Abstract
Background
There were ethnic differences in the prevalence of non-communicable diseases among the elderly in Malaysia.
Objective
To examine ethnic differences in participation in medical check-ups among the elderly.
Design
A nationally representative data set was employed. Multiple logistic regressions were utilised to examine the relationship between ethnicity and the likelihood of undergoing medical check-ups. The regressions were stratified by age, income, marital status, gender, household location, insurance access and health status. These variables were also controlled for in the regressions (including stratified regressions).
Participants
The respondents were required to be residents of Malaysia and not be institutionalised. Overall, 30,806 individuals were selected to be interviewed, but only 28,650 were actually interviewed, equivalent to a 93% response rate. Of those, only 2248 were used in the analyses, because 26,402 were others or below aged 60.
Main Measures
The dependent variable was participation in a medical check-up. The main independent variables were the three major ethnic groups in Malaysia (Malay, Chinese, Indian).
Key Results
Among the elderly aged 70–79 years, Chinese (aOR 1.89; 95% CI 1.28, 2.81) and Indians (aOR 2.39; 95% CI 1.20, 4.74) were more likely to undergo medical check-ups than Malays. Among the elderly with monthly incomes of ≤ RM999, Chinese (aOR 1.44; 95% CI 1.12, 1.85) and Indians (aOR 1.50; 95% CI 0.99, 2.28) were more likely to undergo medical check-ups than Malays. Indian males were more likely to undergo medical check-ups than Malay males (aOR 2.32; 95% CI 1.15, 4.67). Chinese with hypercholesterolaemia (aOR 1.45; 95% CI 1.07, 1.98) and hypertension (aOR 1.32; 95% CI 1.02, 1.72) were more likely to undergo medical check-ups than Malays.
Conclusions
There were ethnic differences in participation in medical check-ups among the elderly. These ethnic differences varied across age, income, marital status, gender, household location, insurance access and health status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The proportion of the ageing population in Malaysia has increased enormously. It rose from 5.2% in 1970 to 6.3% in 2000 and is projected to reach 9.8% by 2020.1 Reducing the prevalence of non-communicable diseases (NCDs) among the elderly is a public health concern. As argued by Teh,2 older people are more likely to use medical care and to also use more care compared with their younger counterparts because they have a higher likelihood of suffering from NCDs. The author highlighted that approximately 80% of Malaysia’s elderly have chronic health conditions that can result in premature mortality.2
Malaysia is a multi-ethnic country with three primary ethnicities (Malay, Chinese and Indian). Ethnic differences in the prevalence of NCDs among the Malaysian elderly have been well documented by Teh et al.3 The authors contend that about 35.4% of the Indian elderly have diabetes, compared with only 15.5% and 14.4% among Malays and Chinese, respectively.3 Moreover, the prevalence of coronary heart disease among the Indian elderly (22.1%) far outweighs the prevalence in Malays (7.1%) and Chinese (7.1%).3
NCDs are preventable if they are diagnosed early. However, the proportion of residents, especially the elderly, undergoing medical check-ups is low. As the report demonstrates, 13.6%, 28.7% and 48.5% of the elderly have undiagnosed diabetes, hypertension and hypercholesterolaemia, respectively.4 The prevalence of undiagnosed hypertension and hypercholesterolaemia is highest among Malays (18.6% and 41.4%), while the prevalence of undiagnosed diabetes is highest among Indians (11.9%).4 Despite the low participation rate in medical check-ups, only a few studies have examined which groups of the elderly undergo medical check-ups in Malaysia. Previous researchers have investigated factors affecting decisions of the elderly to participate in medical check-ups, but they did not analyse ethnic differences in participation in medical check-ups in detail.5, 6
We attempt to contribute to the literature in three ways. First, our study is the first of its kind that uses a nationally representative data set with a large sample size (n = 2248) to examine ethnic differences in participation in medical check-ups among the elderly in Malaysia. Second, the country of interest, Malaysia, is a fast-growing developing country with a high prevalence of NCDs, lacking studies related to participation in medical check-ups. Third, multivariate analyses stratified by age, income, marital status, gender, household location, insurance access and health status are conducted. Findings of any ethnic differences in participation in medical check-ups in these subgroups may assist policymakers in developing more effective intervention measures.
METHODS
Data
Secondary analysis of the Malaysian National Health and Morbidity Survey (NHMS) 2011 was performed.7 In the survey, a two-stage stratified random sampling method was used. First, 794 enumeration block (EBs) were selected from a total of 75,000 EBs. Of the selected EBs, 484 were in urban areas (≥10,000 population) and 310 were in rural areas (< 10,000 population). Second, 12 living quarters (LQs) were randomly chosen from each selected EB. All of the household members who resided in the selected LQs were interviewed. The exclusion criterion was institutionalised individuals, such as those staying at hotels, hospitals and prisons, who were not selected for an interview. Overall, 30,806 individuals were selected for an interview, but only 28,650 were actually interviewed, which was equivalent to the response rate of 93%. Given this high response rate, non-response bias was not an issue.8
Bilingual (Malay, English) structured questionnaires were used by the interviewers to conduct face-to-face interviews. The respondents’ demographic and health profiles were recorded during the survey. Written consent forms were distributed among the respondents before the interview. Only those who signed the forms were allowed to be interviewed. Although the NHMS 2011 is not the latest dataset, it is nationally representative and has a large sample size. Because of the 2-year window, the latest NHMS available to the public is the NHMS 2017.9 However, it is an adolescent health survey and does not have information on medical check-ups. Hence, it was not used. Since the present study uses a secondary data analysis, ethical approval is not necessary. Nevertheless, we have sought permission to use the data from the Ministry of Health Malaysia.
Variables
Participation in medical check-ups was used as the dependent variable. In the survey, the respondents were asked: ‘Have you had your blood glucose measured in the past 12 months?’ A similar question was used for blood cholesterol and blood pressure tests. The respondents were coded as medical check-up participants if they answered ‘yes’ to any of these three questions. Given that blood glucose, blood cholesterol and blood pressure tests are often conducted simultaneously, these three tests were combined to form a single dependent variable. All of the information was self-reported by the respondents. We focused on these three tests because diabetes, coronary heart disease and hypertension are among the most common chronic diseases among Malaysian elderly.3 Additionally, these three tests represent the most basic medical check-ups recommended by the Ministry of Health Malaysia.
The main independent variable was ethnicity. It was categorised into three groups: Malay, Chinese and Indian. We dropped the respondents from other ethnic groups (others), because others are not the primary ethnic group in Malaysia and only a few respondents were others. In our sample, only 249 respondents were others. Malaysia does not have ‘multi-racial’ ethnicity. None of the Malaysians we identified had more than one ethnicity.
Other demographic and health variables were used as controlled variables. These included age, monthly individual income (in Ringgit Malaysia (RM)), education, marital status, gender, household location, insurance access (employer-, government- and private-sponsored insurance) and health status (diabetes, hypercholesterolaemia and hypertension). These variables were selected based on previous studies.10,11,12,13,14,15,16,17
In terms of insurance access, three variables were used: employer-, government- and private-sponsored insurance. In order to determine whether the respondents had any form of insurances, the respondents were asked: ‘Are you covered by any employer-sponsored insurance?’, ‘Are you covered by any government Guarantee Letter for health care?’ and ‘Are you covered by any private health insurance?’ The respondents were considered to have employer-, government- or private-sponsored insurance if they answered ‘yes’ to the first, second or third question, respectively. The details of insurance access among the elderly in Malaysia have been described elsewhere.5, 18
The respondents’ health status was measured by three variables: diabetes, hypercholesterolaemia and hypertension. In order to determine whether the respondents had any of these chronic diseases, the respondents’ blood glucose, blood cholesterol and blood pressure were assessed by health professionals during the survey. The respondents were considered to have diabetes and hypercholesterolaemia if their fasting capillary blood glucose was ≥6.1 mmol/L and total blood cholesterol was ≥5.2 mmol/L. The respondents were considered to have hypertension if their systolic and diastolic blood pressure was ≥ 140 mmHg and ≥ 90 mmHg, respectively.
Statistical Analysis
The elderly refers to adults aged ≥ 60 years.19 In our sample, 26,153 respondents were excluded from the total sample because they were below aged 60. After deleting others and the non-elderly, only 2248 respondents were used for analyses. We constructed a two-way contingency table to cross-classify the sample according to ethnicity and participation in medical check-ups. We then employed the Pearson χ2 test of independence to compare the proportions. Multiple logistic regressions were used to examine the effect of ethnicity on the odds of undergoing a medical check-up. In order to draw ceteris paribus conclusions and avoid omitted variable issues, other demographic (age, income, education, marital status, gender, household location and insurance access) and health (diabetes, hypercholesterolaemia and hypertension) variables were controlled for in the regressions. Additionally, we stratified the regressions into several subgroups (age, income, marital status, gender, household location, insurance access, diabetes, hypercholesterolaemia and hypertension). Since age and years of schooling were highly correlated, we did not stratify the regressions by education. Age, income, education, marital status, gender, household location, insurance access, diabetes, hypercholesterolaemia and hypertension were also controlled for in the stratified regressions. Marginal effects were calculated and presented in the ‘RESULTS’ section and accompanying tables. All of the analyses were performed using Stata.20
RESULTS
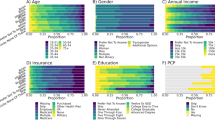
The majority of the sample were Malays (60.23%), followed by Chinese (32.38%) and Indians (7.38%). This ethnic structure was quite similar to that of the Malaysian’s aged population (≥60 years) (57.25% (Malays), 35.82% (Chinese), 6.93% (Indians)).19 Most of the respondents were aged 60–69 years (57.83–63.66%) and had a monthly individual income of ≤ RM999 (66.62–80.12%). The majority of the respondents did not have employer- (96.39–98.89%), government- (71.20–89.01%) or private-sponsored insurance (85.71–97.27%). A large proportion of the respondents had hypercholesterolaemia (50.69–56.50%) and hypertension (67.47–72.08%) (Table 1).
There were no significant differences in the proportion of people undergoing medical check-up across ethnicities (Table 2). The results of multiple logistic regression derived from the total sample showed a possible relationship between ethnicity and participation in medical check-ups. Controlling for all other demographic and health variables, Chinese were 5.3% more likely to undergo medical check-ups than Malays [p = 0.041] (Table 3).
Compared with Malays aged 70–79 years, Chinese [p = 0.002] and Indians [p = 0.013] had a 14.7% and 18.4% higher probability of undergoing medical check-ups, respectively. The probability of undergoing medical check-ups was 9.2% and 8.8% higher among Indians [p = 0.043] and Chinese [p = 0.005], respectively, compared with Malays in the subgroup of the elderly with monthly incomes of ≤RM999 (Table 4).
Widowed/divorced Chinese were 10.2% more likely to undergo medical check-ups than Malays [p = 0.033]. The probability of undergoing medical check-ups was 17.8% higher among Indians compared with Malays in the subgroup of males [p = 0.018]. Compared with Malays, Chinese [p = 0.022] and Indians [p = 0.032] were 7.8% and 10.7% more likely to undergo medical check-ups, respectively, in the urban subgroup.
Among those who did not have government-sponsored insurance, Chinese were 5.3% more likely to undergo medical check-ups than Malays [p = 0.042]. Chinese [p = 0.001] and Indians [p = 0.018] who had diabetes were 12.3% and 12.1% more likely to undergo medical check-ups, respectively, than their Malay counterparts. Compared with Malays, Chinese who had hypercholesterolaemia [p = 0.018] and hypertension [p = 0.038] were 8.2% and 6.2% more likely to undergo medical check-ups, respectively.
DISCUSSION
The multiple regressions show significant ethnic differences in participation in medical check-ups. Overall, the Chinese elderly are more likely to undergo medical check-ups than the Malay elderly. In particular, Chinese with diabetes, hypercholesterolaemia and hypertension have a higher likelihood of undergoing medical check-ups compared with their Malay counterparts. This could explain why the Chinese elderly are likely to participate in medical check-ups. They may have a high risk of suffering from diabetes, hypercholesterolaemia and hypertension, and thus, they are advised to undergo more medical check-ups. Medical check-ups are considered routine or follow-up care to them.
Previous studies have found that age was positively associated with participation in health screening.11, 12, 15 This is because older people have a higher risk of developing diseases than younger people.14 Hence, it is important to understand how the relationship between ethnicity and participation in medical check-ups varies across age. As our findings demonstrate, compared with Malays aged 70–79 years, Indians and Chinese of the same age are more likely to undergo medical check-ups. However, there are no ethnic differences in the likelihood of undergoing medical check-ups among the elderly aged 60–69 years and ≥80 years. This implies that if policymakers plan to encourage participation in medical check-ups among the elderly aged 70–79 years, special attention should be paid to Malays rather than Chinese and Indians. However, equal consideration should be given to all of the ethnic groups if the focus is the age groups spanning 60–69 and ≥80 years.
Findings from previous studies show that the elderly with higher household incomes are more likely to undergo health screenings than those with lower household incomes.5, 14, 16, 17 It appears that a low income is a barrier to participation in health screening, especially given that health insurance in Malaysia seldom covers the cost of preventive medical care.5, 14 Given these findings, we examine the association between ethnicity and participation in medical check-ups in the low-income group and find that Chinese and Indians are more likely to undergo medical check-ups than Malays. However, in the middle- and high-income groups, ethnicity does not determine participation in medical check-ups. An important policy implication of our findings is that if public health administrators want to encourage participation in medical check-ups among the elderly with poor financial backgrounds, they should concentrate more heavily on Malays than Chinese and Indians.
Among the widowed/divorced elderly, Chinese are more likely to undergo medical check-ups than Malays. This finding is crucial for policymakers given the previous findings that being unmarried is associated with a decreased likelihood of participation in health screening.11, 12 Policymakers are therefore encouraged to pay special attention to Malays if the objective of improving participation in medical check-ups among the elderly who are widowed/divorced is to be realised. However, if the targeted population is comprised of those who are single or married, intervention measures should not be designed based on ethnicity, because no ethnic differences in participation in medical check-ups are evidenced in this subgroup.
Compared with Malay males, Indian males are more likely to undergo medical check-ups. The significant Malay-Indian differences in the prevalence of NCDs in the subgroup of the male elderly may explain this outcome. As the findings of Teh et al.3 show, about 40.9% and 21.7% of Indian male elderly have diabetes and chronic heart disease, respectively, whereas only 16.4% and 8% of Malay male elderly have diabetes and chronic heart disease, respectively. However, because the proportion of Chinese male elderly who have diabetes (15.2%) and hypertension (8.9%) is quite similar to that of the Malay male elderly, it is unsurprising to find no significant Malay-Chinese differences in participation in medical check-ups.3 Our findings indicate that public health administrators should place their efforts into promoting participation in medical check-ups among all ethnic groups, with a focus on Malay and Chinese, if their purpose is to effectively increase the number of male elderly undergoing medical check-ups.
Since our findings show no ethnic differences in participation in medical check-ups among rural dwellers, no particular attention should be devoted to a specific ethnic group if the goal of increasing the participation rate for medical check-ups in rural areas is to be achieved. Instead, the elderly from all of the ethnic groups should be treated equally. However, if an intervention measure is designed to be directed toward encouraging participation in medical check-ups in urban areas, Malays should be the focus group, given that they are unlikely to undergo medical check-ups. While previous studies have consistently suggested that residing in urban areas was positively associated with participation in health screening because medical care services were more available in urban areas than in rural areas, they did not examine how participation in health screening in urban areas varied across ethnic groups.21, 22
Malaysia is different from the USA. The government does not provide the elderly with Medicare. Either the elderly buy their own insurance or are sponsored by their employers. Only retired government servants are eligible for government insurance. Therefore, only a small percentage of the elderly have insurance, especially in light of the fact that the majority are unemployed and do not have fixed incomes. Given this phenomenon, it is beneficial to gain insights into how ethnic differences in participation in medical check-ups vary across insurance access. Our findings reveal that Chinese who do not have government-sponsored insurance are more likely to undergo medical check-ups compared with Malays. However, there are no significant ethnic differences in participation in medical check-ups in the subgroups of employer- and private-sponsored insurance. This is unsurprising, because only a small percentage of respondents in our sample have insurance.
Several reasons may explain why the Malay elderly are less likely than the elderly from Chinese and Indian ethnic groups to undergo medical check-ups in various subgroups.3 First, the majority of the Malay elderly may find it unaffordable to participate in medical check-ups because they are of poor socioeconomic status. Second, the Malay elderly tend to live in rural areas, where medical care services are not widely available. Third, on average, the Malay elderly have low educational levels. Therefore, they are unlikely to understand the benefits of medical check-ups. In order to obtain a better understanding of how ethnicity influences participation in medical check-ups, a qualitative research interview should be conducted. This may well be a valuable direction for future research.
As pointed out by Quah,23 several factors related to the health belief model (HBM), such as knowledge of disease, perceived social sanctions and perception of disruption of normal activities, could explain preventive health behaviours among Malays, Chinese and Indians. Since some of the factors in HBM are related to cultural perceptions toward health care, acquiring a better understanding of cultural differences in access to health care is important for policy development. The direct effect of culture on health care practices was also evidenced in other studies.24, 25 The researchers found that cultural beliefs and practice were one of the main barriers to health screening among Hmong and Indian Americans. Moreover, O’Mahony and Donnelly26 found that Canada’s immigrant patients were likely to experience difficulties in accessing health care because of their views on health care maintenance that were influenced by cultural circumstances that were different from those of the residents. The immigrants had a higher tendency to rely on traditional medicine and spiritual beliefs than conventional health care to improve their health. It could, therefore, be concluded that cultural beliefs about health care should be assessed in making recommendations of frequency of check-up visits and health care maintenance among the elderly so that their chronic medical conditions could be addressed more effectively by the providers.
Our study has several limitations. First, the information on participation in medical check-ups is self-reported. Some respondents may fail to recall that they had undergone a medical check-up in the past 12 months, while others may report that they had participated in medical check-ups when they had not in fact undergone these services in the past 12 months. Unfortunately, we do not have access to the information about the respondents’ medical records to verify responses. Second, while the data used in our study is large, it is not up-to-date. Third, the causal relationship between participation in medical check-ups and the risk of suffering from NCDs cannot be identified because of cross-sectional data. Despite these limitations, our study offers important contributions to the extant literature, as well as policy development initiatives.
CONCLUSIONS
Considering the ethnic differences in the prevalence of NCDs, we examine how ethnic factors influence participation in medical check-ups. The population of interest is the elderly. Our findings reach the conclusion that the Malay elderly tend to have a lower likelihood of undergoing medical check-ups compared with the Chinese and Indian elderly. Therefore, it is important for public health administrators to pay greater attention to encouraging participation in medical check-ups among the Malay elderly.
References
Mafauzy M. The problems and challenges of the aging population of Malaysia. Malays J Med Sci 2000;7(1):1–3.
Tey NP. Population ageing in Malaysia. In: Abeykoon A, Murat N, Rocas G, Naraval AC, ed. Ageing: Thailand, Malaysia, Indonesia and Cambodia. Selangor: International Council on Management of Population Programmes (ICOMP); 2017.
Teh JKL, Tey NP, Ng ST. Ethnic and gender differentials in non-communicable diseases and self-rated health in Malaysia. PLoS One 2014;9(3):e91328.
Institute for Public Health. National Health and Morbidity Survey (NHMS) 2015. Kuala Lumpur: Institute for Public Health; 2015.
Cheah YK, Goh KL. Blood glucose screening among elderly Malaysians: Who to target? J Diabetes 2017;9(1):85–92.
Cheah YK, Tang CF. Factors influencing the use of preventive medical care in Malaysia: Evidence from National Health and Morbidity Survey data. Asian Econ J 2017;31(2):119–137.
Institute for Public Health. National Health and Morbidity Survey (NHMS) 2011. Kuala Lumpur: Institute for Public Health; 2011.
Fincham JE. Response rates and responsiveness for surveys, standards, and the journal. Am J Pharm Educ. 2008;72(2):article 43.
Institute for Public Health. National Health and Morbidity Survey (NHMS) 2017: Adolescent Health Survey 2017. Kuala Lumpur: Institute for Public Health; 2017.
Tung EL, Baig AA, Huang ES, Laiteerapong N, Chua KP. Racial and ethnic disparities in diabetes screening between Asian Americans and other adults: BRFSS 2012-2014. J Gen Intern Med 2017;32(4):423–429.
Chang Y, Cho B, Son KY, et al. Determinants of gastric cancer screening attendance in Korea: A multi-level analysis. BMC Cancer 2015;15:336.
Damiani G, Federico B, Basso D, et al. Socioeconomic disparities in the uptake of breast and cervical cancer screening in Italy: A cross sectional study. BMC Public Health 2012;12:99.
So WKW, Choi KC, Chan DNS, et al. Colorectal cancer screening behaviour and associated factors among Chinese aged 50 and above in Hong Kong – A population-based survey. Eur J Oncol Nurs 2012;16:413–418.
Lairson DR, Chan W, Newmark GR. Determinants of the demand for breast cancer screening among women veterans in the United States. Soc Sci Med 2005;61:1608–1617.
Sing MF, Leuraud K, Duport N. Characteristics of French people using organised colorectal cancer screening. Analysis of the 2010 French Health, Healthcare and Insurance Survey. Prev Med 2013;57:65–68.
Guessous I, Cullati S, Fedewa SA, et al. Prostate cancer screening in Switzerland: 20-year trends and socioeconomic disparities. Prev Med 2016;82:83–91.
Halliday T, Taira DA, Davis J, Chan H. Socioeconomic disparities in breast cancer screening in Hawaii. Prev Chronic Dis. 2007;4(4).
Cheah YK. The utilization of diagnostic tests among the elderly: Evidence from Malaysia. Socio Econ Plan Sci 2018;62:121–128.
Tey NP, Siraj SB, Kamaruzzaman SBB, et al. Aging in multi-ethnic Malaysia. Gerontol. 2016;56(4):603–609.
StataCorp. Stata Statistical Software: Release 13.1. College Station, TX: Stata Corporation; 2013.
Coughlin SS, Thompson TD. Colorectal cancer screening practices among men and women in rural and nonrural areas of the United States, 1999. J Rural Health 2004;20(2):118–124.
Coughlin SS, Leadbetter S, Richards T, Sabatino SA. Contextual analysis of breast and cervical cancer screening and factors associated with health care access among United States women, 2002. Soc Sci Med 2008;66:260–275.
Quah SR. The Health Belief Model and preventive health behaviour in Singapore. Soc Sci Med 1985;21:351–363.
Lee HY, Vang S. Barriers to cancer screening in Hmong Americans: The influence of health care accessibility, culture, and cancer literacy. J Community Health 2010;35:302–314.
Risendal B, Roe D, DeZapien J, Papenfuss M, Giuliaono A. Influence of health care, cost, and culture on breast cancer screening: Issues facing urban American Indian women. Prev Med 1999;29(6):501–509.
O’Mahony JM, Donnelly TT. The influence of culture on immigrant women’s mental health care experiences from the perspectives of health care providers. Issues Ment Health Nurs 2007;28:453–471.
Acknowledgements
The authors would like to thank the Director General of Health, Malaysia, for his permission to use the data from the National Health and Morbidity Survey 2011 and to publish this paper. The authors would also like to thank Kim-Leng Goh for his feedback and comments.
Funding
This research received funding from the Fundamental Research Grant Scheme (FRGS) (KOD SO 14218), which is sponsored by the Ministry of Education Malaysia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheah, Y.K., Meltzer, D. Ethnic Differences in Participation in Medical Check-ups Among the Elderly: Evidence from Malaysia. J GEN INTERN MED 35, 2680–2686 (2020). https://doi.org/10.1007/s11606-020-05766-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-020-05766-6