ABSTRACT
BACKGROUND
Patients are asked to assume greater responsibility for care, including use of medications, during transitions from hospital to home. Unfortunately, medications dispensed via respiratory inhalers to patients with asthma or chronic obstructive pulmonary disease (COPD) can be difficult to use.
OBJECTIVES
To examine rates of inhaler misuse and to determine if patients with asthma or COPD differed in their ability to learn how to use inhalers correctly.
DESIGN
A cross-sectional and pre/post intervention study at two urban academic hospitals.
PARTICIPANTS
Hospitalized patients with asthma or COPD.
INTERVENTION
A subset of participants received instruction about the correct use of respiratory inhalers.
MAIN MEASURES
Use of metered dose inhaler (MDI) and Diskus® devices was assessed using checklists. Misuse and mastery of each device were defined as <75% and 100% of steps correct, respectively. Insufficient vision was defined as worse than 20/50 in both eyes. Less-than adequate health literacy was defined as a score of <23/36 on The Short Test of Functional Health Literacy in Adults (S-TOFHLA).
KEY RESULTS
One-hundred participants were enrolled (COPD n = 40; asthma n = 60). Overall, misuse was common (86% MDI, 71% Diskus®), and rates of inhaler misuse for participants with COPD versus asthma were similar. Participants with COPD versus asthma were twice as likely to have insufficient vision (43% vs. 20%, p = 0.02) and three-times as likely to have less-than- adequate health literacy (61% vs. 19%, p = 0.001). Participants with insufficient vision were more likely to misuse Diskus® devices (95% vs. 61%, p = 0.004). All participants (100%) were able to achieve mastery for both MDI and Diskus® devices.
CONCLUSIONS
Inhaler misuse is common, but correctable in hospitalized patients with COPD or asthma. Hospitals should implement a program to assess and teach appropriate inhaler technique that can overcome barriers to patient self-management, including insufficient vision, during transitions from hospital to home.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Transitions in care from hospitals to home are increasingly recognized as a vulnerable period in which patients and their caregivers are asked to assume greater responsibility for their healthcare,1–3 particularly medication management.4,5 This may be especially problematic for patients with asthma or chronic obstructive pulmonary disease (COPD) who are commonly prescribed medications dispensed through respiratory inhalers.6,7 Although inhaled medications offer the advantage of targeted delivery to the site of action (airways), they can be difficult to use8 and require multiple-steps for use.9–13 Moreover, symptom control and prevention of exacerbations often require combination therapy with two or more types of inhalers (e.g., metered-dose-inhalers [MDI], Diskus®), requiring patients to learn and master a different series of device-specific instructions. At times, these instructions are in direct conflict, causing confusion. For instance, patients should inhale slowly when using MDIs, but inhale quickly when using Diskus® devices.
Studies to date on inhaler use focus on patients with asthma and use of MDI devices, 9–11,14,15 and have found multiple risk factors for high rates of inhaler misuse, including the use of multiple devices,11 inadequate instruction,16–18 and low health literacy.9,12,19 Our study is novel from two perspectives. First, although COPD is as prevalent as asthma in the United States and is associated with substantially higher mortality than asthma, data regarding inhaler misuse in hospitalized patients with COPD are limited.20 For example, it is unclear if hospitalized patients with COPD have high rates of inhaler misuse and what barriers may exist in the ability of patients with COPD to learn inhaler technique. Because COPD primarily affects older patients who are at increased risk of poor vision21 and low health literacy,22 hospitalized patients with COPD may have high rates of inhaler misuse.
Second, to our knowledge, no studies have examined the use of Diskus® devices in hospital settings, even though they are routinely prescribed at hospital discharge. Incorrect use of Diskus® devices can cause inadequate dosing or distribution of medication.23 Thus, incorrect use of Diskus® inhalers may represent a missed-opportunity for patients to benefit from highly efficacious therapy.24,25 It is not known how common misuse of Diskus devices is for hospitalized patients with asthma or COPD.
Guidelines for asthma and COPD recommend assessing and correcting inhaler technique at all healthcare encounters, including hospitals.17,18 Therefore, the objective of this study was to extend the existing literature by examining rates of misuse of respiratory inhalers for both rescue and controller medications among hospitalized patients with either asthma or COPD. The secondary objective was to determine if patients with asthma and COPD differed in their ability to learn how to use inhalers correctly.
METHODS
Study participants
The study was conducted from September 2007 to March 2009. Research staff reviewed electronic admission-logs Monday through Friday to identify patients hospitalized with asthma or COPD. Patients who met all inclusion criteria (age of 18-years or older and hospitalized on a medical service with a physician diagnosis of asthma or COPD) and none of the exclusion criteria (inability to provide informed written consent [e.g., non-English speaking, too ill to participate], or previous participant of the study) were eligible to participate. Patients who provided written consent and whose physicians assented were included. The study was approved by the University of Chicago Medical Center and Mercy Hospital and Medical Center Institutional Review Boards.
Study procedures
Participants completed an interviewer-administered survey collecting information on sociodemographics (age, sex, ethnicity, race [white vs. non-white]), and smoking history (ever vs. never). Further, participants’ utilization of several health-services for asthma or COPD was evaluated and included 1) whether participants had a healthcare provider who treats their asthma or COPD (generalist [general practitioner, internist, family medicine physician, nurse practitioner]; specialist [pulmonologist or allergist], or none); 2) number of hospitalizations for asthma or COPD in the past 12-months; and 3) near-fatal respiratory events (intensive care unit admission or intubation in their lifetime).
Health literacy was measured using the Short Test of Functional Health Literacy in Adults (S-TOFHLA).26,27 The S-TOFHLA measures reading comprehension by having participants read sentences (font-size 14) from medical scenarios with missing key words and having them select words from a multiple-choice list to complete the sentences. Participants have up-to seven minutes to complete the 36-item instrument and receive one point for each correct answer. Participants were classified as having less-than-adequate (score <23) or adequate (score ≥23-36) health literacy.26 Prior to administration of the S-TOFHLA, vision was assessed (Snellen screening chart).25 Patients who used corrective-lenses were instructed to use them. Vision was defined as insufficient to complete the S-TOFHLA instrument if vision was worse than 20/50 in both eyes.26
Lung function was measured using the KoKo PFT System for spirometry (version 4.3; PDS, Louisville, Colorado). For safety reasons, participants were excluded from spirometry if systolic and diastolic blood pressures were higher than 180 millimeters-mercury (mmHg) and/or 100 mmHg, respectively, or if trained research assistant did not consider them to be medically stable.
Inhaler technique was assessed utilizing detailed checklists (12-steps for MDI, 10-steps for Diskus®, [Text boxes 1 and 2]). Participants were eligible for assessment of inhaler technique if they had been prescribed the device prior to hospitalization. There is no consensus on the most appropriate threshold for defining correct versus incorrect use of respiratory inhalers. Previous studies demonstrate a wide-range of definitions for incorrect inhaler technique (i.e. inhaler misuse), from anywhere less than 60% of steps correct to less-than 100% of steps correct. 9–13 In the current study, misuse of MDI or Diskus® was defined as <75% of steps correct for each respective device (< 9 of 12 steps for MDI; < 8 of 10 steps for Diskus®). Our threshold is a conservative mid-point that falls within the broad-range of definitions above. The checklists used in this study were developed based on a review of package-inserts and the published literature,6,9–13 and modified by the research team to explicitly identify individual inhaler steps to improve inter-rater reliability (sample of n = 10, kappa for MDI =0.94, kappa for Diskus® =1.0).


We also evaluated whether patients differed in their ability to learn inhaler technique by testing a standardized educational intervention called “teach-to-goal” (TTG) using a pre/post study design. This component of the study was added to the initial cross-sectional study because baseline rates of misuse were so high at the mid-study interim analysis (May 2008). Therefore, all participants enrolled after this interim-analysis received TTG education. TTG is an intervention that assesses skills or knowledge at baseline, then reassesses with patient “teachback” after an educational intervention is performed; this cycle is continued until mastery of the skill or knowledge has been attained. 9,28 The TTG technique is often used in patient safety, has been endorsed as a patient safety standard by the National Quality Forum for informed consent,28 and has been successful among hospitalized with asthmatics.9 In this study, trained research assistants first screened participants’ inhaler technique; those who did not have mastery were provided with both verbal instructions and a demonstration of proper technique. After the first-round of the TTG teaching session, participants were asked to re-demonstrate how to use the inhaler correctly (i.e. “teach-back”). A second-round of teaching was provided, if the participant did not demonstrate mastery during the participants’ teach-back
Statistical analyses
Descriptive statistics used means, standard deviations, and proportions. T-tests were used to test for differences in means. Chi-squared or Fisher’s exact test was used to test for bivariate associations for our primary objectives of comparing inhaler misuse for patients with asthma compared to COPD and our secondary objective of comparing participants’ ability to learn inhaler technique for those with COPD compared to asthma. A two-tailed p-value of less than 0.05 defined statistical significance. Computations were performed using STATA version 10 (StataCorp).
RESULTS
Demographic and descriptive data (Table)
Of the 146 patients that were eligible, 100 participants (68%) were enrolled (Fig. 1). Reasons for declining to participate included not feeling well, not feeling as though they needed education about inhaler use, or simply declining without further explanation. The mean age was 52 years, and the majority of participants had asthma, were African American, female, had been hospitalized within the past 12 months, and had a history of a near-fatal respiratory event. Further, the majority of participants had a healthcare provider (approximately half saw a generalist, and one-third saw a specialist).
More than one-in-four participants had insufficient vision. Of these 29 participants, 3 (10%) were never prescribed corrective lenses, 18 (62%) were prescribed corrective-lenses but did not have them available in the hospital, and 8 (28%) were wearing their corrective-lenses. Of the 71 participants with sufficient vision to complete the S-TOFHLA, approximately one-third (n = 23, 32%) had less-than-adequate health literacy.
Asthma vs. COPD
In general, participants with COPD and participants with asthma had similar characteristics Table 1. However, compared to participants with asthma, COPD participants were older, more likely to be an ever smoker, had worse lung function, were twice as likely to have insufficient vision, and had less-than-adequate health literacy (19% vs. 61%, p = 0.001).
Misuse of respiratory inhalers
All enrolled participants had been previously prescribed an MDI and/or Diskus® device. Nearly all participants with asthma or COPD had been prescribed an MDI (100% vs. 98%, respectively) and the majority had been prescribed a Diskus® device (75% vs. 68%, respectively).
Misuse rates for MDI and Diskus® were similarly high (86% and 71%, respectively, p = 0.07). For MDI devices, the majority of patients were unable to perform the following steps: attaching the spacer (step 3, incorrect in 83% of participants), breathing out fully (step 4, incorrect in 77% of participants) and away from the device (step 5, incorrect in 83% of participants). Similar steps were misused by the majority of patients for the Diskus® device: breathing out fully (step 4, incorrect in 77% of participants) and away from the device (step 5, incorrect in 81% of participants). There were no significant differences in the percent of patients with asthma vs. COPD performing any of the MDI steps correctly (p-values: 0.09 to >0.999) or Diskus steps correctly (p-values: 0.35 to >0.999). [Fig. 2]
Figure 2a: MDI. Percentage of participants demonstrating correct inhaler technique for each of the 12 MDI steps. Data for all participants (All), participants with asthma (Asthma), and participants with chronic obstructive pulmonary disease (COPD) are presented above. There were no statistically significant differences in percentage of participants demonstrating correct inhaler technique for any of the steps when comparing patients with asthma to those with COPD. See Table 1 for the description of each MDI step. Figure 2b: Diskus®. Percentage of participants demonstrating correct inhaler technique for each of the 10 Diskus steps. Data for all participants (All), participants with asthma (Asthma), and participants with chronic obstructive pulmonary disease (COPD) are presented above. There were no statistically significant differences in percentage of participants demonstrating correct inhaler technique for any of the steps when comparing patient with asthma to those with COPD. See Table 1 for the description of each Diskus step.
Misuse of inhalers was similarly common in participants with COPD vs. asthma (MDI, 85% vs. 86%, p > 0.99; Diskus®, 81% vs. 65% p = 0.18). Among participants who had been prescribed both a MDI and a Diskus® (n = 69), MDIs were more often misused, although this difference was not statistically significant (83% vs. 71%, p = 0.07).
Participants with insufficient vision were more likely to misuse Diskus® devices compared to those with sufficient vision (95% vs. 61%, p = 0.004). However, differences in inhaler misuse were not significantly different between groups based on vision for MDIs (89% vs. 84%, p = 0.75). Health literacy was not significantly associated with MDI or Diskus® misuse (MDI misuse in patients with less-than-adequate health literacy vs. adequate health literacy: 83% vs. 85%, p = 0.74; Diskus® 63% vs. 61%, p = 0.58).
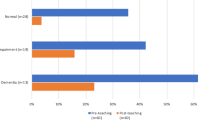
Ability to learn inhaler technique with TTG strategy
Forty-two participants were enrolled after the mid-study analysis, and therefore participated in the TTG intervention. Baseline participant characteristics (age, gender, race, smoking status, level of health literacy, and vision), diagnosis (COPD vs. asthma), and rates of MDI and Diskus® misuse were similar for those who received TTG compared to those enrolled prior to the mid-study analysis (and therefore did not receive TTG; data not shown).
MDI device
After one-round of TTG instruction, 86% (36/42) of participants achieved MDI mastery. There was no difference in ability to learn inhaler technique for patients with asthma compared to those with COPD (87% vs. 84%, p = 0.57), after one-round of TTG. After a second-round of TTG, all participants (42/42, 100%) achieved MDI mastery. Participants with insufficient vision were less-likely to achieve mastery after one-round of TTG compared to those with sufficient vision (58% vs. 97%, p = 0.005). Level of health literacy was not associated with mastery after one-round of teaching (less-than-adequate vs. adequate health literacy: 92% vs. 100%, p = 0.4).
Diskus® device
As with MDIs, the majority of participants (32/41, 78%) achieved mastery after one-round of TTG instruction. Again, there was no difference in ability to learn inhaler technique for patients with asthma compared to those with COPD (74% vs. 83%, p = 0.37) after one-round of TTG. Similar to MDI, after a second-round of TTG, all participants (100%) achieved mastery for the Diskus® device. Additionally, participants with insufficient vision were less-likely to achieve mastery of Diskus® after one-round of TTG compared to those with sufficient vision, though statistical significance was not demonstrated (83% vs. 67%, p = 0.41). While health literacy was also not associated with mastery of Diskus® after one-round of teaching, results approached statistical significance (less-than-adequate vs. adequate health literacy: 64% vs. 94%, p = 0.05).
DISCUSSION
Our study demonstrates that rates of respiratory inhaler misuse are high among hospitalized patients with asthma and COPD. This is interesting since patients with COPD have higher rates of potential risk factors including insufficient vision and less-than-adequate health literacy. Although greater than one-in-four participants had insufficient vision, and these participants were twice-as-likely to misuse Diskus® devices, we also found that all participants, regardless of diagnosis, were able to learn and master both MDI and Diskus® technique.
Our findings extend the results of previous studies mainly done in outpatient and emergency room settings, that found high rates of inhaler misuse (from 32%-100% of patients).9–13,29,30 Further, our study is unique in that it examines the use of respiratory inhalers for both rescue (e.g., MDIs) and controller medications (e.g., MDI and Diskus® devices) in hospitalized patients with asthma or COPD, two of the most common lung conditions, accounting for more than 50 million individuals in the United States.31 Our results suggest that providing hospital-based instruction can overcome barriers to self-management, such as insufficient vision.
One unexpected finding was the high prevalence (more than one–in-four participants) of insufficient vision in our study population. The majority of participants with insufficient vision did not have their corrective-lenses with them in the hospital; the remainder either had corrective-lenses that were not adequate or had not previously been prescribed corrective-lenses. Vision in the range of 20/50 to 20/100 is considered “disabling” in occupations that require work with numbers or extensive reading, thereby making sufficient vision essential to one’s ability to perform certain vocations or tasks.32 Similarly, this concept can be applied to an individual’s ability to manage chronic diseases on a daily basis. For instance, insufficient vision may serve as a barrier to self-management of asthma or COPD, including the use of medications (e.g., respiratory inhalers). For example, one study reported that poor vision is related to the inability of patients to open medication containers.33 Our study demonstrates that insufficient vision is a newly identified barrier to appropriate inhaler use. This finding is not surprising since patient education is heavily weighted with written materials that are not only too complex for patients with lower levels of literacy,12 but may also include font-sizes too small to be legible for patients with insufficient vision.34 For example, font-sizes on package-inserts for MDI and Diskus® devices are well below the size 14-font used with the S-TOFHLA, instrument,35,36 presenting a potential challenge for patients with insufficient vision.
However, insufficient vision does not appear to fully explain inhaler misuse. For instance, although COPD patients had higher rates of insufficient vision, they had similar rates of misuse compared to patients with asthma. Further, while insufficient vision was significantly associated with Diskus® misuse and the inability to learn MDI technique, we did not find significant associations between insufficient vision and MDI misuse, nor did we find significant associations between insufficient vision and ability to learn Diskus® technique. One potential reason is the relatively modest sample size for some of the tests of associations. It is also possible that unmeasured patient confounders such as cognitive status or hearing, among others, play a role in inhaler misuse and ability to learn inhaler technique. There could also be device-specific factors that increase risk for misuse that need to be better evaluated in future studies. These potential unmeasured patient-specific factors may also explain why, even though patients with COPD have higher rates of inadequate health literacy and insufficient vision, patients with asthma are just as likely to misuse inhalers. Larger prospective studies should evaluate the role of insufficient vision, along with other important patient factors, in inhaler misuse and ability to learn inhaler technique.
It was encouraging that the TTG intervention was able to overcome potential barriers, such as insufficient vision, for learning inhaler technique. Our findings suggest that comparative studies to evaluate the relative effectiveness of intensive approaches (e.g., TTG), compared to less-intensive approaches to inhaler instruction, are needed.
Unlike earlier studies, we did not detect an association between health literacy and inhaler misuse.9,12 Although rates of mastery after instruction were larger for patients with less-than-adequate health literacy (compared to adequate health literacy), differences between the groups were not statistically significant. Because we could not measure health literacy for all study participants, we were inadequately powered to detect a statistically significant association between lower-levels of health literacy and inhaler mastery.
Our study has some limitations. Because we enrolled a predominately minority population with frequent exacerbations and hospitalizations, it is not clear if our findings would be generalizable to all hospitalized patients with COPD or asthma. We did not include a control group when evaluating the effectiveness of TTG; thus we cannot provide information about the relative effectiveness of intensive versus less-intensive approaches. TTG employed trained research assistants to provide the intervention, as opposed to clinicians; additional studies are needed to determine whether TTG is effective and feasible when delivered by clinicians. Although TTG was successful at teaching patients while hospitalized, we have no long-term follow-up data from this study to determine its effectiveness post-hospital discharge (retention), or the cost-effectiveness of TTG. Finally, this was a modest-sized study conducted at two urban academic healthcare centers. Larger multi-center studies are need to confirm our findings and more fully examine vision, health literacy, inhaler technique, and ability to learn inhaler technique during transitions in care.
In conclusion, most patients hospitalized with asthma or COPD were unable to use inhalers correctly, and poor vision is a surmountable barrier to inhaler misuse. Comparative effectiveness studies are needed to examine different approaches to assessing and improving inhaler technique in this high-risk population during transitions from hospital to home.
REFERENCES
Kripalani S, Jackson AT, Schnipper JL, Coleman EA. Promoting effective transitions of care at hospital discharge. A review of key issues for hospitalists. J Hosp Med. 2007;2(5):314–23.
Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;140:533–6.
Coleman EA, Smith JD, Frank JC, Min S-J, Ca P, Kramer AM. Preparing patients and caregivers to participate in care delivery across settings: the care transitions intervention. J Am Geriatr Soc. 2004;52:1817–25.
Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication Use Among Inner-City Patients After Hospital Discharge: Patient-Reported Barriers and Solutions. Mayo Clin Proc. 2008;83(5):529–35.
Coleman EA, Smith JD, Raha D, Min S-J. Posthospital medication discrepancies: prevalence and contributing factors. Arch Intern Med. 2005;165:1842–7.
Rydman RJ, Sonenthal K, Tadimeti L, Butki N, McDermott MF. Evaluating the outcome of two teaching methods of breath actuated inhaler in an inner city asthma clinic. Jrnl of Med Syst. 1999;23(5):349–56.
Celli BR, MacNee W and Committee Members. Standards for the diagnosis and treatment of patients with COPD: A Summary of the ATS/ERS Position Paper. Eur Respir J. 2004;23:932–46.
Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy. Evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127:335-71.
Paasche-Orlow MK, Riekert KA, Bilderback A, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6.
Thompson J, Irvine T, Grathwohl K, Roth B. Misuse of metered-dose inhalers in hospitalized patients. Chest. 1994;105:715–7.
van der Palen J, Klein JJ, van Herwaarden CLA, Zielhuis GA, Seydel ER. Multiple inhalers confuse asthma patients. Eur Respir J. 1999;14:1034–7.
Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114:1008–15.
Dahl R, Backer V, Ollgaard B, Gerken F, Kesten S. Assessment of patient performance of the Handihaler® compared with the metered dose inhaler four weeks after instruction. Respir Med. 2003;97:1126–33.
Apter AJ, Tor M, Feldman H. Testing the Reliability of Old and New Features of a New Electronic Monitor for Metered Dose Inhalers. Ann Allergy Asthma Immunol. 2001;86(4):421–4.
Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids: socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157:1810–7.
Melani AS. Inhalatory therapy training: a priority challenge for the physicians. Acta Biomed. 2007;78:233–45.
Guidelines for the diagnosis and management of asthma (EPR-3). Available at: http://www.nhlbi.nih.gov/guidelines/asthma/. Accessed December 15, 2010.
The global initiative for chronic obstructive lung disease (GOLD) guidelines: Available at: http://www.goldcopd.com/. Accessed December 15, 2010.
Thai AL, George M. The effects of health literacy on asthma self-management. J Asthma Allergy Educ. 2010;1(2):50–55.
Effing T, Monninkhof EEM, van der Valk PP, Zielhuis GGA, Walters EH, van der Palen JJ, Zwerink M. Self-management Education for Patients with Chronic Obstructive Pulmonary Disease (Review). The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. Available at http://www2.cochrane.org/reviews/en/ab002990.html. Accessed December 15, 2010.
Nikolaus T, Kruse W, Bach M, Specht-Leible N, Oster P, Schlierf G. Elderly patients’ problems with medication: an in hospital and follow-up study. Eur J Clin Pharmacol. 1996;49:255–9.
Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167(14):1502–9.
Duerden M, Price D. Training issues in the use of inhalers. Dis Manage Health Outcomes. 2001;9(2):75–87.
Hanania NA, Darken P, Horstman D, et al. The efficacy and safety of fluticasone propionate (250 ug)/salmeterol (50ug) combined in the diskus inhaler for the treatment of COPD. Chest. 2003;124:834–43.
Celli BR, Thomas NE, Anderson JA, et al. Effect of pharmacotherapy on rate of decline of lung function in chronic obstructive pulmonary disease. Results from the TORCH study. Am J Respir Crit Care Med. 2008;178:332–8.
Nurss JR, Parker RM, Williams MV, Baker, DW. Short Test of Functional Health Literacy in Adults (STOFHLA). Hartford: Peppercorn Books & Press; 2001.
Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42.
Wu HW, Nishimi RY, Page-Loez CM, Kizer KW. Improving patient safety through informed consent for patients with limited health literacy. An implementation report. National Quality Forum. 2005. Available at: http://www.qualityforum.org/Publications/2005/09/Improving_Patient_Safety_Through_Informed_Consent_for_Patients_with_Limited_Health_Literacy.aspx. Accessed December 15, 2010.
Van der Palen J, Klein JJ, Kerkhoff AHM, van Herwaarden CLA, Seydel ER. Evaluation of the long-term effectiveness of three instruction modes for inhaling medicines. Patient Educ Couns. 1997;32:S87–S95.
Shrestha M, Parupia MFH, Andrews B, et al. Metered-dose inhaler technique of patients in an urban ED: prevalence of incorrect technique and attempt at education. Am J of Emerg Med. 1996;14(4):380–4.
Morbidity and Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Disease. National Institutes of Health National Heart, Lung and Blood Institute. October 2009. Available at: http://www.nhlbi.nih.gov/resources/docs/2009_ChartBook.pdf. Accessed December 15, 2010.
University of Illinois Eye & Ear Infirmary, Chicago, IL. The eye digest. Available at: http://www.agingeye.net/visionbasics/healthyvision.php. Accessed December 15, 2010.
Beckman A, Bernstein C, Parker MG, Thorslund M.Fastbom J. The difficulty of openingmedicines containers in old age: a population based study. Pharm World Sci. 2005;27:393–8.
Fuchs J, Hippius M. Inappropriate dosage instructions in package inserts. Patient Educ Couns. 2007;67:157–68.
Ventolin HFA® Package Insert. Available at: http://us.gsk.com/products/assets/us_ventolin_hfa.pdf. Accessed December 15, 2010.
Advair Diskus® Package Insert. Available at: http://us.gsk.com/products/assets/us_advair.pdf. Accessed December 15, 2010.
Acknowledgements
Contributors
We would like to thank The University of Chicago Asthma and COPD Center and the Department of Medicine Data Management and Statistics Core.
Prior Presentations: Prior poster presentations include the 2009 American Thoracic Society International Meeting in San Diego, the 2009 Society of Hospital Medicine Annual meeting in Chicago IL, and the 2009 and 2010 Society of General Internal Medicine Annual Meetings in Miami, Fl and Minneapolis, MN, respectively. Oral presentations include the 2009 Midwest Society of General Internal Medicine and the 2010 American Thoracic Society International Meeting in New Orleans, LA.
Conflict of Interest
Dr. Press reports receiving funding from the Institute for Translational Medicine, University of Chicago CTSA from the National Center for Research Resources (UL1RR024999) and the American Cancer Society (PSB 08-08). Dr. Arora reports receiving funding from the American Board of Internal Medicine, Agency for Healthcare Research and Quality (R03HS018278), the National Institute of Aging (K23AG033763), and the Accreditation Council of Graduate Medical Education. Dr. Krishnan reports receiving funding from the National Institutes of Health (HL101618) and the Agency for Healthcare Research and Quality (HS016967). Potential conflicts of interest exist for Dr. Shah who is employed with a for profit health care policy firm (Avalere Health, LLC); for Dr. Badlani who has received honoraria for lectures given (Merck Pharmaceuticals and PharmEd Consultants); and for Dr. Naurekas, who has provided expert testimony (once for a plaintiff on Alveolar Hemosiderosis and once for Cook County on thrombotic thrombocytopenic purpura). All other authors do not have any conflicts of interest to disclose related to employment, consultancies, honoraria, stock, expert testimony, patents, royalties or any other relationships.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s11606-011-1671-3
Rights and permissions
About this article
Cite this article
Press, V.G., Arora, V.M., Shah, L.M. et al. Misuse of Respiratory Inhalers in Hospitalized Patients with Asthma or COPD. J GEN INTERN MED 26, 635–642 (2011). https://doi.org/10.1007/s11606-010-1624-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1624-2