Abstract
Hmong Americans face high cancer mortality rates even in comparison to their Asian American counterparts, and report low utilization of cancer screenings. To date, no study has been conducted on the cultural barriers this population faces in undergoing cancer screenings. A systematic review of the literature was conducted to examine the existing knowledge regarding the barriers to cancer screening for Hmong Americans. Potential barriers were identified from this examination to include: health access factors (type of health insurance, ethnicity of provider, low English proficiency, and years spent in the U.S.); cultural factors (belief in the spiritual etiology of diseases, patriarchal values, modesty, and mistrust of the western medical system); and cancer literacy factors (cancer and prevention illiteracy). Based on this review, potential cultural and ethnic group-specific prevention strategies and cancer health policies are discussed to address these barriers and enhance screening behavior among the Hmong.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer poses a significant burden on Asian Americans, who are the only racial group to report cancer as the leading cause of death [1]. Mortality rates among Asian Americans for particular cancers, such as stomach and liver cancers, are roughly twice that of Non-Hispanic Whites [2]. Of particular concern are Hmong Americans—the fastest growing Asian American group in Minnesota and Wisconsin—who report high cancer mortality rates even in comparison to their Asian American counterparts [3]. For example, mortality rates among Hmong Americans for stomach cancer are 3.5 times higher than for Asian Americans overall, and 8.9 times higher than for Non-Hispanic Whites [4]. Average cervical cancer mortality rates for Hmong American women are 2.8 times higher than for all Asian American women, and 4.2 times higher than for Non-Hispanic White women [5].
The Hmong’s high mortality rate appears to correlate with the high prevalence of late stage cancer diagnosis seen in this population. Overall, the Hmong were found to be diagnosed with a later disease stage and a poorer disease grade of cancer than other Asian American subgroups [6]. In fact, data from the California Cancer Registry revealed that only 23.8% of Hmong cancer cases were diagnosed at an early stage [6].
The existing literature indicates that the high prevalence of late stage cancer diagnosis could be reflective of the Hmong’s underemployment of cancer screening tests. Hmong Americans are reported to have one of the lowest rates of cancer screening utilization [7]. For example, only 30% of Hmong women reported ever having undergone a mammography compared to 49% of Korean American women [8, 9]. Additionally, only 28% of Hmong women had ever had a Pap test done in comparison to 79% of all Asian American and Pacific Islanders and 95% of Whites [7, 10]. Moreover, no Hmong in Yang et al.’s study reported ever having undergone a colorectal exam or prostate-specific antigen test (PSA) [7].
Cancer screening has been shown to be effective in detecting cancer at early stages and preventing overall cancer-related mortalities [11–13]. Given the Hmong’s high cancer mortality rate and high prevalence of late stage diagnosis, it is critical to increase the cancer screening use of this population.
However, little is known about the barriers to cancer screening utilization among this population. The purpose of this review is to address this knowledge gap by systematically exploring scholarly literature to identify potential barriers to cancer screening among Hmong Americans and inform culturally and ethnic group-specific prevention strategies and cancer health policies for Hmong Americans. This comprehensive analysis will examine barriers in three major areas: (1) health access, (2) cultural, and (3) cancer literacy factors. As the extant literature in these areas is largely restricted to first-generation Hmong Americans who still practice traditional conventions, this review will consequently be focused primarily on first-generation Hmong Americans.
Hmong Americans
Background
The Hmong are an ethnic minority group of China who migrated to the Southeast Asian region in the nineteenth and twentieth centuries. During the Vietnam War, the Hmong allied with the U.S. against Vietnamese and Laotian communists. After Saigon fell in 1975 and the U.S. withdrew from the Southeast Asian region, the Hmong were persecuted by the new communist government for their involvement in the war. Subsequently, over 200,000 Hmong fled to refugee camps in neutral Thailand [14]. A majority of these refugees were relocated to the U.S., with the most current relocation wave occurring in 2005–2006. Recent data from the 2008 American Community Survey number the Hmong in the U.S. at ~221,948 [15]. California and Minnesota are thought to have the largest number of Hmong, with the Saint Paul-Minneapolis area boasting the largest Hmong population of any U.S. metro area [16].
Socio-Demographic Characteristics
Overall, Hmong Americans have large families (average of 6.2 persons), and are a young population (median of 16.1 years) [17, 18]. They report the lowest per capita income ($32,076) and highest poverty rates (38%) of any Asian American group [17, 19]. Despite gains in educational achievement since arriving in the U.S., the Hmong also report the lowest educational attainment of any Asian American group; about 40% hold a high school degree or higher [17, 19].
Hmong Americans typically practice either Shamanism or Christianity. Shamanism is a religious practice that functions under the principle that spirits, which reside in all living things, have a direct influence over an individual’s health and well-being [20, 21]. Roughly 66% of Hmong living in the Saint Paul-Minneapolis region, and over 60% of Hmong participants in studies conducted in California reported they practice Shamanism [22–24]. A national study estimated that 70% of Hmong living in the U.S. still practice Shamanism [25]. Even those who have converted to Christianity still maintain some Shamanist beliefs and practices [26, 27].
Methods
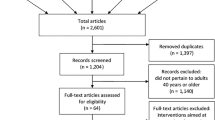
Articles analyzed in this study were obtained using Academic Search, CINHAL, PsycINFO, PubMed, Social Services Abstracts, and Social Work Abstracts databases. Our initial inclusion criteria consisted of articles which focused on Hmong Americans and covered any of the following topics: cancer mortality, screening, incidence, knowledge, or cultural beliefs. We employed the following keywords in combination with Hmong: cancer, screening, cancer belief, cancer literacy, cancer knowledge, cancer incidence, and cancer mortality. We looked at all studies which referred to Hmong in the title or abstract in these areas of research and examined them to see if they had any subgroup-level findings that were specific to this group. This yielded twelve unique articles, which we organized according to author, year, method, findings, and implications for practice and policy (Table 1).
Additionally, we utilized Klein and Bloom’s organizing framework to analyze each article’s contribution to the scholarly literature according to the following five categories: empiricism, technology, conceptualization, valuation, or commentary [28]. According to Klein and Bloom, articles in the empiricism category refer to those of a research nature, which contribute either quantitative or qualitative knowledge; technology pertains to those that provide information on measurement/assessment tools relevant to practice; conceptualization refers to articles that offer theoretical or abstract summaries of articles previously discussed in other categories; valuation papers provide ethical or moral positions that are critical to the profession; and commentaries contribute to the literature by taking a position on an issue [28]. The categorization of each article is presented in Table 1. Data provided in Table 1 was used to inform current statistics of cancer incidence, cancer mortality, and cancer knowledge and beliefs throughout this paper.
Because of the scarcity of available literature on cancer in the Hmong, our search was expanded to include articles focusing on illnesses and diseases in the Hmong in general. These articles were used to generate some insight into the impact of traditional Hmong cultural beliefs and practices on the Hmong’s preventive health behavior. The following keywords were used in combination with “Hmong”: health, health belief, prevention, illness, and disease. Furthermore, the reference sections of retrieved articles were manually searched for additional studies on the Hmong’s health beliefs. Online bibliographies provided by the Hmong Studies Internet Resource Center (www.hmongstudies.org/HmongBibliographies) were also perused for relevant articles. This extended search generated a total of 188 articles and these were reviewed and sorted to be used for this study. The primary criterion used for article inclusion was relevance to informing cancer screening behaviors in terms of heath access, culture, and cancer literacy dimensions of other illnesses. A final 26 articles from this secondary search were utilized for this study.
Results
Health Access Barriers
Health access barriers to cancer screening pertain to type of health insurance, race/ethnicity of health service providers, and immigration-related factors that negatively affect a population’s access to preventive healthcare utilization. The literature widely reports that Hmong Americans face a multitude of health access barriers to healthcare consumption [29–31]. As presented in Table 1, research reported specific health access barriers to cancer screening for Hmong Americans, including a lack of or inadequate health insurance, ethnicity of the healthcare provider, and linguistic difficulties [8].
Health Insurance
While many Hmong Americans have health insurance (mainly through Medicaid, one form of pubic health insurance), it has been reported that this type of health insurance appears to affect decisions to undergo cancer screening [8, 24]. Specifically, having public health insurance imposed barriers that limited access to healthcare. For instance, Gilman, Justice, Saepharn, & Charles reported that consumers with public health insurance faced challenges accessing healthcare, such as having a limited pool of healthcare providers who would accept Medicaid’s low reimbursement rate, and having to wait for long periods at public facilities in order to receive services [25]. In addition, Hmong Americans reported feeling stigmatized when utilizing Medicaid services. Specifically, Hmong participants in Wong et al.’s study reported feeling discriminated when using Medicaid insurance, which could contribute to their nonadherence to treatment and preventive health guidelines [24].
In contrast, it has been reported that having private health insurance has been found to have a positive impact on ever having undergone a cancer screening. Tanjasiri et al. reported that Hmong women were more likely to have undergone cancer screening if they had private health insurance [8]. Ayanian, Kohler, Abe, and Epstein suggested that women with private health insurance were more likely to have a regular physician and thus follow through cancer screening guidelines [32]. This is particularly critical given that having a regular physician who was acquainted with the patient’s medical history was identified as the most significant predictor for having undergone cancer screening [33]. Thus, while many Hmong are covered under public health insurance, obstructions to healthcare could still exist due to the nature in which public health care is utilized, and the negative connotations the Hmong associate with utilizing public health insurance.
Race/Ethnicity of Healthcare Provider
The race/ethnicity of health care providers appears to affect screening behaviors of Hmong Americans. Hmong patients who do not utilize Southeast Asian doctors were found to be more likely to have undergone cancer screenings [8]. Similar findings have been reported for other Southeast Asian groups [34, 35]. For instance, McPhee et al. found that for Vietnamese women, having a Vietnamese physician was negatively associated with ever having undergone a clinical breast examination [35]. While the primary reasons for these findings are not known, it has been suggested that this could be due to Southeast Asian physicians’ lower likelihood to recommend cancer screenings to their patients [8, 36]. Jenkins et al. suggested that Vietnamese physicians may not be strong proponents of preventive care due to their training in their home country, and thus may not recommend them or may not do so insistently [36]. In addition, Southeast Asian physicians may feel they are intruding on a woman’s modesty by recommending cancer screening exams [8]. Given that physician recommendations have been found to be the most significant indicator of ever having had a cancer screening done [37], it is crucial to address any barriers that are potentially associated with having a Southeast Asian physician.
Language Capability
Low literacy and lack of English speaking capability have been reported to be tied to low cancer screening rates [38–40]. Davis et al. reported that women with low literacy skills had less knowledge of mammography and had the most negative attitudes toward mammograms [38]. Similarly, Lindau et al. reported that women with low literacy skills had less knowledge of the purpose of Pap smears, and were also less likely to seek medical attention if they received an abnormal Pap smear [40].
This is concerning, given that the Hmong are a relatively new immigrant group with low literacy levels and limited English language skills. In fact, a majority of Hmong are illiterate in their own language [41]. Roughly 50% of participants in Tanjasiri et al.’s study reported that they cannot read Hmong [8]. Garbers and Chiasson found that low literacy skills in one’s own language increased the barriers individuals faced in utilizing cancer screenings [39]; thus, the Hmong’s low literacy skills may further impede efforts to seek and/or undergo cancer screening. Compounding this barrier, the majority of Hmong are linguistically isolated. The Asian and Pacific Islander American Health Forum reported that 95% of Hmong Americans speak a language other than English at home [42]. Furthermore, Tanjasiri et al. reported that 71% of participants in their study do not read English, underlining the difficulty in disseminating cancer screening information to the Hmong [8].
Years in the US
Longer duration of residence in the U.S. has been positively associated with cancer screening utilization in various immigrant populations. Maxwell et al. reported that Filipino and Korean immigrants were more likely to adhere to cancer screening guidelines if they had spent a higher percentage of their lifetime in the U.S [9]. Similarly, Taylor et al. and Yi reported that having spent longer years in the U.S. was positively associated with having undergone a cervical cancer screening among Vietnamese American women [43, 44]. These findings were also established for Hmong American women in Tanjasiri et al.’s study, where it was found that Hmong women who had resided in the U.S. for a longer period of time were more likely to have undergone a cancer screening [8]. Given that the Hmong are recent refugees who have resided in the U.S. for a short period of time, they may be at high risk for failing to follow through with cancer screening guidelines.
Culture as a Barrier
Cultural beliefs and attitudes toward cancer and cancer screening can influence ethnic minorities’ health behaviors, including decisions to undergo cancer screenings. Asian Americans in particular face a vast number of cultural barriers to cancer screening participation, including a fatalistic view toward cancer, perception of screening as unnecessary in the absence of symptoms, strong sense of modesty, perception of female organs as nonfunctional after procreation, and a tendency to value the welfare of the group over one’s own health [45–47]. To date, no study of Hmong Americans has been conducted that reviewed cultural factors as a barrier to undergoing cancer screenings. However, the literature has documented cultural barriers to general health care utilization among this population, which can provide useful insights into understanding the Hmong’s low cancer screening rate.
Etiology of Illnesses
Traditional Hmong health beliefs typically recognize two root causes of illnesses: natural and spiritual [48]. Illnesses of a natural origin, such as stomachaches and body aches, are believed to be the result of disharmony between yin and yang (hot and cold) properties in the body [49–51]. Therefore, the treatment goal is to bring about balance to the body through the use of herbal medicine, acupuncture, spoon rubbing (where the patient’s body is repeatedly scraped with a silver spoon), or coining (where a coin is repeatedly rolled over the sick person’s body) [48–51].
However, more serious illnesses are typically identified as having underlying spiritual causes, especially if the illness is accompanied by nightmares, is persistent, or is rendered unexplainable [21, 27, 49, 52]. For example, chronic diseases, birth defects, and mental illnesses are commonly perceived to be spirit-rooted illnesses [3, 27, 49, 50, 53]. This is reflective of the Hmong’s traditional religious belief in Shamanism, which dictates that spirits dominate all aspects of human life, including an individual’s health [48, 54]. Spirit-rooted illnesses are often attributed to soul loss, offended spirits of ancestors, or encounters with menacing spirits [48, 49]. When illnesses are believed to be caused by spirits, Hmong patients typically will refuse biomedical treatment due to the belief that it is ineffective or out of fear that accepting such treatments will infuriate a spirit even further [55]. Studies have revealed that the belief in the spiritual etiology of cancer can pose as a barrier to cancer screening. For example, Burhansstipanov et al. reported that even after structural barriers to cancer screening were removed, Native American participants were still reluctant to undergo pap tests out of fear that doing so would invite the cancer spirit [56]. Additionally, Yeo et al. reported that participants from a population known to underutilize cancer services believed coming into contact with evil spirits could cause cancer [57]. Given these findings, the Hmong’s belief in spirit-rooted illnesses could prevent them from seeking cancer screenings.
Additionally, a fatalistic attitude is often taken toward spirit-rooted illnesses, further discouraging this population from adopting preventive health behaviors involving spirit-rooted illnesses [3, 58]. A focus group involving Hmong women revealed that the participants held fatalistic attitudes toward cancer [59]. In view of other findings that fatalism serves as a significant barrier to cancer screening among minority groups, who may not perceive the value in undergoing cancer screenings [60–62], it is possible that the Hmong’s fatalistic attitude toward spiritually rooted illnesses, including cancer, can function as a barrier to cancer screening among this population.
Influence of Patriarchal Values
Patriarchal beliefs have been identified as barriers to breast cancer screening utilization among traditional Asian American women [63, 64]. Similar to other traditional Asian Americans, the Hmong’s family structure is highly patriarchal. Male heads of households have a significant influence over their family members’ health care decisions [48]. Women are expected to defer to their husbands’ opinions [65, 66]. This can present challenges to promoting cancer screening among Hmong women, as they rarely make decisions regarding their own healthcare [55, 67, 68]. Spring et al. reported that Hmong women were hesitant about prenatal care, because they were aware that their husbands disapproved of pelvic examinations [69]. To compound this factor, it is possible that Hmong American women’s adherence to patriarchal dictates could deter them from perceiving a need to initiate self-care activities. Studies have reported that Korean American women from patriarchal communities tend to trivialize their own healthcare needs, and instead focus on the needs of their husbands and children [70, 71]. Thus, Hmong women’s patriarchal values may lead them to undervalue their own healthcare needs, and hinder them from adopting positive cancer screening behaviors.
Modesty
Similar to other traditional Asian American women, Hmong women have a strong sense of modesty, which has prevented them from undergoing physical examinations that may cause embarrassment or shame [53, 69, 72]. For instance, in a study of Hmong American women’s cancer beliefs, participants reported that having discussions about women’s body parts were embarrassing and that showing body parts to a male physician was difficult [59]. Similarly, Barrett et al. reported that due to modesty concerns, Hmong American women held reservations regarding Pap smears and other physical examinations [53]. Given that modesty has been identified as a crucial barrier to breast and cervical cancer screening among other traditional Asian American women, it is possible that Hmong women’s modesty may dissuade them from undergoing cancer screenings [9, 73].
Mistrust Toward Western Medical System
Mistrust toward the western medical system has been identified as another barrier to cancer screening among minority groups [74–77]. In Choi et al.’s study, African American participants’ mistrust of the western medical system—particularly physicians’ intentions—was identified as a barrier to seeking oral cancer screening [75]. Similarly, Giarratano, Bustamante-Forest, & Carter identified mistrust as a crucial barrier to cancer screening among African American and Latina women [77]. The literature widely documents the Hmong’s general mistrust toward the western medical system [48, 55, 78], and its negative impact on Hmong Americans’ willingness to utilize western healthcare [31, 79]. Hmong Americans’ mistrust of the western medical system is largely attributed to their unfamiliarity with western healthcare, the negative experiences individuals in the Hmong community have had, and a general skepticism of western systems due to the betrayal the Hmong felt after the Vietnam War [50, 55]. Uba reported that mistrust of the western medical system contributed to a delay in seeking care, which often resulted in poor outcomes; this in turn amplified the mistrust the community initially held [31]. Investigations have documented that this issue has had a particularly negative effect on the health of some Hmong American children, as Hmong parents have been known to refuse to consent to their child’s treatment due to concerns regarding physicians’ intentions [72, 80]. Arax reported on one incident in which a Hmong American teenager ran away from home to elude court-ordered cancer treatment, after her community voiced their mistrust of the medications [81]. Thus, the Hmong’s mistrust of the western medical system may pose challenges to promoting cancer screening among this population.
Cancer Literacy Factors
Cancer Literacy
Low cancer knowledge appears to function as a barrier to cancer screening. In a group of Mexican–American women, Carpenter and Colwell’s study found that low cancer knowledge was correlated with low cancer screening self-efficacy [82]. Similarly, participants in Shell and Tudiver’s study identified lack of knowledge about cancer as a barrier to cancer screening [83]. Xu et al. reported that cancer literacy was significantly associated with cancer screening behavior [84]. In Pearlman et al.’s study, only 51.8% of respondents who had no knowledge of breast or cervical cancer had ever undergone both a breast exam and a Pap smear, compared to 79.3% of respondents who had some knowledge of breast and cervical cancer [85]. These findings are disconcerting, as the overall cancer literacy among Hmong Americans has been reported to be low [86]. Hmong adolescents in one study reported low knowledge of Hepatitis B Virus (HBV), a major risk factor for liver cancer [22]. For example, only 49% of respondents between the ages of 19–25 knew that HBV could be transmitted sexually [22]. In another study by Vang and Pinzon-Perez, a majority of respondents (60%) reported low knowledge of nasopharyngeal cancer—a highly prevalent cancer in the Hmong [87–89]. Thus, it is critical to address the Hmong’s low cancer knowledge, which could hinder them from adopting positive cancer screening practices.
Illiteracy in Prevention
The literature widely reports that Asian Americans who do not undergo cancer screening do so primarily because they view it as unnecessary in the absence of symptoms [9, 61, 90–92]. In fact, Juon et al. reported that this was the most frequently cited reason for not ever having had a Pap test [90]. Kandula et al. also reported similar findings, and concluded that foreign-born Asian Americans were significantly more likely to adopt such a belief [91]. Such attitudes toward nonpreventive care appear to exist for the Hmong as well. The literature reports that Hmong Americans typically view health care utilization as unnecessary in the absence of symptoms [3, 48, 50]. They generally do not consult a physician until symptoms are severe [50, 93]. This is not suprising, as the concept of prevention in general is novel to the Hmong, whose access to preventive health care was minimal prior to arriving in the U.S [94]. Moreover, Hmong Americans traditionally believe that some illnesses are predetermined and of a spiritual nature, and thus are not preventable [3]. The Hmong’s attitude toward prevention is likely to be an important contributing factor to their low utilization of preventive care and low implementation of preventive health measures [3, 22, 95].
Discussion
This comprehensive review of the scholarly literature explored potential barriers to cancer screening among Hmong Americans to generate culture and ethnic group-specific prevention strategies and cancer health policies for Hmong Americans. The Hmong’s high cancer mortality rate and alarmingly low cancer screening rate underscores the need to increase the Hmong’s utilization of cancer screenings. Very little research has been conducted on cancer practices in the Hmong American population, and no work has systematically examined the wide range of barriers to cancer screening that this population faces. The findings from our analysis will increase the understanding of the cultural, ethnic and historic factors present in the Hmong community that may contribute to their health prevention behaviors. Our review suggests that various barriers to cancer screening exist for Hmong Americans, including accessibility to health care, culture, and cancer literacy barriers, which could explain the Hmong’s low cancer screening rate.
Future interventions should address the stigmatizing nature of utilizing public health services. Our findings suggest that many Hmong Americans who have public health insurance feel unwelcomed and disrespected at public health facilities, which could discourage them from utilizing preventive services, such as cancer screenings. Healthcare workers at every level need to use cultural sensitivity when communicating with the Hmong in order to prevent any miscommunication. In addition, there is a critical need to implement health care practices that take into account the unique needs of Hmong refugees and other special populations, such as the allotment of more time for health education, interpretive services, and discussions regarding the importance of preventive services. It may be necessary to implement health policies that require the incorporation of screening education or recommendation in routine care in order to reduce the cancer screening disparity seen in this group.
Furthermore, our findings indicate that there is a need to educate Southeast Asian physicians about the importance of screening, which may have been overlooked due to overseas training or cultural biases. Southeast Asian doctors’ unique positions as both a member of the community and as a physician call for efforts to be made to teach Southeast Asian physicians how to convey cancer information to Hmong patients, especially Hmong women, without violating cultural norms. Considerations should be made to include women’s husbands or other trusted family members when discussing illness or preventive care that require examining women’s bodies.
Given that Hmong Americans reported low knowledge of cancer, the provision of cancer education to this population is urgent to promote cancer screening. Additionally, interventions to address the Hmong’s low cancer knowledge need to be aware of the literacy difficulties Hmong Americans face in both English and in their own language. As noted earlier, many Hmong Americans are illiterate in their native language. This challenge requires unique approaches and varied venues to be utilized in order to reach this population. An intervention which utilized flipcharts, brochures, and educational videos in Hmong, was found to be effective and could be tried more widely in the community to test its effectiveness [96]. Multiple modes of communication, such as the promotion of cancer screening through the use of educational videos, Hmong television and radio broadcasts, face-to-face education, and word of mouth, should be implemented in order to effectively reach the Hmong population. The delivery of cancer education to this group should also be evidence-informed and/or based and culturally competent, as the Hmong may not believe in the education or intervention offered, especially if it does not share many of the core tenets of Hmong beliefs in regard to etiology and treatment of cancer.
Our findings suggest that interventions to promote cancer screening among the Hmong must address specific cultural barriers this population faces. Hmong Americans’ unique spiritual belief in disease etiology has presented challenges in promoting health in the past, and should be taken into consideration. Culturally competent models that incorporate traditional Shamanist perspectives regarding cancer etiology should be developed. A cancer screening intervention developed in collaboration with Hmong shamans and religious leaders might be useful in persuading the Hmong to adopt a positive attitude toward cancer prevention.
In addition, educational interventions need to be developed that are congruent with the Hmong’s highly patriarchal society. For example, Hmong men should be targeted as well as women in cancer education efforts, as the inclusion of Hmong women’s husbands has been found to be highly effective in increasing both Hmong men and women’s knowledge and positive attitudes toward cancer screening [96].
Additionally, given that modesty has been identified as a crucial barrier to breast and cervical cancer screening among other traditional Asian American women, it is pivotal to encourage providers to develop policies that will alleviate the anxiety many Hmong women experience when undergoing examinations. The employment of female practitioners who understand the cultural expression of modesty should be encouraged. Hmong women should also be given the option to have their husbands and/or female family members present when undergoing cancer screenings to reduce their anxiety level.
The development of interventions to promote cancer screening among the Hmong should also acknowledge the Hmong’s strong mistrust of the western medical system. Trusting relationships need to be built with the Hmong community in order to gain their trust and alleviate their fears toward the system. This could be done by disseminating cancer information through religious leaders (i.e., shamans, Christian pastors) and other well-respected Hmong community leaders or role models, who could make positive reports regarding cancer prevention or screening. In addition, it might be effective to use lay people who have undergone a cancer screening and can speak about their experiences, and thus encourage others in the community to utilize cancer screenings.
In conclusion, a multipronged, culturally sensitive approach to cancer prevention that is tailored to the life circumstances of Hmong Americans is urgently needed based on the low rates of cancer screening and high mortality seen in this population. Health access, culture, and cancer literacy factors affecting the Hmong need to be taken into consideration, along with evidence-based approaches in designing and tailoring intervention strategies. Inclusion of community lay people, religious leaders, and respectful role-models in the process of intervention development is critical in creating a culturally competent intervention approach that gives weight to the core health beliefs and cultural practices of the Hmong. To maximize effectiveness, this effort needs to incorporate a community-based participatory research approach in which all parties including researcher, community leaders, and representatives from the health care system synergize their efforts to discuss the problems and propose a solution which benefits the community immediately and effectively.
References
Chen, M. S. (2005). Cancer health disparities among Asian Americans: What we do and what we need to do. Cancer, 104(12), 2895–2902.
American Cancer Society. (2007). Cancer facts & figures 2007 (pp. 32–33). Atlanta, GA: American Cancer Society.
Viste, J. (2007). Communicating (birth defects) prevention information to a Hmong population in Wisconsin: A study of cultural relevance. Substance Use and Misuse, 42, 753–774.
Yang, R. C., Mills, P. K., & Riordan, D. G. (2005). Gastric adenocarcinoma among Hmong in California, USA, 1988–2000. Gastric Cancer, 8, 117–123.
Yang, R. C., Mills, P. K., & Riordan, D. G. (2004). Cervical cancer among Hmong women in California, 1988–2000. American Journal of Preventive Medicine, 27(2), 132–138.
Mills, P. K., Yang, R. C., & Riordan, D. (2005). Cancer incidence in the Hmong in California, 1988–2000. Cancer, 104(12S), 2969–2974.
Yang, R. C., Mills, P. K., & Dodge, J. L. (2006). Cancer screening, reproductive history, socioeconomic status, and anticipated cancer-related behavior among Hmong adults. Asian Pacific Journal of Cancer Prevention, 7, 79–85.
Tanjasiri, S. P., Kagawa-Singer, M., Foo, M. A., Chao, M., Linayao-Putman, I., Lor, Y. C., et al. (2001). Breast cancer screening among Hmong women in California. Journal of Cancer Education, 16(1), 50–54.
Maxwell, A. E., Bastani, R., & Warda, U. S. (2000). Mammography utilization and related attitudes among Korean-American women. Women and Health, 27(3), 89–107.
Kagawa-Singer, M., & Pourat, N. (2000). Asian American and Pacific Islander breast and cervical carcinoma screening rates and healthy people 2000 objectives. Cancer, 89(3), 696–705.
Jemal, A., Siegel, R., Ward, E., Yongping, H., Xu, J., Murray, T., et al. (2008). Cancer statistics. CA: A Cancer Journal for Clinicians, 58(2), 71–96.
Kohno, M., Takeda, M., Niwano, Y., Saito, R., Emoto, N., Tada, M., et al. (2008). Early diagnosis of cancer by detecting the chemiluminescence of hematoporphyrins in peripheral blood lymphocytes. The Tohoku Journal of Experimental Medicine, 216(1), 47–52.
Raffle, A. E., Alden, B., Quinn, M., Babb, P. J., & Brett, M. T. (2003). Outcomes of screening to prevent cancer: Analysis of cumulative incidence of cervical abnormality and modelling of cases and deaths prevented. British Medical Journal, 326, 901–905.
Yau, J. (2005). The foreign-born Hmong in the United States. Migration Information Source of the Migration Policy Institute, US in Focus. Retrieved October 10, 2008 from http://www.migrationinformation.org/USfocus/display.cfm?id=281.
U.S. Census Bureau. (2008). American Community Survey. Retrieved January 29, 2010 from http://factfinder.census.gov/servlet/IPTable?_bm=y&-geo_id=01000US&-qr_name=ACS_2008_1YR_G00_S0201&-qr_name=ACS_2008_1YR_G00_S0201PR&-qr_name=ACS_2008_1YR_G00_S0201T&-qr_name=ACS_2008_1YR_G00_S0201TPR&-reg=ACS_2008_1YR_G00_S0201:039;ACS_2008_1YR_G00_S0201PR:039;ACS_2008_1YR_G00_S0201T:039;ACS_2008_1YR_G00_S0201TPR:039&-ds_name=ACS_2008_1YR_G00_&-_lang=en&-format=.
Pfeifer, M. (2001). U.S. census 2000: Trends in Hmong population distribution across the regions of the United States. Saint Paul, MN: Hmong Resource Center.
Pfeifer, M., & Lee, S. (2003). Hmong population, demographic, socioeconomic, and educational trends in the 2000 census. In B. Thao, L. Schein, & M. Niedzweick (Eds.), Hmong 2000 census publication: Data & analysis (pp. 3–11). Washington, DC: Hmong National Development, Inc. & Hmong Cultural and Resource Center.
Pinzon-Perez, H., Moua, N., & Perez, M. A. (2005). Understanding satisfaction with shamanic practices among the Hmong in rural California. International Electronic Journal of Health Education, 8, 18–23.
U. S. Department of Commerce. (1993). We the American: Asians. Washington, DC: U.S. Department of Commerce.
Harner, M. (1999). Science, spirits, and core shamanism. Shamanism, 12(1). Retrieved June 4, 2008 from http://www.shamanism.org/articles/article10.html.
Helsel, D. G., Mochel, M., & Bauer, R. (2004). Shamans in a Hmong American community. The Journal of Alternative and Complementary Medicine, 10(6), 933–938.
Butler, L. M., Mills, P. K., Yang, R. C., & Chen, M. S. (2005). Hepatitis B knowledge and vaccination levels in California Hmong youth: Implications for liver cancer prevention strategies. Asian Pacific Journal of Cancer Prevention, 6, 401–403.
Wilder Research Center. (2000). Speaking for themselves: A survey of Hispanic, Hmong, Russian, and Somali immigrants in Minneapolis-Saint Paul. Saint Paul, MN: Amherst H. Wilder Foundation.
Wong, C. C., Mouanoutoua, V., Chen, M., Gray, K., & Tseng, W. (2005). Adherence with hypertension care among Hmong Americans. Journal of Community Health Nursing, 22(3), 143–156.
Lee, T. P., & Pfeifer, M. E. (2007). Building bridges: Teaching about the Hmong in our communities. Hmong Cultural Center. Retrieved June 4, 2008 from http://hmongcc.org/BuildingBridgesGeneralPresentation2007Version.pdf.
Bliatout, B. (1990). Hmong beliefs about health and illness. Hmong Forum, 1, 40–45.
Plotnikoff, G. A., Numrich, C., Wu, C., Yang, D., & Xiong, P. (2002). Hmong shamanism: Animist spiritual healing in Minnesota. Clinical & Health Affairs, 85(6), 29–34.
Klein, W. C., & Bloom, M. (1994). Social work as applied social science: A historical analysis. Social Work, 39, 421–431.
Deinard, A. S., & Dunnigan, T. (1987). Hmong health care—reflections on a six-year experience. International Migration Review, 21(3), 857–865.
Dhooper, S. S. (2003). Health care needs of foreign-born Asian Americans: An overview. Health and Social Work, 28, 63–73.
Uba, L. (1992). Cultural barriers to health care for Southeast Asian refugees. Public Health Reports, 107(5), 544–548.
Ayanian, J. Z., Kohler, B. A., Abe, T., & Epstein, A. M. (1993). The relation between health insurance coverage and clinical outcomes among women with breast cancer. The New England Journal of Medicine, 329, 326–331.
Gordon, N. P., Rundall, T. G., & Parker, L. (1998). Type of health care coverage and the likelihood of being screened for cancer. Medical Care, 36(5), 636–644.
Jenkins, C. N. H., Le, T., McPhee, S. J., Stewart, S., & Ha, N. T. (1996). Health care access and preventive care among Vietnamese immigrants: Do traditional beliefs and practices pose barriers? Social Science Medicine, 43(7), 1049–1056.
McPhee, S. J., Bird, J. A., Ha, N., Jenkins, C. N. H., Fordham, D., & Le, B. (1996). Pathways to early cancer detection for Vietnamese women: Suc khoe la vang! (Health is gold!). Health Education Quarterly, 23, S60–S75.
Jenkins, C. N. H., McPhee, S. J., Bird, J. A., Pham, G. Q., Nguyen, B. H., Nguyen, T., et al. (1999). Effect of a media-led education campaign on breast and cervical cancer screening among Vietnamese-American women. Preventive Medicine, 28, 395–406.
Lerman, C., Rimer, B., Trock, B., Balshem, A., & Engstrom, P. F. (1990). Factors associated with repeat adherence to breast cancer screening. Preventive Medicine, 19(3), 279–290.
Davis, T. C., Dolan, N. C., Ferreira, M. R., Tomori, C., Green, K. W., Sipler, A. M., et al. (2001). The role of inadequate health literacy skills in colorectal cancer screening. Cancer Investigation, 19(2), 193–200.
Garbers, S., & Chiasson, M. A. (2004). Inadequate functional health literacy in Spanish as a barrier to cervical cancer screening among immigrant Latinas in New York City. Preventing Chronic Disease, 1(4), A07.
Lindau, S. T., Tomori, C., Lyons, T., Langseth, L., Bennett, C. L., & Garcia, P. (2002). The association of health literacy with cervical cancer prevention knowledge and health behaviors in a multiethnic cohort of women. American Journal of Obstetrics and Gynecology, 186(5), 938–943.
Perez, M. A., & Cha, K. (2007). Diabetes knowledge, beliefs, and treatments in the Hmong population: An exploratory study. Hmong Studies Journal, 8, 1–21.
Asian and Pacific Islander American Health Forum. (2006). Health brief: Hmong in the United States. Asian and Pacific Islander American Health Forum. Retrieved October 10, 2008 from http://www.apiahf.org/resources/pdf/Hmong_in_the_United_States.pdf.
Taylor, V. M., Schwartz, S. M., Jackson, J. C., Kuniyuki, A., Fischer, M., Yasui, Y., et al. (1999). Cervical cancer screening among Cambodian-American women. Cancer Epidemiology, Biomarkers and Prevention, 8, 541–546.
Yi, J. K. (1994). Factors associated with cervical cancer screening behavior among Vietnamese women. Journal of Community Health, 19, 189–200.
Giuliano, A. R., Mokuau, N., Hughes, C., Tortolero-Luna, G., Risendal, B., Ho, R., et al. (2000). Participation of minorities in cancer research: The influence of structural, cultural, and linguistic factors. Annuals of Epidemiology, 10, S22–S34.
Kagawa-Singer, M. (1999). Cancer and Asian American cultures. Asian American Pacific Islander Journal of Health, 9(6), 383–399.
Lee, M. (1999). Breast and cervical cancer early detection in Chinese American women. Asian American Pacific Islander Journal of Health, 6, 351–357.
Culhane-Pera, K. A., & Xiong, P. (2003). Hmong culture: Tradition and change. In K. A. Culhane-Pera, D. E. Vawter, P. Xiong, B. Babbitt, & M. M. Solberg (Eds.), Healing by heart: Clinical and ethical case stories of Hmong families and Western providers (pp. 11–68). Nashville, TN: Vanderbilt University Press.
Hickman, J. R. (2007). “Is it the spirit or the body?” Syncretism of health beliefs among Hmong immigrants to Alaska. NAPA Bulletin, 27, 176–195.
Reznik, V., Cooper, T., MacDonald, D., Benador, N., & Lemire, J. (2001). Hais cuaj txub kaum txub—To speak of all things: A Hmong cross-cultural case study. Journal of Immigrant Health, 3(1), 23–30.
Smith, L. (1997). Critical thinking, health policy, and the Hmong cultural group, part I. Journal of Cultural Diversity, 4(1), 5–10.
Thao, X. (1986). Hmong perception of illness and traditional ways in healing. In G. L. Hendricks, B. T. Downing, & A. S. Deinard (Eds.), The Hmong in transition (pp. 365–378). New York: Center for Migration Studies.
Barrett, B., Shadick, K., Schilling, R., Spencer, L., del Rosario, S., Moua, K., et al. (1998). Hmong/Medicine interactions: Improving cross-cultural health care. Cultural Competence, 30(3), 179–184.
Lewis, I. M. (2003). Estatic religion. New York: Routledge.
Johnson, S. K. (2002). Hmong health beliefs and experiences in the western health care system. Journal of Transcultural Nursing, 13(2), 126–132.
Burhansstipanov, L., Dignan, M. B., Wound, D. B., Tenney, M., & Vigil, G. (2000). Native American recruitment into breast cancer screening: The NAWWA project. Journal of Cancer Education, 15, 28–32.
Yeo, S. S., Meiser, B., Barlow-Stewart, K., Goldstein, D., Tucker, K., & Eisenbruch, M. (2005). Understanding community beliefs of Chinese-Australians about cancer: Initial insights using an ethnographic approach. Psycho-Oncology, 14, 174–196.
Culhane-Pera, K. A., Her, C., & Her, B. (2007). “We are out of balance here”: A Hmong cultural model of diabetes. Journal of Immigrant and Minority Health, 9(3), 179–190.
Baisch, M. J., Vang, P. C., & Peterman, B. R. (2008). An exploration of Hmong women’s perspectives on cancer. Asian Nursing Research, 2(2), 82–91.
Chavez, L. R., Hubbell, F. A., Mishra, S. I., & Valdez, R. B. (1997). The influence of fatalism on self-reported use of papanicolaou smears. American Journal of Preventive Medicine, 13, 418–424.
Lee, M. (2000). Knowledge, barriers, and motivators related to cervical cancer screening among Korean-American women: A focus group approach. Cancer Nursing, 23(3), 168–175.
Powe, B. D., & Finnie, R. (2003). Cancer fatalism: The state of the science. Cancer Nursing, 26(6), 454–467.
Rajaram, S. S., & Rashidi, A. (1999). Asian-Islamic women and breast cancer screening: A socio-cultural analysis. Women and Health, 28(3), 45–58.
Suh, E. E. (2008). The sociocultural context of breast cancer screening among Korean immigrant women. Cancer Nursing, 31(4), E1–E10.
Foo, L. J. (2002). Asian American women: Issues, concerns, and responsive human and civil rights advocacy. New York: The Ford Foundation.
Morrow, R. D. (1989). Southeast Asian child rearing practices: Implications for child and youth care workers. Child & Youth Care Quarterly, 18(4), 273–287.
Parker, M., & Kiatoukaysy, L. N. (1999). Culturally responsive health care: The example of the Hmong in America. Journal of the American Academy of Nurse Practitioners, 11(12), 511–518.
Sperstad, R. A., & Werner, J. S. (2005). Coming in the cultural “in-between”: Nursing insights from a Hmong birth case study. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 34, 682–688.
Spring, M. A., Ross, P. J., Etkin, N. L., & Deinard, A. S. (1995). Sociocultural factors in the use of prenatal care by Hmong women, Minneapolis. American Journal of Public Health, 85(7), 1015–1017.
Im, E. O. (1997). Neglecting and ignoring menopause within a gendered multiple transitional context: Korean immigrant women. Unpublished doctoral dissertation, University of California, San Francisco. Retrieved October 10, 2008 from Proquest Digital Dissertations.
Im, E. O., Park, Y. S., Lee, E. O., & Yun, S. N. (2004). Korean women’s attitudes toward breast cancer screening tests. International Journal of Nursing Studies, 41, 583–589.
Cha, D. (2003). Hmong American concepts of health, healing and conventional medicine. NewYork: Routledge.
Mo, B. (1992). Modesty, sexuality, and breast health in Chinese-American women. Western Journal of Medicine, 157, 260–264.
Canales, M. K., & Geller, B. M. (2004). Moving in between mammography: Screening decisions of American Indian women in Vermont. Qualitative Health Research, 14, 836–857.
Choi, Y., Dodd, V., Watson, J., Tomar, S. L., Logan, H. L., & Edwards, H. (2008). Perspectives of African Americans and dentists concerning dentist-patient communication on oral cancer screening. Patient Education & Counseling, 71(1), 41–51.
Garner, E. I. O. (2003). Cervical cancer: Disparities in screening, treatment, and survival. Cancer Epidemiology, Biomarkers and Prevention, 12, 242s–247s.
Giarratano, G., Bustamante-Forest, R., & Carter, C. (2005). A multicultural and multilingual outreach program for cervical and breast cancer screening. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 34, 395–402.
Westermeyer, J., & Her, C. (2007). Western psychiatry and difficulty: Understanding and treating Hmong refugees. In J. P. Wilson & C. S. Tang (Eds.), Cross-cultural assessment of psychological trauma and PTSD (pp. 371–393). New York, NY: Springer.
Ohmans, P., Garrett, C., & Treichel, C. (1996). Cultural barriers to health care for refugees and immigrants. Minnesota Medicine, 79, 26–30.
Wells, R., & Sheldon, M. (2000). Case study: Making room for alternatives. The Hastings Center Report, 30(3), 26–28.
Arax, M. (1995). Order for Hmong girl’s cancer treatment dropped. Los Angeles Times, p 3A.
Carpenter, V., & Colwell, B. (1995). Cancer knowledge, self-efficacy, and cancer screening behaviors among Mexican-American women. Journal of Cancer Education, 10(4), 217–222.
Shell, R., & Tudiver, F. (2004). Barriers to cancer screening by rural Appalachian primary care providers. The Journal of Rural Health, 20(4), 368–373.
Xu, Y., Ross, C., Ryan, R., & Wang, B. (2005). Cancer risk factors of Vietnamese Americans in rural south Alabama. Journal of Nursing Scholarship, 37(3), 237–244.
Pearlman, D. N., Clark, M. A., Rakowski, W., & Ehrich, B. (1999). Screening for breast and cervical cancers: The importance of knowledge and perceived cancer survivability. Women and Health, 28(4), 93–112.
Kong, B. H. (1999). Cancer beliefs of the Hmong. Unpublished master’s thesis, Milwaukee: University of Wisconsin.
Vang, T., & Pinzon-Perez, H. (2006). Knowledge of nasopharyngeal carcinoma among Hmong populations in central California. Hmong Studies Journal, 7, 1–24.
Dodge, J. L., Mills, P. K., & Yang, R. C. (2005). Nasopharyngeal cancer in the California Hmong, 1988–2000. Oral Oncology, 41(6), 596–601.
Mills, P. K., & Yang, R. C. (1997). Cancer incidence in the Hmong of Central California, United States, 1987–94. Cancer Causes and Control, 8(5), 706–712.
Juon, H., Seung-Lee, C., & Klassen, A. C. (2003). Predictors of regular pap smears among Korean-American women. Preventive Medicine, 37(6), 585–592.
Kandula, N. R., Wen, M., Jacobs, E. A., & Lauderdale, D. S. (2006). Low rates of colorectal, cervical, and breast cancer screening in Asian Americans compared with non-Hispanic whites. Cancer, 107(1), 184–192.
Kim, K., Yu, E. S. H., Chen, E. H., Kim, J., Kaufman, M., & Purkiss, J. (1999). Cervical cancer screening knowledge and practices among Korean-American women. Cancer Nursing, 22(4), 297–302.
Culhane-Pera, K. A., & Lee, M. (2006). Die another day”: A qualitative analysis of Hmong experiences with kidney stones. Hmong Studies Journal, 7, 1–34.
Kunstadter, P. (1985). Health of Hmong in Thailand: Risk factors, morbidity and mortality in comparison with other ethnic groups. Culture, Medicine and Psychiatry, 9, 329–351.
Vue, H., & Reicks, M. (2007). Individual and environmental influences on intake of calcium-rich food and beverages by young Hmong adolescent girls. Journal of Nutrition Education & Behavior, 39, 264–272.
Tanjasiri, S. P., Kagawa-Singer, M., Foo, M. A., Chao, M., Linayao-Putman, I., Nguyen, J., et al. (2007). Designing culturally and linguistically appropriate health interventions: The “Life is Precious” Hmong breast cancer study. Health Education & Behavior, 34, 140–153.
Ross, J. A., Xie, Y., Kiffmeyer, W. R., Bushhouse, S., & Robison, L. L. (2003). Cancer in the Minnesota Hmong population. Cancer, 97(12), 3076–3079.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, H.Y., Vang, S. Barriers to Cancer Screening in Hmong Americans: The Influence of Health Care Accessibility, Culture, and Cancer Literacy. J Community Health 35, 302–314 (2010). https://doi.org/10.1007/s10900-010-9228-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-010-9228-7