ABSTRACT
BACKGROUND
Hospitalized patients frequently misuse their respiratory inhalers, yet it is unclear what the most effective hospital-based educational intervention is for this population.
OBJECTIVE
To compare two strategies for teaching inhaler use to hospitalized patients with asthma or chronic obstructive pulmonary disease (COPD).
DESIGN
A Phase-II randomized controlled clinical trial enrolled hospitalized adults with physician diagnosed asthma or COPD.
PARTICIPANTS
Hospitalized adults (age 18 years or older) with asthma or COPD.
INTERVENTIONS
Participants were randomized to brief intervention [BI]: single-set of verbal and written step-by-step instructions, or, teach-to-goal [TTG]: BI plus repeated demonstrations of inhaler use and participant comprehension assessments (teach-back).
MAIN MEASURES
The primary outcome was metered-dose inhaler (MDI) misuse post-intervention (<75% steps correct). Secondary outcomes included Diskus® misuse, self-reported inhaler technique confidence and prevalence of 30-day health-related events.
KEY RESULTS
Of 80 eligible participants, fifty (63%) were enrolled (BI n = 26, TTG n = 24). While the majority of participants reported being confident with their inhaler technique (MDI 70%, Diskus® 94%), most misused their inhalers pre-intervention (MDI 62%, Diskus® 78%). Post-intervention MDI misuse was significantly lower after TTG vs. BI (12.5 vs. 46%, p = 0.01). The results for Diskus® were similar and approached significance (25 vs. 80%, p = 0.05). Participants with 30-day acute health-related events were less common in the group receiving TTG vs. BI (1 vs. 8, p = 0.02).
CONCLUSIONS
TTG appears to be more effective compared with BI. Patients over-estimate their inhaler technique, emphasizing the need for hospital-based interventions to correct inhaler misuse. Although TTG was associated with fewer post-hospitalization health-related events, larger, multi-centered studies are needed to evaluate the durability and clinical outcomes associated with this hospital-based education.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Health care reform and recent efforts to improve patient safety have fostered the development, testing, and implementation of novel strategies to coordinate and improve transitions of care at hospital discharge.1,2 These interventions have largely focused on broad concepts such as medication reconciliation,3 patient-care handoffs,4,5 and adherence to prescribed therapies.6 The use of hospital-based education to improve patient self-management skills is an under-studied component of this care.7 Self-management skills allow patients to participate in their care post-hospital discharge, empowering patients and thereby aiming to reduce adverse post-discharge events such as emergency department visits, hospitalizations, and deaths. However, the most effective approach to providing this hospital-based education is still not known.
Asthma and chronic obstructive pulmonary disease (COPD), two of the most common lung disorders, together result in over a million hospitalizations in the United States annually and require significant patient self-management for optimal health.8,9 There is increasing national interest in improving the quality of care for both of these conditions.10,11 COPD, for instance, is the third leading cause of 30-day hospital readmissions.12 Clinical practice guidelines for both asthma and COPD recommend that clinicians assess and teach respiratory inhaler technique at all points of care, including during hospitalizations.13,14 However, studies that we and others have conducted have found that the vast majority of patients hospitalized with asthma or COPD misuse their inhalers.15,16 Improving patients’ ability to use inhalers may help prevent adverse events post-hospital discharge, including hospital readmissions.17–19
Although a handful of randomized trials have demonstrated beneficial effects of hospital-based patient self-management education for asthma,20–23 these studies employed multi-faceted, time-intensive interventions that were compared to usual care. While this literature encourages the use of hospital-based education, direction is lacking as to which intervention or component is most effective. Data are even more limited for patients with COPD. Therefore, data are necessary to demonstrate the effectiveness of educational strategies with discrete components, such as inhaler technique. The objective of our study was therefore to compare two hospital-based interventions to teach inhaler use for inpatients with asthma or COPD.
METHODS
Study Design
A Phase-II, block randomized, stratified clinical trial was used to compare two educational interventions to instruct hospitalized patients with asthma or COPD on respiratory inhaler technique. A biostatistician generated the random allocation sequence (investigators were masked to the block sequences) and assigned participants to interventions. Study investigators and research assessors (RAs) were masked to the intervention. The study was approved by the University of Chicago Institutional Review Board (16900A).
Study Participants
Research staff screened electronic admission-logs Monday through Friday. Patients who met all inclusion criteria and none of the exclusion criteria were eligible to participate. Inclusion criteria included: age of 18-years or older, hospitalized on an inpatient medical service, had a physician diagnosis of asthma or COPD, expected to be discharged home on metered dose inhaler [MDI] by their inpatient physician. Exclusion criteria included: currently in intensive care, no physician assent, unable to provide written informed consent, or previous study participant. Patients who provided written informed consent were enrolled.
Study Procedures
Participants completed interviewer-administered surveys collecting participant demographics (e.g., age, sex, Hispanic vs. non-Hispanic ethnicity, white vs. non-white race) and smoking history (ever [>100 lifetime cigarettes] vs. never). Participants’ baseline utilization of healthcare services for asthma or COPD was assessed by: 1) determining if the participants had sought care in the outpatient setting for their asthma or COPD prior to admission; 2) the number of hospitalizations for asthma or COPD in the past 12-months; and 3) any lifetime near-fatal respiratory event (≥1 intensive care unit admission(s) and/or intubation).
Participants rated their confidence in their ability to use respiratory inhalers using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree) using the following question: “I am confident that I know how to use this [insert MDI or Diskus®] respiratory inhaler correctly.” Inhaler technique was assessed by a trained RA using detailed checklists for MDI (12-steps) and Diskus® (10 steps).15 Misuse was defined as <75% of steps correct for each device (<9/12 steps for MDI; <8/10 steps for Diskus®).15
Because inadequate health literacy is associated with poor inhaler technique,24,25 participants’ health literacy was measured using the Short Test of Functional Health Literacy in Adults (STOFHLA),26,27 a 36-item written comprehension test (scores: range 0-36); less-than-adequate: <23/36; adequate: ≥23/36.26 Participants with screened visual acuity better than 20/50 in ≥1 eye were eligible to complete the STOFHLA.26
Intervention
Upon completion of the initial assessments, participants were randomized to one of two alternate educational strategies, “teach-to-goal” [TTG] and “brief intervention” [BI]. (Text box 1, Fig. 1) The TTG intervention was chosen based on preliminary results from prior work that demonstrated its success as a hospital-based approach for teaching the use of respiratory inhalers.15,16 A variety of alternative comparators were considered, including usual care. Because usual care may vary by institution and provider, a standardized but limited educational strategy, dubbed “brief intervention” (BI) was chosen. The time it took to complete the inhaler education was recorded for both interventions.
Textbox 1. Side-by-Side Comparison of TTG* vs. BI† Education

TTG Intervention
The TTG educational strategy employed repeated rounds of assessment and education with the aim of participants’ mastering inhaler technique (i.e., 12/12 steps correct for MDI; 10/10 steps correct for Diskus®).15 The first step of the TTG intervention utilized trained, masked RAs to evaluate participants’ baseline inhaler technique. The RA left the room and a trained research educator (RE) provided a demonstration of correct inhaler use, followed by re-assessment of participants’ technique (i.e., “teachback”). The cycle was repeated for up to two rounds for any participant who did not demonstrate mastery. Finally, participants received written instructions and a pamphlet describing basic information about their condition (asthma vs. COPD). After completion of the educational intervention, the RA performed a final assessment of participants’ technique.
BI Intervention
Participants randomized to BI also underwent an initial assessment by the masked RA. The trained RE then entered and simply provided the participant with verbal instructions (i.e., read each step out-loud without any demonstration) as well as a copy of the written instructions. To make the treatments approximately equal in time, the BI group received verbal education on the pamphlet for their condition (asthma vs. COPD). After completion of the education, the RA performed a final assessment of the participants’ technique.
Follow-up Interviews
Symptom questionnaires and utilization of health care services was collected at 30-days post-hospital discharge using a 10-minute phone interview. Acute health-related events were defined as one or more event for a participant that included: all-cause emergency department visits, hospitalizations, or deaths within 30 days after hospital discharge.
Statistical Analyses
Outcomes were determined a priori. The primary outcome was differential post-education prevalence of inhaler misuse for MDI. Secondary outcomes included differential post-education prevalence of inhaler misuse for Diskus®, acute health-related events at 30 days, and self-reported confidence for inhaler use. Descriptive statistics included means, standard deviations, and proportions. Two sample t-tests were used to test for differences in means. Chi-square or Fisher’s exact test was used to test for differences in the prevalence of MDI or Diskus® misuse and acute health-related events at 30 days in the TTG vs. BI groups. Self-reported confidence for inhaler use was analyzed as a dichotomous variable using McNemar’s test. A two-tailed p-value of less than 0.05 defined statistical significance. As this was a Phase-II trial, power calculations were not performed; rather the data were collected in part to be used to estimate treatment effect size. SAS 9.3.1 was used to create the randomization schedule by random number generation. All statistical analyses were performed using STATA version 11 (College Station, Texas: StataCorp LP).
RESULTS
Baseline Characteristics
Of 80 eligible participants, 50 (63%) were enrolled and randomized into TTG (n = 24) or BI (n = 26) between July 2009 and April 2010. (Fig. 2) Participants’ mean age was 54 years. The majority had a diagnosis of COPD, were African American, female, and had been hospitalized within the past 12 months. Almost half had had a near-fatal respiratory event. Almost all participants had a healthcare provider for their asthma or COPD. Among the 50% who had sufficient vision, one-quarter had less-than-adequate health literacy. All participants had previously been prescribed MDIs; 18 had been prescribed Diskus® devices. Baseline characteristics were similar in both groups, although there was a higher proportion of less-than-adequate health literacy in the BI versus TTG group. (Table 1)
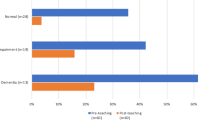
The majority of participants misused MDI and Diskus® devices (BI vs. TTG: 78% vs. 65%; 80% vs. 75%, respectively) at baseline. (Fig. 3) Of the 72% who were confident in their MDI technique, more than two-thirds (69%) misused their MDIs. Almost all participants (94%) were confident in their Diskus® technique. Among these participants, three-quarters (76%) misused their device.
a) Percentage of patients demonstrating incorrect use of metered-dose inhaler (MDI) before and after either a brief intervention (BI) or TTG intervention (TTG). b) Percentage of patients demonstrating incorrect use of Diskus inhaler before and after either a brief intervention (BI) or TTG intervention (TTG).
Outcomes
Inhaler Technique
TTG took three times longer than BI (mean of 6.3 vs. 2 minutes, p < 0.0001) to teach inhaler technique. The proportion who misused MDIs post-intervention decreased in both groups. Among the 50 participants tested for MDI misuse, prevalence of misuse significantly decreased both post-BI education compared to pre-BI education (78 vs. 46%, p = 0.008) and post-TTG education compared to pre-TTG education (65 vs. 13%, p = 0.01); however, TTG post-education MDI misuse prevalence was significantly lower for those receiving TTG compared to those receiving BI education (13% vs. 46%, p = 0.01). (Fig. 3a) There was also a non-significant decrease in prevalence of Diskus® misuse after TTG compared to BI. Among the 18 participants tested for Diskus® misuse, prevalence of misuse post-BI education compared to pre-BI education remained the same (80 vs. 80%, p > 0.999). While prevalence of misuse decreased post-TTG education compared to pre-TTG education (75 vs. 25%, p = 0.13), the findings were not statistically significant. TTG post-education Diskus® misuse prevalence was lower for those receiving TTG compared to those receiving BI education (25 vs. 80, p = 0.05, borderline significance). (Fig. 3b)
Acute Health-Related Events Within 30 Days Post-Discharge
Thirty-nine participants (78%) had follow-up data (BI n = 20, TTG n = 19), the remainder were lost to follow-up. Compared to those with follow-up data, participants without data were just as likely to misuse MDI and Diskus® devices at baseline (77 vs. 73%; 75 vs. 100%, respectively), be hospitalized within the previous 12 months (59 vs. 55%), or have had near-fatal respiratory events (44 vs. 45%) prior to this admission. Nine participants had one or more all-cause acute health-related events at 30 days post-discharge (BI n = 8, TTG n = 1). Individuals with an event(s) were eight-times as common in the BI group than in the TTG group (40 vs. 5%, p = 0.02). There were 6 participants with ED visits and/or hospitalizations (BI n = 5, TTG n = 1), and 3 separate participants who died (BI n = 3, TTG =0) prior to 30 days post-discharge. Due to missing data on post-discharge health events, a sensitivity analysis was performed. The prevalence of replacing participants’ missing data with ‘no event,’ vs. replacing with an ‘event’ was 18% (TTG 31 vs. BI 4%, p = 0.024) vs. 40% (TTG 54 vs. BI 25%, p = 0.048).
DISCUSSION
Hospital-based education is successful in reducing inhaler misuse in this patient population. TTG was generally more effective than BI in reducing misuse of MDI and Diskus® devices, though differences were significant only for MDI. Moreover, we found that participants in the TTG group had significantly fewer acute health-related events at 30 days than those in the BI group.
Our study extends the literature on hospital-based assessment and educational interventions for inpatients with asthma or COPD. While studies have evaluated patient preference for inhaler devices,28,29 to our knowledge, this is the first study to directly compare inhaler technique confidence versus technique. These findings suggest that hospital-based interventions for assessment and instruction on respiratory inhaler use may be required for all hospitalized patients with asthma or COPD, not only those who self-report the inability to use inhalers. Further, it is the first randomized trial that we are aware of that specifically evaluates hospital based self-management education for patients with COPD. Our study is also unique in that it directly compares two interventions for patients with asthma or COPD. Finally, the educational strategies studied a single component, inhaler technique, that can be replicated and inform future studies and/or practice.
The finding that the TTG intervention was superior to BI for providing this hospital-based education on respiratory inhaler use may be due to a phenomenon termed the “testing effect.”30 This is a phenomenon whereby memory is enhanced through the act of retrieving information while learning. The TTG technique has been endorsed as a patient safety standard by the National Quality Forum for informed consent,31 and has been used for heart failure educational interventions,32 and has been successful among patients hospitalized with asthma and COPD.15,16 Because TTG uses ‘teachback,’ (i.e., re-assessment after education), inhaler technique recall may be enhanced for this group.
Finally, we were interested to find that participants receiving BI were eight-times more likely to have a post-discharge health event than those receiving TTG. This may signal that TTG has durable and clinically important effects for patients after they have been discharged, perhaps related to the testing effect phenomenon. However, it is difficult to assign causality based on this study alone. The role(s) of health literacy and/or vision, are left unanswered by our data, but may have played a role in the differential findings. These results are also limited by loss-to-follow-up for a fifth of our participants. Further, the health-related events were self-reported, and it is possible that not all health events were captured. Therefore, these findings simply signal that more work needs to be done to understand the true differential effectiveness of TTG versus BI.
There are other limitations of our study. First, although a key strength of the current study is that we employed two active comparators for both rescue and controller type devices, results were not consistent between the two devices. For instance, both TTG and BI proved to have merit for MDI devices, but only TTG tended to decrease Diskus® misuse. The reasons for this differential effect of BI by inhaler device are unclear; though it may be due to insufficient power.
Second, we were unable to determine if health literacy modified the relative effects of TTG and BI on inhaler use. Our study employed a written health literacy test. Unfortunately, only half the participants had sufficient vision to complete it, leading to small numbers of patients in either group (TTG, BI) with health literacy data. Given the known effect of health literacy on self-management skills and clinical outcomes,33–36 our study informs the planning of future studies. For instance, it may be necessary to either use a measure not dependent on vision (e.g., interview-based assessment), or to stratify based on level of health literacy. It will be important for future studies to evaluate which sub-groups may benefit from BI alone, and which may require the more intensive TTG strategy (e.g., health literacy levels), as BI may be ideal for low-resource environments, while the added resources required to provide TTG may be justified to prevent costly and morbid risks associated with repeated acute exacerbations and re-hospitalizations for some patients.
One element of this Phase-II study was to develop estimates of the comparative effect sizes of TTG compared to BI, and was therefore not powered to evaluate device-specific differences in misuse following education. Future studies should enroll a sufficient sample size to determine device-specific differences in teaching strategies. It was also beyond the scope of this study to test the durability of the interventions; a study with post-discharge assessments is needed. Similarly, although a signal was found that TTG may reduce the risk of post-hospital acute health-related events versus BI, the study was not powered on this outcome. These data, therefore, must be considered in light of the non-trivial missing data for both groups, limiting the conclusions that can be drawn. Further, we did not assess for participants’ self-reported inhaler education that they may or may not have received prior to this hospitalization.
Finally, the results from this study may not be generalizable because the enrolled participants represented a high-risk, predominantly minority population (though limited ethnic diversity), from one urban academic center. However, since this population is often under-studied, data from our study may inform efforts to reduce health disparities, particularly if larger, multi-institutional studies replicate our findings. Also, the study was limited to English-speaking participants and all educational materials were provided in English. Future work will need to study whether these educational strategies are effective in other languages and/or for patients whose first language is not English.
In summary, our study found that providing hospital-based education on inhaler technique for inpatients with asthma or COPD can decrease risk of misuse at the time of hospital discharge. The TTG strategy may be particularly effective at educating patients on inhaler use, compared to a brief intervention. Our study also shows that relying on patient self-report is problematic for identifying patients in need of educational interventions for respiratory inhaler use, further emphasizing the need for hospital-based assessment and education. Finally, our study found a signal that may indicate that TTG could lead to improved clinical outcomes compared to BI. Larger, multi-institution comparative studies are needed to evaluate the effects of TTG vs. BI in different patient subgroups (e.g., patients with and without limited health literacy, patients using a variety of respiratory inhaler devices), to test the durability of hospital-based education after discharge from the hospital, and to understand the implications of the interventions (BI vs. TTG) on clinical outcomes and fostering safe transitions of care.
References
Connors EE, Gostin LO. Health care reform--a historic moment in US social policy. JAMA. Jun 23 2010;303(24):2521–2522.
Washington AE, Lipstein, SH. The Patient-Centered Outcomes Research Institute--Promoting Better Information, Decisions, and Health. N Engl J Med. 2011:365(15):e31..
Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge: a review of key issues for hospitalists. J Hosp Med. Sep 2007;2(5):314–323.
Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. Sep 2009;4(7):433–440.
Coleman EA, Smith JD, Raha D, Min SJ. Post hospital medication discrepancies: prevalence and contributing factors. Arch Intern Med. Sep 12 2005;165(16):1842–1847.
Kripalani S, Robertson R, Love-Ghaffari MH, et al. Development of an illustrated medication schedule as a low-literacy patient education tool. Patient Educ Couns. Jun 2007;66(3):368–377.
Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. Aug 9–23 2004;164(15):1641–1649.
Centers for Disease Control and Prevention: FastStats: Asthma. Available at: http://www.cdc.gov/asthma/default.htm. Accessed March 13, 2012.
World Health Organization: Chronic obstructive pulmonary disease (COPD). Available at: http://www.who.int/respiratory/copd/en/. Accessed March 13, 2012.
2010 Physician Quality Reporting Imitative (PQRI) Measures. Available at: https://www.cms.gov/PQRS/Downloads/2010_PQRI_MeasuresList_111309.pdf. Accessed March 13, 2012.
Healthy People 2020 Topics and Objectives. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx. Accessed March 13, 2012.
Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. Oct 11 2010;170(18):1664–1670.
Guidelines for the Diagnosis and Management of Asthma (EPR-3). Available at: https://www.nhlbi.nih.gov/guidelines/asthma/. Accessed March 12, 2013.
The Global initiative for Chronic Obstructive Disease (GOLD) Guidelines: Available at: http://www.goldcopd.com/. Accessed March 13, 2012.
Press VG, Arora VM, Shah LM, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med. Jun 2011;26(6):635–642.
Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. Oct 15 2005;172(8):980–986.
Hanania NA, Darken P, Horstman D, et al. The efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus inhaler for the treatment of COPD. Chest. Sep 2003;124(3):834–843.
Mathison DA, Koziol JA. Utility and efficacy of fluticasone propionate and salmeterol inhaled from a single inhaler for persistent asthma. J Asthma. Dec 2005;42(10):829–831.
Celli BR, Thomas NE, Anderson JA, et al. Effect of pharmacotherapy on rate of decline of lung function in chronic obstructive pulmonary disease: results from the TORCH study. Am J Respir Crit Care Med. Aug 15 2008;178(4):332–338.
George MR, O’Dowd LC, Martin I, et al. A comprehensive educational program improves clinical outcome measures in inner-city patients with asthma. Arch Intern Med. Aug 9–23 1999;159(15):1710–1716.
Morice AH, Wrench C. The role of the asthma nurse in treatment compliance and self-management following hospital admission. Respir Med. Nov 2001;95(11):851–856.
Castro M, Zimmermann NA, Crocker S, Bradley J, Leven C, Schechtman KB. Asthma intervention program prevents readmissions in high healthcare users. Am J Respir Crit Care Med. Nov 1 2003;168(9):1095–1099.
Osman LM, Calder C, Godden DJ, et al. A randomised trial of self-management planning for adult patients admitted to hospital with acute asthma. Thorax. Oct 2002;57(10):869–874.
Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. Nov 2003;51(3):267–275.
Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. Oct 1998;114(4):1008–1015.
Nurss JR PR, Williams MV, Baker, DW. Short Test of Functional Health Literacy in Adults (STOFHLA). Peppercorn Books and Press; 2001.
Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. Sep 1999;38(1):33–42.
van der Palen J, Klein JJ, van Herwaarden CL, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. Eur Respir J. Nov 1999;14(5):1034–1037.
Innes JA, Lenney J, Crompton GK. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. Resp Med. May 2000;94(5):496–500.
Roediger HL, Karpicke JD. The Power of Testing Memory Basic Research and Implications for Educational Practice. Perspect Psychol Sci. Sep 2006;1(3):181–210.
Wu HW NR, Page-Loez CM, Kizer KW. Improving Patient Safety Through Informed Consent for Patients with Limited Health Literacy. An implementation report. 2005. Accessed May 7, 2010.
Baker DW, Dewalt DA, Schillinger D, et al. "Teach to Goal": Theory and Design Principles of an Intervention to Improve Heart Failure Self-Management Skills of Patients with Low Health Literacy. J Health Commun. Sep 30 2011;16(sup3):73–88.
Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. Jama-J Am Med Assoc. Jul 24 2002;288(4):475–482.
Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. J Gen Intern Med. Aug 2006;21(8):813–817.
Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J Gen Intern Med. Dec 1998;13(12):791–798.
Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. Jul 23 2007;167(14):1503–1509.
Acknowledgements
Contributors
We would like to thank the members of the Data and Safety Monitoring Board. In addition, we would like to thank the research staff of the University of Chicago Asthma and COPD Center and the University of Chicago Data and Biostatistics Management Core. Finally, we would like to thank Nicole Babuskow for her essential help with this project.
Funding
Dr. Press reports receiving funding from the Institute for Translational Medicine, University of Chicago CTSA from the National Center for Research Resources (UL1RR024999). Dr. Krishnan reports funding from the National Institutes of Health [HL101618] and the Agency for Healthcare Research and Quality [HS016967].
Prior Presentations
Prior poster presentations include the 2010 and 2011 Society of General Internal Medicine Annual Meetings in Minneapolis, Minnesota and Phoenix, Arizona respectively, the 2010 Society for Hospital Medicine Annual Meeting in Washington, DC, the 2011 Midwest Society of General Internal Medicine Regional Meeting in Chicago, Illinois, and the 2011 Midwest Society of Hospital Medicine. Prior oral presentations include the 2011 American Thoracic Society International Meeting in Denver Colorado.
Conflict of Interest
Dr. Shah is employed with a for profit company, Clinovations; Dr. Naureckas has provided expert testimony for Cook County; none of the other authors have conflicts of interest to disclose related to employment, consultancies, honoraria, stock, expert testimony, patents, royalties or any other relationships.
Author information
Authors and Affiliations
Corresponding author
Additional information
Registry Number: Clinicaltrials.gov NCT01456494
Rights and permissions
About this article
Cite this article
Press, V.G., Arora, V.M., Shah, L.M. et al. Teaching the Use of Respiratory Inhalers to Hospitalized Patients with Asthma or COPD: a Randomized Trial. J GEN INTERN MED 27, 1317–1325 (2012). https://doi.org/10.1007/s11606-012-2090-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2090-9