be possible or even more realistic as the technical aids can be used beyond the study period without further regular guidance.
Fifth, the model did not include a transition for admissions to nursing homes unrelated to hip fractures. This assumption neglects the impact of the patient’s co-morbidity on the overall results. Compared to non-frail individuals, even in the absence of fracture frail individuals may have an increased probability of being admitted to a nursing home, which would lead to an overestimation of cost-effectiveness in our analysis [46]. An additional structural sensitivity analysis including admissions to nursing homes unrelated to hip fractures showed a tendency for a less favorite cost-effectiveness ratio.
Sixth, for the analysis, we applied the full amount of excess mortality in the first 6 months after hip fracture [14]. However, to some extent, excess mortality after hip fracture might result from a patient’s co-morbidity and not from the fracture itself [39]. A structural sensitivity analysis assuming lower excess mortality after hip fracture revealed a lower ICER for women and a higher ICER for men. This effect might be attributable to different risk profiles of women and men. In both women and men, a lower excess mortality after hip fracture results in higher costs of long-term care and an increased number of re-fractures. However, because of a higher probability of survival after the first fracture, in women, a higher number of re-fractures could be avoided by the intervention which—in contrast to men—made HSM more cost-effective.
Finally, in case of a hip fracture, we assumed a considerable number of patients being prescribed to a more cost and resource-consuming level of care. However, the older a patient at the time of fracture is, the less might be the savings from preventing a fracture (because previous to a fracture he might already receive a higher level of care as a result of his co-morbidities). In addition, the relatively low intervention costs used for the model were based on a German study which might not be representative for the resource use in other countries. Hence, the cost-saving potential should be considered with caution.
Comparison with previous studies
In addition to several trial-based cost-effectiveness analyses, there are three previous Markov-model-based cost utility studies, two from Australia and one from New Zealand which have evaluated the cost-effectiveness of an HSM [47,46,49]. Compared to our analysis, these studies differed in various methodological aspects. These differences included the preferred model structure, the definitions used for a high-risk population, the inclusion of cost of added life years, the selection of the discount rate, or the assumed effect duration. However, the cost-effectiveness ratios of these analyses are similar to our results. While two of these modeling studies used the rate of falls as clinical outcome, one study was based on the surrogate parameter “rate of injurious falls” which were assumed to be reduced to the same degree as the rate of (injurious or not-injurious) falls [47].
Conclusion
To summarize, the high-risk group of non-institutionalized elderly women at long-term care might benefit most from HSM. Future clinical studies evaluating HSM for long-term care patients should rather be based on fractures than on a surrogate parameter “rate of falls.” Although the “rate of falls” is well correlated with fractures resulting from falls, the assumption of equal reduction rates for fractures and falls remains open to question. Potential additional benefits such as a reduction of injurious falls suffered by relatives could be addressed in order to present a more comprehensive picture about the costs and benefits of HSM.
References
Järvinen TL, Sievänen H, Khan KM, Heinonen A, Kannus P (2008) Shifting the focus in fracture prevention from osteoporosis to falls. Br Med J 336(7636):124–126
Bleibler F, Konnopka A, Benzinger P, Rapp K, König HH (2013) The health burden and costs of incident fractures attributable to osteoporosis from 2010 to 2050 in Germany – a demographic simulation model. Osteporos Int 24:835–847
Cameron ID, Murray GR, Gillespie LD, Robertson MC, Hill KD, Cumming RG, Kerse N (2010) Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev (1):CD005465. https://doi.org/10.1002/14651858.CD005465.pub2
The National Association of Statutory Health Insurance Funds (2016) Recommendations of the National Prevention Conference 2016. https://www.gkv-spitzenverband.de/media/dokumente/presse/pressemitteilungen/2016/Praevention_NPK_BRE_verabschiedet_am_19022016.pdf. [Accessed 21 August 2018]
Lord SR, Menz HB, Sherrington C (2006) Home environment risk factors for falls in older people and the efficacy of home modifications. Age Ageing 35(Suppl 2):ii55–ii59
Connell BR, Wolf SL (1997) Environmental and behavioral circumstances associated with falls at home among healthy elderly individuals. Arch Phys Med Rehabil 78:179–186
Peel NM (2011) Epidemiology of falls in older age. Can J Aging 30(1):7–19
Heinrich S, Rapp K, Rissmann U, Becker C, König HH (2010) Cost of falls in old age: a systematic review. Osteoporos Int 21(6):891–902
Rapp K, Rothenbacher D, Magaziner J, Becker C, Benzinger P, König HH, Jaensch A, Büchele G (2015) Risk of nursing home admission after femoral fracture compared with stroke, myocardial infarction and Pneumonia. J Am Med Dir Assoc 16(8):715.e7–715.e12
Rapp K, Becker C, Cameron ID, Klenk J, Kleiner A, Bleibler F, König HH, Büchele G (2012) Femoral fracture rates in people with and without disability. Age Ageing 41(5):653–658
Rivara FP, Grossman DC, Cummings P (1997) Injury prevention. N Engl J Med 337(9):613–618
Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P (2009) Hip fracture patients at risk of second hip fracture: a Nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res 24(7):1299–1307
Seger W, Sittaro NA, Lohse R, Rabba J (2011) Comparison of survival under domestic or institutional care: the Hannover morbidity and mortality long-term care study. Deutsche Med Wochenschr 136:1465–1471
Rapp K, Becker C, Lamb SE, Icks A, Klenk J (2008) Hip fractures in institutionalized elderly people: incidence rates and excess mortality. J Bone Miner Res 23(11):1825–1831
Luthy C, Cedraschi C, Allaz AF, Herrmann FR, Ludwig C (2015) Health status and quality of life: results from a national survey in a community-dwelling sample of elderly people. Qual Life Res 24(7):1687–1696
Alagic V, Staudinger B (2011) Lebensqualität in deutschen Pflegeeinrichtungen – Ergebnisse einer Befragung mittels dem EQ-5D Instrument. Gesundheitswesen 73(12):795–802
Peasgood T, Herrmann K, Kanis JA, Brazier JE (2009) An updated systematic review of health state utility values for osteoporosis related conditions. Osteoporos Int 20(6):853–868
Nikolaus T, Bach M (2003) Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized falls-HIT trial. J Am Geriatr Soc 51(3):300–305
Kassenärztliche Vereinigung Berlin (2016) Vergütungsliste Physiotherapie. https://www.kvberlin.de/20praxis/50verordnung/20heilmittel/hm_verguetung/verguetung_physio.pdf. [Accessed 21 August 2018]
DRG Research Group (2016) Webgrouper. http://drg.uni-muenster.de/index.php?option=com_webgrouper&view=webgrouper&Itemid=112. [Accessed 21 August 2018]
Müller-Mai CM, Schulze Raestrup US, Kostuj T, Dahlhoff G, Günster C, Smektala R (2015) Einjahresverläufe nach proximalen Femurfrakturen. Unfallchirurg 118(9):780–794
Bundesministerium für Gesundheit (2014) Gesetzliche Krankenversicherung Endgültige Rechnungsergebnisse 2014. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/Statistiken/GKV/Finanzergebnisse/KJ1_2014.pdf. [Accessed 21 August 2018]
Specht-Leible N, Schultz U, Kraus B, Meeder PJ, Quentmeier A, Ewerbeck V, Voss E, Martin M, Oster P (2003) Case-Management und funktionelle Ergebnisse nach proximaler Femurfraktur im höheren Lebensalter. Unfallchirurg 106(3):207–214
Lögters T, Hakimi M, Linhart W, Kaiser T, Briem D, Rueger J, Windolf J (2008) Die geriatrische Frührehabilitation nach hüftgelenknahem Oberschenkelbruch. Unfallchirurg 111(9):719–726
Statistisches Bundesamt (2016) Pflegestatistik 2013. https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Pflege/PflegeDeutschlandergebnisse5224001139004.pdf . [Accessed 21 August 2018]
Kassenärztliche Vereinigung Berlin (2016) Vergütungsliste Ergotherapie https://www.kvberlin.de/20praxis/50verordnung/20heilmittel/hm_verguetung/verguetung_ergo.pdf. [Accessed 21 August 2018]
GKV-Spitzenverband (2016) Leistungsbeschreibung Physiotherapie. https://www.gkv-spitzenverband.de/media/dokumente/krankenversicherung_1/ambulante_leistungen/heilmittel/heilmittel_rahmenempfehlungen/125_Anlage_1a_208.pdf. [Accessed 21 August 2018]
Institut der deutschen Wirtschaft Köln (2016) REHADAT Hilfsmittel http://www.rehadat-hilfsmittel.de/de/. [Accessed 21 August 2018]
Kreck S, Klaus J, Leidl R, von Tirpitz C, Konnopka A, Matschinger H, König HH (2008) Cost effectiveness of ibandronate for the prevention of fractures in inflammatory bowel disease-related osteoporosis. Pharmacoeconomics 26(4):311–328
Kassenärztliche Bundesvereinigung (2016) Online-Version des EBM. http://www.kbv.de/html/online-ebm.php. [Accessed 21 August 2018]
Lauer-Fischer GmbH (2016) Lauer-Taxe®. http://www2.lauer-fischer.de/home/. [Accessed 21 August 2018]
Bundesministerium für Gesundheit: Leistungsansprüche der Versicherten im Jahr 2015 an die Pflegeversicherung im Überblick. https://www.familienservice.uni-mainz.de/files/2015/08/Leistungen-der-Pflegeversicherung-2015.pdf. [Accessed 21 August 2018]
Bundesministerium für Familie, Senioren, Frauen und Jugend (2005) Möglichkeiten und Grenzen selbständiger Lebensführung in privaten Haushalten (MuG III). https://www.bmfsfj.de/blob/79306/eac099e1655fa73eb5866d5b33b7e998/selbststaendigkeit-im-alter-kurzfassung-data.pdf. [Accessed 21 August 2018]
Briggs AH (2004) Handling uncertainty in economic evaluation and presenting the results. In: Drummond M, McGuire A (eds) Economic evaluation in health care. Oxford University Press, New York
Institute of Quality and Efficiency in Health Care (2017) General Methods. https://www.iqwig.de/download/IQWiG_Methoden_Version_4-2.pdf. [Accessed 21 August 2018]
Statistisches Bundesamt: Verbraucherpreisindex für Deutschland. https://www.destatis.de/DE/Publikationen/Thematisch/Preise/Verbraucherpreise/VerbraucherpreiseM.html. [Accessed 21 August 2018]
Rothgang H, Pieper D, Müller R, Unger R (2009) GEK-Pflegereport 2009. Asgard-Verlag, 2009
Lange A, Zeidler J, Braun S (2014) One-year disease-related health care costs of incident vertebral fractures in osteoporotic patients. Osteoporos Int 25(10):2435–2443
Kanis JA, Oden A, Johnell O, De Laet C, Johnsson B, Oglesby AK (2003) The components of exess mortality after hip fracture. Bone 32(5):468–473
Bouxsein ML, Delmas PD (2008) Considerations for development of surrogate endpoints for antifracture efficacy of new treatments in osteoporosis: a perspective. J Bone Miner Res 23(8):1155–1167
Kannus P, Niemi S, Parkkari J, Palvanen M, Heinonen A, Sievänen H, Järvinen T, Khan K, Järvinen M (2002) Why is the age-standardized incidence of low-trauma fractures rising in many elderly populations? J Bone Miner Res 17:1363–1367
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J (2005) Prevention of falls and consequent injuries in elderly people. Lancet 366:1885–1893
Schwartz AV, Nevitt MC, Brown BW Jr, Kelsey JL (2005) Increased falling as a risk factor for fracture among older women: the study of osteoporotic fractures. Am J Epidemiol 161(2):180–185
Dargent-Molina P, Favier F, Grandjean H, Baudoin C, Schott AM, Hausherr E, Meunier PJ, Bréart G (1996) Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet 348(9021):145–149
Robertson MC, Campbell AJ, Gardner MM, Devlin N (2002) Preventing injuries in older people by preventing falls: a metaanalysis of individual-level data. J Am Geriatr Soc 50(5):905–911
Schwenkglenks M, Lippuner K (2007) Simulation-based cost-utility analysis of population screening-based alendronate use in Switzerland. Osteoporos Int 18(11):1481–1491
Pega F, Kvizhinadze G, Blakely T, Atkinson J, Wilson N (2016) Home safety assessment and modification to reduce injurious falls in community-dwelling older adults: cost-utility and equity analysis. Inj Prev 22(6):420–426
Church J, Goodall S, Norman R, Haas M (2016) The cost-effectiveness of falls prevention interventions for older community-dwelling Australians. Aust N Z J Public Health 36(3):241–248
Smith RD, Widiatmoko D (1998) The cost-effectiveness of home assessment and modification to reduce falls in the elderly. Aust N Z J Public Health 22(4):436–440
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
ESM 1
(DOCX 206 kb)
Rights and permissions
About this article
Cite this article
Kunigkeit, C., Stock, S. & Müller, D. Cost-effectiveness of a home safety intervention to prevent falls in impaired elderly people living in the community. Arch Osteoporos 13, 122 (2018). https://doi.org/10.1007/s11657-018-0535-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0535-4