Abstract
OBJECTIVE
To examine the change in women’s self-reported physical symptoms over 2 time points in relation to intimate partner violence (IPV) exposure.
DESIGN
Prospective interview study of 267 women recruited from 8 health care settings and surrounding communities in Metropolitan Boston.
METHODS
We created sums of somatic symptoms at 2 separate time points (a mean of 9.5 months apart) using items from a modified PHQ-15. A measure of symptom change was computed to measure the net change in symptoms over time. A negative score indicated reduction in total symptoms, or improvement. Exposure to IPV was measured at both time points.
RESULTS
Women who reported ongoing IPV across both time points experienced an increase in their overall physical symptoms compared to women with past abuse (p = .0054) and no abuse (p = .0006). In multivariate regression analysis, ongoing IPV at both time points was a statistically significant predictor of symptom change. This relationship persisted even after controlling for age, race, education, depression, self-report of co-morbid illness, and history of child abuse and prior sexual assault (p = .0076).
CONCLUSIONS
Women exposed to ongoing IPV report increased physical symptoms over time. Clinicians should consider the possibility of IPV in patients who remain persistently symptomatic over time in addition to employing more traditional means of detecting IPV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
BACKGROUND AND SIGNIFICANCE
Intimate partner violence (IPV) affects nearly one-quarter of American women during their lifetime,1 and is known to cause adverse mental and physical health states,2–4 increased health care utilization and costs,5–8 and, at its extreme, mortality.9 The Centers for Disease Control and Prevention (CDC) defines intimate partner violence (IPV) as “physical, sexual, or psychological harm by a current or former partner or spouse.”10
A symptom is defined as subjective evidence of disease or physical disturbance observed by the patient. Symptoms are often the catalyst for patients to seek medical care. Highly symptomatic patients tend to utilize more medical care11 and present a challenge to clinicians.12,13 Different forms of abuse are all associated with increases in common somatic symptoms such as headaches, abdominal pain, and pelvic pain.14–22 Physical,3,14–16,18–20,22,23 sexual,3,14–16,22–24 and emotional abuse3,14,21 in adulthood, and abuse in childhood3,19,23,25–27 have all been linked to increased symptom reporting. Physical symptoms appear to increase in a dose–response fashion with severity18,19 or recency3 of abuse.
Prior work in this area has used either cross-sectional or retrospective designs, limiting our knowledge of how physical symptoms might change over time with varying exposure to abuse. Researchers have yet to investigate abused women’s physical symptoms prospectively. The aim of the present study is to describe the change in symptoms reported by women over time and to determine whether IPV exposure is associated with that change. The longitudinal design of our study allows us to explore whether women who are abused and symptomatic continue to have physical symptoms after violence remits, or whether such symptoms diminish in the wake of past violence. Understanding whether patients who exhibit a high burden of symptoms over time are more likely to have experienced IPV could assist physicians in properly treating and referring these patients.
METHODS
The study is based on 2 longitudinal interviews with women recruited from a larger cohort study, which was designed to characterize the health of abused women. In-person and telephone interviews were conducted with 274 women over 2 time points (88.7% retention rate). A volunteer sample was drawn from the initial cohort of 2,465 women who were surveyed in waiting rooms across 8 different health care settings in departments of Internal Medicine, Obstetrics and Gynecology, Emergency, Pediatrics, and Addiction Recovery. The human subjects committees of the participating institutions approved the study.
These women completed a brief written survey and were invited to participate in future interviews. The methods and results of this initial phase of the study are reported elsewhere.28,29 Volunteers were also recruited through posters displayed in public places and health care sites in the Greater Boston area. Initial interviews (Time 1) took place at a secure research facility with trained interviewers in 2003–2004; a subsequent phone interview (Time 2) was conducted an average of 9.5 months later (range 69–782 days). Interviews contained the same questions at both time points about IPV, physical symptoms, and overall health. Questions about demographics (age, race, education), housing, and employment status were also included.
Measurement of Intimate Partner Violence
Women were queried about IPV using 6 items from the Conflict Tactics Scale30 at both time points.
“In the past year how often did a partner
-
1.
push or shove you?
-
2.
slap you?
-
3.
do anything else that physically threatened or hurt you?”
-
4.
Use force (like hitting, holding down, or using a weapon) to make you have sexual intercourse?
-
5.
Use a gun on you?
-
6.
Punch or hit you with something that could hurt?
Any indication of physical abuse was coded as IPV in the past 12 months. Responses were used to create four dummy-coded variables reflecting violence exposure across the 2 interview time points: a) no abuse at either time point; b) abuse at Time 1 but none at Time 2; c) no abuse at Time 1 but abuse at Time 2; and d) abuse at both time points.
During the in-person interview (Time 1), we measured emotional IPV using the Women’s Experiences of Battering (WEB) Scale.31 Additional forms of abuse (childhood abuse and sexual assault) known to be associated with physical symptoms were also included in the first interview. Childhood trauma was assessed using 4 questions from 4 different scales (physical abuse, emotional abuse, emotional neglect, and sexual abuse) of the Childhood Trauma Questionnaire.32 One single question was used to assess unwanted sexual experiences: “At any point during your life has a man (excluding your current partner) forced you to have sexual intercourse when you did not want to by using some degree of physical force like twisting your arm or holding you down?”33
Symptom Inventory
Participants were queried about 11 physical symptoms in the preceding 2 weeks that correspond to a modified version of the PHQ-15.34 Response categories were yes/no. The symptoms included were:
-
1.
Back pain
-
2.
Headaches
-
3.
Pain in hands/feet
-
4.
Fainting
-
5.
Feeling numb or paralyzed
-
6.
Diarrhea
-
7.
Stomach pain or nausea
-
8.
Vomiting
-
9.
Pain during intercourse
-
10.
Excessive menstrual bleeding
-
11.
Fatigue
A symptom count was created for each time point by summing affirmative responses (no = 0, 1 = yes) across the 11 items. A measure of symptom change across time points was constructed by subtracting the symptom count at Time 2 from the count at Time 1; a negative number indicates improvement or reduction in symptoms. If a woman becomes less symptomatic over time, her total score should go down by Time 2, conversely, a positive score indicates net worsening in the burden of symptoms over time.
Measurement of Comorbid Disease and Health Status
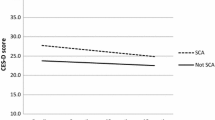
Because symptoms are often associated with a range of underlying health conditions, we measured comorbidities with a number of different measures. At Time 1, women completed the SF-12 assessing overall health35 and the CES-D to measure depression.36
Women were asked whether they had ever been diagnosed with any of the following 10 conditions: Asthma, Diabetes, Cardiovascular Disease and Hypertension, Arthritis, Cancer, HIV, autoimmune disorders (e.g., thyroid, arthritis), hepatitis, and neurological disease (including multiple sclerosis and seizure disorders). Medical diagnoses were combined into a disease count by summing the “yes” responses for each diagnosis.
We also asked participants about their history of gynecological and reproductive health conditions. The conditions queried were: endometriosis, ovarian cyst, uterine fibroids, gonorrhea, chlamydia, syphilis, genital warts, genital herpes, pelvic inflammatory disease, vaginal infections (vaginitis), and urinary tract infections. The reproductive health conditions were similarly summed and combined into a separate count to model the burden of illness from gynecologic and reproductive health conditions.
At Time 2, participants were asked “Since your last interview (date) has a doctor or medical provider told you that you had any chronic illness or provided you with a diagnosis?” The response categories were yes/no and women who answered affirmatively were asked what the diagnosis was. This same question format was used for self-report of new gynecologic diagnoses. We created variables for these new medical and gynecological diagnoses, respectively, and examined these as covariates in our model.
The relationship between health status as measured by the SF-12 and our symptom count measure (the modified PHQ-15) was examined using a Pearson correlation to establish construct validity as the original PHQ-15 was shown to be inversely correlated with the SF-20 when it was developed.34 The CES-D36 was administered to measure depression at Time 1 (using the recommended cutoff point of 16 to indicate current depression). Potentially hazardous alcohol use was measured with 1 question from the AUDIT: “(During the past 30 days) How often do you have 4 or more drinks on one occasion?”37 at both time points. The AUDIT is designed to detect hazardous drinking behavior. For women, concern for harmful drinking occurs at consumption levels of more than 3 drinks per occasion or more than 7 drinks in a week.38 We categorized women who answered “never” or “less than monthly” as nondrinkers or moderate drinkers and those who answered “monthly,” “weekly,” or “daily” as potentially problem drinkers in keeping with prior study definitions.29
Statistical Analysis
Initially, summary and descriptive statistics were performed on the data set. Unadjusted regressions were performed to test the relationship of the independent variables (IPV, emotional abuse at Time 1, child abuse, lifetime sexual assault, race, educational status, recruitment method, problem drinking, medical and gynecologic comorbidity at baseline and new onset by Time 2) to symptom change.
Because different forms of abuse may be interrelated, we performed Pearson correlations to test the level of association between different forms of abuse (IPV, child abuse, emotional abuse) before entering these into a multivariate model together. We checked for collinearity using the variance inflation factor and tolerance methods. None of the variables met any of the criteria for collinearity.
We then estimated predictors of symptom change over time by constructing a multivariate linear regression model. We entered basic demographic variables: age, race (white as reference), and educational status (college education as reference) into the model to control for potential confounding. Time between interviews was put in the model to adjust for any potential differences in time elapsed between interviews. Also retained in the model were variables for which there is strong evidence linking them to physical symptoms (IPV, sexual assault, child abuse, and depression). Emotional abuse was not kept in the final model because of a strong correlation with the IPV variables (Pearson correlation >0.4). Finally, covariates that were significant on bivariate analysis were also included in the final model. All analyses were conducted using SAS (Version 9.1 Cary, NC).
RESULTS
After both interviews, 103 participants (39%) reported IPV at 1 or both time points (Table 1). At Time 2, 274 (88.6%) women remained in the study; however, 3 participants’ data were omitted from subsequent analyses because violence status at this time point was missing and could not be reliably imputed. This reduced the sample size to 271. Four who reported no IPV at Time 1 newly reported it at Time 2. Exclusion of these 4 women from the model did not significantly alter the coefficients, so these 4 participants were excluded from subsequent analyses, resulting in a final sample size of 267 with data at both time points.
Demographic characteristics are shown in Table 1. Participants were mostly non-white with a high prevalence of depression and unemployment. By Time 2, only 31 (12%) women reported ongoing abuse. Symptoms at each time point were inversely correlated with both the mental (MCS) and physical component summaries (PCS) of the SF-12 computed from our data (Pearson correlations: MCS = −.41, PCS = −.46), suggesting that our modified PHQ-15 has construct validity as a symptom measure. As a result of this correlation, SF-12 scores were not retained in subsequent analyses.
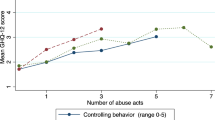
Symptom Change Over Time by Abuse Status
Women who reported IPV at both time points demonstrated an increase in symptoms over time. They also had the highest total symptoms of the 3 groups at Time 2. Women with IPV only at Time 1 showed a decline in symptoms over time, and women who had never been abused had the lowest burden of symptoms, which also trended downward over time (Fig. 1). We found a gradient of symptom change from never abused (−.439, p = .04, 2-sided T test) to abuse at Time 1 only (−.278, p = .821, 2-sided T test) to abuse at both time points (1.00, p = .007, 2-sided T test).
Symptom Change by Recruitment Method
Participants recruited through community posters had a mean symptom change of 0.37, suggesting worsening over time, whereas women recruited in waiting rooms had a lower mean symptom score of −0.39, p = .019 (2-sample T test).
Estimation of Symptom Change Over Time
In bivariate regression analyses, IPV at both time points was associated with symptom change as was the method of recruitment, hazardous alcohol use, and employment status (Table 2). Medical and gynecological comorbidity at baseline or Time 2 were not significant on bivariate analysis and did not significantly alter the coefficients when they were added back into the model, so the new onset covariates were kept out of the final model.
Because child abuse and prior sexual assault are known to be strongly associated with somatic symptoms but not associated with our measure of net symptom change, we examined the association between these variables and the cross-sectional symptom sums at the 2 separate time points (2-sided T test). Both child abuse and lifetime sexual assault were associated with the absolute number of symptoms at Time 1 and Time 2.
In the final adjusted regression model, a woman’s report of continued IPV at Time 1 and Time 2 remained associated with symptom change. Even with adjustment for confounding and control for other factors known to be related to somatic symptoms, the coefficient remains positive suggesting increased symptoms over time for women who report abuse at both time points. Hazardous drinking and working part-time also remained associated with symptom change over time (Table 2).
DISCUSSION
Women exposed to IPV over time experience more physical symptoms prospectively than do never abused women or women who have experienced an abuse-free interval. This relationship persists when controlling for additional forms of abuse and for comorbid medical diagnoses. Women who report hazardous alcohol consumption and less than full-time employment also report a higher burden of symptoms. Our results confirm those of prior studies that have found increased physical symptoms among women who have experienced IPV and other forms of abuse, but adds the dimension of examining this association longitudinally. Our results also suggest an effect gradient from no IPV to past experience of IPV to ongoing IPV similar to the reduction of adverse health effects from withdrawing other harmful exposures like smoking.39 Although child abuse and sexual abuse are known to be associated with physical symptoms, the magnitude of the effect is less than that of ongoing IPV. Past studies have tended not to adjust for comorbid illness, so our results are robust even in the presence of other reported medical conditions.
The study has a number of important limitations. As with any convenience sample, selection bias is a concern. Our use of two different methods of recruitment added depth to our sample, but may have introduced additional selection bias. Women recruited through posters appeared to have more housing and economic problems compared with the women recruited in waiting rooms; however, 96% (55/57) of the women recruited through posters report a usual source of medical care. Only 4 reported obtaining that care in emergency departments; the remainder reported attending non-emergency department settings, such as hospital-based clinics. We believe that these women comprise an important subset of patients presenting to urban medical settings and have equal access to health care in the state in which we conducted our study. Where possible, we have controlled for socioeconomic variables that may affect symptom reporting in our sample.
Another limitation of this study is the loss to follow-up between interviews. It appears that women exposed to IPV at Time 1 and women recruited via posters constituted a majority of those lost to follow-up after Time 1. This suggests that the remaining cohort at Time 2 was potentially healthier. This may have biased our findings toward the null because the women who were sicker and less likely to experience an improvement in symptoms were no longer in the study by Time 2 and could not have a net symptom score computed. Thus, our finding that symptoms are increased in women experiencing ongoing abuse may have been attenuated by this differential loss to follow-up.
Another potential limitation is that the analyses do not take into account whether the reported IPV was perpetrated by the same or a new partner. It is unclear whether IPV inflicted in a new relationship has the same impact on self-reported health as IPV inflicted within a long-standing one. Another potential concern is matching the exact timing of incidents of abuse with particular emergence or remission of symptoms. Although our study is prospective, the time frame for abuse is broad (past 12 months) and that of symptoms is more narrow (last 2 weeks). The degree to which abuse is temporally concomitant with a woman’s experience of symptoms cannot be determined in the present study. The context of violence in relationships, however, may make such precise timing—as is reported in diary studies—difficult to ascertain.
We did not use the actual PHQ-15, therefore the responses and time frame are different than those of the validated instrument. The finding that our measure of symptoms is inversely correlated with SF-12 scores at baseline lends validity to the assumption that our modified instrument functions similarly to the original. The use of a composite symptom score does not take into account the value an individual patient (or clinician) may place on the improvement of 1 set of symptoms over another.
It is noteworthy that whereas child abuse and adult lifetime sexual abuse are associated with symptoms at baseline, they do not appear to influence net symptom change. This finding is consistent with our results that suggest that it is recency of abuse exposure that most impacts change in symptoms.
CONCLUSION
Abused women have an overall higher burden of physical symptoms than do women who have not experienced abuse. As an adjunct to routine inquiry and case finding in clinical settings, clinicians who follow patients longitudinally should be attuned to continued reporting of multiple physical symptoms as a marker for ongoing IPV. It may remain easier for a patient to talk about her somatic symptoms than to directly disclose ongoing abuse. In prior work, we found that physicians’ discussion of IPV with patients is associated with receipt of interventions for IPV and improved overall health.40 This makes it incumbent upon clinicians to inquire about IPV when faced with clinical presentations suggestive of IPV, such as increasing physical symptoms. Future study could examine symptom change over longer periods of time and also query which medical interventions are useful to reduce the burden of physical symptoms in patients with past or ongoing abuse.
References
Extent, nature, and consequences of intimate partner violence: findings from the National Violence Against Women Survey. Washington (DC): Department of Justice (US); 2000. http://www.ncjrs.gov/txtfiles1/nij/181867.txt. Updated Last Updated Date. Accessed 2/28/2007
Coker A, Davis K, Arias I, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002;23:260–8.
McNutt L, Carlson B, Persaud M, Postmus J. Cumulative abuse experiences, physical health and health behaviors. Ann Epidemiol. 2002;12:123–30.
Campbell J, Jones A, Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Int Med. 2002;162:1157–63.
Coker A, Reeder C, Fadden M, Smith P. Physical partner violence and Medicaid utilization and expenditures. Public Health Rep. 2004;119:557–67.
Rivara FP, Anderson ML, Fishman P, et al. Healthcare utilization and costs for women with a history of intimate partner violence. Am J Prev Med. 2007;32(2):89–96.
Ulrich YC, Cain KC, Sugg NK, Rivara FP, Rubanowice DM, Thompson RS. Medical care utilization patterns in women with diagnosed domestic violence. Am J Prev Med. 2003;24(1):9–15.
Wisner CL, Gilmer TP, Saltzman LE, Zink TM. Intimate partner violence against women: do victims cost health plans more? J Fam Pract. 1999;48(6):439–43.
Campbell JC, Webster D, Koziol-McLain J, et al. Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health. 2003;93(7):1089–97.
Centers for Disease Control. http://www.cdc.gov/ncipc/dvp/IPV/ipv-definitions.htm. Accessed 11/7/2007.
Sha MC, Callahan CM, Counsell SR, Westmoreland GR, Stump TE, Kroenke K. Physical symptoms as a predictor of health care use and mortality among older adults. Am J Med. 2005;118(3):301–6.
Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159(10):1069–75.
Hahn SR. Physical symptoms and physician-experienced difficulty in the physician–patient relationship. Ann Intern Med. May 1 2001;134(9 Pt 2):897–904.
Bonomi AE, Thompson RS, Anderson M, et al. Intimate partner violence and women’s physical, mental, and social functioning. Am J Prev Med. 2006;30(6):458–66.
Kovac SH, Klapow JC, Kroenke K, Spitzer RL, Williams JB. Differing symptoms of abused versus nonabused women in obstetric-gynecology settings. Am J Obstet Gynecol. 2003;188(3):707–13.
Lown EA, Vega WA. Intimate partner violence and health: self-assessed health, chronic health, and somatic symptoms among Mexican American women. Psychosom Med. 2001;63(3):352–60.
McCauley J, Kern DE, Kolodner K, et al. The “battering syndrome”: prevalence and clinical characteristics of domestic violence in primary care internal medicine practices. Ann Intern Med. 15 1995;123(10):737–46.
McCauley J, Kern DE, Kolodner K, Derogatis LR, Bass EB. Relation of low-severity violence to women’s health. J Gen Intern Med. 1998;13(10):687–91.
Nicolaidis C, Curry M, McFarland B, Gerrity M. Violence, mental health, and physical symptoms in an academic internal medicine practice. J Gen Intern Med. 2004;19(8):819–27.
Porcerelli JH, Cogan R, West PP, et al. Violent victimization of women and men: physical and psychiatric symptoms. J Am Board Fam Pract. 2003; 16(1):32–9.
Porcerelli JH, West PA, Binienda J, Cogan R. Physical and psychological symptoms in emotionally abused and non-abused women. J Am Board Fam Med. 2006;19(2):201–4.
Samelius L, Wijma B, Wingren G, Wijma K. Somatization in abused women. J Women’s Health. 2007;16(6):909–18.
Krantz G, Ostergren PO. The association between violence victimisation and common symptoms in Swedish women. J Epidemiol Community Health. 2000;54(11):815–21.
Golding JM. Sexual assault history and physical health in randomly selected Los Angeles women. Health Psychol. 1994;13(2):130–8.
Morse DS, Suchman AL, Frankel RM. The meaning of symptoms in 10 women with somatization disorder and a history of childhood abuse. Arch Fam Med. 1997;6(5):468–76.
Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl. 2003;27(11):1247–58.
Walker EA, Gelfand A, Katon WJ, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999;107(4):332–9.
McCloskey LA, Lichter E, Ganz ML, et al. Intimate partner violence and patient screening across medical specialties. Acad Emerg Med. 2005;12(8):712–22.
Gerber MR, Ganz ML, Lichter E, Williams CM, McCloskey LA. Adverse health behaviors and the detection of partner violence by clinicians. Arch Intern Med. 2005;165(9):1016–21.
Straus M, Hamby S, Boney-McCoy S, Sugarman D. The revised conflict tactics scales (CTS2): development and preliminary psychometric data. J Fam Issues. 1996;17:283–316.
Smith PH, Earp JA, DeVellis R. Measuring battering: development of the Women’s Experience with Battering (WEB) Scale. Women’s Health. 1995;1(4):273–88.
Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–36.
Koss MP, Oros CJ. Sexual Experiences Survey: a research instrument investigating sexual aggression and victimization. J Consult Clin Psychol. 1982;50(3):455–57.
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66.
Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56(4):423–32.
Fiellin DA, Reid MC, O’Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med. 2000;160(13):1977–89.
Ebbert JO, Yang P, Vachon CM, et al. Lung cancer risk reduction after smoking cessation: observations from a prospective cohort of women. J Clin Oncol. 2003;21(5):921–26.
McCloskey LA, Lichter E, Williams C, Gerber M, Wittenberg E, Ganz M. Assessing intimate partner violence in health care settings leads to women’s receipt of interventions and improved health. Public Health Rep. 2006;121(4):435–44.
Acknowledgments
The authors would like to thank the following for their assistance: Erika Lichter, ScD, University of Southern Maine; Jane Liebschutz, MD, MPH, Boston University, Michael Law, MSc, Department of Ambulatory Care and Prevention, Harvard Medical School, and William R. Bachman, MD.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented in abstract form at the UNH International Family Violence Conference, July 2006, Portsmouth, NH. It was supported by a grant from the Agency for Healthcare Research and Quality, Rockville, MD.
Rights and permissions
About this article
Cite this article
Gerber, M.R., Wittenberg, E., Ganz, M.L. et al. Intimate Partner Violence Exposure and Change in Women’s Physical Symptoms Over Time. J GEN INTERN MED 23, 64–69 (2008). https://doi.org/10.1007/s11606-007-0463-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0463-2