ABSTRACT
BACKGROUND
Two clinical trials suggest that procalcitonin-guided antibiotic therapy can safely reduce antibiotic prescribing in outpatient management of acute respiratory tract infections (ARTIs) in adults. Yet, it remains unclear whether procalcitonin testing is cost-effective in this setting.
OBJECTIVE
To evaluate the cost-effectiveness of procalcitonin-guided antibiotic therapy in outpatient management of ARTIs in adults.
DESIGN
Cost-effectiveness model based on results from two published European clinical trials, with all parameters varied widely in sensitivity analyses.
PATIENTS
Two hypothetical cohorts were modeled in separate trial-based analyses: adults with ARTIs judged by their physicians to require antibiotics and all adults with ARTIs.
INTERVENTIONS
Procalcitonin-guided antibiotic therapy protocols versus usual care.
MAIN MEASURES
Costs and cost per antibiotic prescription safely avoided.
KEY RESULTS
We estimated the health care system willingness-to-pay threshold as $43 (range $0–$333) per antibiotic safely avoided, reflecting the estimated cost of antibiotic resistance per outpatient antibiotic prescribed. In the cohort including all adult ARTIs judged to require antibiotics by their physicians, procalcitonin cost $31 per antibiotic prescription safely avoided and the likelihood of procalcitonin use being favored compared to usual care was 58.4 % in a probabilistic sensitivity analysis. In the analysis that included all adult ARTIs, procalcitonin cost $149 per antibiotic prescription safely avoided and the likelihood of procalcitonin use being favored was 2.8 %.
CONCLUSIONS
Procalcitonin-guided antibiotic therapy for outpatient management of ARTIs in adults would be cost-effective when the costs of antibiotic resistance are considered and procalcitonin testing is limited to adults with ARTIs judged by their physicians to require antibiotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Acute respiratory tract infections (ARTIs) account for 10 % of all ambulatory visits and 44 % of all antibiotic prescriptions in the United States.1 Despite the predominant viral etiology of most ARTIs, antibiotics are prescribed in > 50 % of such infections and an increasing proportion of these are broad-spectrum agents.1–5 Excessive antibiotic use for ARTIs is concerning, because there is little evidence of individual patient benefit from such therapy and strong evidence of increased antibiotic resistance and healthcare costs.6–10 With increasing antibiotic resistance and few new agents under development, antibiotic stewardship has become a national health priority.11
A number of interventions to reduce unnecessary antibiotic prescribing have been evaluated, including media campaigns, physician education, practice guidelines, chart reminders and audit and feedback systems.12,13 The modest effectiveness of these strategies, however, lead the authors of a recent Cochrane review to conclude that “these interventions are unlikely to lead to a reduction in the incidence of antibiotic-resistant bacteria causing community-acquired infection.”12 The disappointing impact of such interventions on antibiotic prescribing is responsible in part for a growing interest in the use of laboratory tests to detect serum inflammatory markers such as C-reactive protein (CRP) and procalcitonin to guide antibiotic decision-making in the management of ARTIs.
While CRP has been used to detect community-acquired pneumonia and differentiate between bacterial and viral etiologies in lower respiratory tract infections, this test suffers from suboptimal sensitivity and specificity and when applied clinically, it does not appear to reduce antibiotic prescribing compared to existing decision support algorithms.14,15 More recently, procalcitonin has emerged as a promising alternative for guiding antibiotic therapy, because this serum marker is elevated in bacterial infections, but not in viral infections or non-specific inflammatory reactions.16 Procalcitonin has been studied in ambulatory and emergency department settings for guiding antibiotic therapy in adults with ARTIs and been found to reduce antibiotic use and treatment duration without increasing morbidity or mortality.16 Two randomized controlled trials (RCTs) have investigated the use of procalcitonin to guide management of ARTIs in the outpatient setting and found that procalcitonin use was associated with 15–72 % absolute reductions in antibiotic exposure without changes in safety endpoints.17,18
While procalcitonin-guided antibiotic therapy for adults with ARTIs managed in the outpatient setting is supported by clinical trials, the cost-effectiveness of this approach remains unclear. Our study aims to evaluate the cost-effectiveness of procalcitonin-guided antibiotic therapy in this setting.
METHODS
Model Perspective and Cohort
To evaluate the cost-effectiveness of procalcitonin testing in adults with ARTIs managed in the outpatient setting, we developed a decision analysis model using TreeAge Pro 2009 software (TreeAge Software, Inc., Williamstown, MA). We assumed a health care system perspective and used an ARTI treatment episode as our time horizon. Because data are available from two European randomized controlled trials (RCTs) evaluating the safety and effectiveness of procalcitonin testing in adults with ARTIs managed in the outpatient setting, we performed two separate analyses using cohorts from each trial.17,18 The first cohort (Briel et al. 2008) included all adults presenting to an outpatient clinic with an ARTI and judged by their physicians to require an antibiotic prescription.17 The second cohort (Burkhardt et al. 2010) included all adults presenting to an outpatient clinic with an ARTI prior to any decision to initiate antibiotic therapy.18
Model Structure
We evaluated two strategies: usual care and procalcitonin-guided antibiotic therapy (Fig. 1). For usual care, we assumed that patients were prescribed antibiotics based on the probability of an empiric antibiotic prescription in each trial cohort (Table 1). In the procalcitonin strategy, we assumed that all patients were also evaluated with a point-of-care procalcitonin test prior to prescribing antibiotics, as occurred in each trial. The procalcitonin level could either be normal (≤ 0.25 ng/ml) or elevated (> 0.25 ng/ml) based on probabilities of these outcomes in each cohort (Table 1). We assumed that all patients with an elevated procalcitonin level were prescribed antibiotics in accordance with likely physician behavior and recent recommendations.12 For patients with a normal procalcitonin level, we assumed that physicians could either follow the procalcitonin protocol and withhold antibiotics or overrule the procalcitonin protocol and give antibiotics, based on published data on physician compliance with procalcitonin protocols for ARTI management (Table 1). We assumed no difference in clinical outcomes between the strategies, since neither trial revealed significant differences in symptom duration, hospitalization or death between usual care and procalcitonin testing treatment groups.17,18 For both cohorts, the model structure was identical. The only differences between the cohorts were the probabilities of initiating empiric antibiotics in each trial cohort, an elevated procalcitonin level, and physician adherence with algorithm recommendations to withhold antibiotics for patients with normal procalcitonin levels (Table 1).
The most widely described and routinely used procalcitonin test is a laboratory test requiring 20–50 μl of serum and 2–4 hours to return a result.17 Because procalcitonin testing would likely be adopted in ambulatory settings only if it was available as a point-of-care test, and because such testing is likely to emerge in the near future, we assumed point-of-care test availability, biasing the analysis towards procalcitonin testing.
Probabilities and Costs
For each cohort, we obtained data from published clinical trials for the following parameters: probability of initiating empiric antibiotic therapy in the usual care arm, probability of an elevated procalcitonin level, and probability of physician compliance with algorithm recommendations to withhold antibiotics given a normal procalcitonin level.17,18 We also modeled costs of antibiotic therapy, procalcitonin testing, and physician time to explain the decision to withhold antibiotics (Table 1). We estimated average antibiotic costs based on pricing for antibiotics commonly used for ARTI treatment.19 Procalcitonin costs were based on Medicare reimbursement.20 All costs were in 2012 U.S. dollars.
Primary Analysis
For each cohort, we compared the procalcitonin and usual care strategies from cost and cost-effectiveness perspectives, performing base case, one-way and probabilistic sensitivity analyses to examine the robustness of the model to parameter variation, and because we were unable to account for missing data in the two RCTs. In probabilistic sensitivity analyses, we varied all parameters simultaneously over their distributions, generally varying probabilities over beta distributions and costs over gamma distributions (Table 1). Because trials have suggested that procalcitonin testing reduces antibiotic use in primary care settings with no change in symptom duration, hospitalization risk or mortality, evaluating the cost-effectiveness of procalcitonin testing in cost per quality-adjusted life years (QALYs) would not capture the value of procalcitonin testing.16–18 Given that the primary rationale for procalcitonin use is to improve the appropriateness of antibiotic prescribing by distinguishing between patients with and without bacterial infections, we chose to measure cost-effectiveness in cost per antibiotic prescription safely avoided.9,10 While this outcome measure has been previously reported in the literature, there are not accepted willingness-to-pay thresholds for this metric.21
To estimate the health care system willingness-to-pay threshold for the cost per antibiotic prescription safely avoided, we assumed that the intrinsic value of an antibiotic prescription safely avoided would equal the health care system cost of antibiotic resistant infections attributable to that antibiotic prescription. To estimate this figure, we multiplied a literature estimate for the total annual excess cost of antibiotic resistance in the United States ($20 billion) by the percentage of antibiotics in the U.S. given to humans (20 %), the relative impact of human versus animal antibiotic use on antibiotic resistance in humans (200 %), the percentage of human antibiotics prescribed in the ambulatory setting (80 %), and the percentage of U.S. annual ambulatory antibiotic prescriptions prescribed for adult ARTIs (27 %) and divided this estimate by the U.S. annual number of antibiotic prescriptions for adult ARTIs (40 million; Table 2). We assumed a linear relationship between reductions in antibiotic use and costs of antibiotic resistance in the absence of published data quantifying this relationship. Due to uncertainties inherent in this approach, we varied parameters widely to arrive at low and high estimates for the health care system willingness-to-pay threshold.
Secondary Analysis
In a secondary analysis, we repeated the base case cost-effectiveness analysis for both cohorts using cost per QALY saved instead of cost per antibiotic safely avoided as the outcome measure. We assumed no difference in duration of illness, hospitalization risk or mortality between the usual care and procalcitonin strategies, based on data from the two published RCTs.17,18 The primary difference between the two strategies was the probability of antibiotic-associated side effects and associated decrements in QALYs. We assumed that 15 % of patients given antibiotics developed antibiotic-associated side effects (e.g. diarrhea, nausea, vomiting, rash) and that the duration of antibiotic side effects was four days.17,18 We assumed that QALYs were a function of time spent in a given health state multiplied by the utility value of that health state, with utility values ranging from 0 (death) to 1 (perfect health). The utility values of the well, acute respiratory tract infection and antibiotic-associated side effect health states were assumed to be 1.0, 0.7, and 0.7, respectively.22,23
RESULTS
Willingness-to-Pay Threshold: Costs of Antibiotic Resistance per ARTI Antibiotic Prescription
We estimated the base case health care system willingness-to-pay threshold to be $43 per antibiotic prescription safely avoided (range: $0–$333), reflecting the total annual U.S. excess costs of antibiotic resistance attributable to antibiotic prescriptions for adult ARTIs divided by the number of antibiotic prescriptions for adult ARTIs (Table 2). This estimate suggests that 8.5 % of the total excess U.S. healthcare costs of antibiotic resistance are attributable to antibiotic prescriptions for adults with ARTIS presenting in the ambulatory setting (range: 0.9–26.6 %; Table 2).
Cost and Cost-Effectiveness Analyses in Adults with ARTIs Judged by Their Physician to Require Antibiotics17
In an analysis limited solely to costs, the procalcitonin strategy cost more than the usual care strategy in the base case ($51 vs. $29) and across all parameter values tested in one-way sensitivity analyses, except when the antibiotic cost >$61 or the procalcitonin testing cost <$17.
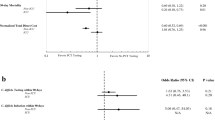
In the cost-effectiveness analysis, the procalcitonin strategy cost more ($51 vs. $29 per patient) and reduced the number of antibiotic prescriptions (0.25 vs. 0.97 antibiotic prescriptions per patient) compared to usual care, resulting in an incremental cost-effectiveness ratio (ICER) of $31 per antibiotic prescription safely avoided. Given an annual total of 40 million antibiotic prescriptions for adult ARTIs, this result suggests that nation-wide adoption of procalcitonin testing could result in 30 million fewer antibiotic prescriptions annually.25 In one-way sensitivity analyses, the parameters with the greatest impact on results were antibiotic cost, procalcitonin cost, and the probability of physician adherence with algorithm recommendations to withhold antibiotics given a normal procalcitonin level (Table 3). The procalcitonin strategy dominated usual care (i.e., was both more effective and less costly) when the antibiotic cost >$61 or procalcitonin testing cost <$17. The procalcitonin ICER was less than the base case willingness-to-pay threshold ($43 per antibiotic safely avoided) across all parameter values tested in one-way sensitivity analyses, except when the antibiotic cost ≤$18, procalcitonin testing cost ≥$48, probability of physician adherence with algorithm recommendations to withhold antibiotics given a normal procalcitonin level was ≤ 68.8 %, or probability of empiric antibiotics was ≤ 83.8 %. In the probabilistic sensitivity analysis, simultaneously varying all parameters over distributions 3,000 times, the likelihoods of the procalcitonin strategy being preferred over usual care at base case ($43 per antibiotic prescription safely avoided), low ($0) and high ($333) willingness-to pay thresholds were 58.4 %, 11.1 % and 100 %, respectively (Fig. 2a). In the secondary analysis in which the primary outcome was cost per QALY saved, the procalcitonin strategy cost more ($51 vs. $29 per patient) and reduced the number of QALYs lost (0.00746 vs. 0.00765 QALYs lost) compared to usual care, resulting in an incremental cost-effectiveness ratio (ICER) of $118,828 per QALY.
Probabilistic sensitivity analysis for procalcitonin-guided antibiotic therapy versus usual care for outpatient management of acute respiratory tract infections (ARTIs) in adults. Results are presented in the form of an acceptability curve for procalcitonin testing (a) in adults with ARTIs judged by their physician to require antibiotics based on Briel et al. 2008 cohort and (b) in all adults with ARTIs based on Burkhardt et al. 2010 cohort. The x-axis depicts willingness-to-pay thresholds, representing the estimated health care system cost of antibiotic resistance per antibiotic prescription (base case: $43, range: $0–$333). The y-axis depicts the likelihood that strategies would be considered cost-effective for each willingness-to-pay threshold.
Cost and Cost-Effectiveness Analyses in all Adults with ARTIs18
In an analysis limited solely to costs, the procalcitonin strategy cost more than the usual care strategy in the base case ($49 vs. $15 per patient) and across all parameter values tested in one-way sensitivity analyses.
In the cost-effectiveness analysis, the procalcitonin strategy cost more ($49 vs. $15 per patient) and reduced the number of antibiotic prescriptions (0.14 vs. 0.37 antibiotic prescriptions per patient) compared to usual care, resulting in an ICER of $149 per antibiotic prescription safely avoided. In one-way sensitivity analyses, the parameters with the greatest impact on the results were again the procalcitonin testing cost, probability of physician adherence with algorithm recommendations to withhold antibiotics given a normal procalcitonin level, and antibiotic cost (Table 3). Compared to usual care, the procalcitonin strategy cost more than the base case willingness-to-pay threshold ($43 per antibiotic safely avoided) across all parameter values in one-way sensitivity analyses, except when procalcitonin cost <$15. Conversely, the procalcitonin strategy cost less than the high estimate for the willingness-to-pay threshold ($333 per antibiotic safely avoided) in all one-way sensitivity analyses, except when the probability of physician adherence with algorithm recommendations to withhold antibiotics given a normal procalcitonin level was ≤ 73.8 %. In the probabilistic sensitivity analysis, the likelihoods of the procalcitonin strategy being preferred over usual care at base case, low and high willingness-to pay thresholds were 2.8 %, 0.3 % and 62.9 %, respectively (Fig. 2b). In the secondary analysis in which the primary outcome was cost per QALY saved, the procalcitonin strategy cost more ($49 vs. $15 per patient) and reduced the number of QALYs lost (0.00743 vs. 0.00749 QALYs lost) compared to usual care, resulting in an ICER of $575,249 per QALY.
DISCUSSION
Employing a trial-based approach, we found that procalcitonin testing is unlikely to be preferred over usual care when costs alone are considered, but is likely to be cost-effective when the costs of antibiotic resistance are considered and the test is used only in adults with ARTIs judged to require antibiotics by their physicians. In this clinical scenario, procalcitonin testing becomes more favored as antibiotic costs increase, procalcitonin costs decrease and physician adherence with algorithm recommendations increases.
This study adds to the literature by providing data on the cost-effectiveness of procalcitonin-guided antibiotic therapy in adult ARTIs and identifying situations in which procalcitonin testing is more likely to be economically reasonable. The two RCTs of procalcitonin-guided antibiotic therapy in adults with ARTIs in outpatient settings have found significant procalcitonin-associated reductions in antibiotic use without compromising medical outcomes.17,18 Yet, there were important differences in trial design that made the optimal scenario for adoption of procalcitonin unclear. In one trial, procalcitonin was used only in adults with ARTIs who were judged by their physicians to require antibiotics, and thus the probability of empiric antibiotics in the usual care arm (97 %) and of an elevated procalcitonin level (9.9 %) were relatively high.17 In the other, procalcitonin testing was performed in all adults with ARTIs; thus, the probability of antibiotic use in the usual care arm (36.7 %) and of an elevated procalcitonin level (0.9 %) were relatively low.18 Our analyses suggest that, compared to procalcitonin use in all adults with ARTIs, procalcitonin use only in adults with ARTIs judged by their physicians to require antibiotics would have a higher likelihood of being cost-effective. This population is potentially large; > 50 % of patients in the United States presenting with ARTIs are prescribed an antibiotic.1–4 Using procalcitonin in this population has several advantages in that it preserves an important role for clinical judgment and reserves a costly test for patients with a higher pre-test probability of an abnormal result.
This study has several strengths. First, the two analyses used different parameters that reflect unique patient cohorts and results from each of two RCTs. Thus, our analyses closely approximate the cost-effectiveness of procalcitonin-guided antibiotic therapy as deployed in two RCTs, facilitating comparisons between the trials. Second, model results were relatively robust to parameter variation in sensitivity analyses and were in agreement with previous findings suggesting that antibiotic cost and physician adherence with algorithm recommendations are major determinants of the cost-effectiveness of procalcitonin testing.24 Of note, the secondary analyses that compared procalcitonin testing and usual strategies in terms of cost per QALY saved found that the ICER of procalcitonin testing was >$100,000/QALY in both cohorts, supporting our initial hypothesis that procalcitonin testing is unlikely to be cost-effective when the costs of antibiotic resistance are not considered.
We acknowledge several limitations of this study. First, this study assumes the availability of a point-of-care procalcitonin test, an assumption which biases the analysis towards procalcitonin testing prior to the emergence of a point-of-care test. Second, this study was based on two RCTs in which ARTIs included the common cold, acute pharyngitis, acute otitis media, acute bronchitis, influenza, community-acquired pneumonia, asthma exacerbations and chronic obstructive pulmonary disease exacerbations.17,18 Thus, broad physician acceptance of this study’s findings may be limited by the different management strategies and perceived value of antibiotics for each of these illnesses. Third, these analyses measure cost-effectiveness in costs per antibiotic safely avoided and estimate willingness-to-pay thresholds based on the health care system costs of antibiotic resistance per antibiotic prescription. This estimate for the willingness-to-pay threshold is potentially problematic in that it is based on an estimate for incremental total annual U.S. costs of antibiotic resistance, which itself has limitations given the complexity of quantifying resistance costs.25,26 Further, this estimate likely represents a lower bound estimate given the many potential sources of incremental costs attributable to antibiotic resistance, including treatment failure, use of costly second line antibiotics antibiotic stewardship programs and new antibiotic development. Fourth, this analysis relies on data from two European trials, and evidence suggests that physician compliance with procalcitonin protocols is higher among European physicians relative to U.S. physicians.27 When varied widely in sensitivity analyses, however, this parameter had a relatively minor impact on the favorability of the procalcitonin strategy.
In summary, this study suggests that procalcitonin-guided antibiotic therapy for management of adult ARTIs in the ambulatory setting would be cost-effective compared to usual care when the costs of antibiotic resistance are considered and procalcitonin testing is limited to adults with ARTIs judged by their physicians to require antibiotics. Given that > 50 % of adults with ARTIs in the United States are prescribed antibiotic therapy, the potential to reduce unnecessary antibiotic prescribing with procalcitonin testing is substantial.1,3
REFERENCES
Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302(7):758–66.
Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278(11):901–4.
Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33(5):757–62.
Huchon GJ, Gialdroni-Grassi G, Leophonte P, Manresa F, Shaberg T, Woodhead M. Initial antibiotic therapy for lower respiratory tract infection in the community: a European survey. Eur Respir J. 1996;9(8):1590–5.
Steinman MA, Landefield CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003;289(6):719–25.
Arroll B, Kenealy T. Antibiotics for the common cold and acute purulent rhinitis (review). Cochrane Database Syst Rev. 2010:CD000247.
Smith SM, Fahey T, Smucny J, Becker LA. Antibiotics for acute bronchitis (review). Cochrane Database Syst Rev. 2012:CD000245.
Ahovuo-Saloranta A, Rautakorpi UM, Borisenko OV, Liira H, Williams JW, Mäkelä M. Antibiotics for acute maxillary sinusitis (review). Cochrane Database Syst Rev. 2011:CD000243.
Goosens H, Ferech M, Stichele RB, Elseviers S. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365(9459):579–87.
van de Sande-Bruinsma N, Grundman J, Verloo D, et al. Antimicrobial drug use and resistance in Europe. Emerg Infect Dis. 2008;14(11):1722–30.
The Interagency Task Force on Antimicrobial Resistance. A public health action plan to combat antimicrobial resistance: 2012 update. Available at: www.cdc.gov/drugresistance/actionplan/actionplan.html. Accessed October 10, 2013.
Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2009:CD003539.
Goosens H, Guillemot D, Ferech M, et al. National campaigns to improve antibiotic use. Eur J Clin Pharmacol. 2006;62(5):373–9.
van der Meer V, Neven AK, van den Broek PJ, Assendelft WJJ Diagnostic value of C reactive protein in infections of the lower respiratory tract: a systematic review. BMJ. 2005;331(757):26.
Gonzales R, Aagaard EM, Camargo CA, et al. C-reactive protein testing does not decrease antibiotic use for acute cough illness when compared to a clinical algorithm. J Emerg Med. 2011;41(1):1–7.
Schuetz P, Chiappa V, Briel M, Greenwald JL. Procalcitonin algorithms for antibiotic therapy decisions: a systematic review of randomized controlled trials and recommendations for clinical algorithms. Arch Intern Med. 2011;171(15); 1322–31.
Briel M, Schuetz P, Mueller B, et al. Procalcitonin-guided antibiotic use vs a standard approach for acute respiratory tract infections in primary care. Arch Intern Med. 2008;168(18): 2000–7.
Burkhardt O, Ewig S, Haagen U, et al. Procalcitonin guidance and reduction of antibiotic use in acute respiratory tract infection. Eur Respir J. 2010;36(3): 601–7.
Mainous AG, Hueston WJ. The cost of antibiotics in treating upper respiratory tract infections in a Medicaid population. Arch Fam Med. 1998;7(Jan/Feb):45–9.
Centers for Medicare & Medicaid Services. New Clinical Laboratory Fee Schedule Test Codes. Procalcitonin. Available at: www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/Downloads/CY2011-CLFS-New-Test-Codes.pdf. Accessed October 10, 2013.
Gonzales R, Corbett KK, Wong S, et al. “Get Smart Colorado,” Impact of a mass media campaign to improve community antibiotic use. Med Care. 2008;46(6):597–605.
Oppong R, Billingsley K, Nuttall J, Hood K, Smith RD, Cost J. The impact of using different tariffs to value EQ-5D health state descriptions: an example from a study of acute cough/lower respiratory tract infections in seven countries. Eur J Health Econ. 2013;14(2):197–209.
Gold MR, Franks P, McCoy KI, Fryback DG. Toward consistency in cost-utility analysis: using national measures to create condition-specific values. Med Care. 1998;36(6):778–92.
Smith KJ, Wateska A, Nowalk MP, Raymund M, Lee BY, Zimmerman RK, Fine MJ. Cost-effectiveness of procalcitonin-guided antibiotic use in community acquired pneumonia. J Gen Intern Med. 2013;28(9):1157–64.
Bush K, Courvalin P, Dantas G, et al. Tackling antibiotic resistance. Nat Rev Microbiol. 2011; December(9):894–6.
Phelps T. Bud/drug resistance: sometimes less is more. Med Care. 1989;27(2): 194–203.
Albrich WC, Dusemund F, Bucher B, et al. Effectiveness and safety of procalcitonin-guided antibiotic therapy in lower respiratory tract infections in “real life”: an international, multicenter poststudy survey (ProREAL). Arch Intern Med. 2012;172(9):715–22.
Annual Salary, Physician – Internal Medicine. Available at www1.salary.com/Physician-Infectious-Disease-Salary.html. Accessed October 10, 2013.
The Pew Charitable Trusts Health Initiative. Record-high antibiotic sales for meat and poultry production. Available at: www.pewhealth.org/other-resource/record-high-antibiotic-sales-for-meat-and-poultry-production-85899449119. Accessed October 10, 2013.
Wise R, Hart T, Cars O, et al. Antimicrobial resistance is a major threat to public health. BMJ. 1998;September 5(317):609–10.
Hersh AL, Shapiro DJ, Pavia AT, Shah S. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128(6):1053–61.
Hersh AL, Shapiro DJ, Hicks LA. Antibiotic prescribing in ambulatory care in the United States: estimates from the National Ambulatory and National Hospital Ambulatory Medical Care Surveys (NAMCS/HAMCS). Abstract, 2012 IDWeek Conference.
Acknowledgements
This study was supported by the National Institute of Allergy and Infectious Diseases (Grant No. R01AI076256), the National Institute of Health (T32 Grant No. AG21885) and the Doris Duke Charitable Foundation. This study has not previously been presented in part or in full at any prior conference.
Conflict of Interest
Dr. Zimmerman and Dr. Nowalk have a research grant from Merck to study the HPV vaccine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michaelidis, C.I., Zimmerman, R.K., Nowalk, M.P. et al. Cost-Effectiveness of Procalcitonin-Guided Antibiotic Therapy for Outpatient Management of Acute Respiratory Tract Infections in Adults. J GEN INTERN MED 29, 579–586 (2014). https://doi.org/10.1007/s11606-013-2679-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-013-2679-7