Abstract
Objectives
To explore the prevalence and ethnic differences of osteosarcopenic obesity (OSO) and dyslipidemia and their relationship among Maonan, Mulam, Hmong, and Yao minorities in China.
Methods
A total of 2315 Maonan, Mulam, Hmong, and Yao women aged 20–95 from Guangxi were included in this study. Questionnaire survey was carried out and their blood lipids were tested. Body compositions were measured by bioelectrical impedance analysis, and T-score was assessed by ultrasonic examination, respectively.
Results
Our study showed ethnic-specific prevalence of OSO. In older women, the incidence rates of OSO in Mulam were 4.9, 12.6, and 11.5% in Maonan, Mulam, and Hmong ethnicity, respectively. In younger group, the incidence rates of OSO were 0.4, 0.4, and 0.6%, respectively. However, there is no prevalence of OSO in Yao women in two groups. The prevalence of dyslipidemia in younger women was 22.86, 29.89, 43.35, and 80.00% in group numbering one, two, and three, respectively. In older women, it was 29.13, 39.02, 41.37, and 52.38%, respectively. Based on logistic regression analysis, after controlling for covariates, dyslipidemia in younger group was positively associated with a higher number of adverse body composition, especially for OSO (OR = 12.53, 95%CI 1.34–116.99). Compared with normal women, OSO women in older group were also more likely to have dyslipidemia (OR = 6.75, 95%CI 3.19–14.31).
Conclusion
OSO may be a risk factor for dyslipidemia in the ethnic groups. Thus, efforts to promote healthy aging should be focused on preventing obesity and maintaining bone health and muscle mass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The two greatest epidemiological trends that characterize our generation are the aging of the population and the obesity epidemic [1]. It is predicted that, in the fifth decade of the twenty-first century, two billion people of earth will be older than 60 [2]. With that population boom looming, efforts to deal with problems of older age will become major challenges. Besides, due to a decreased physical activity and westernized diet, the prevalence of metabolic syndrome has dramatically increased in recent years [3]. How to prevent the risk factors for cardiametabolic diseases such as obesity and dyslipidemia has challenged the elderly Chinese population.
Aging is accompanied by changes in body composition, (1) decline in bone health, manifested as osteopenia and/or osteoporosis (OP); (2) deterioration of muscle quantity and quality, manifested as sarcopenia; and (3) increased presence of adipose tissue, manifested as obesity. These body composition (bone mass, muscle mass, and adipose tissues) are interconnected [4]. The mechanism of interactions between bone and muscle is well established, and age-related declines in muscle mass are associated with low bone mineral density [5]. It is not surprising that there is a growing number of research that suggests a striking parallel between OP and sarcopenia [6]. Besides, the increase in adipose tissues also related to the loss of muscle and bone mass [4]. While sarcopenia remains undiagnosed, sarcopenia and sarcopenia obesity (SO) are commonly studied and have been recognized in the last decade [7]. Recently, a combination of osteopenia and/or OP, sarcopenia, and obesity, the newly termed osteosarcopenic obesity (triad of bone, muscle, and adipose tissue impairment), has been given special attention. However, despite the growing important of OSO, studies evaluating the prevalence of OSO are limited. Moreover, there is also a lack of report about the association with OSO and dyslipidemia in China.
Maonan, Mulam, Yao, and Hmong are the major indigenous ethnic groups in Guangxi, China. These minorities have been reported to exhibit significant differences in their genetic background [8] and morphology [9]. Therefore, the elucidation of ethnic variation in OSO and its associations with dyslipidemia in these ethnicities are essential for the development of public health programs for the increasingly elderly Chinese population.
This study aimed to investigate the prevalence and ethnic differences of OSO among a representative sample of younger and older Maonan, Mulam, Hmong, and Yao adult women living in China, and to determine the association of OSO with dyslipidemia among these ethnic groups.
Materials and methods
Participants
Maonan, Mulam, Yao, and Hmong are the major indigenous ethnic groups in Guangxi, China. They live in different villages. Maonan ethnicity has a population of 69,000, accounting for 0.15% of Guangxi’s population. Mulam ethnicity has a population of 15.26 million, accounting for 98% of the national Mulam population and 0.34% of the Guangxi’s population. Yao ethnicity has a population of 1.349 million, accounting for 62% of the national Yao population, accounting for 3% of Guangxi’s population. Hmong ethnic group in Guangxi has a population of 423,000, accounting for 5.5% of the national Miao population and 1% of Guangxi’s population. We used a stratified sampling method to choose a representative sample of the general population of these four minorities of Guangxi, China. The inclusion criteria of each ethnicity was that both of each woman’s parents were of the same ethnicity. The exclusion criteria was included: (1) if they were pregnant, breast-feeding, took OP or dyslipidemia medication, and used estrogen or progesterone; and (2) participants with serious metabolic, cardiovascular, or endocrine diseases (i.e., Cushing syndrome, hypothyroidism, hyperthyroidism, prolactinoma, hyperparathyroidism, renal insufficiency) based on their health history. In this way, a total of 2315 unrelated and healthy women aged 20–95 years, were randomly selected from villages of Guangxi Province and were invited to be participants. We classified all participants into two groups by age: younger group (age < 60 years, including 264 Maonan, 255 Mulam, 458 Yao, and 491 Hmong women) and older group (age ≥ 60 years, including 182 Maonan, 182 Mulam, 214 Yao, and 269 Hmong women). T-score, blood lipids, height, weight, and other indices of body composition were measured at the same time by trained technicians. Written informed consent was obtained from all participants in this cross-sectional study, which has been supported by the National Natural Science Foundation of China and given approval by the Institution Review Board for studies using human subjects.
Anthropometry
Anthropometry measurements, with participants wearing no shoes and light clothing, were taken by trained research staff in each village. Height was measured to the nearest 0.1 cm, using a stadiometer. The circumference of the waist and hip was determined on uncovered skin using an inelastic measuring tape measure. Waist circumference was measured to the nearest 0.1 cm with a standard flexible tape measure at the level of the iliac crest. Hip circumference was measured to the nearest 0.1 cm with a standard flexible tape measure at the maximum extension at the buttock level. In addition, the BMI was calculated as the weight (kg) divided by height squared (m2), and the waist-to-hip ratio (WHR) was calculated as the waist circumference divided by hip circumference.
Whole-body composition
Body composition indices including weight, FFM, whole-body and segmental (trunk, right and left upper limbs, and right and left lower limbs) FM, whole-body and segmental (trunk, right and left upper limbs, and right and left lower limbs) MM, visceral fat contents (VFC), and subcutaneous fat contents (SFC) were assessed using bioelectrical impedance analysis (BIA) (TANITA-MC180, Japan). The participants were instructed to refrain from exercise for 12 h, to refrain from eating for 3 h and to consume 500 ml of water 1 h before BIA measurement. They were also required to empty their bladder immediately prior to the measurements. They held a handgrip with two electrodes per hand with bare feet on the analyzer’s footpads in light clothing. Quality control was performed through daily calibration with a phantom supplied by the manufacturer. In accordance with each of the manufacturers, the precision of the method is 1.0–3.0% for each of the three scanners. The percentage of body fat (BF%) was calculated as 100 × FM/weight. ASM was the appendicular skeletal muscle mass, and AFM was the sum of appendicular fat mass.
Definition of OP
Bone mineral density was estimated in all participants using a SONOT3000 ultrasound bone densitometer (Korea), which measured the transmission of high-frequency sound waves through the heel after the participant siting positioned with the right foot bared. From the measured signal, three ultrasound parameters are simultaneously determined: the speed of sound (SOS), broadband ultrasound attenuation (BUA), and the quantitative ultrasound index (QUI). The SONOT3000 system software estimates bone mineral density from the QUI and compares it with that of young, healthy, sex-matched participants to produce a T-score [10]. The T-score is widely used to assist in the interpretation of bone mineral density results and is employed to define the degree of bone mineral density. According to the WHO criteria [11], OP was defined as a T-score value of − 2.5 or lower, while osteopenia was defined as a T-score between − 1.0 and − 2.5, and normal bone was defined as a T-score above − 1.0.
Definition of dyslipidemia
Blood lipids and lipoproteins were tested on samples obtained after an overnight fast (8 h at least). Total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) were measured in EDTA plasma. Hypercholesterolemia was defined as TC > 6.22 mmol/L, hypertriglyceridemia as TG > 2.26 mmol/L, reduced HDL-C as HDL-C < 1.04 mmol/L, and increased LDL-C as LDL-C > 4.14 mmol/L. Dyslipidemia was defined by the presence of one or more than one abnormal serum lipid concentration [12].
Definitions of sarcopenia and OSO
There is a lack of standardized criteria for the definition of OSO, with several combinations and cut-off points in use. One of the most widely used diagnostic criteria in sarcopenia is Baumgartner’s methods [13]. In this way, sarcopenia was defined as ASM (kg) divided by height squared (m2) (ASM/Ht2) that was < 2 SDs below the sex- and ethnic-specific mean of a young reference group. The cutoff value was 6.05, 6.17, 5.44, and 6.31 kg/m2 in Maonan, Mulam, Yao, and Hmong ethnicity, respectively. Obesity was defined as the two upper quintiles for BF% [14]. Therefore, the diagnostic criteria for OSO must be based on the combination of bone and muscle loss, and increased adiposity [15]. Based on the number of adverse body composition. We divided all subjects into four non-overlapping groups: 0 (normal; without low bone mass, low muscle mass, or obesity), 1 (having one of the components), 2 (having two of the components), and 3 (osteosarcopenic obesity).
Statistical analyses
Descriptive statistics were expressed as the mean ± s.d. for the continuous variables and as frequencies for the categorical variables. Independent t test was used to assess the difference in the continuous variables between younger and older women of each ethnicity. chi-square test with an R × C contingency table was used to assess the significance of the age- and ethnic-specific differences in the categorical variables (the detection rate of osteopenia/OP/dyslipidemia). Analysis of variance (ANOVA) was employed to compare differences between the four groups. Logistic regression analysis was applied to estimate the odds ratios (ORs) of dyslipidemia with OSO. Because age and ethnicity were associated with all of these measures, we adjusted for these confounding factors in the logistic regression analysis. All analyses were performed using SPSS 16.0 (SPSS Inc., Chicago, IL) and R language software. Statistical significance was set at p < 0.05.
Results
Characteristics of the study population
The baseline characteristics of all studied populations (n = 2315) among four ethnic groups are detailed in Table 1. Compared with the younger group, the older group showed significantly lower mean value of body composition, including height, weight, BMI, FFM, FM, MM, SFC, AFM, TMM, ASM, and T-score in different ethnic groups (p < 0.05), but higher VFC, TC, and TG, and more likely to have OP and DL (p < 0.05). However, there was no significant difference in BF%, WHR, TFM, LDL-C, and HDL-C among all ethnicities (Table 1).
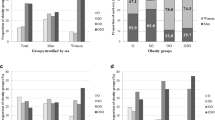
Prevalence of OSO
The prevalence of OSO in younger and older group among the four ethnic groups is shown in Figs. 1 and 2, respectively. In younger group, the incidence rates of OSO among Maonan, Mulam, and Hmong ethnicity were 0.4, 0.4, and 0.6%, respectively (Fig. 1). In older women, the incidence rates of OSO among Maonan, Mulam, and Hmong ethnicity were 4.9, 12.6, and 11.5%, respectively (Fig. 2), while there was no prevalence of OSO in Yao women in two age groups.
Comparison of BC and dyslipidemia among osteopenia/OP/sarcopenia/obesity groups
Among younger women, for the number of adverse body composition, 468 (31.88%) had none, 649 (44.21%) had one, 346 (23.57%) had two, and 5 (0.34%) had all three (OSO). In older women, it was 103 (12.16%), 287 (33.88%), 394 (46.52%), and 63 (7.44%), respectively. The prevalence of dyslipidemia in younger women was 107 (22.86%) in group 0, 194 (29.89%) in group 1, 150 (43.35%) in group 2, 4(80.00%) in group 3, respectively. The prevalence of dyslipidemia in older women was 30 (29.13%) in group 0, 112 (39.02%) in group 1, 163 (41.37%) in group 2, 33 (52.38%) in group 3, respectively.
In younger group, with an increasing number of adverse body composition, women tended to be older, less FFM, MM, TMM, ASM, HDL-C, and more likely to be dyslipidemia. In older group, those having a higher number of adverse body composition were more likely to be older, and had more BMI, FM, BF%, WHR, VFC, SFC, TFM, AFM, TC, and TG LDL-C, and had more dyslipidemia women and less FFM, MM, and ASM.
ORs from logistic regression models predicting dyslipidemia
According to the results shown in Tables 1, 2, and 3, and Figs. 1 and 2, statistically significant differences were detected in all variables among the four different ethnic groups, especially for the associations between OSO and dyslipidemia, ethnic groups, and age. Further comparison was performed in Table 4. Dyslipidemia was significantly associated with an increased adverse body composition between both younger group and older group. In younger group, the ORs for the number of adverse body composition in the development of dyslipidemia were 13.50 in the OSO group (95%CI 1.49–122.03), 2.58 in group 2 (95%CI 1.91–3.49), and 1.44 in group 1 (95%CI 1.09–1.89). After adjusting for ethnicity and age, ORs for the number of adverse body composition in the development of dyslipidemia were 12.53 in the OSO group (95%CI 1.34–116.99), 2.42 in group 2 (95%CI 1.75–3.35), and 1.37 in group 1 (95%CI 1.03–1.05). In older women, the ORs for the number of adverse body composition in the development of dyslipidemia were 2.68 in the OSO group (95%CI 1.40–5.14), 1.72 in group 2 (95%CI 1.07–2.75), and 1.56 in group 1 (95%CI 0.96–2.53). After adjusting for ethnicity and age, ORs for the number of adverse body composition in the development of dyslipidemia were 6.75 in the OSO group (95%CI3.19–14.31), 3.53 in group 2 (95%CI2.04–6.12), and 2.28 in group 1 (95%CI 1.35–3.83).
Discussion
This epidemiological survey mainly estimated the prevalence of OSO among four minorities and explored the association of OSO with dyslipidemia in different ethnic groups. Our results indicated that there was ethnic-specific prevalence of OSO and demonstrated that dyslipidemia was strongly associated with multiple adverse body composition, especially for OSO in whether younger or older age.
Although accurate case identification of sarcopenia and SO remained controversial. Sarcopenia and SO have been studied and recognized, and several representative definitions of sarcopenia and SO had already been proposed. Zoico et al. [16] defined SO as the two lower quintiles of ASM/Ht2 plus two higher quintiles of BF% and reported that the prevalence of SO was 12.4%. In addition, Jessen et al. [17] defined sarcopenia as skeletal muscle mass index (skeletal muscle mass (kg)/weight (kg) × 100) of one or two SDs below the mean for a young reference group. In our study, we used a diagnostic criteria that had been widely used in previous studies to define SO [18]. Using this diagnostic criteria, they reported that the prevalence of SO was 3.0% in women over 60 years of age in the New Mexico Aging Process Study.
OSO has recently been identified as a multifactorial condition of age-related changes in body composition, including loss of bone and muscle coexistent with increased adiposity. The diagnostic criteria are just being developed and described earlier [15]. Therefore, there are relatively few estimates for the prevalence of OSO. A study conducted in 258 overweight/obese postmenopausal women revealed that more than 12% of the women had OSO [19]. Another study conducted in 434 women over 50 years old found that 19% of participants could be diagnosed with OSO [20]. However, an analysis conducted in 2008–2010, consisting of 5980 (2485 men, 3423 women) aged over 50 years old, reported that 13.5% in men and 25% in women had OSO [21]. In our study, our findings confirmed that there was age- and ethnic-specific difference in the prevalence of OSO. In younger group, the prevalence of OSO was 0.4, 0.4, and 0.6% in Maonan, Mulam, and Hmong ethnicity, respectively. In older group, the prevalence of OSO was 4.9, 12.6, and 11.5%, respectively. However, there was no prevalence of OSO in Yao women in each age group. A reasonable explanation for the variations might be the correlation of genetic variation, environmental factors, and lifestyle factors in these four minorities. Maonan, Mulam, Yao, and Hmong were the four indigenous ethnic groups in Guangxi, China. Their ancestral allocation to different regional areas of Guangxi goes back for hundreds of years. They formed a relatively homogeneous group with regard to socioeconomic status, dietary, and occupational exposure. Moreover, these minorities had been reported to exhibit significant differences in their genetic background [8] and morphology [9]. Lifestyle factors such as dietary patterns and physical activity play a substantial role in preserving bone mass, muscle mass, and reducing obesity with age [22]. The important role of serum vitamin D level in reducing odds of OSO has been thoroughly reported previously [21]. A recent analysis of US National Health and Nutrition Examination Survey (NHANES) data shows that energy imbalance, lower long-chain polyunsaturated fatty acid intakes, lower protein intakes, and excess of carbohydrates may contribute to OSO [22]. Physical activity is needed to improve bone health, maintain muscle mass, and reduce adiposity with aging [16]. However, due to the limits of our study, we did not investigate the lifestyle factors, and genetic and environmental status of the ethnic group that might affect the prevalence of OSO. In addition, ethnic-specific differences in the prevalence of OSO, its consequences, and pathogenesis were largely unknown. The carrying out of further studies addressing these factors should be advocated to better understand the differences in the prevalence of OSO among ethnic groups and minorities.
Dyslipidemia was significantly associated with multiple adverse body composition, especially for OSO group in younger and older women among four minorities. After adjusting for age and ethnicity, OSO group was 12.53 and 6.75 times more likely to have dyslipidemia compared with normal women in younger and older group, respectively. To our knowledge, few study had demonstrated the significant association between dyslipidemia and multiple adverse body composition in minorities.
Numerous studies had also investigated the relationship between dyslipidemia and individual composition (low bone mass, low muscle mass, or obesity). A study involving 6300 South Koreans from 2008 to 2010 showed that bone mineral density was inversely correlated with dyslipidemia [23]. Besides, sarcopenia was known to be positively associated with metabolic syndrome including dyslipidemia [24]. A strong relationship between obesity and dyslipidemia had also been reported in a qualitative systematic review among Koreans [25].
However, relatively few studies had examined the relationship between dyslipidemia and combined indices of body composition [7, 26, 27]. Baek et al. [27] found that SO was more strongly associated with dyslipidemia than sarcopenia and obesity alone. Besides, Lu et al. [26] used bioimpedance analysis and demonstrated that those in the combined group with loss of muscle mass and increased of fat mass had a higher risk for abnormal lipid metabolism than those in the sarcopenic or obese groups.
The possible mechanism of dyslipidemia in the bone, muscle, and body fat has been suggested as follows: (1) Oxidized LDL-C suppressed the differentiation of bone marrow stromal cells to osteoblasts, which may result in bone mass reduction [28]. (2) The loss of muscle mass decreased muscle glycogen synthesis, accelerating insulin resistance in skeletal muscle. The insulin resistance played a key role in the pathogenesis of the metabolic syndrome and atherogenic dyslipidemia by diverting energy derived from ingested carbohydrate away from muscle glycogen synthesis into increased hepatic de novo lipogenesis [29]. (3) Increasing fat mass elevated the levels of inflammatory cytokines such as IL-6 and TNF-a, which might also induce insulin resistance and TG infiltration into the muscle [29]. Further research was necessary for better understanding of the pathogenesis.
Our study has several limitations that must be considered. First, the cross-sectional nature of this study did not allow us to identify causal relationships of the observed associations for which prospective data were needed. Second, it is very difficult to recruit a sufficient number of participants because of the four minority groups scattered in remote mountainous areas, and the statistical power may be limited in some of the analyses. Besides, the European Working Group on Sarcopenia in Older People (EWGSOP) recommends using the documentation of both low muscle mass and low muscle function (strength or performance) for the diagnosis of sarcopenia [30]. However, the definition of sarcopenia in our study only referred to muscle mass, because the majority diagnostic thresholds for sarcopenia have been developed on muscle mass. In future studies, we can evaluate muscle function in addition to muscle mass for better understanding age-related associations OSO and dyslipidemia.
Conclusions
In summary, this study comprehensively examined the age- and ethnic-specific prevalence of OSO among Maonan, Mulam, Yao, and Hmong women. Furthermore, our results showed that dyslipidemia was significantly associated with multiple adverse body composition, especially for OSO group in younger and older women in four minorities. Ultimately, optimal strategies may be developed to maintain bone mass or minimize bone loss and strengthen the prevention of obesity in older adults in different populations and to effectively reduce the burden of OSO in the growing elderly population in China.
References
Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP (2001) The continuing epidemics of obesity and diabetes in the United States. Jama 286:1195–1200
Nikolich-Žugich J (2012) The aging immune system: challenges for the 21st century. Semin Immunol 24:301–302
Tao Y, Yu J, Tao Y, Pang H, Yu Y, Yu Y, Jin L (2016) Comparison of the combined obesity indices to predict cardiovascular diseases risk factors and metabolic syndrome in Northeast China. Int J Environ Res Public Health 13:801
Ormsbee MJ, Prado CM, Ilich JZ, Purcell S, Siervo M, Folsom A, Panton L (2014) Osteosarcopenic obesity: the role of bone, muscle, and fat on health. J Cachexia Sarcopenia Muscle 5:183–192
Cooper C, Dere W, Evans W et al (2012) Frailty and sarcopenia: definitions and outcome parameters. Osteoporos Int 23:1839–1848
Bijlsma AY, Meskers CG, Westendorp RG, Maier AB (2012) Chronology of age-related disease definitions: osteoporosis and sarcopenia. Ageing Res Rev 11:320–324
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, Kim KW, Lim JY, Park KS, Jang HC (2010) Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care 33:1652–1654
Deng Q, Xu L, Gong J, Zhou L, Li S, Deng X, Luo G, Xie X (2007) Genetic relationships among four minorities in Guangxi revealed by analysis of 15 STRs. J Genet Genomics 34:1072–1079
Du R (2004) Population genetics in China. Science Press, Beijing
Saadi H, Reed R, Carter A, Qazaq H, Al-Suhaili A (2001) Bone density estimates and risk factors for osteoporosis in young women. East Mediterr Health J 7:730–737
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int 4:368–381
guide jcoCadp (2007) Chinese adult dyslipidemia prevention guide. Journal of Chinese Cardiology 35:390–419
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR (2013) Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: the Framingham Study. The journals of gerontology Series A, Biological sciences and medical. sciences 68:168–174
Ilich JZ, Kelly OJ, Inglis JE, Panton LB, Duque G, Ormsbee MJ (2014) Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res Rev 15:51–60
Kelly OJ, Gilman JC (2017) Can unconventional exercise be helpful in the treatment, management and prevention of osteosarcopenic obesity? Curr Aging Sci 10:106–121
Janssen I, Heymsfield SB, Ross R (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 50:889–896
Baumgartner RN (2000) Body composition in healthy aging. Ann N Y Acad Sci 904:437–448
Ilich JZ, Inglis JE, Kelly OJ, McGee DL (2015) Osteosarcopenic obesity is associated with reduced handgrip strength, walking abilities, and balance in postmenopausal women. Osteoporos Int 26:2587–2595
Szlejf C, Parra-Rodriguez L, Rosas-Carrasco O (2017) Osteosarcopenic obesity: prevalence and relation with frailty and physical performance in middle-aged and older women. J Am Med Dir Assoc 18:733 e731–733 e735
Kim J, Lee Y, Kye S, Chung YS, Lee O (2017) Association of serum vitamin D with osteosarcopenic obesity: Korea National Health and Nutrition Examination Survey 2008–2010. J Cachexia Sarcopenia Muscle 8:259–266
Kelly OJ, Gilman JC, Kim Y, Ilich JZ (2016) Micronutrient intake in the etiology, prevention and treatment of osteosarcopenic obesity. Curr Aging Sci 9:260–278
Kim YH, Nam GE, Cho KH, Choi YS, Kim SM, Han BD, Han KD, Lee KS, Park CH, Kim DH (2013) Low bone mineral density is associated with dyslipidemia in South Korean men: the 2008–2010 Korean National Health and Nutrition Examination Survey. Endocr J 60:1179–1189
Ishii S, Tanaka T, Akishita M, Ouchi Y, Tuji T, Iijima K, Kashiwa study i (2014) Metabolic syndrome, sarcopenia and role of sex and age: cross-sectional analysis of Kashiwa cohort study. PLoS One 9:e112718
Kang YJ, Wang HW, Cheon SY, Lee HJ, Hwang KM, Yoon HS (2016) Associations of obesity and dyslipidemia with intake of sodium, fat, and sugar among Koreans: a qualitative systematic review. Clin Nutr Res 5:290–304
Lu CW, Yang KC, Chang HH, Lee LT, Chen CY, Huang KC (2013) Sarcopenic obesity is closely associated with metabolic syndrome. Obes Res Clin Pract 7:e301–e307
Baek SJ, Nam GE, Han KD, Choi SW, Jung SW, Bok AR, Kim YH, Lee KS, Han BD, Kim DH (2014) Sarcopenia and sarcopenic obesity and their association with dyslipidemia in Korean elderly men: the 2008–2010 Korea National Health and Nutrition Examination Survey. J Endocrinol Investig 37:247–260
Yamaguchi T (2011) Bone metabolism in dyslipidemia and metabolic syndrome. Clin Calcium 21:677–682
Petersen KF, Dufour S, Savage DB et al (2007) The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci U S A 104:12587–12594
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39:412–423
Acknowledgments
We thank the participants and relevant research staff for their contributions to the survey.
Funding
This work was supported by grants from the National Science Foundation of China (No. 31160222).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Written informed consent was obtained from all participants in this cross-sectional study, which has been supported by the National Natural Science Foundation of China and given approval by the Institution Review Board for studies using human subjects. Ethical approval was given by the medical ethics committee of Guangxi Medical University.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Mo, D., Hsieh, P., Yu, H. et al. Osteosarcopenic obesity and its relationship with dyslipidemia in women from different ethnic groups of China. Arch Osteoporos 13, 65 (2018). https://doi.org/10.1007/s11657-018-0481-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0481-1