Abstract
Previous studies have demonstrated uncertainty regarding the effect of metabolic syndrome (MetS) on bone. In the present work, we investigated the association between MetS, its components, and decreased bone mineral density (BMD) in a cross-sectional study of patients who underwent BMD measurement by dual-energy X-ray absorptiometry during a health examination. Decreased BMD was defined as either osteopenia or osteoporosis. MetS components and body mass index (BMI) were compared between individuals with normal and decreased BMD, and simple and multivariate logistic regression analyses were used to evaluate the association between the variables and decreased BMD in women and men. Among 1162 subjects in the study, the mean age was 59.9 ± 7.3 years, and 59.5% were men. The prevalence of MetS and osteoporosis was 34.2 and 19.6%, respectively. MetS was positively associated with BMD in men, while in women it was negatively associated with BMD. Regarding the relationship between MetS components and BMD, we found that in women, waist circumference (WC) and systolic and diastolic blood pressure were negatively associated with BMD, while high-density lipoprotein cholesterol (HDL-C) was positively associated. In men, WC and fasting glucose were positively associated with BMD, while HDL-C was negatively associated. We also found that an increase in the number of MetS components resulted in a significantly increased positive association with BMD, both before and after adjusting for age, in men but not in women, revealing a gender difference in the correlation between MetS components and BMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic skeletal disease and is one of the most prevalent public health problems in elderly populations, with higher fracture risk leading to higher morbidity and mortality [1]. With increased life expectancy and the corresponding expanding elderly population, the economic burden of osteoporosis is likely to rise. Some studies have shown that osteoporosis and atherosclerotic cardiovascular disease share risk factors and pathophysiological mechanisms such as aging, smoking, sedentary lifestyle, pro-inflammatory state, and increased oxidative stress [2,3,4].
Metabolic syndrome (MetS) is a complex disorder comprising central obesity, high blood pressure (BP), hyperglycemia, hypertriglyceridemia, and a low concentration of high-density lipoprotein cholesterol (HDL-C). In addition to the association with cardiovascular disease and diabetes mellitus, MetS and its component elements have their own independent effects on bone metabolism. However, the studies of individual component or combined effects of MetS on bone mass are inconsistent [5, 6]. In a cross-sectional study of 2745 Korean women, the mean vertebral bone mineral density (BMD) was significantly lower in women with MetS [5]. However, another study showed that MetS was associated with higher BMD [6]. Based on these conflicting results, and given the increasing prevalence of osteoporosis, MetS, and obesity in the aging Taiwanese population, we conducted a cross-sectional study to examine the association between MetS, its components, body mass index (BMI), and BMD among a healthy Taiwanese population.
Materials and methods
Subjects
From January 2014 to December 2014, 5444 subjects visited the health management and evaluation center of a tertiary medical care facility located in southern Taiwan for routine health examinations. Our center offers a variety of tests and procedures, including BMD measured by dual-energy X-ray absorptiometry (DEXA; Hologic QRD 2000, Hologic, Inc., Waltham, MA, USA). The majority of subjects underwent a self-paid physical check-up; others were employees coming for their regular medical check-up. Most of the subjects were free of symptoms and were not chronic alcohol drinkers. Of the 5444 subjects, 1162 who had undergone BMD measurement with complete data available and who were over 50 years of age were enrolled in this cross-sectional study. The study was approved by the institutional review board of the hospital in which the study was conducted.
Measurements of anthropometric parameters
Height was measured while subjects stood erect, barefoot, with feet together, looking forward. Weight was measured by an automatic scale, with subjects wearing light clothes. BMI was then calculated as weight in kilograms divided by height in meters squared (kg/m2). A normal BMI level was defined as 18.5–23.9 kg/m2, according to the guidelines set forth by the Taiwan Department of Health. Waist circumference (WC) was measured at the mid-level between the iliac crest and the lower border of the 12th rib while the subject stood with feet 25–30 cm apart. A normal WC level in men and women was defined as 90 and 80 cm, respectively. BMD values were measured in g/cm2 by dual-energy X-ray absorptiometry (Lunar Prodigy Advance; GE Healthcare, Madison, WI, USA) at the lumbar spine, total femoral (total hip), femoral neck, and radius head.
Definition of metabolic syndrome and osteoporosis
In this study, MetS was defined according to the modified National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) for Asian populations. The WC cutoff measurement was adjusted according to the criteria of the Bureau of Health Promotion, Department of Health, because the absolute risk of diabetes and cardiovascular disease is greater in Asians with a lower degree of obesity [7, 8]. MetS was diagnosed when at least three of the following five components were found: (1) WC ≥90 cm for men and ≥80 cm for women; (2) high BP (systolic pressure ≧130 mmHg and/or diastolic pressure ≧85 mmHg, under treatment, or previously diagnosed with hypertension); (3) high serum triglyceride (≧150 mg/dL); (4) decreased HDL-C (<40 mg/dL for men and <50 mg/dL for women); (5) high fasting glucose (FG) ≧100 mg/dL, under treatment, or previously diagnosed with diabetes mellitus). Cardiovascular risk, which is determined by a ratio of total cholesterol (TC) to HDL-C >5 and correlates significantly with the risk for cardiovascular events [9].
The estimated glomerular filtration rate (eGFR) was calculated using the abbreviated Modification of Diet in Renal Disease (MDRD) study equation: eGFR (mL/min/1.73 m2) = 186 × (serum creatinine [mg/dL[) − 1.154 × age − 0.203 (× 0.742 if female) [12]. Subjects were divided into three groups with respect to eGFR: ≥90 mL/min/1.73 m2 or more, 60–90 mL/min/1.73 m2 and <60 mL/min/1.73 m2. Chronic kidney disease (CKD) was defined as an eGFR <60 mL/min/1.73 m2.
The diagnosis of osteoporosis was defined according to the World Health Organization (WHO) definition. The T-score was calculated automatically, and the lowest value was chosen for the diagnosis of osteoporosis. Osteoporosis was defined as T-score ≤−2.5; osteopenia as −2.5 < T-score <− 1, normal as ≥−1. The definition of decreased BMD included both osteopenia and osteoporosis.
Statistical analyses
The characteristics of subjects are presented as mean ± SD for continuous variables and as frequencies for categorical variables. Differences between groups were compared by the χ 2 test for categorical variables and Student’s t test for continuous variables. Odds ratios (OR) for subjects with decreased BMD were analyzed by simple and multiple logistic regression analyses. All statistical analyses were performed using SPSS version 19.0 software (IBM Corp., Armonk, NY, USA). A two-tailed p value <0.05 was considered statistically significant.
Results
Prevalence of osteoporosis and MetS
Among 1162 subjects in the study, the mean age was 59.9 ± 7.3 years (range 50–90), and 59.5% were men. The mean age was 59.9 ± 6.9 for women and 60.1 ± 7.5 for men. The overall prevalence of MetS was 34.2%: 32.1% in women and 35.6% in men. The overall prevalence of osteoporosis was 19.6%: 27.4% in women and 14.3% in men. Other baseline characteristics of subjects stratified by sex are summarized in Table 1.
Characteristics of subjects with normal and decreased BMD
The differences between women and men with normal and decreased BMD are shown in Table 2. When compared with those with normal BMD, women with decreased BMD were older, had higher BMI, WC, hip circumference, and systolic and diastolic BP, and a higher percentage of MetS, and had significantly lower values of height and weight and HDL-C levels. (all p < 0.001, except systolic and diastolic BP).
When compared with those with normal BMD, men with decreased BMD were older and had higher HDL-C levels, and had significantly lower height, weight, BMI, WC, hip circumference, and fasting glucose values and a lower percentage of MetS.
Simple and multiple stepwise logistic regression analyses of variables associated with decreased BMD
The results from the simple and multiple stepwise logistic regression analyses in women and men are show in Tables 3 and 4. In simple logistic regression analysis of women, height (OR = 0.88; 95% CI 0.84–0.92), weight (OR = 0.93; 95% CI 0.91–0.95), and HDL-C (OR = 0.98; 95% CI 0.97–0.99) were positively associated with BMD, while age (OR = 1.17; 95% CI 1.11–1.23), BMI (OR = 1.24; 95% CI 1.15–1.35), WC (OR = 1.06; 95% CI 1.03–1.09), hip circumference (OR = 1.08; 95% CI 1.04–1.12), systolic BP (OR = 1.02; 95% CI 1.01–1.03), and diastolic BP (OR = 1.04; 95% CI 1.02–1.06) were negatively associated with BMD. In multiple logistic regression analysis in women, height (OR = 0.95; 95% CI 0.90–0.998) and weight (OR = 0.93; 95% CI 0.90–0.96) were independent positively associated with BMD, while age (OR = 1.15; 95% CI 1.09–1.22) and BMI (OR = 1.17; 95% CI 1.06–1.29) were independent negatively associated with BMD. In simple logistic regression analysis in men, height (OR = 0.94; 95% CI 0.92–0.97), weight (OR = 0.95; 95% CI 0.93–0.96),
BMI (OR = 0.87; 95% CI 0.83–0.92), WC (OR = 0.97; 95% CI 0.95–0.98), hip circumference (OR = 0.93; 95% CI 0.91–0.96), and fasting glucose (OR = 0.99; 95% CI 0.99–0.994) were positively associated with BMD, while age (OR = 1.03; 95% CI 1.01–1.06) and HDL-C (OR = 1.02; 95% CI 1.00–1.03) were negatively associated. In multiple logistic regression analysis in men, fasting glucose (OR = 0.99; 95% CI 0.99–1.00) and weight (OR = 0.90; 95% CI 0.88–0.93) were independent positively associated with BMD, while WC (OR = 1.06; 95% CI 1.03–1.10) was independently negatively associated.
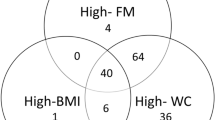
Association between MetS, MetS components, and BMD
We analyzed the OR of the number of MetS components for decreased BMD. Table 5 shows that in women, the OR for decreased BMD was progressively increased with the number of MetS components in unadjusted and adjusted models. Table 6 shows that in men, the OR for decreased BMD was progressively decreased with the number of MetS components. MetS (MetS components ≥3) was positively associated with BMD in men, while in women MetS was negatively associated with BMD.
Discussion
The prevalence of MetS in this study was 34.2%, with a higher rate in men than women (35.6% in men; 32.1% in women), according to the NCEP-ATP III definition. This prevalence is higher than in the general population of Taiwan, which was only 15.5% in men and 10.5% in women in a 2004 survey [10]. The overall prevalence of osteoporosis was 19.6%, with more women affected than men (27.4% in women, and 14.3% in men).This prevalence was higher than that in a 2004 survey by Yang et al. [11], who reported only 10.08 and 7.45% in lumbar vertebrae and femoral neck, respectively.
Data from previous studies regarding the relationship between MetS, its components, and osteoporosis is controversial. A meta-analysis by Zhou et al. [12] showed a negative effect of MetS on BMD in men but not in women. In another meta-analysis, Xue et al. [13] reported that MetS may have a beneficial influence on BMD in white populations. A cross-sectional study by Tseng et al. [14] found no association between MetS and bone mineral loss in either sex. Our study showed that MetS was positively associated with BMD in men, but negatively associated with BMD in women. We also found that an increase in the number of MetS components resulted in a significantly increased positive association with BMD, both before and after adjusting for age, in men (Table 6) but not in women (Table 5), thus revealing a gender difference in the correlation between MetS components and BMD. This means that, although age, MetS, and its components have a significant effect on BMD, sex is a major risk factor for osteoporosis.
There is strong evidence that patients with type 1 diabetes show decreased BMD [15,16,17]. The relation between type 2 diabetes and osteoporosis remains controversial. Tseng et al. [14] found no significant association between fasting glucose and BMD. Previous cross-sectional studies have shown that patients with type 2 diabetes had higher BMD [18, 19]. The study by Muka et al. [20] also showed that the glucose component (unrelated to diabetes status) was positively associated with femoral neck BMD in both men and women. Although meta-analyses from Esposito et al. [21] and Yang et al. [22] have shown that the existence of MetS is associated with less fracture risk, Oz et al. [23] found that increased fasting glucose, a component of MetS, may lower bone turnover but increase skeletal fragility, which results in increased fracture risk despite a higher BMD. Our study showed that fasting glucose was independently positively associated with BMD in men but not in women; however, the prevalence of fracture was not considered, and thus the relationship between MetS and fracture could not be determined.
The relationship between central obesity and BMD is inconsistent. Some studies have shown a significant association between central obesity and low bone mass [20, 24,25,26,27], while others have reached the opposite conclusion [28, 29]. Several studies have found high BMI to be a protective factor against excessive bone loss [30,31,32,33]. The present results showed a significant positive association between WC (central obesity), BMI, body weight, and BMD in men, but in women, only weight was positively associated with BMD, while WC and BMI were negatively associated. Some researchers have suggested that higher BMD with MetS is largely determined by abdominal obesity, and that the protective effects of fat mass may promote bone formation via high mechanical loading [34]. However, the answer to why there are differences between men and women with regard to the association of WC and BMI with BMD requires further prospective study.
Some studies have reported that hypertension is related to low bone mass due to the changes in serum intact parathyroid hormone (PTH) concentration or urinary calcium excretion [35, 36], but the results are inconsistent. Hanley et al. [37] found an independent association between hypertension and higher BMD for both genders, while Mussolino and Gillum [38] found no significant relation between BP and BMD at any bone site. Tseng et al. [14] showed no significant association between systolic BP and BMD in either sex, although there was a strong inverse relationship between diastolic BP and bone mineral loss in both men and women. Yang et al. [39] showed that women with hypertension had lower BMD at the femoral neck, whereas hypertension in men was associated with higher femoral neck BMD. Hypertension is associated with increased fracture risk in women, and the association is independent of BMD, but there is no significant association between hypertension and fracture risk in men. Our results showed that systolic and diastolic BP were not significantly associated with BMD in men, but a significant negative relationship was found in women.
The relationship between dyslipidemia and osteoporosis is also controversial. One study showed a significant positive correlation between BMD and serum lipids, especially HDL-C in postmenopausal women [40]. However, other studies have found BMD to be negatively associated with HDL-C and positively associated with total cholesterol (TC), triglyceride (TG), and LDL-C [14, 41,42,43]. Our study also showed a positive correlation between BMD and HDL-C in women, but a negative correlation between BMD and HDL-C in men, and there was no significant association of TC and TG with BMD.
Oxidative stress has been implicated in the pathogenesis of osteoporosis. Uric acid, a potent antioxidant, has been associated with BMD, but previous studies have yielded conflicting results. Ishii et al. and Makovay et al. [44, 45] demonstrated a positive association between uric acid and BMD in peri- and postmenopausal women. Our study did not show a significant association between uric acid and BMD in either sex. Simple logistic regression analysis showed that hip circumference had a positive association with BMD in men but a negative association in women, but we found no independent significant association with BMD in multiple logistic regression analysis. This may indicate that MetS components have a greater effect than hip circumference on BMD.
Shin et al. [46] showed that BMD was negatively related to CKD in women before adjusting for age, and was positively related to CKD in men. Kong et al. [47] showed that mild-to-moderate CKD was not independently associated with decreased BMD. In our study, eGFR and CKD were not significantly associated with decreased BMD.
The present study has several limitations. First, the study population comprised self-referred participants who visited a health promotion center, and they may not be representative of the general population. Second, it is a cross-sectional study, and the cause-and-effect relationship of BMD with MetS should be clarified by a prospective study. Lastly, the study population was exclusively Taiwanese, and therefore we cannot be certain that our results can be extrapolated to other populations.
In conclusion, through this retrospective cross-sectional study, we found that MetS (MetS components ≧3) was positively associated with BMD in men, while in women, MetS was negatively associated with BMD. Moreover, in women, MetS components such as WC and systolic and diastolic BP were negatively associated with BMD, while HDL-C was positively associated. In men, WC and fasting glucose were positively associated with BMD, while HDL-C was negatively associated. We also found that an increase in the number of MetS components had a significantly increased positive association with BMD, both before and after adjusting for age, in men but not in women.
References
Johnell O, Kamis JA (2006) An estimated of worldwide prevalence and disability associated with osteoporosis fractures. Osteoporosis Int 17:1726–1733
Fink HA, Ewing SK, Ensrud KE, Barrett-Connor E, Taylor BC, Cauley JA et al (2006) Association of testosterone and estradiol deficiency with osteoporosis and rapid bone loss in older men. J Clin Endocrinol Metab 91:3908–3915
Ding C, Parameswaran V, Udayan R, Burgess J, Jones G (2008) Circulating levels of inflammatory markers predict change in bone mineral density and resorption in older adults: a longitudinal study. J Clin Endocrinol Metab 93:1952–1958
Almeida M, Han L, Martin-Millan M, Plotkin LI, Stewart SA, Roberson PK et al (2007) Skeletal involution by age-associated oxidative stress and its acceleration by loss of sex steroids. J Biol Chem 282:27285–27297
Hwang DK, Choi HJ (2010) The relationship between low bone mass and metabolic syndrome in Korean women. Osteoporos Int 21:425–431
Park KK, Kim SJ, Moon ES (2010) Association between bone mineral density and metabolic syndrome in postmenopausal Korean women. Gynecol Obstet Invest 69:145–152
Jia WP, Xiang KS, Chen L, Lu JX, Wu YM (2002) Epidemiological study on obesity and its comorbidities in urban Chinese older than 20 years of age in Shanghai, China. Obes Rev 3:157–165
Gill TP (2001) Cardiovascular risk in the Asia-Pacific region from a nutrition and metabolic point of view: abdominal obesity. Asia Pac J Clin Nutr 10:85–89
Wang TD, Chen WJ, Chien KL, Seh-Yi Su SS, Hsu HC, Chen MF, Liau CS, Lee YT (2001) Efficacy of cholesterol levels and ratios in predicting future coronary heart disease in a Chinese population. Am J Cardiol 88:737–743
Chuang SY, Chen CH, Chou P (2004) Prevalence of metabolic syndrome in a large health check-up population in Taiwan. J. Chin. Med. Assoc. 67:611–620
Yang TS, Chen YR, Chen YJ, Chang CY, Ng HT (2004) Osteoporosis: prevalence in Taiwanese women. Osteoporos Int 15:345–347
Zhou Jiaojiao, Zhang Qiang, Yuan Xiaolan, Wang Jijiao, Li Chunyan, Sheng Hui, Shen Qu, Li Hong (2013) Association between metabolic syndrome and osteoporosis: a meta-analysis. Bone 57:30–35
Xue P, Gao P, Li YK (2012) The association between metabolic syndrome and bone mineral density: a meta-analysis. Endocrine 42:546–554
Tseng Yao-Hsien, Huang Kui-Chou, Liu Mann-Li, Shu Wei-Tzu, Sheu Wayne Huey-Herng (2009) Association between metabolic syndrome and bone mineral loss: a cross-sectional study in Puli Township in Taiwan. Arch Gerontol Geriatr 49:S37–S40
Ersoy B, Gökşen D, Darcan S, Mavi E, Oztürk C (1999) Evaluation of bone mineral density in children with diabetes mellitus. Indian J Pediatr 66:375–379
Hough FS (1987) Alterations of bone and mineral metabolism in diabetes mellitus. Part II. Clinical studies in 206 patients with type I diabetes mellitus. S Afr Med J 72:120–126
Forst T, Pfützner A, Kann P, Schehler B, Lobmann R, Schäfer H, Andreas J, Bockisch A, Beyer J (1995) Peripheral osteopenia in adult patients with insulin dependent diabetes mellitus. Diabet Med 12:874–879
Kao WH, Kammerer CM, Schneider JL, Bauer RL, Mitchell BD (2003) Type 2 diabetes is associated with increased bone mineral density in Mexican–American women. Arch Med Res 34:399–406
Schwartz AV, Sellmeyer DE, Strotmeyer ES, Tylavsky FA, Feingold KR, Resnick HE, Shorr RI, Nevitt MC, Black DM, Cauley JA, Cummings SR, Harris TB (2005) Health ABC Study. Diabetes and bone loss at the hip in older black and white adults. J Bone Miner Res 20:596–603
Muka T, Trajanoska K, Kiefte-de Jong JC, Oei L, Uitterlinden AG, Hofman A et al (2015) The association between metabolic syndrome, bone mineral density, hip bone geometry and fracture risk: the Rotterdam study. PLoS One 10:e0129116. doi:10.1371/journal.pone.0129116
Esposito K, Chiodini P, Capuano A, Colao A, Guigliano D (2013) Fracture risk and bone mineral density in metabolic syndrome: a meta-analysis. J Clin Endocrinol Metab 98:3306–3314
Yang L, Lv X, Wei D, Yue F, Guo J, Zhang T (2016) Metabolic syndrome and the risk of bone fractures: a meta-analysis of prospective cohort studies. Bone 84:52–56
Oz SG, Guven GS, Kilicarslan A, Calik N, Beyazit Y, Sozen T (2006) Evaluation of bone metabolism and bone mass in patients with type-2 diabetes mellitus. J Natl Med Assoc 98:1598–1604
Jankowska EA, Rogucka E, Medras M (2001) Are general obesity and visceral adiposity in men linked to reduced bone mineral content resulting from normal ageing? A population-based study. Andrologia 33:384–389
Blaauw R, Albertse EC, Hough S (1996) Body fat distribution as a risk factor for osteoporosis. S Afr Med J 86:1081–1084
Torti C, Mazziotti G, Soldini PA, Focà E, Maroldi R, Gotti D, Carosi G, Giustina A (2001) High prevalence of radiological vertebral fractures in HIV-infected males. Endocrine 41:512–517
Moon SS, Lee YS, Kim SW (2012) Association of nonalcoholic fatty liver disease with low bone mass in postmenopausal women. Endocrine 42:423–429
Edelstein SL, Barrett-Connor E (1993) Relation between body size and bone mineral density in elderly men and women. Am J Epidemiol 138:160–169
Agbaht K, Gurlek A, Karakaya J, Bayraktar M (2009) Circulating adiponectin represents a biomarker of the association between adiposity and bone mineral density. Endocrine 35:371–379
Felson DT, Zhang Y, Hannan MT, Anderson JJ (1993) Effects of weight and body mass index on bone mineral density in men and women: the Framingham study. J Bone Miner Res 8:567–573
Marcus R, Greendale G, Blunt BA, Bush TL, Sherman S, Sherwin R, Wahner H, Wells B (1994) Correlates of bone mineral density in the postmenopausal estrogen/progestin interventions trial. J Bone Miner Res 9:1467–1476
De Laet C, Kanis JA, Odén A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Gimble JM, Nuttall ME (2004) Bone and fat: old questions, new insights. Endocrine 23:183–188
Kim BJ, Ahn SH, Bae SJ, Kim EH, Kim TH, Lee SH, Kim HK, Choe JW, Kim SY, Koh JM, Kim GS (2013) Association between metabolic syndrome and bone loss at various skeletal sites in postmenopausal women: a 3-year retrospective longitudinal study. Osteoporos Int 24:2243–2252
Grobbee DE, Hackeng WH, Birkenhäger JC, Hofman A (1988) Raised plasma intact parathyroid hormone concentrations in young people with mildly raised blood pressure. Br Med J (Clin Res Ed) 296:814–816
Hughes GS Jr, Oexmann MJ, Margolius HS, Epstein S, Bell NH (1988) Normal vitamin D and mineral metabolism in essential hypertension. Am J Med Sci 296:252–259
Hanley DA, Brown JP, Tenenhouse A, Olszynski WP, Ioannidis G, Berger C, Prior JC, Pickard L, Murray TM, Anastassiades T, Kirkland S, Joyce C, Joseph L, Papaioannou A, Jackson SA, Poliquin S, Adachi JD, Canadian Multicentre Osteoporosis Study Research Group (2003) Associations among disease conditions, bone mineral density, and prevalent vertebral deformities in men and women 50 years of age and older: crosssectional results from the Canadian Multicentre Osteoporosis Study. J Bone Miner Res 18:784–790
Mussolino ME, Gillum RF (2006) Bone mineral density and hypertension prevalence in postmenopausal women: results from the Third National Health and Nutrition Examination Survey. Ann Epidemiol 16:395–399
Yang S, Nguyen ND, Center JR, Eisman JA (2014) Association between hypertension and fragility fracture: a longitudinal study. Osteoporosis Int 25:97–103
Yamaguchi T, Sugimoto T, Yano S, Yamauchi M, Sowa H, Chen Q, Chihara K (2002) Plasma lipids and osteoporosis in postmenopausal women. Endocr J 49:211–217
Adami S, Braga V, Zamboni M, Gatti D, Rossini M, Bakri J, Battaglia E (2004) Relationship between lipids and bone mass in 2 cohorts of healthy women and men. Calcif Tissue Int 74:136–142
Von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E (2007) Associations between the metabolic syndrome and bone health in older men and women: the Rancho Bernardo Study. Osteoporos Int 18:1337–1344
Dennison EM, Syddall HE, Aihie Sayer A, Martin HJ, Cooper C (2007) Lipid profile, obesity and bone mineral density: the Hertfordshire Cohort Study. QJM 100:297–303
Ishii S, Miyao M, Mizuno Y, Tanaka-Ishikawa M, Akishita M, Ouchi Y (2014) Association between serum uric acid and lumbar spine bone mineral density in peri- and postmenopausal Japanese women. Osteoporosis Int l25:1099–1105
Makovey J, Macara M, Chen JS, Hayward CS, March L, Seibel MJ, Sambrook PN (2013) Serum uric acid plays a protective role for bone loss in peri- and postmenopausal women: a longitudinal study. Bone 52:400–406
Shin JH, Kim SH, Yu SH (2014) Metabolic syndrome and chronic kidney disease as risk factors of osteoporosis. Clin Nephrol 81:1–8
Kong X, Tang L, Ma X, Liu W, Wang Z, Cui M, Xu D (2015) Relationship between mild-to-moderate chronic kidney disease and decreased bone mineraldensity in Chinese adult population. Int Urol Nephro 47:1547–1553
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
About this article
Cite this article
Loke, SS., Chang, HW. & Li, WC. Association between metabolic syndrome and bone mineral density in a Taiwanese elderly population. J Bone Miner Metab 36, 200–208 (2018). https://doi.org/10.1007/s00774-017-0826-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-017-0826-7