Abstract
Summary
We examined the relationships between bone mineral density (BMD) and metabolic syndrome in 6,659 men and 7,826 women from South Korean. After adjusting for age, body mass index (BMI), tobacco and alcohol use, and regular exercise, low BMD is especially associated with metabolic syndrome in South Korean men.
Purpose
This study examined the relationships between BMD and metabolic syndrome (MS) in South Korean adults.
Methods
A total of 14,485 adults (6,659 men and 7,826 women) in the Korea National Health and Nutrition Examination Survey conducted from 2008 to 2010 were analyzed. We used multivariable regression models to examine the relationship between low BMD and MS. We calculated homeostasis model assessment and insulin resistance (HOMA-IR). MS was defined according to AHA/NHLBI criteria for Asians. BMD was measured at the lumbar spine (LS), femur neck (FN), total hip (TH), trochanter, and intertrochanter.
Results
After adjustment for age, BMI, tobacco and alcohol use, and regular exercise, the TH and FN BMD were significantly lower in men with MS than in men without MS (p < 0.05). However, there were no differences in premenopausal and postmenopausal women. In men, BMD was positively correlated with BMI, and high density lipoprotein cholesterol, but was negatively correlated with insulin, HOMA-IR, and triglyceride at all three sites (p < 0.05). Along with an increase of BMD (0.1 g/cm2), the odds ratios (ORs) for obesity and abdominal obesity were all greater than 1 at all sites in both genders. The ORs for hypertension and MS were 0.937 (0.879–0.998) and 0.899 (0.840–0.962), respectively at FN, and the OR for diabetes mellitus was 1.103 (1.017–1.196) at LS in men. In postmenopausal women, the OR for hypertension was 1.133 (1.029–1.246) at LS.
Conclusions
Low BMD was especially associated with MS in South Korean men.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risks of osteoporosis and cardiovascular disease increase with age, and these conditions cause high levels of morbidity and mortality in the elderly [1, 2]. Postmenopausal women are at high risk of osteoporosis and cardiovascular disease due to decreases in hormones, and it has been reported that 64 % of women who experience sudden death related to heart disease showed no prior signs [3]. Also, patients with osteoporosis have no clear symptoms until osteoporotic fractures develop. Therefore, early diagnosis and prevention of osteoporosis and cardiovascular disease is an important health issue.
Some studies have shown that low bone mineral density (BMD) is related with the incidence of cardiovascular diseases in postmenopausal women [4–6]. For example, there was a study which showed that postmenopausal women with stroke had low BMD at the femur neck [7]. Even in the Framingham study, the BMD of women who had coronary heart disease and stroke was typically low [8]. These cardiovascular diseases are associated with risk factors such as abdominal obesity, high blood pressure, and dyslipidemia, which make up the definition of metabolic syndrome (MS) [9]. MS is known to be the pre-condition before development of cardiovascular diseases and diabetes mellitus [10, 11], and the prevalence of MS is increasing. Currently, 25 % of the general population in the USA has MS, and the prevalence among individuals who are over 50 years of age is approximately 45 % [12, 13]. According to the 2005 Korea National Health and Nutrition Examination Survey (KNHANES), 32.9 % of men and 31.8 % of women had MS [14].
There have also been some studies of the relationship between MS and BMD [15–18]. According to the Camargo cohort study, Caucasian postmenopausal women with MS had higher BMD than postmenopausal women without MS at the lumbar spine (LS), femoral neck (FN), and total hip (TH) after adjusting for age, but there were no significant differences in BMD in men with and without MS [15]. In the National Health and Nutrition Examination Survey (NHANES) III, which enrolled 8,197 Americans, people with MS had higher FN BMD than those without MS [16]. However, in the Rancho Bernardo Study (RBS), which targeted Caucasian men and postmenopausal women, men with MS showed distinctly lower BMD than men without MS after adjustment with covariates [17]. Another study that targeted Koreans showed similar results. MS had a negative association with FN BMD in men, but no association was found in postmenopausal women [18]. The results of these last two studies conflict with those of the two aforementioned studies [15, 16]. In addition, some previous studies that targeted Korean men and women did not coincide in results [18, 19]. Therefore, we studied the relationship between BMD and MS in Korean men and women, using data from the Korean National Health Examination and Nutrition Survey (KHNANES) conducted in 2008–2010.
Subjects and methods
Subjects
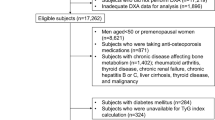
We used data from the KNHANES conducted between 2008 and 2010 by the Korea Centers for Disease Control and Prevention and the Korean Ministry of Health and Welfare. A total of 21,811 subjects (12,417 men and 13,487 women) between the ages of 20 and 85 were included in the KNHANES. The survey was made up of three parts: a health interview survey, a health examination survey, and a nutrition survey. KNHANES represents a nationwide study of non-institutionalized civilians and used a stratified and multistage probability sampling design with a rolling survey-sampling model. The sampling units were based on household unit data from the 2005 National Census Registry, which includes age, sex, and geographic area. Using a structured questionnaire, trained interviewers conducted face-to-face interviews.
Only subjects who were measured for BMD were included in the present analysis. Subjects who presented with thyroid disease (n = 342), chronic hepatitis B or C (n = 122), liver cirrhosis (n = 34), chronic kidney disease (n = 49), cancer (n = 276), pregnancy (n = 133), or pulmonary and extrapulmonary tuberculosis (n = 29) were excluded. Subjects who had histories of osteoporosis treatment (n = 438), hormone replacement therapy (n = 616), or hysterectomy (n = 404) were also excluded. Those who did not answer questions about past medical histories (n = 153) and those who had not fasted for more than 8 h before measurement (n = 870) were also excluded. A total of 14,485 subjects were finally included in the present study.
The subjects were divided into three groups by gender and menopause status: 6,659 men, 4,547 premenopausal women, and 3,279 postmenopausal women. Subjects were surveyed regarding age, physical activities, and current smoking and drinking statuses. We surveyed physical activities using the International Physical Activity Questionnaire [20]. Subjects were divided into either exercise group or non-exercise group. Regular exercise group includes subjects who exercised moderately more than five times a week for more than 30 min per one session or subjects who exercised intensively more than three times a week for more than 20 min per one session. Postmenopausal status was defined by the absence of menses for at least 1 year. The study protocol was approved by the Korean Ministry of Health and Welfare, and the study was conducted according to the Ethical Principles for Medical Research Involving Human Subjects as defined by the Helsinki Declaration. All subjects provided written consent.
Anthropometric measurements
A trained staff member took measurements of the subjects. Waist circumference (WC) was measured to the nearest 0.1 cm on a horizontal plane at the midpoint level between the iliac crest and the costal margin at the end of normal expiration. The heights (centimeters) and weights (kilograms) of the subjects were measured to the nearest 0.1 cm and 0.1 kg, respectively, with light clothing on and shoes removed. Body mass index (BMI) was calculated by dividing weight (kilograms) by the square of height (square meters). Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured three times using a mercury sphygmomanometer (Baumanometer; W. A. Baum Co., Inc., Copiague, NY, USA). Each subject was seated and rested for at least 5 min before BP was measured. The final BP value was calculated by taking the average of the second and third measurements. We used average BP values for statistical analysis.
Biochemical measurements
Blood samples were taken after a minimum of 8 h of fasting. Serum insulin levels were measured by immunoradiometric assay using the 1470 Wizard Gamma Counter (PerkinElmer, Turku, Finland). The coefficient of variation of the assays for serum insulin was 1.2 %. The serum levels of fasting blood glucose (FBG), total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), triglyceride (TG), low-density lipoprotein-cholesterol (LDL-C), white blood cell (WBC) count, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) were measured enzymatically using a Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan) after delivering the samples to the Central Testing Institute in Seoul, Korea. Insulin resistance was calculated using the Homeostasis Model Assessment of estimated insulin resistance (HOMA-IR) which was obtained by the following formula: fasting insulin [microunits per milliliter] × fasting glucose [milligramse per deciliter]/405 [21].
Definition of metabolic syndrome
MS was defined according to the American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement (AHA/NHLBI) criteria for Asians [10]. For the diagnosis of MS, three or more of the following criteria must be fulfilled: WC ≥ 90 cm in men and ≥80 cm in women, fasting TG ≥ 150 mg/dL or use of lipid-lowering medication, HDL-C < 40 mg/dL in men and <50 mg/dL in women or use of medication, BP ≥ 130/85 mmHg or use of antihypertensive medication, and FBG ≥ 100 mg/dL or current use of anti-diabetes medication.
BMD measurement
In the KNHANES, whole body dual-energy X-ray absorptiometry (DXA) was performed with a QDR Discovery (formerly known as the QDR 4500A) fan beam densitometer (Hologic, Inc., Bedford, MA, USA) following procedures recommended by the manufacturer. All subjects were dressed in light clothing and removed all jewelry and other items that could hinder the examination. BMD were measured at LS, FN, TH, trochanter, and intertrochanter sites. The results of DXA were analyzed using the standard techniques of the Korean Society of Osteoporosis and Hologic Discovery software (version 13.1).
Statistical analyses
Data are presented as either means ± standard errors (SEs) or as percentages (SE). In order to compare baseline characteristics, the chi-square test was used for categorical variables and analysis of variables (ANOVA) was used for continuous variables. Analysis of covariance (ANCOVA) was used to compare the BMD levels of subjects with and without MS at the LS, FN, and TH after adjusting for covariates. ANCOVA was also used to compare the BMD at the LS, FN, and TH after adjusting for covariates according to the number of MS components. The covariates included age, BMI, current smoking and alcohol statuses, and regular physical exercise. Age-adjusted linear regressions were used to examine the relationships between BMD and cardiometabolic risk factors. Using multivariable logistic regression analysis, odds ratio (OR) and 95 % confidence interval (CI) of an increase in BMD (0.1 g/cm2) for major cardiometabolic risk factors were obtained. All statistical tests were two-tailed, and statistical significance was defined as p < 0.05. The SAS software package version 9.2 for Windows (SAS institute, Cary, NC, USA) was used for all analyses.
Results
There are differences in all baseline characteristics such as anthropometric measurements, biochemical indexes, and BMD among men, premenopausal, and postmenopausal women (Table 1). On average, men have higher percentage of current smoking, alcohol drinking, and higher levels of regular physical exercise than women. Although premenopausal women have lower WC (74.85 ± 0.21 cm), BMI (22.54 ± 0.07 kg/m2), TG (93.59 ± 1.30 mg/dL), and MS (11.73 ± 0.60 %), the HDL-C level (57.01 ± 0.23 mg/dL) of this group is higher than those of the other two groups.
Table 2 shows the differences in BMD according to MS in both genders. For men, the BMD of the MS (+) group is significantly lower than that of the MS (−) group after adjusting for covariates at TH and FN (p = 0.030 and p < 0.001, respectively). On the other hand, premenopausal women with MS have significantly lower BMD than those without MS, at all sites, before adjustment. However, there is no difference in BMD according to MS after adjustment with covariates in premenopausal and postmenopausal women.
We analyzed the changes in BMD according to the number of MS components at the LS, TH, and FN (Table 3). In men, as the number of components increased, BMD decreases significantly after adjusting for covariates at FN and TH. Unlike men, premenopausal and postmenopausal women do not show any significant change in BMD at any site.
Table 4 shows the association of LS, TH, and FN BMD with cardiometabolic risk factors by multivariable-adjusted linear regression. In men, BMD shows positive correlations with BMI and HDL-C. Meanwhile, BMD is negatively correlated with insulin, HOMA-IR, TG, AST, and ALT at all three sites (p < 0.05). WBC count is also negatively correlated with TH and FN (β = −0.81, −0.69; both p < 0.001 for TH, FN, respectively). The correlation between BMD and WC is negative only at the TH (β = −2.41; p = 0.007). Similarly to the results seen in men, BMI shows a positive correlation with BMD at all three sites in pre- and postmenopausal women. In premenopausal women, BMD is negatively correlated with HOMA-IR at TH and FN, but not LS (β = −0.37, −0.33; p = 0.034, 0.036 for TH, FN, respectively). In postmenopausal women, the correlation between BMD and cardiometabolic risk factor is not consistent except for WBC count at TH and FN (β = −1.45, −1.61; all p < 0.001, for TH, FN, respectively).
Table 5 shows the ORs (95 % CI) of every increment of 0.1 g/cm2 in LS, TH, and FN BMD for each cardiometabolic risk factor after adjusting for covariates. The ORs for obesity and abdominal obesity are all greater than 1 at all sites in both genders. In men, the ORs for hypertension (HTN) and MS are 0.937 (0.879–0.998) and 0.899 (0.840–0.962), respectively, at FN. DM is only associated with an increase of LS BMD (OR = 1.103, 95 % CI 1.017–1.196). In postmenopausal women, an increase in LS BMD is associated with a higher OR of HTN (OR = 1.133, 95 % CI 1.029–1.246).
Discussion
In this study, we found that men with MS had lower BMD than men without MS. In addition, low BMD was associated with a prevalence of cardiometabolic risk factors and a number of MS components, especially in men. The relationship between BMD and cardiometabolic risk factors in women was not consistent with results in men.
Cardiometabolic risk factors such as abdominal obesity, insulin resistance, hypertension, and dyslipidemia are included in the definition of MS [22]. Recently, many studies have found that components of MS, such as hypertriglyceridemia, low HDL-C, and abdominal obesity, are related to low BMD in postmenopausal women and men [15–17]. Although the mechanism governing the relationship between MS and low BMD is unclear, it is worthy to note that adipose cells and osteoblasts originate from the same mesenchymal stem cells [23]. Also, the fact that many types of cytokines and peroxisome proliferator-activated receptor-γ have effects in the differentiation and growth of the two cell types can explain the relationship as well [24]. This finding suggests a linkage between the two diseases.
Generally, people with high BMI have high BMD compared to people with low BMI because high weight causes mechanical stress on the bone, which is leading to bone hardness [25]. So, men with MS may have high possibility to have a higher BMD than men without MS. However, this assumption was not consistent in the many studies that analyzed BMD according to gender and MS. In the Camargo cohort study, which was conducted in 495 Caucasian men and 1,013 Caucasian postmenopausal women, postmenopausal women with MS had higher BMD than the control group at LS, FN, and TH after adjusting for age, but there were no significant differences in men [15]. Kinjo et al. found that both genders with MS had higher FN BMD than those without MS in the NHANES III study, which enrolled 8,197 Americans [16]. These two studies showed positive correlations between MS and BMD. But some other studies showed opposite results. In the RBS, which included 417 Caucasian men and 671 postmenopausal Caucasian women, men with MS had lower FN BMD than men without MS, but there was no relationship between BMD and MS in postmenopausal women after adjustment for all covariates [17]. Also, in a French cohort study (the MINOS study) that included 762 men, the group with MS had lower BMD than the group without MS [26]. Like the present study, Kim et al. studied 1,780 Korean men and 1,108 postmenopausal Korean women and found similar results only in men with MS at FN BMD [18].
Most studies commented that the major cause of the negative association between BMD and MS in men was abdominal obesity, which is representative of insulin resistance. In the present study, WC had a negative correlation with TH BMD, and HOMA-IR was negatively associated with LS, TH, and FN BMD in men with MS (Table 4). Many cytokines, derived from adipose tissue, can contribute to an increase in insulin resistance. Adipokines, such as leptin and adiponectin, have been associated with MS and central obesity [27]. Increased levels of leptin stimulate proinflammatory cytokines including interleukins 6 and 18, and tumor necrosis factor-α in people with abdominal obesity, and these cytokines promote bone resorption [28, 29]. Furthermore, numerous studies have revealed that these adipokines are negatively associated with BMD [30, 31]. However, in the present study, such association is not found in postmenopausal women. The difference in association between BMD and MS by gender can be partially explained by the different fat distribution in men and women [32, 33]. Caucasian men with MS have higher visceral fat than women with MS even at the same WC [34, 35]. Korean men with MS are also likely to have a higher visceral/subcutaneous adipose tissue ratio than women with MS [36]. Compared to Caucasians, Asians tend to have higher levels of visceral fat at the same BMI [37], and therefore, we postulated that Korean men with MS may be more prone to low BMD than women with MS.
Another explanation for this different association by gender is hormonal dysregulation. Jankowska et al. [38] examined the hormonal effects of adipose tissue on BMD and reported that adipose tissue in postmenopausal women was a source of extra-ovarian estrogen that protected against bone loss. Meanwhile, visceral adipose tissue could cause several hormonal and metabolic dysregulation by an increase in estrogen levels [39], and a decrease of androgen and growth hormone levels in men [40]. Generally, levels of testosterone, which stimulates bone formation, were decreased in men with MS [41]. Therefore, we suppose that the negative effects of increased insulin resistance and hormonal dysregulation on BMD are greater than the positive effects of weight on BMD in men with MS. But more precise and prospective studies are needed to confirm these results.
This study revealed a negative association between TG and BMD in men, but not in postmenopausal women. In contrast, Kim et al.[18] did not find a relationship between FN BMD and TG in men, but found that FN BMD was negatively correlated with TG in postmenopausal women (β = − 0.097, p = 0.001). Many other studies, however, found that TG was positively associated with BMD. Brownbill et al. [42] found that TG and TC were positively correlated with the femoral shaft and total body BMD, respectively, in Caucasian postmenopausal women. Furthermore, Adami et al. [43] found that TG and LDL-C levels were positively correlated with the BMDs of the hip and LS in 746 Italian men and women. In addition, Turkish postmenopausal women with spinal fractures had lower levels of TG, TC, and LDL-C than those without fractures [44]. There is a hypothesis that explains the relationship between lipid and BMD involving the oxidization of lipid. Oxidized lipids enhance the inflammatory process of the arterial wall and the formation of atherosclerotic plaques, but inhibit the calcification and differentiation of osteoblasts [45]. However, this mechanism was only suitable for men in our study. Since the results on the relationship between TG and BMD are very controversial, further evaluations to investigate the mechanism are needed.
The present study does have several limitations. First, it was impossible to reveal a causal relationship between low BMD and MS in this cross-sectional study. Therefore, prospective studies are needed. Second, we did not analyze data regarding the duration of menopause in postmenopausal women. Last, we only checked WC for abdominal obesity. A more accurate method such as abdominal computed tomography (CT) would be preferable for the measurement of visceral fat, but that is costly and would require radiation exposure. Although the AHA/NHLBI criteria for MS include WC, abdominal CT can be a more precise method to clarify the role of subcutaneous and visceral fat in the relationship between BMD and cardiovascular risk factors.
Despite these limitations, there are several strengths to our study. This is the first study to examine the association between MS and BMD at multiple sites (LS, TH, and FN) using a sample population representative of Korean adults. Previous Korean studies only examined either FN or vertebral BMD and included subjects who had undergone a private health examination in a university hospital [18, 19]. Those studies were not representative of the whole Korean population and might have selection bias.
In conclusion, low BMD is related to MS after adjusting for covariates, and this trend is more prominent in Korean men than in Korean women. We recommend careful examinations for cardiometabolic risk factors in men with low BMD. In addition, since low BMD is related to insulin resistance in Korean men, further prospective studies will be required to reveal any causal relationships between osteoporosis and cardiovascular events.
References
Braithwaite RS, Col NF, Wong JB (2003) Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 51(3):364–370
Van Der Klift M, Pols HA, Geleijnse JM, Van Der Kuip DA, Hofman A, De Laet CE (2002) Bone mineral density and mortality in elderly men and women: the Rotterdam Study. Bone 30(4):643–648
Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J, American Heart Association Statistics C, Stroke Statistics S (2010) Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation 121(7):e46–e215. doi:10.1161/circulationaha.109.192667
Browner WS, Pressman AR, Nevitt MC, Cauley JA, Cummings SR (1993) Association between low bone density and stroke in elderly women. The study of osteoporotic fractures. Stroke; a J of Cerebral Circulation 24(7):940–946
Mussolino ME, Gillum RF (2006) Bone mineral density and hypertension prevalence in postmenopausal women: results from the Third National Health and Nutrition Examination Survey. Ann Epidemiol 16(5):395–399. doi:10.1016/j.annepidem.2005.06.051
Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR (2005) Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone and Mineral Res: The Official J of the Am Soc for Bone and Mineral Res 20(11):1912–1920. doi:10.1359/jbmr.050711
Jørgensen L, Engstad T, Jacobsen BK (2001) Bone mineral density in acute stroke patients: low bone mineral density may predict first stroke in women. Stroke; a J of Cerebral Circulation 32(1):47–51
Samelson EJ, Kiel DP, Broe KE, Zhang Y, Cupples LA, Hannan MT, Wilson PW, Levy D, Williams SA, Vaccarino V (2004) Metacarpal cortical area and risk of coronary heart disease: the Framingham Study. Am J Epidemiol 159(6):589–595
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A (2001) Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285(19):2486–2497
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F, American Heart A, National Heart L, Blood I (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112(17):2735–2752. doi:10.1161/circulationaha.105.169404
Rana JS, Nieuwdorp M, Jukema JW, Kastelein JJ (2007) Cardiovascular metabolic syndrome—an interplay of, obesity, inflammation, diabetes and coronary heart disease. Diabetes, obesity & metabolism 9(3):218–232. doi:10.1111/j.1463-1326.2006.00594.x
National Cholesterol Education Program Expert Panel on Detection E, Treatment of High Blood Cholesterol in A (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106(25):3143–3421
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288(21):2709–2716
Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention (2006) The Third Korea National Health and Nutrition Examination Survey (KNHANES III), 2005: Health Examination. Korea Centers for Disease Control and Prevention, Seoul
Hernández JL, Olmos JM, Pariente E, Martínez J, Valero C, García-Velasco P, Nan D, Llorca J, González-Macías J (2010) Metabolic syndrome and bone metabolism: the Camargo Cohort study. Menopause (New York, NY) 17(5):955–961. doi:10.1097/gme.0b013e3181e39a15
Kinjo M, Setoguchi S, Solomon DH (2007) Bone mineral density in adults with the metabolic syndrome: analysis in a population-based U.S. sample. J Clin Endocrinol Metab 92(11):4161–4164. doi:10.1210/jc.2007-0757
von Muhlen D, Safii S, Jassal SK, Svartberg J, Barrett-Connor E (2007) Associations between the metabolic syndrome and bone health in older men and women: the Rancho Bernardo Study. Osteoporosis Int 18(10):1337–1344. doi:10.1007/s00198-007-0385-1
Kim HY, Choe JW, Kim HK, Bae SJ, Kim BJ, Lee SH, Koh JM, Han KO, Park HM, Kim GS (2010) Negative association between metabolic syndrome and bone mineral density in Koreans, especially in men. Calcif Tissue Int 86(5):350–358. doi:10.1007/s00223-010-9347-2
Hwang DK, Choi HJ (2010) The relationship between low bone mass and metabolic syndrome in Korean women. Osteoporosis Int 21(3):425–431. doi:10.1007/s00198-009-0990-2
Hagströmer M, Oja P, Sjöström M (2006) The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutrition 9(6):755–762
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28(7):412–419
Sakkinen PA, Wahl P, Cushman M, Lewis MR, Tracy RP (2000) Clustering of procoagulation, inflammation, and fibrinolysis variables with metabolic factors in insulin resistance syndrome. Am J Epidemiol 152(10):897–907
Rosen CJ, Bouxsein ML (2006) Mechanisms of disease: is osteoporosis the obesity of bone? Nat Clin Pract Rheumatol 2(1):35–43. doi:10.1038/ncprheum0070
Lazarenko OP, Rzonca SO, Hogue WR, Swain FL, Suva LJ, Lecka-Czernik B (2007) Rosiglitazone induces decreases in bone mass and strength that are reminiscent of aged bone. Endocrinology 148(6):2669–2680. doi:10.1210/en.2006-1587
Beck TJ, Petit MA, Wu G, LeBoff MS, Cauley JA, Chen Z (2009) Does obesity really make the femur stronger? BMD, geometry, and fracture incidence in the women’s health initiative-observational study. J Bone and Mineral Res 24(8):1369–1379. doi:10.1359/jbmr.090307
Szulc P, Varennes A, Delmas PD, Goudable J, Chapurlat R (2010) Men with metabolic syndrome have lower bone mineral density but lower fracture risk—the MINOS study. J Bone and Mineral Res 25(6):1446–1454. doi:10.1002/jbmr.13
Rasouli N, Kern PA (2008) Adipocytokines and the metabolic complications of obesity. J Clin Endocrinol Metab 93(11 Suppl 1):S64–S73. doi:10.1210/jc.2008-1613
Wellen KE, Hotamisligil GS (2003) Obesity-induced inflammatory changes in adipose tissue. J Clin Invest 112(12):1785–1788. doi:10.1172/jci20514
Thomas T, Burguera B (2002) Is leptin the link between fat and bone mass? J Bone and Mineral Res 17(9):1563–1569. doi:10.1359/jbmr.2002.17.9.1563
Ağbaht K, Gürlek A, Karakaya J, Bayraktar M (2009) Circulating adiponectin represents a biomarker of the association between adiposity and bone mineral density. Endocrine 35(3):371–379. doi:10.1007/s12020-009-9158-2
Barbour KE, Zmuda JM, Boudreau R, Strotmeyer ES, Horwitz MJ, Evans RW, Kanaya AM, Harris TB, Cauley JA (2012) The effects of adiponectin and leptin on changes in bone mineral density. Osteoporosis Int 23(6):1699–1710. doi:10.1007/s00198-011-1768-x
Blaauw R, Albertse EC, Hough S (1996) Body fat distribution as a risk factor for osteoporosis. South African Med J = Suid-Afrikaanse tydskrif vir geneeskunde 86(9):1081–1084
Saarelainen J, Honkanen R, Kroger H, Tuppurainen M, Jurvelin JS, Niskanen L (2011) Body fat distribution is associated with lumbar spine bone density independently of body weight in postmenopausal women. Maturitas 69(1):86–90. doi:10.1016/j.maturitas.2011.02.009
Kuk JL, Lee S, Heymsfield SB, Ross R (2005) Waist circumference and abdominal adipose tissue distribution: influence of age and sex. Am J Clin Nutr 81(6):1330–1334
Schreiner PJ, Terry JG, Evans GW, Hinson WH, Crouse JR 3rd, Heiss G (1996) Sex-specific associations of magnetic resonance imaging-derived intra-abdominal and subcutaneous fat areas with conventional anthropometric indices. The Atherosclerosis Risk in Communities Study. Am J of Epidemiol 144(4):335–345
Kang SM, Yoon JW, Ahn HY, Kim SY, Lee KH, Shin H, Choi SH, Park KS, Jang HC, Lim S (2011) Android fat depot is more closely associated with metabolic syndrome than abdominal visceral fat in elderly people. PLoS One 6(11):e27694. doi:10.1371/journal.pone.0027694
Abate N, Chandalia M (2003) The impact of ethnicity on type 2 diabetes. J Diabetes Complications 17(1):39–58
Jankowska EA, Rogucka E, Medraś M (2001) Are general obesity and visceral adiposity in men linked to reduced bone mineral content resulting from normal ageing? A population-based study. Andrologia 33(6):384–389
Ljung T, Holm G, Friberg P, Andersson B, Bengtsson BA, Svensson J, Dallman M, McEwen B, Björntorp P (2000) The activity of the hypothalamic-pituitary-adrenal axis and the sympathetic nervous system in relation to waist/hip circumference ratio in men. Obes Res 8(7):487–495. doi:10.1038/oby.2000.61
Rosmond R, Björntorp P (2000) Low cortisol production in chronic stress. The connection stress-somatic disease is a challenge for future research. Lakartidningen 97(38):4120–4124
Muller M, Grobbee DE, den Tonkelaar I, Lamberts SW, van der Schouw YT (2005) Endogenous sex hormones and metabolic syndrome in aging men. J Clin Endocrinol Metab 90(5):2618–2623. doi:10.1210/jc.2004-1158
Brownbill RA, Ilich JZ (2006) Lipid profile and bone paradox: higher serum lipids are associated with higher bone mineral density in postmenopausal women. J Women’s Health 15(3):261–270. doi:10.1089/jwh.2006.15.261
Adami S, Braga V, Zamboni M, Gatti D, Rossini M, Bakri J, Battaglia E (2004) Relationship between lipids and bone mass in 2 cohorts of healthy women and men. Calcif Tissue Int 74(2):136–142. doi:10.1007/s00223-003-0050-4
Sivas F, Alemdaroğlu E, Elverici E, Kuluğ T, Kulug T, Ozoran K (2009) Serum lipid profile: its relationship with osteoporotic vertebrae fractures and bone mineral density in Turkish postmenopausal women. Rheumatol Int 29(8):885–890. doi:10.1007/s00296-008-0784-4
Parhami F, Morrow AD, Balucan J, Leitinger N, Watson AD, Tintut Y, Berliner JA, Demer LL (1997) Lipid oxidation products have opposite effects on calcifying vascular cell and bone cell differentiation. A possible explanation for the paradox of arterial calcification in osteoporotic patients. Arterioscler Thromb Vasc Biol 17(4):680–687
Acknowledgments
The authors thank the Korea Centers for Disease Control and Prevention, who performed the KNHANES. Thanks to Anna Kim for translating this manuscript into English.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, YH., Cho, KH., Choi, Y.S. et al. Low bone mineral density is associated with metabolic syndrome in South Korean men but not in women: The 2008–2010 Korean National Health and Nutrition Examination Survey. Arch Osteoporos 8, 142 (2013). https://doi.org/10.1007/s11657-013-0142-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-013-0142-3