Abstract
Objective
To evaluate the cost effectiveness of interventions designed to prevent falls and fall-related injuries among older people living in residential aged care facilities (RACFs) from an Australian health care perspective.
Methods
A decision analytic Markov model was developed that stratified individuals according to their risk of falling and accounted for the risk of injury following a fall. The effectiveness of the interventions was derived from two Cochrane reviews of randomized controlled trials for falls/fall-related injury prevention in RACFs. Interventions were considered effective if they reduced the risk of falling or reduced the risk of injury following a fall. The interventions that were modelled included vitamin D supplementation, annual medication review, multifactorial intervention (a combination of risk assessment, medication review, vision assessment and exercise) and hip protectors. The cost effectiveness was calculated as the incremental cost relative to the incremental benefit, in which the benefit was estimated using quality-adjusted life-years (QALYs). Uncertainty was explored using univariate and probabilistic sensitivity analysis.
Results
Vitamin D supplementation and medication review both dominated ‘no intervention’, as these interventions were both more effective and cost saving (because of healthcare costs avoided). Hip protectors are dominated (less effective and more costly) by vitamin D and medication review. The incremental cost-effectiveness ratio (ICER) for medication review relative to vitamin D supplementation is AU$2442 per QALY gained, and the ICER for multifactorial intervention relative to medication review is AU$1,112,500 per QALY gained. The model is most sensitive to the fear of falling and the cost of the interventions.
Conclusion
The model suggests that vitamin D supplementation and medication review are cost-effective interventions that reduce falls, provide health benefits and reduce health care costs in older adults living in RACFs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Injuries from falls are a major cause of morbidity and mortality in older people and are a serious financial and social burden to society. |
Falls prevention interventions such as vitamin D supplementation and medication reviews are cost-effective in reducing falls, providing health benefits and reducing health care costs. |
1 Introduction
Falls are common among older people, with one in three people aged over 65 years in the community falling at least once a year [1, 2]. This problem is exacerbated in residential aged care facilities (RACFs), where up to half of all residents fall at least once a year [3–5]. The consequences of falls are often traumatic, including reduced independence, injury or death [6]. The burden of falls to society is also substantial. In Australia, residents of aged care account for more than one in five fall-related hospital in-patient costs (AU$558.5 million in 2006/2007) [7]. With the population aged over 75 years being projected to more than double in the next 20 years, the number of people living in residential aged care, the number of fall-related hospital admissions and the costs of follow-up care will inevitably rise [8]. Identification and implementation of cost-effective interventions to reduce falls in this setting has the potential to significantly benefit older people and reduce the health care burden.
Evidence from randomized controlled trials has demonstrated a number of strategies that are effective in reducing falls or fall-related injuries among residents of RACFs. These include vitamin D supplementation, medication review, hip protectors and exercise-focused multifactorial interventions delivered by a multidisciplinary team [6, 9]. These interventions can be categorized into three types: (1) interventions designed to reduce the risk of falling; (2) interventions designed to reduce the risk of injury subsequent to a fall; and (3) interventions designed to reduce the risk of falling and injury.
A number of economic evaluations have been published exploring the cost effectiveness of multiple falls prevention interventions in older people in community settings [10–12]. These have demonstrated that tai chi programmes and psychotropic medication review may be cost effective. A systematic review of economic evaluations found that a home-based exercise programme aimed at those aged 80 years and older may be cost effective [13]. However, the findings of these analyses cannot easily be extrapolated to the RACF setting because the baseline risk of falling, the effectiveness of the intervention and the cost of delivering the intervention may all differ significantly between the community and RACF settings.
In published economic evaluations of interventions targeting older people living in RACFs, the commonly reported outcome is cost per fracture or cost per fall prevented [14–19]. For example, using this approach, a number of studies have demonstrated that hip protectors are cost effective in preventing hip fractures in residents of RACFs [15, 20–23]. While this approach is useful for comparing different falls prevention strategies, it does not provide the information necessary to convey whether a particular intervention represents value for money relative to other health care programmes. To overcome this limitation, a cost–utility analysis framework, using a generic outcome measure, is preferred.
Injurious falls directly reduce quality of life, but the fear of falling may also indirectly reduce quality of life by restricting mobility, reducing the capacity to undertake daily activities and causing depression [24, 25]. Iglesias et al. suggest that the fear of falling imposes a significant burden on morbidity, which is detrimental to an individual’s quality of life, even in those who have not experienced a fall [26]. The fear of falling and the associated loss in quality of life have largely been ignored in economic modelling of falls prevention in the RACF setting.
This study adds to the literature in a number of ways. First, we adopt a multiple technology appraisal model comparing all effective falls prevention and fall-related injury prevention strategies (as identified by the recent Cochrane reviews [6, 9]) in RACFs within a single model. The advantages of this approach are that interventions can be ranked according to cost, and dominated interventions (interventions that are most costly and less effective) can be excluded, providing a better indication of the relative cost effectiveness of each strategy. Second, the model has been designed to account for the fact that some interventions may reduce falls, while some are designed to prevent injuries subsequent to a fall. Third, we report the outcomes in terms of quality-adjusted life-years (QALYs) gained, which reflect both physical injuries and psychological effects, such as the fear of falling, which can occur with both injurious and non-injurious falls. Finally, the model accounts for different risks of falling based on an individual’s baseline risk profile. In the model, individuals are classified as being at low, medium or high risk of falling, depending on their age and prior history of falls.
2 Methods
2.1 Economic Evaluation
A decision analytic Markov model was developed to assess the cost effectiveness of falls and fall-related injury prevention strategies. The rationale of the model is that falls prevention strategies reduce the number of individuals who fall, and consequently such strategies reduce the risk of falling in the future, which in turn reduces the number of injuries and/or hospitalizations due to falling. Injurious falls can have serious impacts on morbidity and mortality; therefore, any reduction in the number of fall-related injuries is likely to result in measureable increases in QALYs gained. An incremental cost-effectiveness ratio (ICER) was calculated for interventions in the RACF population, using an Australian health system perspective. Please see the technical appendix in the Electronic Supplementary Material for details of the model development.
2.1.1 Model
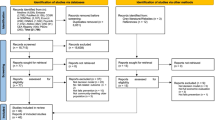
The Markov model was designed to capture the transition between four health states. Individuals were initially assigned to one of three Markov states: (1) low-risk (individuals who have never fallen); (2) medium risk (individuals who have previously fallen but incurred no injury); or (3) high risk (individuals who have previously fallen and incurred an injury). Individuals are able to transition between these states or to a terminal state, death. Individuals move between states by following a multiple-event decision tree. The decision tree incorporates the ability to adjust the probability of falling or the probability of injury due to a fall (Fig. 1).
Costs and outcomes were incorporated into the model as a mean value per event per cycle, weighted by the probability of the event occurring. The cycle length was 1 year, and all costs and outcomes were discounted at a rate of 5 % per annum [27]. A sensitivity analysis was conducted (described in detail below). All analysis was conducted using TreeAge Pro Suite 2014 (TreeAge Software Inc., Williamstown, MA, USA).
2.1.2 Effectiveness
The effectiveness data were derived from two systematic reviews conducted by the Cochrane Collaboration [6, 9]. Interventions that significantly reduced the rate of falling or the risk of injury following a fall were included in the model.Footnote 1 Medication review, vitamin D supplementation and a multifactorial intervention with a multidisciplinary team all reduced the rate of falling, with the multifactorial intervention also reducing the risk of falling [6]. For these interventions, the estimated rate ratio reported in the reviews was used to adjust the probability of falling for each intervention compared with ‘no intervention’. Hip protectors reduce the risk of a hip fracture (rather than rate of falling), and the model was adjusted for this decrease in the risk of injury and not the rate of falling [9]. The rate ratios and risk ratio (for hip protectors) used in the model are listed in Table 1.
2.1.3 Costs
The cost of each intervention is outlined in Table 1. Intervention costs were sourced from the Medicare Benefits Schedule (MBS), Pharmaceutical Benefits Scheme (PBS), Department of Veterans’ Affairs, New South Wales (NSW) nurse wage rates and other publicly available online price lists. All health care-related costs, including emergency department (ED) attendance, admission to hospital and medical attendances, were sourced from Watson et al. [7]. All costs were adjusted to 2015 dollars, using the average Australian Institute of Health and Welfare (AIHW) health expenditure price index [28] and applied on a per fall basis in the cycle in which they occurred. All costs included in the model and the ranges around the estimates are listed in Table 1.
A medication review was considered to include a Residential Medication Management Review (RMMR), which includes a review by a pharmacist in collaboration with a general practitioner (GP) and other members of the residents’ health care team, plus an MBS item to cover the involvement of the GP in the review. Vitamin D supplementation is based on 1000 IU daily plus 600 mg of calcium daily. The multifactorial interventions included a falls risk assessment and follow-up, a medication review, education of staff, exercise classes (two per week), an optical assessment and environmental modifications.
2.1.4 Transition Probabilities
The initial population distributions were assigned as follows: 49.5 % were considered low risk (no fall in the previous year) [29], 39.5 % were considered medium risk (non-injurious fall in the previous year) and 11 % were considered high risk (injurious fall in the previous year). The latter percentage is based on the number of falls requiring hospitalizations [7]. At baseline, the probability of falling in the medium-risk group was set at 50 % per year. The estimated probabilities of falling in the low-risk (32 %) and high-risk groups (72 %) were used to estimate falling rates for the low-risk and high-risk groups adjusted according to the findings of Lord et al. [30] and using expert opinion (Professor Stephen Lord, personal communication). The transition probabilities of attending an ED, consulting other medical services, hospital admission or death due to a fall were obtained from Watson et al. (Table 1) [7]. The probability of attending an ED is estimated by dividing the number of falls requiring an ED attendance by the number of falls in each age group. The same calculation is used to estimate the number of falls requiring other medical services. The probability of being admitted to hospital because of a fall, contingent on ED attendance, was calculated as the number of hospital admissions divided by the total number of ED attendances.
2.1.5 Utility
The baseline utility estimates used in the model were based on Australian Population Norms, derived from the SF-36 using the SF-6D algorithm (Household, Income and Labour Dynamics in Australia [HILDA] survey) [31]. A utility decrement (−0.06) was subtracted from the population norms to take into account RACF residential status [32]. Additional utility decrements were also incurred once an individual attended ED (−0.014), was admitted to hospital (−0.144) or had a previous fracture from a fall in the previous year (−0.072). The utility decrements for a hospitalization and previous fall were calculated using a weighted average due to a hip (94 %) or vertebral fracture (6 %) [33, 34]. The utility loss due to a wrist fracture [35] was used for a non-hospitalized injury that presented at ED, as wrist fractures are the most common facture not requiring hospital admission in the older population [36]. No quality-of-life decrement was assumed in subsequent years after the decrement for a wrist fracture in the first year [37]. A utility decrement to account for the fear of falling (−0.045) was included in the model once a fall occurred, regardless of injury or hospitalization [26]. The decrement was estimated by weighting the mean utility decrement by the respondent’s baseline fear of falls from the three studies included in the analysis by Iglesias et al. [26].
2.2 Base-Case Analysis
The starting age of the cohort was based on the mean age of residents in Australian RACFs (84 years) [38, 39]. The model was run until all members of the cohort had died. The costs and benefits of the interventions were assumed to occur in every year of the model. A health care system perspective was adopted for both costs and benefits. The risk of falling was adjusted on the basis of the rate ratio obtained in the literature. For hip protectors, the rate of hospitalization was adjusted each year.
Outcomes from the model were measured in terms of falls avoided and QALYs gained. The results include the cost of providing the intervention plus any costs for medical treatment incurred as a result of an injurious fall. In this respect, the ‘no intervention’ alternative is not costless, because this option incurs the highest fall-related treatment costs.
2.3 Sensitivity Analysis
Sensitivity analysis was undertaken using confidence intervals (where available), using the best estimates of ranges or by adjusting the parameter by 25 %. A probabilistic sensitivity analysis (PSA) was also undertaken. A distribution was estimated for each of the parameters in the model, based on either confidence intervals, standard errors or an appropriate range of estimates around the mean. By assigning distributions to the model parameters, a Monte Carlo simulation with 10,000 draws was performed to reflect the joint parameter uncertainty. Table 1 shows the distributions for all of the transition probabilities, costs and utility values included in the model.
3 Results
Table 2 summarizes the estimated costs and outcomes for each intervention. Vitamin D supplementation (AUD$2289) and medication review (AUD$2321) are both less costly than the ‘no intervention’ option (AUD$2925). This is due to health care costs avoided. The most expensive intervention is the multifactorial intervention, which costs on average AUD$4991. In terms of benefits, the ‘no intervention’ option is the least effective; under this scenario, it is predicted that individuals will fall on average 2.059 times and gain 1.225 QALYs. Vitamin D supplementation, medication review and multifactorial intervention are the most effective interventions in terms of reduction in falls. On average, it is estimated that vitamin D will result in 0.593 falls being avoided and 1.260 QALYs gained (an average incremental gain of 0.035 QALYs relative to no intervention); medication review will result in 0.818 falls being avoided and 1.273 QALYS gained (an incremental gain of 0.048 QALYs); and multifactorial intervention will result in 0.858 falls being avoided and 1.276 QALYs gained. In terms of cost per fall avoided, vitamin D and medication review dominated ‘no intervention’, as the health care costs avoided from a reduced number of falls rendered the interventions cost saving compared with ‘no intervention’ with higher health care costs.
The interventions were then ranked according to their relative cost. Dominated interventions were removed, and ICERs were calculated. The ‘no intervention’ option is dominated by both vitamin D supplementation and medication review. In other words, both of these interventions are less costly and more effective than ‘no intervention’. When the interventions are ranked according to cost, hip protectors are also dominated by vitamin D and medication review. This is because vitamin D supplementation and medication review provide greater benefit at a lower cost than hip protectors. The resulting ICER for medication review compared with vitamin D is AU$2442 per QALY. Multifactorial intervention provides more QALYs than the next best option (medication review); however, the ICER is AU$1,112,500 per QALY gained.
3.1 Sensitivity Analysis
The costs of the interventions, starting age of the cohort and fear of falling are drivers in the model. When fear of falling is excluded from the model, vitamin D supplementation and medication review still dominate ‘no intervention’. The effect of adjusting the probability of falling or the utility loss from a fracture had little impact on the overall ICERs (Fig. 2). An additional sensitivity analysis where hip protectors are limited to medium- and high-risk populations (reflecting a more real-world setting) still resulted in hip protectors being dominated by vitamin D and medication review. Threshold analysis demonstrated that the cost of the multifactorial intervention would need to be lower than AU$280 to be considered cost effective (AU$50,000 per QALY) relative to medication review. Moreover, applying the lower rate ratio for multifactorial intervention (0.50) and the upper rate ratio for medication review (0.72) resulted in an ICER of AU$75,620 per QALY for multifactorial intervention compared with medication review.
The cost-effectiveness acceptability curve (Fig. 3) demonstrates the probability of each intervention being cost effective across a range of willingness-to-pay thresholds. At a threshold of AU$0–20,000 per QALY, vitamin D is the most cost-effective option. At a threshold of >AU$20,000 per QALY, medication review supplementation is the most cost-effective option. At a threshold of approximately AU$1,200,000, multifactorial intervention is unlikely to be considered cost effective. Hip protectors and no intervention are not considered to be cost effective.
4 Discussion
In this paper, we report the findings of a decision analytic model designed to compare the cost effectiveness of interventions with proven effectiveness in preventing falls or fall-related injuries in older people living in RACFs.
The findings are interesting for a number of reasons. First, new health technologies generally tend to provide additional benefits at additional cost; however, we demonstrate that vitamin D supplementation and medication review provide additional benefits at lower cost relative to the ‘no intervention’ option. This is because vitamin D supplements and conducting an annual medication review are low-cost interventions and the health care costs saved when falls are avoided outweigh the costs of providing either intervention. Second, although the multifactorial intervention and hip protectors appear cost effective when compared with ‘no intervention’ (AUD$41,074/QALY gained and AUD$1935/QALY gained), when compared with the next best alternative (medication review), hip protectors interventions are dominated, as medication review is more effective and less costly. The ICER for multifactorial intervention is greater than AUD$1.2 million, which would not be considered cost effective at current willingness-to-pay thresholds.
These findings demonstrate the importance of using a multiple technology appraisal approach when evaluating the cost effectiveness of a number of competing health care interventions. In the case of falls prevention, where there are a number of possible alternative interventions with demonstrable effectiveness [6], economic evaluations that compare a single strategy against ‘no intervention’ may provide spurious cost-effectiveness estimates that overestimate the real value for money. This is because ‘no intervention’ may not be the best alternative comparator.
Many economic evaluations of falls prevention strategies report results in terms of cost per fall avoided [40–45]. This endpoint is useful when the decision maker has decided to invest in a falls prevention strategy, because the lowest incremental cost per fall avoided can be identified. However, there are limitations to such an approach, since it is difficult to judge whether an intervention represents value for money in terms of the total health care budget. Unless the value that society is willing to pay to avoid a fall is known, an alternative approach is required. The approach taken in this paper was to use the generic outcome measure of QALYs gained. The advantage of using QALYs as the outcome measure is that interventions aimed at different health conditions (not just falls prevention) can be compared. In fact, it was essential to use QALYs in this model because multiple endpoints were compared. For example, evaluations of medication review typically measure success in terms of falls avoided, while the effectiveness of hip protectors is usually measured in terms of fractures avoided. For an intervention to be cost saving, the model assumes that the health care costs avoided compensate for the cost of the interventions. Given the health funding arrangement in Australia, this would require the federal and state governments to subsidize the falls prevention strategies within RACF facilities. If the RACF facilities funded the intervention without subsidization, then the assumption of cost saving would no longer apply to the RACF facility.
Another advantage of using QALYs is that other factors considered important can be incorporated into the model—for example, fear of falling. The fear of falling decrement used in the model captures the anxiety and loss of confidence that may occur following a fall. When the utility decrement for fear of falling is excluded from the model, vitamin D supplementation and medication review still dominate ‘no intervention’ (since they are both cost saving). A criticism of including a utility for fear of falling in the model is that it may result in double counting, as the disutility associated with an injurious fall may have already been taken into account in the QALY measurement.
There are number of limitations to the model. It is assumed that the benefits and costs of the interventions are incurred each year the model is run. This assumption may overestimate the cost effectiveness of interventions if the results of the clinical trial cannot be replicated in subsequent years. The point estimates used in the economic model are based on Cochrane reviews of interventions aimed at falls prevention and falls-related injuries [6, 9]. While random-effects models may explain statistical heterogeneity, they do not fully take into account heterogeneity within interventions. For example, the duration of the follow-up is not consistent between studies, and the pooled estimates of costs and effectiveness may mask the fact that intensive interventions (e.g. higher doses of vitamin D versus lower doses of vitamin D, or exercise three times a week compared to once a week) are more effective relative to the cheaper equivalent. Furthermore, the authors of the Cochrane review caution that the effectiveness of hip protectors remains uncertain because of bias in many of the cluster-randomized trials, low adherence rates among participants and extrapolation of the results to all types of hip protectors. Finally, the generalizability of the results may not be as strong for multifactorial interventions compared with vitamin D or medication review, given the variation in the delivery of the interventions across jurisdictions.
Previous studies have demonstrated that hip protectors are either cost effective or cost saving relative to ‘no intervention’ for the prevention of hip fractures [14–23]. Our results concur with these findings when compared with ‘no intervention’; however, hip protectors were extendedly dominated by a combination of vitamin D and ‘no intervention’. The other interventions included in this study have largely been ignored in the cost-effectiveness literature. Although we conclude that some falls prevention interventions may be cost saving and may dominate the ‘no intervention’ option, clearly this depends on the perspective of the analysis. In this study, we adopt a health care system perspective, which assumes that the provider of health care services also funds the falls prevention intervention. If this is not the case (e.g. private provision of RACF services), the cost savings estimated in this analysis may not be realized by the funder of the intervention.
5 Conclusion
Fall-related injuries are a leading cause of morbidity and mortality in older people living in RACFs. We found that ‘no intervention’ was dominated by vitamin D supplementation and medication review, since these low-cost interventions provide additional health benefits at lower costs than the ‘no intervention’ option. Relative to vitamin D supplementation, medication review appears to be cost effective; hip protectors and multifactorial interventions are unlikely to be cost effective from an Australian health care system perspective.
Notes
Note, exercise (gait, balance, functional training) was also deemed effective in the systematic review but was not included in the analysis, as only trials with greater than 20 participants in each arm were included. Two trials in the Cochrane review [3] (Shimada et al. (2004) and Sihvonen et al. (2004)) had 20 participants or fewer, and removing these trials resulted in a non-significant rate ratio.
References
Gill T, Taylor AW, Pengelly A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology. 2005;51(5):340–5 (PubMed PMID: 16110237).
Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994;42(10):1110–7.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146 (PubMed PMID: 22972103).
Barker AL, Nitz JC, Low Choy NL, Haines T. Measuring fall risk and predicting who will fall: clinimetric properties of four fall risk assessment tools for residential aged care. J Gerontol A Biol Sci Med Sci. 2009;64(8):916–24.
Norton R, Butler M. Prevention of falls and fall-related injuries among institutionalised older people. Wellington: University of Auckland; 1997.
Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev. 2012;12:CD005465 (PubMed PMID: 23235623).
Watson WL, Clapperton AJ, Mitchell RJ. The incidence and cost of falls injury among older people in New South Wales 2006/07. Sydney: NSW Department of Health; 2010.
Australian Bureau of Statistics. Household and family projections, Australia, 2006 to 2031. Canberra: Commonwealth of Australia; 2010.
Gillespie WJ, Gillespie LD, Parker MJ. Hip protectors for preventing hip fractures in older people. Cochrane Database Syst Rev. 2010;(10):CD001255 (PubMed PMID: 20927724. Epub 2010/10/12. eng).
Church J, Goodall S, Norman R, Haas M. The cost-effectiveness of falls prevention interventions for older community-dwelling Australians. Aust N Z J Public Health. 2012;36(3):241–8.
Frick KD, Kung JY, Parrish JM, Narrett MJ. Evaluating the cost-effectiveness of fall prevention programs that reduce fall-related hip fractures in older adults. J Am Geriatr Soc. 2010;58(1):136–41 (PubMed PMID: 20122044. Epub 2010/02/04. eng).
Day L, Hoareau E, Finch C, Harrison J, Segal L, Bolton T, et al. Modelling the impact, costs and benefits of falls prevention measures to support policy-makers and program planners. Monash University Accident Research Centre. Melbourne: Monash University Accident Research Centre; 2009.
Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. Does a home based strength and balance programme in people aged ≥80 years provide the best value for money to prevent falls? A systematic review of economic analyses of falls prevention interventions. Br J Sports Med. 2009 (PubMed PMID: 19666627. Epub 2009/08/12. Eng).
van Schoor NM, de Bruyne MC, van der Roer N, Lommerse E, van Tulder MW, Bouter LM, et al. Cost-effectiveness of hip protectors in frail institutionalized elderly. Osteoporos Int. 2004;15(12):964–9 (PubMed PMID: 15103454. Epub 2004/04/23. eng).
Singh S, Sun H, Anis AH. Cost-effectiveness of hip protectors in the prevention of osteoporosis related hip fractures in elderly nursing home residents. J Rheumatol. 2004;31(8):1607–13 (PubMed PMID: 15290742. Epub 2004/08/04. eng).
Honkanen LA, Schackman BR, Mushlin AI, Lachs MS. A cost-benefit analysis of external hip protectors in the nursing home setting. J Am Geriatr Soc. 2005;53(2):190–7 (PubMed PMID: 15673340. Epub 2005/01/28. eng).
Meyer G, Wegscheider K, Kersten JF, Icks A, Muhlhauser I. Increased use of hip protectors in nursing homes: economic analysis of a cluster randomized, controlled trial. J Am Geriatr Soc. 2005;53(12):2153–8 (PubMed PMID: 16398901. Epub 2006/01/10. eng).
Kumar BA, Parker MJ. Are hip protectors cost effective? Injury. 2000;31(9):693–5 (PubMed PMID: 11084156. Epub 2000/11/21. eng).
Wilson CJ, Datta SK. Tai chi for the prevention of fractures in a nursing home population: an economic analysis. J Clin Outcomes Manag. 2001;8(3):19–27.
Waldegger L, Cranney A, Man-Son-Hing M, Coyle D. Cost-effectiveness of hip protectors in institutional dwelling elderly. Osteoporos Int. 2003;14(3):243–50 (PubMed PMID: 12730792. eng).
Gandjour A, Weyler E-J. Cost-effectiveness of preventing hip fractures by hip protectors in elderly institutionalized residents in Germany. Value Health. 2008;11(7):1088–95.
Segui-Gomez M, Keuffel E, Frick KD. Cost and effectiveness of hip protectors among the elderly. Int J Technol Assess Health Care. 2002;18(1):55–66 (PubMed PMID: 11987442. Epub 2002/05/04. eng).
Colon-Emeric CS, Datta SK, Matchar DB. An economic analysis of external hip protector use in ambulatory nursing facility residents. Age Ageing. 2003;32(1):47–52 (PubMed PMID: 12540348. Epub 2003/01/24. eng).
Boyd R, Stevens JA. Falls and fear of falling: burden, beliefs and behaviours. Age Ageing. 2009;38(4):423–8 (PubMed PMID: 19420144. eng).
Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001;30 Suppl 4:3–7 (PubMed PMID: 11769786. eng).
Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. 2009;20(6):869–78 (PubMed PMID: 18846400. eng).
Department of Health Pharmaceutical Evaluation Branch. Guidelines for preparing submissions to the Pharmaceutical Benefits Advisory Committee (version 4.4). Canberra: Department of Health; 2015. Available from: http://www.pbac.pbs.gov.au/section-d/section-d-cea/d4-variables-in-the-economic-evaluation.html.
Australian Institute of Health and Welfare. Health expenditure Australia 2012–13. Canberra: Australian Institute of Health and Welfare; 2014.
Delbaere K, Close JC, Menz HB, Cumming RG, Cameron ID, Sambrook PN, et al. Development and validation of fall risk screening tools for use in residential aged care facilities. Med J Aust. 2008;189(4):193–6 (PubMed PMID: 18707561. eng).
Lord SR, Ward JA, Williams P, Anstey KJ. An epidemiological study of falls in older community-dwelling women: the Randwick Falls and Fractures Study. Aust J Public Health. 1993;17(3):240–5 (PubMed PMID: 8286498. eng).
Norman R, Church J, van den Berg B, Goodall S. Australian health-related quality of life population norms derived from the SF-6D. Aust N Z J Public Health. 2013;37(1):17–23.
Honkanen LA, Mushlin AI, Lachs M, Schackman BR. Can hip protector use cost-effectively prevent fractures in community-dwelling geriatric populations? J Am Geriatr Soc. 2006;54(11):1658–65 (PubMed PMID: 17087691. eng).
Peel NM, Kassulke DJ, McClure RJ. Population based study of hospitalised fall related injuries in older people. Inj Prev. 2002;8:280–3.
Strom O, Borgstrom F, Sen SS, Boonen S, Haentjens P, Johnell O, et al. Cost-effectiveness of alendronate in the treatment of postmenopausal women in 9 European countries—an economic evaluation based on the Fracture Intervention Trial. Osteoporos Int. 2007;18(8):1047–61 (PubMed PMID: 17333449. eng).
Brazier JE, Green C, Kanis JA. A systematic review of health state utility values for osteoporosis related conditions. Osteoporos Int. 2002;13:768–76.
Boufous S, Finch C, Close J, Day L, Lord S. Hospital admissions following presentations to emergency departments for a fracture in older people. Inj Prev. 2007;13(3):211–4 (PubMed PMID: 17567981. Pubmed Central PMCID: 2598384. Epub 2007/06/15. eng).
Zethraeus N, Borgstrom F, Strom O, Kanis JA, Jonsson B. Cost-effectiveness of the treatment and prevention of osteoporosis—a review of the literature and a reference model. Osteoporos Int. 2007;18(1):9–23 (PubMed PMID: 17093892. eng).
Australian Bureau of Statistics. Population by age and sex, regions of Australia, 2013 (3235.0). Canberra: Commonwealth of Australia; 2013.
Australian Institute of Health and Welfare. Residential aged care in Australia 2007–08: a statistical overview. Aged Care Statistics Series 28. Cat. no. AGE 58. Canberra: Australian Institute of Health and Welfare; 2009.
Campbell AJ, Robertson MC, La Grow SJ, Kerse NM, Sanderson GF, Jacobs RJ, et al. Randomised controlled trial of prevention of falls in people aged ≥75 with severe visual impairment: the VIP trial. BMJ. 2005;331(7520):817 (PubMed PMID: 16183652. eng).
Rizzo JA, Baker DI, McAvay G, Tinetti ME. The cost-effectiveness of a multifactorial targeted prevention program for falls among community elderly persons. Med Care. 1996;34(9):954–69 (PubMed PMID: 8792783. eng).
Robertson MC, Devlin N, Gardner MM, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls: 1. Randomised controlled trial. BMJ. 2001;322(7288):697–701 (PubMed PMID: 11264206. eng).
Robertson MC, Gardner MM, Devlin N, McGee R, Campbell AJ. Effectiveness and economic evaluation of a nurse delivered home exercise programme to prevent falls: 2. Controlled trial in multiple centres. BMJ. 2001;322(7288):701–4 (PubMed PMID: 11264207. eng).
Salkeld G, Cumming RG, O’Neill E, Thomas M, Szonyi G, Westbury C. The cost effectiveness of a home hazard reduction program to reduce falls among older persons. Aust N Z J Public Health. 2000;24(3):265–71 (PubMed PMID: 10937402. eng).
Smith RD, Widiatmoko D. The cost-effectiveness of home assessment and modification to reduce falls in the elderly. Aust N Z J Public Health. 1998;22(4):436–40 (PubMed PMID: 9659769. eng).
Liu Z. The probability of nursing home use over a lifetime in Australia. Int J Soc Welf. 2000;9:169–80.
Rubenstein LZ, Josephson KR, Robbins AS. Falls in the nursing home. Ann Intern Med. 1994;121(6):442–51 (PubMed PMID: 8053619. Epub 1994/09/15. eng).
Acknowledgments
This study was funded as part of the Costing for Health Economic Evaluation Program (CHEEP), funded by NSW Health and the Cancer Institute NSW. The authors thank the NSW Health Advisory Committee for their contribution to the project, and also thank the referees for their time spent reviewing the paper and their comments, which helped improve the final version.
Author contributions
All authors were involved in the conception and planning of the economic analysis. J. Church developed the economic model. J. Church and S. Goodall interpreted and synthesized the results of the economic model and drafted the manuscript. All authors reviewed the draft manuscript and approved the final version for submission.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors (J. Church, S. Goodall and M. Haas) declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Church, J.L., Haas, M.R. & Goodall, S. Cost Effectiveness of Falls and Injury Prevention Strategies for Older Adults Living in Residential Aged Care Facilities. PharmacoEconomics 33, 1301–1310 (2015). https://doi.org/10.1007/s40273-015-0313-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-015-0313-8