Abstract
Summary
Younger adults and males had a higher prevalence of vitamin D deficiency compared to older participants and females. Low intake of milk, central obesity, and lack of use of vitamin D supplements were associated with vitamin D deficiency, highlighting potentially important avenues for preventive intervention.
Background
Vitamin D deficiency is a public health concern. This study’s objective was to measure the prevalence of vitamin D deficiency and determine its correlates among Saudi adults in Riyadh, Saudi Arabia.
Methods
A cross-sectional study was conducted with 2835 Saudi males and females aged 30–75 years in 18 different primary health care centers (PHCC) in Riyadh. Detailed interviews on sociodemographic and lifestyle factors and anthropometric measurements were conducted. Serum calcium, phosphorus, parathyroid, alkaline phosphatase, and 25(OH) vitamin D were measured. Multiple logistic regression analyses were conducted.
Results
The mean age (SD) of male and female participants was 43.0 (± 11.7) and 42.8 (± 10.3) years, respectively. Serum 25(OH) vitamin D assays for participants revealed that 72.0% (n = 695) of males and 64.0% (n = 1191) of females had levels < 50 nmol/L (deficiency), whereas 17.3% (n = 166) and 19.4% (n = 362), respectively, had levels of 50–75 nmol/L (insufficiency). Multivariate analyses for males revealed that lack of use of vitamin D supplements [adjusted odds ratio (aOR) = 4.0, 95% CI 1.7, 9.4], younger age [30–40 years aOR = 3.6, 95% CI 1.7, 7.3 and 41–50 years aOR = 4.2, 95% CI 2.0, 8.8], low milk intake [aOR = 1.7, 95% CI 1.0, 2.8], consumption of cola drinks [aOR = 2.0, 95% CI 1.1, 3.9], and central obesity [aOR = 1.8, 95% CI 1.0, 3.4] were associated with low vitamin D. In females, lack of use of vitamin D supplements [aOR = 3.7, 95% CI 2.8, 4.9], younger age [30–40 years aOR = 3.4, 95% CI 2.0, 5.8 and 41–50 years aOR = 2.8, 95% CI 1.6, 4.7], central obesity [aOR = 1.4, 95% CI 1.0, 2.2], and seasonal variation [aOR = 1.6, 95% CI 1.3, 2.1] had higher odds for vitamin D deficiency. Significantly lower levels were observed for men than women for mean serum 25(OH) vitamin D [42.6 (± 24.1) vs. 46.8 (± 30.5)], parathyroid hormone [5.3 (± 2.9) vs. 5.9 (± 2.7)], and phosphorus [1.1 (± 0.2) vs. 1.2 (± 0.2)], respectively; alkaline phosphatase levels [106 (± 32.8) vs. 99 (± 27.8)] [p < 0.01] were significantly higher in males than females.
Conclusion
Vitamin D deficiency was highly prevalent, particularly among young adults and those with central obesity. Proper fortification policy, health education, and regular screening PHCCs may help prevent and treat vitamin D deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hypovitaminosis D (vitamin D deficiency) is an established international and national public health concern [1,2,3]. A review by Mithal et al. found that individuals in almost all regions of the world are suffering from vitamin D deficiency (25-hydroxy vitamin D (25(OH)D) < 75 nmol/L); however, extreme deficiency (< 25 nmol/L) was highly prevalent in regions of South Asia and the Middle East [4]. A recent study from United Arab Emirates (UAE) found that 82.5% of patients had vitamin D deficiency/insufficiency (≥ 25–< 75 nmol/L), with 26.4% of females and 18.4% of males exhibiting severe deficiency (< 25 nmol/L) [1].
Small and large studies from Saudi Arabia have found that the prevalence of vitamin D deficiency ranged from 40% to more than 80% among the Saudi adult population [5,6,7,8,9]. Traditionally, age and gender comparison studies have found that elderly females are at higher risk than males for vitamin D deficiency [5,6,7,8]. However, recently, inconsistent results have been reported on prevalence of vitamin D deficiency with respect to age and gender [1, 9,10,11].
Several factors, such as obesity, low sun exposure, low physical activity, low socioeconomic status, lack of use of vitamin D supplements, and smoking have been associated with vitamin D deficiency [5,6,7,8]. Vitamin D deficiency is thus potentially preventable, and it is important to recognize it in a timely manner, as associations of vitamin D deficiency have been found with several adverse health conditions, including bone problems, chronic diseases, and cancers [12,13,14]. Adequate intake of dietary dairy products, liver, eggs, and vitamin D-fortified products can help reduce vitamin D deficiency, as they are good sources for vitamin D [3, 4].
Despite increased awareness, especially among females, the prevalence of vitamin D deficiency remains high [5,6,7,8]. Inadequate information is available on the prevalence and factors related to vitamin D deficiency and gender differences in the adult population in Saudi Arabia. The recent inconsistent findings and limited community-based studies impelled us to design a study to measure the prevalence and gender-specific correlates of vitamin D deficiency among Saudi adults (aged 30–75 years) in Riyadh, Saudi Arabia.
Methodology
Study design and setting
This study was part of a large cross-sectional survey (Women in Saudi Arabia Health Examination Survey, WISHES) to measure the prevalence, severity, and factors associated with chronic diseases (cardiovascular diseases, vitamin D deficiency, obesity) in males and females aged 30–75 years in Riyadh, Saudi Arabia. Data were collected from December 2014 to August 2015, and analysis performed during August/September 2016. Riyadh has 105 primary health care centers (PHCCs), out of which, 18 PHCCs were randomly selected from the five administrative regions of Riyadh. In addition, five Government institutions (technical institutes, college/university, and social organizations) were selected to identify and enroll eligible participants.
Study participants
Saudi adults between 30 and 75 years of age and permanent residents of Riyadh were eligible to participate in the WISHES study. Non-Saudis, pregnant women, and those with gross mental incapacity were not included in the study. Multiple strategies were adopted to invite the participants. These included placing advertisements at the selected PHCCs and at the nearest major shopping malls, distributing invitation pamphlets among patients/attendants, and making announcements through the local mosque.
In total, 3100 adults (1000 males and 2100 females) were invited to participate, out of those, 968 males and 2029 females fulfilled the eligibility criteria and provided signed informed consent. Further, 165 participants were excluded because they had osteoporosis and were being treated; hence, finally, 2832 (males = 962, females =1870) were included in the final analyses. The number of male participants was low as compared to females, because the morning timing of the study coincided with the office timings. We tried to overcome this by visiting and enrolling participants from Government offices. The study protocol was approved by the Institutional Review Board, King Saud University (E-12-658) and the Institutional Review Board of the Ministry of Health (MOH), Dammam (IRB ID MOH0151).
Questionnaire-based interviews
Detailed interview, including sociodemographic characteristics, common dietary habits, sun exposure, and reproductive history (from females only), were conducted with each of the participants. Sociodemographic information included age, marital status, education, occupation, housing type, and income. Information on dietary items was collected using a food frequency questionnaire, which included frequency of consumption on a daily, weekly, or monthly basis. Sun exposure was determined by asking information on number of days/week exposed to sun, the average duration of exposure, and timing of exposure during the day. The International Physical Activity questionnaire (IPAQ, short form) was used to measure physical activity [15]. The IPAQ is a validated questionnaire and measures physical activity as low, moderate, and vigorous intensity level. It includes both the frequency and the time spent doing that activity.
Measurement of serum 25(OH)D, parathyroid hormone, calcium, phosphorus, and alkaline phosphatase
To determine serum 25(OH) vitamin D, calcium, phosphorus, parathyroid hormone, and alkaline phosphatase concentrations, 3–5 ml of blood was obtained from each participant by venipuncture collected in specific test tubes. The specimens were then centrifuged, and serum was collected. All samples were tested at King Khalid University hospital laboratory.
Serum 25(OH) vitamin D levels were measured using electro-chemiluminiscence (ECLIA immunoassay, Modular Analytics E170, Roche Diagnostics GmbH, Mannheim, Germany). The Endocrine Society defines vitamin D deficiency as serum 25(OH)D levels of < 50 nmol/l and insufficiency as ≥ 50 ≤ 75 nmol/L [16]. Serum parathyroid hormone (PTH) was measured in picomoles per liter by a sandwich assay based on electrochemiluminescence immunoassay (ECLIA) using the Roche Elecsys analyzer. Serum calcium levels (corrected for albumin binding) were measured in millimoles per liter by using o-cresolphthalein complexone (OCPC) reagent. Calcium reacts with this reagent to form a purple Calcium-OCPC complex which was measured spectrophotometrically using a bichromatic (577, 540 nm) endpoint technique. Serum phosphorus levels were measured in millimoles per liter by using a molybdate reagent. Inorganic phosphate combines with molybdate (MoO4) in an acid solution to form a complex which is reduced by p-methylaminophenol sulfate (PMAPS) and bisulfite. Reduced phosphomolybdate solution absorbs at 340 nm and is proportional to the inorganic phosphorus concentration and was measured spectrophotometrically using a bichromatic (340, 383 nm) endpoint technique. Serum alkaline phosphatase (ALP) levels were measured in units per liter (U/L) by using a p-nitrophenyphosphate (p-NPP) substrate reagent which is catalyzed by alkaline phosphatase in a transphosphorylation reaction to p-nitrophenol (p-NP). The change in absorbance at 405 nm due to formation of p-NP is directly proportional to the ALP activity. The serum was run on the Siemens StreamLab RxL Max clinical chemistry analyzer for measuring calcium, phosphorus, and alkaline phosphatase.
Anthropometric measurements
A standard protocol was followed to measure the anthropometric indices, which included weight, measured with an electronic scale (Seca 220—Hamburg, Germany, 2009), and height measured with a meter scale [17]. Body mass index (BMI) was computed as weight in kg/(height in m)2. Waist circumference (WC), to determine central obesity, was measured at the mid-point between the lowest rib and top of the hip bone (iliac crest) [18].
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences software package (IBM SPSS statistics version 21.0). Means and standard deviations were computed for continuous variables, and proportions were calculated for categorical variables. The food frequency questionnaire included responses on a daily, weekly, or monthly basis. Pearson correlation coefficients (r) were measured between 25(OH) vitamin D levels and serum calcium, parathyroid, phosphorus, and alkaline phosphatase levels. The outcome variable (serum vitamin D level) was evaluated as a dichotomous variable with normal participants being those having vitamin D ≥ 75 nmol/L (coded 0) vs. insufficient/deficient considered as hypovitaminosis D (having vitamin D < 75 nmol/L and coded as 1). The level of statistical significance was set at p < 0.05. Potential confounding factors were identified based on biological plausibility and statistical significance of their association with the outcome. In addition, the variables changing the estimates more than 10% or resulting in a significant change in the log likelihood ratio were retained in the final model. All plausible interactions were checked before developing the final model. Multiple logistic regression modeling was performed using the ENTER method to explore the independent relationships between hypothesized variables, providing adjusted odds ratios (aOR) and 95% confidence intervals (CI) for the associations. The Hosmer-Lemeshow goodness of fit test was used to assess model fit.
Results
The mean age of the participants was 42.9 (± 10.8) years. No significant difference was observed in the mean age (SD) of male and female participants [43.0 (± 11.7) and 42.8 (± 10.3) years, respectively (p = 0.5)]. The majority of the participants (89% of males and 92% of females) were married. A considerable proportion of males (64%) were working as secretaries, teachers, or office staff, whereas 50% of females were house-wives (Table 1). More than half of the females had > 5 children, and 15% (n = 420) were postmenopausal (results not shown). Over a quarter (27.7%, n = 266) of males and 2.0% (n = 41) females were current smokers. The mean (SD) waist circumferences for males and females were 96.2 (± 14.2) and 92.2 (± 14.0) cm, respectively (p < 0.001). Keeping the cut-off as > 90 cm for males and > 80 cm for females, 56% (537) and 82% (1544), respectively, had central obesity (Table 1). The mean (±SD) BMIs for males and females were 29.6 (± 6.4) and 31.4 (± 6.5), respectively.
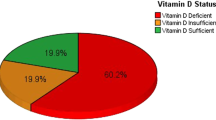
Most male (89%, n = 861) and female (82%, n = 1553) participants were categorized as having hypovitaminosis D (insufficient plus deficient < 75 nmol/L) (Fig. 1). Serum 25(OH) vitamin D levels were deficient (< 50 nmol/L) for the majority of males and females [72.0% (n = 695) and 64.0% (n = 1191)], respectively, whereas 17.3% (n = 166) and 19.4% (n = 362), respectively, were insufficient (50–75 nmol/L). More males than females (49.7% vs. 36.3) had levels ≥ 25 to < 50 nmol/L, whereas a higher percentage of females than males had very low vitamin D (< 25 nmol/L) levels (22.6 vs. 27.4) (Fig. 1).
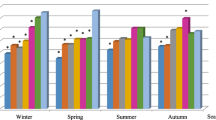
The majority of participants (> 50% males and > 60% females) did not expose themselves to direct sunlight in summer or winter. Among those who were exposed, exposure was mostly for few days per week and for 15 min or less per day (results not shown). Significant variation was observed for mean vitamin D levels (42.3 (± 27.8) vs. 48.5 (± 28.9), p < 0.001) between blood samples collected during winter (December–February) vs. those collected during summer (March–June) (Fig. 2). The mean serum vitamin D levels for males during summer and winter were 41.5 (± 24.3) nmol/L vs. 43.7 (± 23.8) nmol/L (p = 0.15), respectively, and for females, they were 42.7 (± 29.4) vs. 51.2 (± 31.0) (p < 0.001), respectively. Only 36 (3.7%) males and 429 (21.0%) females were taking some form of vitamin D supplements.
On average, males reported more frequent intake of milk than did females (6 days/week vs. 5 days/week, p < 0.01) (Table 2). In addition, the males reported consuming a higher quantity of milk intake than did females (350 vs. 250 ml, p < 0.001). The average amount of reported consumption of cola drinks per day was also higher in males than in females (375 vs. 250 ml, p < 0.05).
The multivariate logistic regression model for Saudi males revealed that younger age groups [ages 30–40 years aOR = 3.6, 95% CI 1.7, 7.3 and 41–50 years aOR = 4.2, 95% CI 2.0, 8.8] compared to those > 60 years of age, not taking vitamin D supplements [aOR = 4.0, 95% CI 1.7, 9.4], central obesity [aOR = 1.8, 95% CI 1.0, 3.4] vs. normal waist circumference, infrequent milk intake [weekly aOR = 1.7, 95% CI 1.0, 2.8 and monthly aOR = 1.8, 95% CI 1.0, 3.3] vs. daily milk intake, and daily consumption of cola drinks [aOR = 2.0, 95% CI 1.1, 3.9] vs. monthly intake had higher odds for vitamin D deficiency. The model was adjusted for type of housing and seasonal variation (Table 3).
The multivariate final model for Saudi females revealed that younger age categories [30–40 years aOR = 3.4, 95% CI 2.0, 5.8 and 41–50 years aOR = 2.8, 95% CI 1.6, 4.7] vs. those aged > 60 years, not taking vitamin D supplements [aOR = 3.7, 95% CI 2.8, 4.9], central obesity [aOR = 1.4, 95% CI 1.0, 2.2] vs. normal waist circumference, seasonal variation [aOR = 1.6, 95% CI 1.3, 2.1], living in apartments (aOR = 1.8, 95% CI 1.1, 2.8) and Arabic type or small house (aOR = 1.6, 95% CI 1.1, 2.3) had higher odds for vitamin D deficiency (Table 4).
Significant differences between males and females were observed in the mean (±SD) values for serum 25(OH) vitamin D, calcium, phosphorus, alkaline phosphatase, and parathyroid hormone levels (p < 0.001) (Table 5). Pearson correlation coefficients revealed that 25(OH) vitamin D levels were positively correlated with calcium in males and females (r = 0.11 and 0.15, respectively, p < 0.001) and negatively correlated with parathyroid hormone (− 0.20 and − 0.26, respectively, p < 0.001). Phosphorus levels were weakly positively correlated with 25(OH) vitamin D only in females (r = 0.08, p < 0.001). No significant correlation was observed between 25(OH) vitamin D levels and alkaline phosphatase in either males or females (p = 0.8).
Discussion
This study has not only identified a high prevalence of vitamin D deficiency (85%, n = 2414) among the adult Saudi population but has also found that younger adult (78% were in the age group of 30 to 50 years) and males (72.0% vs. 64.0%) had a higher prevalence when compared to older and female participants. Several reasons could explain the increased prevalence of vitamin D deficiency in young male adults. First, the Saudi males usually remain indoors due to their job commitments and lifestyle and avoid sun exposure due to extreme temperatures [5,6,7,8]. Second, the majority of the males do not visit the PHCC regularly, and do not have any workplace screening or health education programs available to screen, detect, and treat vitamin D deficiency in a timely manner. In fact, a large proportion of young healthy male adult participants (n = 816, 87%) were unaware of their vitamin D status when identified as deficient by this study. In addition, 107 out of 146 males (74.0%), who despite being diagnosed as vitamin D deficient in the past, had low vitamin D levels measured in the present study. Hence, the public needs to be educated about proper screening, prevention, and potential health complications due to vitamin D deficiency. In addition, non-compliance by the patient or taking an insufficient dosage of a vitamin D supplement may also lead to continuous deficiency.
Vitamin D supplements are a reliable, cheap, and convenient method to prevent vitamin D deficiency [4,5,6,7]. In comparison to males, older females had a lower prevalence, probably due to the successful initiatives by the Ministry of Health in creating awareness among the elderly, especially at the PHCC level. The Ministry of Health strongly recommends prophylactic 25(OH) vitamin D and calcium supplements for all females (especially ≥ 40 years of age), and it seems that they have been partially successful as 27% of females were taking vitamin D supplements. Even though vitamin D supplements are freely available at all the PHCCs in Saudi Arabia, only a small percentage of males (3.7%) were taking these supplements. Hence, we strongly recommend that along with females, similar rigorous efforts should target the adult male population as well.
Previous studies have identified the role of sedentary life style, sun exposure, obesity, and lack of dietary supplements and its association with vitamin D deficiency; however, results have varied due to social and cultural differences [4, 6, 7, 19]. Although physical inactivity was not directly associated with the deficiency in our study, associations of vitamin D deficiency in this study with factors such as central obesity (which may reflect physical inactivity), cola drinks, inadequate sun exposure, infrequent milk intake, and inadequate intake of supplements highlight the importance of these factors with respect to 25(OH) vitamin D levels. Milk and other dairy products, if fortified with 25(OH) vitamin D, are considered a good source for vitamin D [4]; however, in the majority of cases, the dairy fortification is not adequate and does not fulfill the daily recommended quantity. A study by Sedat et al. found inadequate fortification of milk with 25(OH) vitamin D in Saudi Arabia, which may be the reason for persistent vitamin D deficiency (a liter of milk contains 40 IU of vitamin D3, which is around 15% of the daily requirement) [20]. Proper fortification of milk, dairy products, and juices, in addition to nutrition education, can help in reducing the vitamin D deficiency [20]. We did not find a significant association with milk intake in females, which may be because of differences in the type of milk consumed (skimmed, low fat, etc.). Sea-food (salmon, sardines, and canned tuna fish) and fish oil are also considered a rich source for 25(OH) vitamin D; however, we did not find a significant association between fish intake and vitamin D deficiency. This may be because only about 20.0% of participants reported consuming fish on a weekly basis, and the majority (80.0%) were consuming it only on a monthly basis; a negligible percentage (≤ 2.0%) were consuming it on a daily basis.
Recently, association between 25(OH) vitamin D levels and cola drinks/sweet beverages has been explored [21]. Our results are in support of animal and human studies showing an association between sugar-sweetened beverages (including colas, other carbonated drinks, and sweet fruit drinks) and decreased plasma 25(OH) vitamin D levels [21, 22]. About 40% of males and 30% of females in our study reported drinking cola drinks (Pepsi and Coca-Cola) on a daily or weekly basis. Cola drinks may contribute to 25(OH) vitamin D deficiency by two pathways. First, it is hypothesized that constituents, such as fructose, caffeine, and phosphoric acid may be responsible for decreasing the absorption of 25(OH) vitamin D levels available through dietary sources [21, 22]. We observed a negative but weak correlation between number of cans of cola drinks consumed and 25(OH) vitamin D levels (r = − 0.06, p = 0.01). Secondly, intake of unhealthy foods, such as sugar-sweetened cola, and other drinks can lead to an increase in calories consumed and thus weight gain [23, 24]. Overweight and obese individuals have higher rates of vitamin D deficiency compared to normal weight individuals [23, 24]. Ardawi et al. found that serum 25(OH) vitamin D was lower (p < 0.001) in individuals in the upper quintiles of body mass index and waist-to-hip ratio (WHR) [6, 7]. The association can be explained based on the sequestering effect of a high quantity of subcutaneous fat, which leads to reduced circulating 25(OH) vitamin D levels [25, 26]. With the increasing prevalence of obesity among the Saudi population [27], it is important to track serum 25(OH) vitamin D levels at regular intervals.
Results for seasonal variation in serum 25(OH) vitamin D levels were similar to those from previously conducted studies in Saudi Arabia and the United Arab Emirates, [28, 29]; however, results from countries other than Middle East are in contradiction [30, 31]. The participants in our study whose samples were collected during the winter months (December–March) had higher mean levels for 25(OH)D than those whose samples were collected during summer (April–August). A probable reason for this inverse trend may be avoidance of sunlight during the summer season due to intense sunrays and hot temperatures in Saudi Arabia. In addition, the Saudi tradition is for both males and females to cover the whole body with clothing. Sun exposure is the best source for vitamin D; however, 52% of males and 67% of females in our study reported no sun exposure. Both timing and duration of exposure are also important factors [32]. The recommended appropriate time is 8.00 am–4:00 pm [32], whereas in our study, the majority participants reported sun exposure before 10:00 am. During the winter, only 26% of males and 30% of females (results not shown) reported sun exposure according to the recommended optimum time (10;00 am to 2:00 pm) [32].
Inconsistent findings have been reported for the association between socioeconomic status (SES) and 25(OH)D levels [33, 34]. Sixteen percent of our female participants were not sure about their monthly income; hence, type of housing was used as a proxy indicator for socioeconomic status. The participants who were living in villas had an average monthly income of ≥ 10,000 SAR (US$ 2666), whereas those living in apartments and Arabic/small house had monthly incomes < 10,000. In addition, a significant but weak correlation was found between income level and 25(OH) vitamin D levels [r = 0.09, p < 0.001]. Previous studies have reported low levels of education (another proxy indicator used to determine SES status) associated with low 25(OH)D levels [3, 6, 7]; however, we did not find any significant association with education level.
Among the various bone markers, serum calcium, parathyroid, and phosphorus levels acquire an important position because of their significant association with varying levels of 25(OH) vitamin D levels [35]. The mean levels in our study differed significantly between males and females, suggesting gender differences in the physiological make-up along with the roles of various other known and unknown factors. Similar to results from other studies [36, 37], we did not find a significant association between 25(OH) vitamin D and alkaline phosphatase, questioning the role of alkaline phosphatase in predicting vitamin D levels.
The present study was conducted on a sample of the Saudi population that included adults from a wide age range (30–75 years) and from different socioeconomic and educational levels, thus improving the generalizability of the results. However, our study had some limitations. The information on sun exposure, diet, and physical activity were based on subjective responses and were not validated; therefore, information/reporting bias cannot be ruled out. Also, this was a cross-sectional study so that temporal relations and causality could not be established.
Conclusion
National awareness campaigns directed to young males and females are required to educate Saudis about the best ways to improve and maintain 25(OH) vitamin D levels. Vitamin D supplements, adequate sun exposure, and physical activity are important factors to avoid low 25(OH) vitamin D levels. The Ministry of Health should take strong measures for adequate fortification of common food items in the Kingdom as well as educational programs to promote adequate Vitamin D intake and to prevent Vitamin D deficiency.
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available because it includes personal information of the participants but are available from the corresponding author on reasonable request.
References
Haq A, Svobodová J, Imran S, Stanford C, Razzaque MS (2016) Vitamin D deficiency: a single centre analysis of patients from 136 countries. J Steroid Biochem Mol Biol 164:209–213
Tuffaha M, El Bcheraoui C, Daoud F, Al Hussaini HA, Alamri F, Al Saeedi M et al (2015) Deficiencies under plenty of sun: vitamin D status among adults in the Kingdom of Saudi Arabia, 2013. N Am J Med Sci 7:467–475
Fields J, Trivedi NJ, Horton E, Mechanick JI (2011) Vitamin D in the Persian Gulf: integrative physiology and socioeconomic factors. Curr Osteoporos Rep 9(4):243–250
Mithal A, Wahl DA, Bonjour JP, Burckhardt P, Dawson-Hughes B, Eisman JA, IOF Committee of Scientific Advisors (CSA) Nutrition Working Group et al (2009) Global vitamin D status and determinants of hypovitaminosis D. Osteoporos Int 20:1807–1820
Hussain AN, Alkhenizan AH, El Shaker M, Raef H, Gabr A (2014) Increasing trends and significance of hypovitaminosis D: a population-based study in the Kingdom of Saudi Arabia. Arch Osteoporos 9:190
Ardawi MS, Qari MH, Rouzi AA, Maimani AA, Raddadi RM (2011) Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre- and postmenopausal women. Osteoporos Int 22:463–475
Ardawi MS, Sibiany AM, Bakhsh TM, Qari MH, Maimani AA (2012) High prevalence of vitamin D deficiency among healthy Saudi Arabian men: relationship to bone mineral density, parathyroid hormone, bone turnover markers, and lifestyle factors. Osteoporos Int 23:675–686
Alsuwadia AO, Farag YM, Al Sayyari AA, Mousa DH, Alhejaili FF, Al-Harbi AS et al (2013) Prevalence of vitamin D deficiency in Saudi adults. Saudi Med J 34:814–818
Alfawaz H, Tamim H, Alharbi S, Aljaser S, Tamimi W (2014) Vitamin D status among patients visiting a tertiary care center in Riyadh, Saudi Arabia: a retrospective review of 3475 cases. BMC Public Health 14:159
Kanan RM, Al Saleh YM, Fakhoury HM, Adham M, Aljaser S, Tamimi W (2013) Year-round vitamin D deficiency among Saudi female out-patients. Public Health Nutr 16:544–548
Sadat-Ali M, Al Elq AH, Al-Turki HA, Al-Mulhim FA, Al-Ali AK (2011) Influence of vitamin D levels on bone mineral density and osteoporosis. Ann Saudi Med 31:602–608
Basit S (2013) Vitamin D in health and disease: a literature review. Br J Biomed Sci 70:161–172
Wacker M, Holick MF (2013) Vitamin D—effects on skeletal and extraskeletal health and the need for supplementation. Nutrients 5:111–148
Nabi G, Hobani Y, Sarwat M (2015) High prevalence of vitamin D deficiency and cancer in Saudi Arabian populations: can we hypothesize a link? Med Hypotheses 85:117–119
Lee PH, Macfarlane DJ, Lam TH, Stewart SM (2011) Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act 8:115. https://doi.org/10.1186/1479-5868-8-115
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Endocrine Society et al (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930
National Health and Nutrition Examination Survey (NHANES). Anthropometry procedure manual. Accessed on January 2014 at https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf
World Health Organization (2008) Waist circumference and waist-hip ratio report of a WHO expert consultation Geneva, 8–11 December 2008. Available http://apps.who.int/iris/bitstream/10665/44583/1/9789241501491_eng.pdf
Soininen S, Eloranta AM, Lindi V, Venäläinen T, Zaproudina N, Mahonen A, Lakka TA (2016) Determinants of serum 25-hydroxyvitamin D concentration in Finnish children: the Physical Activity and Nutrition in Children (PANIC) study. Br J Nutr 115:1080–1091
Sadat-Ali M, Al Elq A, Al-Farhan M, Sadat NA (2013) Fortification with vitamin D: comparative study in the Saudi Arabian and US markets. J Fam Commun Med 20:49–52
Olson ML, Maalouf NM, Oden JD, White PC, Hutchison MR (2012) Vitamin D deficiency in obese children and its relationship to glucose homeostasis. J Clin Endocrinol Metab 97:279–285
Karonova T, Belyaeva O, Jude EB, Tsiberkin A, Andreeva A, Grineva E et al (2016) Serum 25(OH)D and adipokines levels in people with abdominal obesity. J Steroid Biochem Mol Biol
Abbas MA (2016) Physiological functions of Vitamin D in adipose tissue. J Steroid Biochem Mol Biol
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72(3):690–693
Al-Quwaidhi AJ, Pearce MS, Critchley JA, Sobngwi E, O’Flaherty M (2014) Trends and future projections of the prevalence of adult obesity in Saudi Arabia, 1992-2022. East Mediterr Health J 20:589–595
Duchaine CS, Diorio C (2014) Association between intake of sugar-sweetened beverages and circulating 25-hydroxyvitamin D concentration among premenopausal women. Nutrients 6:2987–2999
García-Contreras F, Paniagua R, Avila-Díaz M, Cabrera-Muñoz L, Martínez-Muñiz I, Foyo-Niembro E, Amato D (2000) Cola beverage consumption induces bone mineralization reduction in ovariectomized rats. Arch Med Res 31:360–365
Al Anouti F, Thomas J, Abdel-Wareth L, Rajah J, Grant WB, Haq A (2011) Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermatoendocrinology 3:235–239
Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, El-Kholie E, Yousef M et al (2012) Increased vitamin D supplementation recommended during summer season in the gulf region: a counterintuitive seasonal effect in vitamin D levels in adult, overweight and obese Middle Eastern residents. Clin Endocrinol (Oxf) 76:346–350
Jing C, Yun C, He Y, Piao J, Yang L, Yang X (2017) Vitamin D status among the elderly Chinese population: a cross-sectional analysis of the 2010-2013 China National Nutrition and Health Survey (CNNHS). Nutr J 16:3
Schleicher RL, Sternberg MR, Looker AC, Yetley EA, Lacher DA, Sempos CT, Taylor CL, Durazo-Arvizu RA, Maw KL, Chaudhary-Webb M, Johnson CL, Pfeiffer CM (2016) National estimates of serum total 25-hydroxyvitamin D and metabolite concentrations measured by liquid chromatography-tandem mass spectrometry in the US population during 2007–2010. J Nutr 146:1051–1061
Alshahrani FM, Almalki MH, Aljohani N, Alzahrani A, Alsaleh Y, Holick MF (2013) Vitamin D: light side and best time of sunshine in Riyadh, Saudi Arabia. Dermatoendocrinology 5:177–180
Mehboobali N, Iqbal SP, Iqbal MP (2015) High prevalence of vitamin D deficiency and insufficiency in a low income peri-urban community in Karachi. J Pak Med Assoc 65:946–949
Wakayo T, Belachew T, Vatanparast H, Whiting SJ (2015) Vitamin D deficiency and its predictors in a country with thirteen months of sunshine: the case of school children in Central Ethiopia. PLoS One 10:e0120963
Sahota O (2000) Osteoporosis and the role of vitamin D and calcium-vitamin D deficiency, vitamin D insufficiency and vitamin D sufficiency. Age Ageing 29(4):301–304 Review
Shaheen S, Noor SS, Barakzai Q (2012) Serum alkaline phosphatase screening for vitamin D deficiency states. J Coll Physicians Surg Pak 22(7):424–427. 07.2012/JCPSP.424427
Hashemipour S, Larijani B, Adibi H, Sedaghat M, Pajouhi M, Bastan-Hagh MH, Soltani A, Javadi E, Shafaei AR, Baradar-Jalili R, Hossein-Nezhad A (2006) The status of biochemical parameters in varying degrees of vitamin D deficiency. J Bone Miner Metab 24(3):213–218
Acknowledgements
We shall like to thank the Deanship of Research Chairs program, College of Medicine, King Saud University, for facilitating us in conducting this important research. We shall like to acknowledge the Princess Nora Research Chair for Women Health Research for their support and cooperation in conducting this study. We wish to express our appreciation for the efforts of Prof. Ellen B. Gold for reviewing the manuscript and for Mrs Maha Younis and Mr Bushra Abdulwahab for their efforts in supervising the research assistants, collecting the samples, sending it to the lab and arranging other logistics related to the project. We thank all the participants for their time and cooperation.
Funding
This study was financially supported by the Deanship of Research Chair Program, King Saud University, Riyadh. The funding agency had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
JAQ conceptualized the study, wrote the proposal, supervised the data collection, and participated in write-up and critical review of the manuscript; AK supervised the training and data collection, conducted the analysis, and participated in the write-up; MF was involved in the proposal writing, conducting the trainings, write-up of discussion, and critical review of the manuscript; NA was involved in the write-up and critical review of the whole manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study protocol was approved by the Institutional Review Board, King Saud University (E-12-658) and the Institutional Review Board of the Ministry of Health, Dammam (IRB ID MOH0151). Participants were enrolled in the study after they read, understood, and signed the consent form.
Consent for publication
The consent form included statement related to processing and publication of data for a scientific research paper.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
AlQuaiz, A.M., Kazi, A., Fouda, M. et al. Age and gender differences in the prevalence and correlates of vitamin D deficiency. Arch Osteoporos 13, 49 (2018). https://doi.org/10.1007/s11657-018-0461-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0461-5