Abstract
Summary
Link between obesity and bone health is controversial. It seems that maybe the difference in metabolic status leads to this difference. We studied relation between metabolically healthy/unhealthy components with bone mineral density. Results showed metabolically unhealthy obesity (MUHO) phenotypes have better bone status at hip site than metabolically healthy obesity (MHO). Also, component metabolic can effect on BMD in different sites.
Purpose/Introduction
This cross-sectional study aimed to compare total BMD and L-L4 BMD in MHO and MUHO base on Karelis criteria.
Methods
We enrolled 272 Iranian obese women and men (BMI ≥ 30). According to Karelis criteria, the participants were grouped base to MHO and MUHO. The body composition and BMD were assessed for all cases. Serum HDL-C, LDL-C, total cholesterol, triglyceride (TG), fasting blood glucose, homeostatic model assessment-insulin resistance (HOMA-IR), and hypersensitive C-reactive protein (hs-CRP) levels were quantified by ELISA method.
Results
Our results demonstrate MUHO phenotype have high total BMD more than MHO (P = 0.01, CI = 0.12 to 0.21). Also, the results of logistic regression analysis showed MUHO have strongly associated with total BMD (β = −0.42, CI = − 0.31 to − 0.04, P = 0.009), but did not affected L2-L4 BMD (β = − 0.09, CI = − 0.14 to 0.08, P = 0.578); this represents that there was discordance in MUHO subjects. Our evidence implicated that HOMA-IR, high level serum TG, hs-CRP, and low level serum HDL had mediatory effect on relationship between obesity and high BMD at the hip region in MUHO subjects (P < 0.05).
Conclusion
Present evidence indicates that, could be a novel link between difference in MUH phenotype and MH phenotype with bone status. Also, component metabolic can effect on BMD in different sites.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity prevalence is increasing worldwide, with the condition predicted to affect more than one billion people by 2030 [1,2,3]. Obesity is a chronic disease whose origin is determined by genetic factors as well as environmental influences [4]. It is associated with increased risk of developing co-morbidities including type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD) and is associated with many other conditions, including certain types of cancer, mental health, and increased mortality [5,6,7].
However, these cardio-metabolic abnormalities are not found in all obese people. Recent interest has focused on an obese subgroup with a healthy metabolic profile despite increased adiposity and has been investigated by several researchers [8,9,10]. Metabolically healthy obesity (MHO) describes the absence of any overt cardio-metabolic disease and the absence of the metabolic syndrome and favorable metabolic profile and inflammation profile, characterized by high levels of insulin sensitivity, low prevalence of hypertension, and components in an individual with a BMI ≥30 kg/m2. Evidence suggests that MHO individuals may account for as much as 20–30% of the obese population. [1, 5, 6].In longitudinal studies, this phenotype was associated with reduced risks of developing T2DM and CVD [7]. However, it is generally agreed that there is no evidence that these subjects are permanently protected from the risk of obesity-related co-morbidities [11]. Metabolically unhealthy obesity (MUHO), in contrast to the MHO group, displays the typical obesity-related metabolic disturbances of hyperinsulinemia, insulin resistance, hypertriglyceridemia, and possibly elevated risk of developing T2DM and CVD [12].
Overweight and obesity can strengthen the bone, which may decrease osteoporotic fracture risk by increasing bone mineral density (BMD), a well-known indicator for osteoporosis [13].
This protective effect of obesity is called the “obesity paradox” or “reverse epidemiology” and has been controversial, while some studies have shown that obesity is positively associated with high BMD as a result of the obesity-related increased levels of leptin, insulin, and estrogen that stimulate growth of bone and inhibit bone remodeling. The studies of National Osteoporosis Foundation and others suggested that low BMI should be included in the risk assessment tools for evaluation of osteoporosis and osteoporotic fracture risk. Several studies have reported that obesity was negatively associated with BMD [14,15,16,17,18].
In the present study, we tested the hypothesis that difference in metabolic status in MUHO and MHO leads to difference in bone status.
Materials and methods
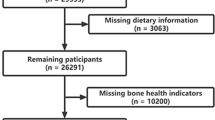
Study population
The study was conducted as a cross-sectional method on 272 obese adults aged 17–69 years old who fulfilled the study criteria. All participants were recruited from a nutrition clinic of the Shariati Hospital’s outpatient clinic. The registered patients in the clinic were enrolled in our study according to inclusion and exclusion criteria. Eight hundred participants were invited to a screening visit between November 2013 and December 2014. Individuals were included if they met the following criteria: having a BMI ≥ 30, absence of any acute or chronic inflammatory disease, no medical history of hypertension, no alcohol or drug abuse, not being pregnant, no medical history of any condition affecting inflammatory markers, absence of thyroid diseases, no malignancies, no current smoking, absence of diabetes mellitus, absence of any cardiovascular disease including heart failure, no acute or chronic infections, and absence of hepatic or renal diseases. Finally, we enrolled 272 obese Tehrani men and women (BMI ≥ 30) in this study. All participants provided written and informed consent forms (approved by TUMS Ethics Committee, with the following identification (91-02-27-18041-69439). The study protocol was approved by the local ethical committee of Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences.
Anthropometric measurements
Height and weight were measured. The BMI was calculated by dividing the weight (kg) by the square of the height (cm). Blood pressure was measured using a standardized sphygmomanometer after 5 minutes of rest. The waist circumference was measured in the standing position, at the middle point between the anterior iliac crest and lower border of rib by a single examiner.
Measurement of biochemical parameters
Serum was prepared from blood sample after having 10–12 h fasting state from each subject. Serum samples were aliquot into 1 ml tubes and stored at − 80 C. All baseline blood samples were obtained between 8:00 and 10:00 a.m. Serum was centrifuged, aliquoted, and stored at a temperature of − 80 C. All samples were analyzed by means of a single assay. Glucose Oxidase Phenol 4-Aminoantipyrine Peroxidase (GOD/PAP) method was used for the measurement of fasting serum glucose, and triglyceride levels were measured by Glycerol-3-phosphate oxidase Phenol 4-Aminoantipyrine Peroxidase (GPOPAP) method. Total cholesterol levels were measured by enzymatic endpoint method, and direct high- and low-density lipoproteins were measured by enzymatic clearance assay. Serum hypersensitive C-reactive protein (hs-CRP), a pro-inflammatory biomarker, was determined using a high-sensitivity immunoturbidimetric assay (Hitachi 902 Analyzer; Hitachi LTD, Tokyo, Japan). All inter-assay calculated coefficients of variation were within the normal range of enzymatic kits data sheets. Serum insulin concentrations were analyzed through enzyme-linked immunosorbent assay (ELISA) method (Human insulin ELISA kit, DRG Pharmaceuticals, GmbH, Germany). Minimum detectable concentration was 1.76 mIU/ml, intra CV was 2.19%, and inter CV was 4.4%.
The HOMA-IR calculation
Insulin resistance was calculated by the homeostatic model assessment (HOMA) according to the following equation: HOMA-IR = [fasting plasma glucose (mmol/l) × fasting plasma insulin (mIU/l)]/22.5 [19].
Determination of metabolic health status
Metabolic health status was defined using a MH definition based on Karelis criteria. According to Karelis criteria, metabolically healthy phenotype requires four or more of the following five components: TG ≤ 150 mg/dl, HDL-C ≥ 50 mg/dl and no treatment, LDL-C ≤ 100 mg/dl and no treatment, hs-CRP ≤ 3.0 mg/l, and HOMA-IR ≤ 1.95 [20]. We for examined the results from BMD and metabolic statues and effect blood parameter base on Karelis criteria and divided the participants into two groups, normal and abnormal, in terms of HDL-C, LDL-C, TG, HOMA, and hs-CRP.
Complete body composition analysis
The researchers assessed the body composition of all cases with the use of Body Composition Analyzer BC-418MA-Tanita (UK) by strictly following the techniques, procedure, and precaution of the manufacturer’s protocol. The device calculates body fat percentage, fat mass, and fat-free mass and predicts muscle mass on the basis of data obtained by dual energy X-ray absorptiometry (DXA) using bioelectrical impedance analysis (BIA) as described completely in previous study [19].
Bone mineral density measurement
All the subjects had undergone BMD measurements by dual energy X-ray absorptiometry (DEXA) of the lumbar spine (vertebrae L2-L4) and hip. The coefficient of variation for longitudinal BMD measurements in the DEXA machine averaged at 1.04%. Normal bone mass was defined as BMD measurements at or above one standard deviation (S.D.) from the optimal peak BMD (T score) of healthy young adults of the same sex. BMD measurement at or below − 2.5 S.D. from the optimal peak BMD of healthy young adults of the same sex was osteoporotic, as per World Health Organization standard definitions. The results are presented as absolute values in g/cm2 and as standard deviation units (Z score) based on comparison with age- and sex-matched BMD [21].
Statistical analyses
Data on quantitative characteristics were reported as the mean + SD and data on qualitative characteristics were expressed as percentage. We compare qualitative variables with analysis of variance (ANOVA) and independent t test to compare the quantitative variables. The linear regression model (LRM) analysis was used for finding the relationship of metabolic status on total BMD and L2-L4 BMD. In this model, BMD measurements including total BMD, total T score, total Z score, BMD L2-L4, L2-L4 T score, and L2-L4 Z score were entered as dependent variable, and metabolic status were entered as covariates. For finding the role of metabolic status in this model, we next added the metabolic status in crude and adjusted for age, sex, and BMI. The level of significance was set at a probability of ≤ 0.05 for all tests. Statistical analysis was performed using SPSS version 22.0 (SPSS, Chicago, IL, USA).
Result
Anthropometric measures and clinical characteristics
A total 272 subjects (19.1% male, 80.9%female) including 79 metabolically healthy (29.05%) and 193 metabolically unhealthy individuals (70.95%) were included in this study, and 68.8% female and 82.69% men were in MHO group. The mean age, weight, height, and BMI of the study participants were 39.12 years (SD 11.90), 93.68 kg (14.75), 162.42 cm (8.80), and 47.70 kg/m2 (3.98), respectively (Table 1). MHO ratio in different age groups < 20, 20–39, 40–59, and > 60 was respectively 50, 73.64, 71.13, and 57.89%. Clinical and anthropometric characteristics of the study population according to MH and MUH status are presented in Table 2. We found that 3.30% met 5/5 criteria, 25.73% met 4/5 criteria, 22.79% met 3/5 criteria; 22.05% met 2/5 criteria, 20.58% met 1/5 criteria, and 5.51% met 0/5 criteria.
In comparison with their MUHO participant, MHO individuals had 18% lower fasting blood glucose. Moreover, MHO subjects showed more favorable lipid profile, specifically they had respectively 50, 17, and 17% lower mean serum triglyceride, total cholesterol, and LDL-C, as well as 10% higher mean serum HDL-C compared to MUHO participants. There was statistically significant difference between two groups serum triglyceride (P < 0.0001), total cholesterol (P = 0.0002), LDL-C (P < 0.0001), HDL (P < 0.0001), FBS (P < 0.0001), and hs-CRP (P < 0.0001). As far as body composition is concerned, our result demonstrated that there was statistically significant difference regarding fat percentage (P < 0.0001), fat spine (P < 0.0001), and trunk fat (P < 0.0001) between two groups. In particular, MUHO subjects had respectively 1 and 2.83% higher total fat percentage and fat mass in comparison with MHO participant.
However, MUHO individuals showed 17% higher mean total BMD compared to MHO participants and there was statistically significant difference between two groups (P < 0.0001), but there was no statistically significant difference in L2-L4 BMD among the two groups (P > 0.05).
Also, there was no statistically significant difference between two sexes (P = 0.057) and between different age groups (P = 0.38).
Metabolic status and BMD relationship
We examine the association of BMD and metabolic features in MHO and MUHO subjects after controlling age, sex, and BMI effect (Table 3). The results of independent sample t test analysis for comparing the mean of characteristics between MH and MUHO groups showed that MUHO subjects have better BMD than MHO subjects (P ≤ 0.05). In the other words, a significant positive correlation was seen between unfavorable metabolic profile including high level serum TG, high level serum hs-CRP, low level serum HDL, high level serum HOMA-IR and LDL in MUHO subjects, and total BMD (β = −0.39, CI = − 0.30 to − 0.02, P = 0.020), total T score (β = − 0.43, CI = − 1.98 to − 0.30, P = 0.009), total Z score (β = − 0.48, CI = − 1.92 to − 0.40, P = 0.004); even after adjusting for age, sex, and BMI, this association was observed total BMD (β = − 0.42,CI = − 0.31 to − 0.04, P = 0.009), total T score (β = − 0.45, CI = − 1.89 to − 0.48, P = 0.002), total Z score (β = − 0.48, CI = − 1.89 to − 0.45, P = 0.002). But this positive association was only seen at the hip region (Table 3). In the other words, there was no statistically significant correlation between unfavorable metabolic profile in MUHO subjects and L2-L4 BMD (β = − 0.09, CI = − 0.14 to 0.08, P = 0.578), L2-L4 T score (β = − 0.10, CI = − 1.18 to 0.66, P = 0.570), L2-L4 Z score (β = − 0.11, CI = − 1.21 to 0.64, P = 0.531). MHO individuals have favorable metabolic and inflammation profile but increase the risk of osteoporosis because they have lower total BMD than MUHO, mean total BMD in MHO and MUHO subjects 0.98 vs 1.15, respectively, P < 0.0001 (Table 2).
Possible correlation between normal and abnormal components of Karelis criteria on BMD in different sites
We found positive association between total BMD with abnormal components of Karelis criteria including serum TG (P = 0.003, CI = − 0.11 to − 0.02), hs-CRP (P = 0.001, CI = − 0.11 to − .03), HOMA-IR (P = 0.0001, CI = − 0.16 to − 0.07), and HDL (P = 0.0001, CI = − 0.14 to − 0.05), and this represented that there was discordance in MUHO subjects. Also, high level serum LDL has no statistically significant correlation with total BMD (P = 0.06, CI − 0.08 to 0.002) (Fig. 1).
Possible correlation between normal and abnormal components of Karelis criteria on bone status in different sites. a Total BMD and L2-L4 BMD level between normal and abnormal TG, normal (n %): 85 (31%). b Total BMD and L2-L4 BMD level between normal and abnormal LDL, normal (n %): 113 (41%). c Total BMD and L2-L4 BMD level between normal and abnormal hs-CRP, normal (n %): 156 (57%). d Total BMD and L2-L4 BMD level between normal and abnormal HOMA, normal (n %): 94 (34%). e Total BMD and L2-L4 BMD level between normal and abnormal HDL, normal (n %): 94 (34%)
Discussion
Many studies have investigated the relation between BMD and BMI; the results were inconsistent. Unique feature of this study is the comparison between total BMD and L2-L4 BMD in MHO and MUHO ones base on Karelis criteria and association between metabolic status of healthy and unhealthy on BMD of hip site and lumbar. We observed that MUHO was positively associated with total BMD more than MHO, while no association with L2-L4 BMD.
Generally, in this study, the obesity reduced the risk for osteoporosis, osteopenia, and low BMD in Iranian people. The previous results of studies on the link between obesity and bone health are controversial. Cui et al. [22] studied men and women in rural Korea and reported that fat mass may positively contribute to BMD only in postmenopausal women and older men. These findings correlated with the results of Salamat et al. [23] which found that both BMI and weight are associated with BMD of the hip and vertebrae. Other authors have also confirmed the existence of the obesity paradox in so osteoporosis. The studies of National Osteoporosis Foundation and others suggested that low BMI should be included in the risk assessment tools for evaluation of osteoporosis and osteoporotic fracture risk [24]. Overall, obesity has a protective effect on osteoporosis because weight-bearing can cause a rise in bone density, especially at the hip and proximal femur regions. In addition, obesity provides cushioning for the hip in the event of a fall [14]. While some authors have reported that the increase in adipose tissue was not beneficial for BMD [25]. The inconsistencies between these results could be attributable to the specific study populations, specific gender, age, or site of measurement, genetic backgrounds, research designs, sampling methods, sample size, and methodological differences.
In present study, we found that MUHO phenotype was strongly associated with total BMD, total T score, and total Z score; even after adjusting for age, sex, and BMI, this association was maintained. Subjects with MUHO status have higher BMD more than MHO subjects. However, only total BMD was positively associated with MUHO and there was no statistically significant correlation between MUHO and L2-L4 BMD. In other words, just the metabolic unhealthy status had links with high BMD at hip site.
In our study, HOMA-IR and fasting plasma insulin concentration were positively associated with total BMD. Obesity was associated with elevated oxidative stress and increased production of proinflammatory cytokines that lead to insulin resistant [26]. In an insulin-resistant state, the plasma insulin level increased to compensate for the reduced responsiveness of target cells to insulin action. Bone is now recognized as an insulin target organ, and insulin receptor signaling in osteoblasts has been found to be important for proliferation, differentiation, and survival of osteoblasts [27, 28]. Furthermore, hyperinsulinemia may also have a negative impact on sex hormone-binding globulin, hence increasing free androgens and estrogens hormone which may protect against bone loss [29, 30]. The thesis that insulin increases BMD is biologically plausible. Insulin is structurally similar to IGF-I, to be regulator of bone formation [31]. In in vitro studies, IGF-I has been shown to enhance the replication of pre-osteoblastic cells, stimulate the differentiated function of osteoblasts, and increase bone collagen synthesis and matrix apposition [32, 33]. Also, controlling for various confounding factors, including age, sex, and BMI, is necessary for the assessment of the association between insulin resistance and bone mass, even after adjustment confounding factors seen high total BMD in MUHO. Thus, insulin resistance had directly affected on total BMD.
Several studies have suggested that favorable serum lipid profiles and reduced osteoporosis were closely related [34, 35]. Our analysis showed higher LDL level was not statistically significantly associated with high total BMD and lumbar BMD. Hypercholesterolemia had been associated with low BMD in some but not all studies. Recent reports by Parhami et al. indicated that cholesterol and its metabolites influence the functional activity of osteoblasts in vitro and in vivo conditions [36, 37]. However, studies evaluating a direct association between serum lipid profiles and BMD have reported inconsistent findings. Some reported that higher LDL-C is associated with lower BMD and suggested that hyperlipidemia could be associated with osteoporosis [38].
In this study, our analyses show abnormal serum HDL in MUHO phenotype statistically significantly associated with high total BMD. Previous studies have suggested biological pathways to explain the association between bone mineral density and high-density lipoprotein [39]. In order to explain the negative correlation between BMD and HDL, differentiation of mesenchymal stem cells (MSC) is highly regarded because those cells induce metabolic pathways of osteocytes [40]. It is likely that HDL may affect BMD through their positive influence on bone biomarkers such as osteocalcin [41]. Genetic diversity may be another reason which could explain this challenging correlation [39]. Therefore, further investigation in studies of more advanced design seems necessary in order to clarify the causal association between HDL-C and BMD.
However, subjects with higher serum TG levels showed lower lumbar BMD values, but had high total BMD. These findings suggested that there was a difference in the effect of TG levels on BMD at various skeletal sites in MUHO subjects. Numbers of studies have reported a positive relationship between BMD and TG levels [42, 43].However, it was difficult to illustrate the role of TG serum level on total BMD through a cross-sectional study, such as the present study. Moreover, the references in the effect of serum TG on BMD are scarce.
In the present study, total BMD in MUHO subjects was higher more than lumbar BMD of ones. Even, after adjusted for age, sex, and BMI, this correlation was maintained. Several possible explanations for discordance in this study could be proposed [44]. Generally, the impact of BMI on BMD differs depending on the skeletal site. Weight-bearing can cause a rise in BMD, especially in the hip and proximal femur. Non-uniform weight-bearing is also a well-known cause of physiologic dissimilarity in the hip and femurs [45]. Kyeong et al. showed that reduced overall weight-bearing due to low BMI may increase the risk of low BMD in the femur but not in the spine and can be the cause of the discordance [46]. Also, genetic differences, physiology between individuals and bone cell [47], and relationship between BMD at each site and genetic polymorphisms, such as the estrogen receptor-alpha and collagen-type I alpha 1 genes [48] or the sex hormone-binding globulin gene could be the other reasons for this discordance [49] .
In this study, MHO and MUHO subjects have same BMI, but MUHO subjects have higher fat percentage, fat spine, visceral fat, and trunk fat than MHO subjects and could be reason for higher total BMD in MUHO ones. The effect of fat mass on BMD may be due to the effect of adipokines and secretion adipokines impact on BMD in different sites, for example, leptin contributes to the positive association between adipose and bone tissue [50]. Also, higher HOMA-IR in MUHO phenotype led to increased total BMD more than MHO (Fig. 2).
To our knowledge, the strength of this study is the first study that evaluates possible link between metabolic unhealthy phenotype with total BMD and L2-L4 BMD in obese subjects. Studies in that possible relationship between BMD and metabolic feature in obese subjects require more clinical trial and cohort researches. The main limitation of the present study was the relatively small number of subjects. Also the cross-sectional design of our study, in which we could not determine the causality or mechanism of the relationship metabolic statues and BMD, could be considered as the study’s limitations.
Conclusion
In summary, specific skeletal sites (e.g., weight-bearing versus non-weight-bearing) as well as skeletal compartments (e.g., cortical versus trabecular) may also be differentially affected by obesity. Also, genetic differences and physiology between individuals can be the other reasons for this obesity paradox and BMD. Present evidence indicates that could be a novel link between difference in MUHO phenotype and MHO phenotype in BMD.
Abbreviations
- BMI:
-
Body mass index
- BIA:
-
Bioelectrical impedance analysis
- BMD:
-
Bone mineral density
- BW:
-
Body weight
- DXA:
-
Dual-energy X-ray absorptiometry
- FBS:
-
Fasting blood glucose
- FFM:
-
Fat-free mass
- FM:
-
Fat mass
- HOMA-IR:
-
Homeostatic model assessment-insulin resistance
- HDL:
-
High-density lipoprotein cholesterol
- LDL:
-
Low-density lipoprotein cholesterol
- LRM:
-
Linear regression models
- L2-L4 BMD:
-
Lumbar spine (vertebrae L2-L4) bone mineral density
- hs-CRP:
-
Hypersensitive C-reactive protein
- IL-6:
-
Interleukin-6
- IGF-I:
-
Insulin-like growth factor 1
- MH:
-
Metabolically healthy
- MUH:
-
Metabolically unhealthy
- MHO:
-
Metabolically healthy obesity
- MUHO:
-
Metabolically unhealthy obesity
- TBW:
-
Total body water
- Total-Chol:
-
Total cholesterol
- Total BMD:
-
Hip bone mineral density
- TG:
-
Triglyceride
References
Hwang LC, Bai CH, Sun CA, Chen CJ (2012) Prevalence of metabolically healthy obesity and its impacts on incidences of hypertension, diabetes and the metabolic syndrome in Taiwan. Asia Pac J Clin Nutr 21(2):227–233
Phillips CM, Dillon C, Harrington JM, McCarthy VJ, Kearney PM, Fitzgerald AP et al (2013) Defining metabolically healthy obesity: role of dietary and lifestyle factors. PLoS One 8(10):e76188
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML et al (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet 378(9793):804–814
Di Ciaula A, Portincasa P (2017) Diet and contaminants: driving the rise to obesity epidemics? Curr Med Chem
van Vliet-Ostaptchouk JV, Nuotio ML, Slagter SN, Doiron D, Fischer K, Foco L et al (2014) The prevalence of metabolic syndrome and metabolically healthy obesity in Europe: a collaborative analysis of ten large cohort studies. BMC Endocr Disord 14:9
Bell JA, Kivimaki M, Hamer M (2014) Metabolically healthy obesity and risk of incident type 2 diabetes: a meta-analysis of prospective cohort studies. Obes Rev 15(6):504–515
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K et al (2008) General and abdominal adiposity and risk of death in Europe. N Engl J Med 359(20):2105–2120
Hinnouho GM, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A (2013) Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diabetes Care 36(8):2294–2300
Karelis AD, Brochu M, Rabasa-Lhoret R (2004) Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metabolism 30(6):569–572
Messier V, Karelis AD, Prud'homme D, Primeau V, Brochu M, Rabasa-Lhoret R (2010) Identifying metabolically healthy but obese individuals in sedentary postmenopausal women. Obesity 18(5):911–917
Marini MA, Succurro E, Frontoni S, Hribal ML, Andreozzi F, Lauro R et al (2007) Metabolically healthy but obese women have an intermediate cardiovascular risk profile between healthy nonobese women and obese insulin-resistant women. Diabetes Care 30(8):2145–2147
Shaharyar S, Roberson LL, Jamal O, Younus A, Blaha MJ, Ali SS et al (2015) Obesity and metabolic phenotypes (metabolically healthy and unhealthy variants) are significantly associated with prevalence of elevated C-reactive protein and hepatic steatosis in a large healthy Brazilian population. J Obes 2015:178526
Felson DT, Zhang Y, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Mineral Res 8(5):567–573
Salamat MR, Salamat AH, Janghorbani M (2016) Association between obesity and bone mineral density by gender and menopausal status. Endocrinol Metab (Seoul) 31(4):547–558
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE et al (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332(12):767–773
Ravn P, Cizza G, Bjarnason NH, Thompson D, Daley M, Wasnich RD et al (1999) Low body mass index is an important risk factor for low bone mass and increased bone loss in early postmenopausal women. Early Postmenopausal Intervention Cohort (EPIC) study group. J Bone Mineral Res 14(9):1622–1627
Janicka A, Wren TA, Sanchez MM, Dorey F, Kim PS, Mittelman SD et al (2007) Fat mass is not beneficial to bone in adolescents and young adults. J Clin Endocrinol Metab 92(1):143–147
Zhao LJ, Liu YJ, Liu PY, Hamilton J, Recker RR, Deng HW (2007) Relationship of obesity with osteoporosis. J Clin Endocrinol Metab 92(5):1640–1646
Mirzaei K, Hossein-Nezhad A, Keshavarz SA, Eshaghi SM, Koohdani F, Saboor-Yaraghi AA et al (2014) Insulin resistance via modification of PGC1alpha function identifying a possible preventive role of vitamin D analogues in chronic inflammatory state of obesity. A double blind clinical trial study. Minerva Med 105(1):63–78
Hinnouho G-M, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A (2013) Metabolically healthy obesity and risk of mortality. Diabetes Care 36(8):2294–2300
Hossein-Nezhad A, Nikoo MK, Mirzaei K, Mokhtarei F, Meybodi HA (2010) Comparison of the bone turn-over markers in patients with multiple sclerosis and healthy control subjects. Eur J Inflammation 8(2):67–73
Cui LH, Shin MH, Chung EK, Lee YH, Kweon SS, Park KS et al (2005) Association between bone mineral densities and serum lipid profiles of pre- and post-menopausal rural women in South Korea. Osteoporos Int 16(12):1975–1981
Salamat MR, Salamat AH, Abedi I, Janghorbani M (2013) Relationship between weight, body mass index and bone mineral density in men referred for dual-energy X-Ray absorptiometry scan in Isfahan. Iran J Osteoporosis 2013:205963
Black DM, Steinbuch M, Palermo L, Dargent-Molina P, Lindsay R, Hoseyni MS et al (2001) An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12(7):519–528
Taes YE, Lapauw B, Vanbillemont G, Bogaert V, De Bacquer D, Zmierczak H et al (2009) Fat mass is negatively associated with cortical bone size in young healthy male siblings. J Clin Endocrinol Metab 94(7):2325–2331
Cao JJ (2011) Effects of obesity on bone metabolism. J Orthop Surg Res 6:30
Thrailkill KM, Lumpkin CK Jr, Bunn RC, Kemp SF, Fowlkes JL (2005) Is insulin an anabolic agent in bone? Dissecting the diabetic bone for clues. Am J Physiol Endocrinol Metab 289(5):E735–E745
Shin D, Kim S, Kim KH, Lee K, Park SM (2014) Association between insulin resistance and bone mass in men. J Clin Endocrinol Metab 99(3):988–995
Dennison EM, Syddall HE, Aihie Sayer A, Craighead S, Phillips DI, Cooper C (2004) Type 2 diabetes mellitus is associated with increased axial bone density in men and women from the Hertfordshire Cohort Study: evidence for an indirect effect of insulin resistance? Diabetologia 47(11):1963–1968
Birkeland KI, Hanssen KF, Torjesen PA, Vaaler S (1993) Level of sex hormone-binding globulin is positively correlated with insulin sensitivity in men with type 2 diabetes. J Clin Endocrinol Metab 76(2):275–278
Tritos NA, Klibanski A (2016) Effects of growth hormone on bone. Prog Mol Biol Transl Sci 138:193–211
Canalis E, Lian JB (1988) Effects of bone associated growth factors on DNA, collagen and osteocalcin synthesis in cultured fetal rat calvariae. Bone 9(4):243–246
Thiebaud D, Ng KW, Findlay DM, Harker M, Martin TJ (1990) Insulinlike growth factor 1 regulates mRNA levels of osteonectin and pro-alpha 1(I)-collagen in clonal preosteoblastic calvarial cells. J Bone Mineral Res 5(7):761–767
Edwards CJ, Hart DJ, Spector TD (2000) Oral statins and increased bone-mineral density in postmenopausal women. Lancet 355(9222):2218–2219
Orozco P (2004) Atherogenic lipid profile and elevated lipoprotein (a) are associated with lower bone mineral density in early postmenopausal overweight women. Eur J Epidemiol 19(12):1105–1112
Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y et al (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 17(4):680–687
Parhami F, Garfinkel A, Demer LL (2000) Role of lipids in osteoporosis. Arterioscler Thromb Vasc Biol 20(11):2346–2348
Orozco P (2004) Atherogenic lipid profile and elevated lipoprotein (a) are associated with lower bone mineral density in early postmenopausal overweight women. Eur J Epidemiol 19(12):1105–1112
Ackert-Bicknell CL (2012) HDL cholesterol and bone mineral density: is there a genetic link? Bone 50(2):525–533
Nombela-Arrieta C, Ritz J, Silberstein LE (2011) The elusive nature and function of mesenchymal stem cells. Nat Rev Mol Cell Biol 12(2):126–131
Chin KY, Ima-Nirwana S, Mohamed IN, Ahmad F, Ramli ES, Aminuddin A et al (2014) Serum osteocalcin is significantly related to indices of obesity and lipid profile in Malaysian men. Int J Med Sci 11(2):151–157
Dennison EM, Syddall HE, Aihie Sayer A, Martin HJ, Cooper C (2007) Lipid profile, obesity and bone mineral density: the Hertfordshire Cohort Study. QJM 100(5):297–303
Adami S, Braga V, Zamboni M, Gatti D, Rossini M, Bakri J et al (2004) Relationship between lipids and bone mass in 2 cohorts of healthy women and men. Calcif Tissue Int 74(2):136–142
Woodson G (2000) Dual X-ray absorptiometry T-score concordance and discordance between the hip and spine measurement sites. J Clin Densitom 3(4):319–324
Kohrt WM, Snead DB, Slatopolsky E, Birge SJ Jr (1995) Additive effects of weight-bearing exercise and estrogen on bone mineral density in older women. J Bone Mineral Res 10(9):1303–1311
Park KH, Lim JS, Kim KM, Rhee Y, Lim SK (2016) Z-score discordance and contributing factors in healthy premenopausal women with low bone mineral density: the Korean National Health and Nutrition Examination Survey 2008–9. J Bone Miner Metab 34(6):668–677
Duncan EL, Danoy P, Kemp JP, Leo PJ, McCloskey E, Nicholson GC et al (2011) Genome-wide association study using extreme truncate selection identifies novel genes affecting bone mineral density and fracture risk. PLoS Genet 7(4):e1001372
Erdogan MO, Yildiz H, Artan S, Solak M, Tascioglu F, Dundar U et al (2011) Association of estrogen receptor alpha and collagen type I alpha 1 gene polymorphisms with bone mineral density in postmenopausal women. Osteoporos Int 22(4):1219–1225
Napoli N, Varadharajan A, Rini GB, Del Fiacco R, Yarramaneni J, Mumm S et al (2009) Effects of polymorphisms of the sex hormone-binding globulin (SHBG) gene on free estradiol and bone mineral density. Bone 45(6):1169–1174
Weiss LA, Barrett-Connor E, von Muhlen D, Clark P (2006) Leptin predicts BMD and bone resorption in older women but not older men: the Rancho Bernardo study. J Bone Mineral Res 21(5):758–764
Funding
This study was supported by Osteoporosis Research Center, Endocrine Diseases and Metabolism Research Institute, Tehran University of Medical Sciences and grants of Tehran University of Medical Sciences (Grants ID: 91-02-27-18041 and 94-02-161-29547).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All participants provided written and informed consent forms (approved by TUMS Ethics Committee, with the following identification (91-02-27-18041-69439). The study protocol was approved by the local ethical committee of Endocrinology and Metabolism Research Institute of Tehran University of Medical Sciences.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Mirzababaei, A., Mirzaei, K., Khorrami-nezhad, L. et al. Metabolically healthy/unhealthy components may modify bone mineral density in obese people. Arch Osteoporos 12, 95 (2017). https://doi.org/10.1007/s11657-017-0381-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0381-9