Abstract
Objectives
To examine the role of abuse severity in predicting women’s trajectories in mental and physical health and psychological quality of life during the 18 months following abuse identification in a health care setting.
Methods
The present analysis used growth curve modeling in a sample of 411 women positive for abuse on the Composite Abuse Scale.
Results
A high proportion of women experienced severe combined abuse (SCA; 55 % at baseline and 29 % at 18 months). On average, there was an improvement in depressive symptoms and psychological quality of life over time. Controlling for sociodemographic characteristics, women scoring positive versus negative for SCA experienced increased depressive symptoms and decreased quality of life; however, exposure to severe abuse did not affect the rate of change over time in these outcomes. Severe abuse was not associated with physical health.
Conclusions
There is an important association between abuse severity and women’s health and well-being over time. Understanding the role of different abuse experiences, risk and protective factors, and trajectories can assist in more accurate identification and appropriate care provision for women exposed to IPV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intimate partner violence (IPV) is defined by the World Health Organization as “behaviour by an intimate partner or ex-partner that causes physical, sexual or psychological harm, including physical aggression, sexual coercion, psychological abuse and controlling behaviours” (World Health Organization 2010). In Canada past 5-year IPV against women is estimated at 4 % (Statistics Canada 2016), and lifetime IPV at 30 % (Rodgers 1994); self and official reports underestimate IPV, and rates will vary according to where and how women are asked (e.g., rates in health settings are generally higher). Women are four times more likely to be victims of intimate partner homicide than are men (Miladinovic and Mulligan 2015).
Women exposed to IPV suffer from significant physical and mental health problems, and reduced life quality compared to women in the general population (Afifi et al. 2009; Campbell 2002; Coker et al. 2002; Hegarty et al. 2004; Rees et al. 2011; Ellsberg et al. 2008). However, this substantial body of evidence is largely based on cross-sectional studies (e.g., Campbell and Soeken 1999). Emerging longitudinal research has begun to show that the mental health of women who have experienced IPV, recruited primarily through shelters or domestic violence services (which likely differ from “general population” samples), generally improves over time, with the greatest improvements noted after the cessation of violence (Anderson et al. 2003; Beeble et al. 2009; Campbell et al. 1995; Gerber et al. 2008). Some studies indicate that more severe and/or frequent abuse is associated with higher re-victimization rates, more serious injury, and poorer mental, and possibly physical health (Garcia-Moreno et al. 2005; Campbell 2002; Coker et al. 2002; Golding 1999). However, substantial gaps remain in understanding trajectories of women’s health over time, and whether severity of IPV (and not simply exposure), and other contextual and abuse-specific factors, including the cumulative effects of violence across the lifespan (MacIntosh et al. 2015; Davies et al. 2015), affect women’s mental and physical health and quality of life over time.
Using data from a randomized controlled trial (RCT) (MacMillan et al. 2009), this secondary-analysis study examines how the health trajectories of abused women change over time and in particular how one key factor—abuse severity—influences these trajectories. We used growth curve modeling to address the following questions: (1) (how) do the physical health, depressive symptoms, and quality of life of women who have disclosed past-year IPV change over an 18-month period? (2) What is the role of abuse severity in predicting these outcome trajectories? (3) (how) is abuse severity associated with the rate of change in outcome trajectories over time? (4) Do any effects of abuse severity remain after adjusting for key demographic variables? and (5) (how) are key demographic variables associated with women’s outcome trajectories?
Methods
Design and participants
Between July 2005 and December 2006, 6743 English-speaking female patients (ages 18–64) from 26 primary health care settings, including family medicine practices, women’s health clinics, and emergency departments in Ontario, Canada were recruited for a cluster randomized controlled trial evaluating the effectiveness of universal IPV screening (MacMillan et al. 2009). All women who presented to a study site were approached by a study recruiter to determine eligibility. The current research involves the subset of 411 women who were positive for IPV exposure during the previous 12 months according to both the screening instrument (Woman Abuse Screening Tool (WAST); Brown et al. 2000), and the validated abuse measure [Composite Abuse Scale (CAS), Hegarty et al. 1999, 2005] at time of enrolment in the trial, and who consented to participate. All women completed both instruments—the screened group prior to the clinical visit with the results reported on their chart to the health care provider, and the control group as part of their exit interview—i.e., not reported to the health care provider. Women provided sociodemographic information at time of enrolment and completed a questionnaire package containing key predictor and outcome measures, including standardized instruments on depressive symptoms, quality of life, and global physical health at baseline (i.e., within 2 weeks of trial enrolment), and at 6, 12, and 18 months. Further methodological details can be found in MacMillan et al. (2009).
Measures
Our analysis involves three types of variables: (1) time-invariant predictors (i.e., demographics: age, education, minority status, born outside Canada); (2) time-varying predictors [ongoing IPV (re-) exposure; demographics: marital status, number of children at home, current pregnancy, employment, income, rural residence]; and, (3) time-varying primary outcome variables (depressive symptoms, quality of life, and physical health).
IPV (re) exposure
The Composite Abuse Scale (CAS; Hegarty et al. 2005) is a 30-item validated self-report tool with four subscales measuring the frequency with which participants’ partners engaged in a variety of abusive behaviours. Sample items include “[My partner]… slapped me”; “…kept me from medical care”; “…harassed me over the telephone”; and “…told me I wasn’t good enough”. It comprises four subscales that reflect various acts of physical and sexual abuse, emotional abuse, and harassment (Hegarty et al. 2005), and uses a response scale ranging from 0 (never) to 5 (daily). Items were summed, and based on recommended scoring, a score of 7 or higher was used as the criterion for IPV exposure (MacMillan et al. 2009). At time of enrollment, the reference period was the previous 12 months; subsequent time points used a reference point of the previous 6 months (i.e., since last completion of the instrument for the study). The Cronbach alpha (α) in this sample is .92.
IPV severity
In this study, all women at baseline, by definition, had experienced some form(s) of partner abuse within the last 12 months, as determined by the CAS. The most severe forms of violence are captured in the 8-item severe combined abuse (SCA) subscale, and this was used to measure IPV severity. In accordance with the scoring recommendation of Hegarty et al. (2005), SCA was scored dichotomously such that women who reported at least one episode of SCA (e.g., “[My partner] …used a knife or gun or other weapon”) scored positively for SCA. For the purpose of our analyses, we grouped women’s abuse status into two categories: “no SCA” (i.e., not scoring positive for SCA at a specific time-point), and “SCA” (scoring positive for SCA). [Note: while all women included in the analysis were positive for past 12-month IPV at baseline, some women may have had CAS scores at subsequent follow-up point(s) that were below the CAS-positive cut-point of 7. These women were still included in the analysis, and categorized as “no SCA” for analytical purposes].
Depressive symptoms
Depressive symptoms were assessed using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977), which uses a 4-point scale on which respondents indicate the number of times during the past week that a symptom has been experienced (0 = not at all, 1 = occasionally, 2 = frequently, 3 = almost all the time). Sample items include “I felt sad” and “I could not get ‘going’”. Scores range from 0 to 60, with high scores indicating greater depressive symptoms (α = .92 in this sample).
Psychological quality of life
The 6-item psychological subscale from the World Health Organization Quality of Life (WHOQOL)-Brief instrument was used to measure psychological quality of life (Bonomi et al. 2000; WHOQOL Group 1998). The six domains covered by these items are: bodily image and appearance; negative feelings; positive feelings; self-esteem; spirituality, religion, personal beliefs; and thinking, learning, memory and concentration. Using 5-point scales, participants responded to items such as “How often do you have negative feelings such as blue mood, despair, anxiety, depression?” (1 = never, 3 = quite often, 5 = always) and “How satisfied are you with yourself?” (1 = very dissatisfied, 5 = very satisfied). After score transformation, scores range from 0 to 100, with high scores indicating greater quality (α = .79 in this sample).
Physical health
The Short-Form 12 Health Survey, version 2 (SF-12 v2; SF-36.org online; Ware et al. 2002), a valid and reliable brief version of the Short-Form 36, measures functional health and well-being. The SF-12 v2 has 12 questions covering eight health domains: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health. A sample item is “During the past 4 weeks, how much did pain interfere with your normal work (including both work outside the home and housework)?” Responses are made on a 5-point scale (e.g., 1 = not at all, 5 = extremely), most with respect to the last four weeks. To assess current physical health functioning for the analysis, we used the physical component summary score that is derived from the scale and standardized by using an algorithm so that mean = 50 and SD = 10. Higher scores indicate better overall health (α = .84 in this sample).
Demographics
The following sociodemographic characteristics were assessed using women’s self-report to survey questions: age in years, years of education attained, marital status (married or live with a common-law partner versus other status), working full- or part-time outside the home, total annual household income of less than $24,000 Canadian dollars, living with child(ren) age 16 or younger at least half the time, currently pregnant, minority status, born outside Canada, and living in a rural area (a community with fewer than 3000 residents).
Analysis
Women’s demographic characteristics at baseline were analysed using descriptive statistics. The mean and standard deviation for each of the three outcomes at all four time points—baseline, 6, 12, and 18 months—were assessed by women’s IPV exposure status. Age, education, minority status, and birth place were fixed (time-invariant) characteristics collected at baseline only; all other demographic characteristics were assessed at four time points and treated as time-varying covariates in the growth curve models.
The effects of exposure to SCA on trajectories of depressive symptoms, physical health, and psychological quality of life were examined using growth curve modeling (Singer and Willett 2003). Variables were added to the model in a hierarchical manner: the first step in the growth model estimated the unconditional means (null) model; the second step added the time variable to estimate the unconditional linear model, where time was centred such that the model intercept represents the outcome score at the last time-point; the third step added SCA exposure and its interaction with time; and, the final step added the sociodemographic co-variates to provide unbiased estimates of effects. Full information maximum likelihood was used to account for missing data in the models. Bayesian information criterion (BIC) was assessed for an overall model fit (lower scores indicate better fit). All analyses were conducted in SAS v 9.3 (SAS Institute Inc.), and growth curve models were estimated using PROC MIXED.
Compliance with ethical standards
The original trial from which these data were drawn was approved by the Research Ethics Board (REB) of McMaster University/Hamilton Health Sciences, protocol #05-102.
Results
Sample characteristics
Table 1 presents the demographic characteristics of the 411 women by IPV exposure status at baseline. Compared to those without SCA, women with exposure to SCA had attained fewer years of education, were less likely to be employed, and less likely to be married or living with a common-law partner. There were no group differences in other demographic characteristics at baseline. Table 2 presents women’s IPV exposure across time; while over half of women (55 %) report SCA at baseline, this drops to 35 % by 6 months, but still remains relatively high (29 %) at 18 months. A significant proportion (from a quarter to more than a third) fell below the CAS criterion score of 7 for current IPV exposure across the three follow-up times. Table 3 presents the means and standard deviations of row scores of outcome variables by SCA exposure status at all-time points.
SCA and trajectories
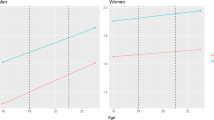
Table 4a–c and Figs. 1, 2, and 3 present results from the growth curve models for depressive symptoms, psychological quality of life, and physical health, respectively. In Table 4a, Model 2 shows an overall decrease in depressive symptoms over time (B = −1.09, SE = 0.21, p < .001). The significant random effect covariance (B = 14.22, SE = 2.95, p < .001) indicates a positive association between the intercept and slope. As shown in Model 3, women with exposure to SCA had higher depressive symptoms compared with those without SCA (B = 2.08, SE = 0.87, p = .017). SCA had no significant effect on the rate of change in depressive symptoms over time (B = −0.58, SE = 0.42, p = .163). Model 4 shows the adjusted association for SCA, which remained significant (B = 2.33, SE = 0.92, p = .012), as well as significant associations between older age, not being employed, and not being married or in a common-law relationship, and increased depressive symptoms. These results are depicted in Fig. 1.
Table 4b presents the results for women’s quality of life trajectories. Model 2 shows the overall increase in psychological quality of life over time (B = 1.51, SE = 0.29, p < .001). The significant random effect covariance (B = 26.71, SE = 6.10, p < .001) indicates a positive association between the intercept and slope. Model 3 indicates the significant negative effect of exposure to SCA on women’s quality of life (B = −3.15, SE = 1.25, p = .012). The exposure to SCA had no effect on the rate of change in quality of life scores over time (B = −0.01, SE = 0.60, p = .989). The main effect of SCA remained significant in Model 4 when covariates were added (B = −3.00, SE = 1.30, p = .021). Model 4 also indicates that older age, low income, and not being employed were associated with lower quality of life, whereas currently being pregnant, born outside Canada, and rural residence were associated with better quality of life. These results are depicted in Fig. 2.
Table 4c shows the results for women’s physical health trajectories. Model 2 indicates that physical health scores stay unchanged over time (B = 0.22, SE = 0.19, p = .252). The significant random effect covariance (B = 11.13, SE = 2.68, p < .001) indicates a positive association between the intercept and slope. There was no effect of exposure to SCA on this outcome (B = 0.77, SE = 0.84, p = .360, Model 3). The final model indicates that older age, not being employed, being married or in common-law relationship, currently pregnant, and minority status were associated with lower physical health scores. These results are depicted in Fig. 3.
Discussion
Our findings provide important new knowledge regarding the relationship, over time, between abuse severity and health and psychological quality of life. These results also show the high prevalence of severe abuse among a sample of women experiencing IPV who presented to an Ontario health care setting. Looking at bivariate associations between demographic characteristics and abuse severity, we found that only education, employment and relationship type differed significantly according to IPV severity status. This adds to previous literature regarding risk indicators correlated with IPV versus no IPV exposure (Wathen et al. 2007), pointing to the factors that might be predictive of more severe forms of violence, or, on the other hand, those factors that might be protective in terms of severe abuse. For example, there is emerging evidence that being employed may both mediate (Adams et al. 2013a) and moderate (Wathen et al. 2016) the negative health effects of IPV exposure. While acknowledging the complexity of the inter-relationships among these variables (Swanberg and Logan 2007; Rothman et al. 2007), the added role of abuse severity is under-explored. That said, given the relationship between IPV, educational attainment and employment status (Adams et al. 2013b), it is perhaps not surprising that these were two of the demographic characteristics where bivariate differences between the SCA and no SCA group were found. The finding that women who were not married or living in a common-law relationships were more likely to experience SCA is more difficult to explain. It may be that women who are dating, or separated from, abusive partners have, on average, more transitional or less stable relationships. For example, there is good evidence that women’s risk of violence increases in the early period after separation (Hardesty 2002; Johnson and Sacco 1995). More information is needed about the nature of women’s partner relationships in this sample in order to more fully explain these findings.
In terms of violence exposure, we found that the proportion of women reporting SCA declined across time, with the most precipitous drop from baseline to 6 months. In fact, a significant proportion of women, as time went on, fell below the cut-point for IPV exposure as measured by the CAS, perhaps reflecting more episodic periods of IPV, changes in relationship or life status that reduced exposure to abuse, or regression towards the mean. While the present data are not able to explain why abuse/abuse severity declined, findings such as these are not uncommon (Fritz and O’Leary 2004).
Trajectories of mental health, assessed via depressive symptoms and psychological life quality, showed similar patterns of findings: both improved across time for the entire sample, but were significantly worse for women reporting SCA (though SCA did not affect the rate of change in these scores). For both outcomes, the main effect of SCA remained significant when demographic covariates were added, and each outcome was associated with unique, and overlapping, covariates: depressive symptoms were higher and psychological quality of life poorer for women who were older, and unemployed; depressive symptoms were also worse for those not married/in a common-law relationship, while quality of life was also poorer for women reporting low income. Of note, quality of life was better for pregnant women, those born outside Canada, and those living in rural areas. These findings regarding the effects of specific characteristics on women’s health and well-being trajectories—with and without the impact of severe abuse—deepen our understanding of the nature and influence of risk and protective factors across time, an area that has been underexplored in longitudinal research and requires additional examination.
Our findings did not show effects of SCA on physical health trajectories. It is possible that impact of IPV on physical health may be delayed in comparison to mental health. Additional, longer-term research is needed, building on emerging findings such as those showing that both injuries and mental health symptoms may mediate the relationship between severity of IPV and physical health (Wuest et al. 2010), and that physical health consequences of IPV are linked to longer-term cellular and epigenetic changes (Newton et al. 2011; Fernandez-Botran et al. 2011; Humphreys et al. 2012; Out et al. 2012).
While this is a relatively large sample of abused women, all were recruited in health care settings in the same province of a high-income country; women recruited from community settings, or violence-specific services or those in low- or middle-income countries, may have different patterns of abuse experiences and trajectories. In addition, all outcomes were self-reported, and the primary outcome measures based on brief standardized instruments. While these had reasonable psychometric properties and have been used in other IPV-specific research studies, they may be more limited than comprehensive diagnostic measures. It is also the case that while this sample provided longitudinal data, the time period—18 months—was relatively short, especially for certain types of health outcomes; research over longer time periods is required.
Conclusions
This paper highlights the important association between abuse severity and women’s mental health and well-being across time. Trajectories for two of the outcomes—depressive symptoms and psychological quality of life—were remarkably consistent, with both showing significant main effects of abuse severity, such that women reporting severe abuse were more likely to have worse outcomes. The third outcome—physical health—remained more stable, for all women, across the 18-month time frame under study. Specific demographic covariates that showed stronger bivariate relationships to severe abuse and that influenced trajectories were also noted, with older age, unemployment and relationship type showing consistent negative impacts.
Ultimately, preventing IPV and other forms of gender-based violence should be the highest priority. However, understanding—and assessing—the role of different abuse experiences, risk and protective factors, and trajectories should serve to assist care providers in more accurate identification of women’s experiences of IPV, and in more tailored and appropriate care provision. Additional examination of the factors influencing outcomes for women in low- and middle-income countries, and their experiences of abuse, is urgently required.
References
Adams AE, Bybee D, Tolman RM, Sullivan CM, Kennedy AC (2013a) Does job stability mediate the relationship between intimate partner violence and mental health among low-income women? Am J Orthopsychiatr 83(4):600–608
Adams AE, Greeson MR, Kennedy AC, Tolman RM (2013b) The effects of adolescent intimate partner violence on women’s educational attainment and earnings. J Interpers Violence 28(17):3283–3300
Afifi TO, MacMillan H, Cox BJ, Asmundson GJ, Stein MB, Sareen J (2009) Mental health correlates of intimate partner violence in marital relationships in a nationally representative sample of males and females. J Interpers Violence 24(8):1398–1417
Anderson DK, Saunders DG, Yoshihama M, Bybee DI, Sullivan CM (2003) Long-term trends in depression among women separated from abusive partners. Violence Against Women 9(7):807–838
Beeble ML, Bybee D, Sullivan CM, Adams AE (2009) Main, mediating, and moderating effects of social support on the well-being of survivors of intimate partner violence across 2 years. J Consult Clin Psychol 77(4):718–729
Bonomi AE, Patrick DL, Bushnell DM, Martin M (2000) Validation of the United States’ version of the World Health Organization Quality of Life (WHOQOL) instrument. J Clin Epidemiol 53(1):1–12
Brown JB, Lent B, Schmidt G, Sas G (2000) Application of the Woman Abuse Screening Tool (WAST) and WAST-short in the family practice setting. J Fam Pract 49(10):896–903
Campbell JC (2002) Health consequences of intimate partner violence. Lancet 359:1331–1336
Campbell J, Soeken K (1999) Women’s responses to battering over time: an analysis of change. J Interpers Violence 14(1):21–40
Campbell R, Sullivan CM, Davidson WS (1995) Women who use domestic violence shelters: changes in depression over time. Psychol Women Quart 19:237–255
Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, Smith PH (2002) Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 23(4):260–268
Davies L, Ford-Gilboe M, Willson A, Varcoe C, Wuest J, Campbell J, Scott-Storey K (2015) Patterns of cumulative abuse among female survivors of intimate partner violence: links to women’s health and socioeconomic status. Violence Against Women 21(1):30–48
Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C, WHO Multi-country Study on Women’s Health and Domestic Violence against Women Study Team (2008) Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. Lancet 371(9619):1165–1172
Fernandez-Botran R, Miller JJ, Burns VE, Newton TL (2011) Correlations among inflammatory markers in plasma, saliva and oral mucosal transudate in post-menopausal women with past intimate partner violence. Brain Behav Immun 25(2):314–321
Fritz PA, O’Leary KD (2004) Physical and psychological partner aggression across a decade: a growth curve analysis. Violence Vict 19(1):3–16
Garcia-Moreno C, Jansen H, Ellsberg M, Heise L, Watts C (2005) WHO multi-country study on women’s health and domestic violence against women. Initial results on prevalence, health outcomes and women’s responses. World Health Organization, Geneva
Gerber MR, Wittenberg E, Ganz ML, Williams CM, McCloskey LA (2008) Intimate partner violence exposure and change in women’s physical symptoms over time. J Gen Intern Med 23(1):64–69
Golding JM (1999) Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence 14(2):99–132
Hardesty J (2002) Separation assault in the context of postdivorce parenting: an integrative review of the literature. Violence Against Women 8(5):597–625
Hegarty K, Sheehan M, Schonfeld C (1999) A multidimensional definition of partner abuse: development and preliminary validation of the Composite Abuse Scale. J Fam Violence 14(4):399–415
Hegarty K, Gunn J, Chondros P, Small R (2004) Association between depression and abuse by partners of women attending general practice: a descriptive cross-sectional survey. BMJ 328:621–624
Hegarty K, Bush R, Sheehan M (2005) The Composite Abuse Scale: further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Vict 20(5):529–547
Humphreys JC, Epel ES, Copper B, Lin J, Blackburn EH, Lee KA (2012) Telomere shortening in formerly abused and never abused women. Biol Res Nurs 14(2):115–123
Johnson H, Sacco VF (1995) Researching violence against women: statistics Canada’s national survey. Can J Criminol 37:281–304
MacIntosh J, Wuest J, Ford-Gilboe M, Varcoe C (2015) Cumulative effects of multiple forms of violence and abuse on women. Violence Vict 30(3):502–521
MacMillan HL, Wathen CN, Jamieson E, Boyle MH, Shannon HS, Ford-Gilboe M, the McMaster Violence Against Women Research Group (2009) Screening for intimate partner violence in health care settings: a randomized trial. J Am Med Assoc 302(5):493–501
Miladinovic Z, Mulligan L (2015) Homicide in Canada, 2014. Canadian Centre for Justice Statistics Catalogue no. 85-002-X ISSN 1209-6393, Statistics Canada, Ottawa
Newton TL, Fernandez-Botran R, Miller JJ, Lorenz DJ, Burns VE, Fleming KN (2011) Markers of inflammation in midlife women with intimate partner violence histories. J Women Health 20(12):1871–1880
Out D, Hall RJ, Granger DA, Page GG, Woods SJ (2012) Assessing salivary C-reactive protein: longitudinal associations with systemic inflammation and cardiovascular disease risk in women exposed to intimate partner violence. Brain Behav Immun 26(4):543–551
Radloff LS (1977) The CES-D scale a self-report depression scale for research in the general population. Appl Psych Meas 1(3):385–401
Rees S, Silove D, Chey T, Ivancic L, Steel Z, Creamer M, Forbes D (2011) Lifetime prevalence of gender-based violence in women and the relationship with mental disorders and psychosocial function. J Am Med Assoc 306(5):513–521
Rodgers K (1994) Wife assault: the findings of a national survey. Juristat. Cat. 85-002, 14(9). Canadian Centre for Justice Statistics, Statistics Canada, Ottawa, Ontario
Rothman EF, Hathaway J, Stidsen A, de Vries HF (2007) How employment helps female victims of intimate partner violence: a qualitative study. J Occup Health Psych 12(2):136–143
SF-36.org (n.d.). The SF-12®: an even shorter health survey. http://www.sf-36.org/tools/sf12.shtml#version2. Accessed 28 July 2015
Singer JD, Willett JB (2003) Applied longitudinal data analysis: modeling change and event occurrence. Oxford University Press, USA
Statistics Canada (2016) Family violence in Canada: a statistical profile, 2014. Canadian Centre for Justice Statistics Catalogue no. 85-002-X ISSN 1209-6393, Ottawa
Swanberg JE, Logan T (2007) Intimate partner violence, employment and the workplaces: an interdisciplinary perspective. J Interpers Violence 22(3):263–267
Ware JE, Kosinski M, Turner-Bowker DM, Gandek B (2002) SF-12v2: how to score version 2 of the SF-12 health survey. QualityMetric Incorporated, Lincoln, pp 29–38
Wathen CN, Jamieson E, Wilson M, Daly M, Worster A, MacMillan HL, McMaster University Violence Against Women Research Group (2007) Risk indicators to identify intimate partner violence in the emergency department. Open Med 1(2):e113
Wathen CN, MacGregor JCD, MacQuarrie BJ (2016) The relationship between intimate partner violence, work, and health. J Interpers Violence. doi:10.1177/0886260515624236
WHOQoL Group (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med 28(03):551–558
World Health Organization/London School of Hygiene and Tropical Medicine (2010) Preventing intimate partner and sexual violence against women: taking action and generating evidence. World Health Organization, Geneva
Wuest J, Ford-Gilboe M, Merritt-Gray M, Wilk P, Campbell J, Lent B, Varcoe C, Smye V (2010) Pathways of chronic pain in survivors of intimate partner violence: considering abuse-related injury, symptoms of post-traumatic stress disorder, depressive symptoms, and child abuse. J Womens Health 19(9):1665–1674
Acknowledgments
This research was supported by funds from the Canadian Institutes of Health Research (CIHR) Institute of Gender and Health (IGH) and Institute of Neurosciences Mental Health and Addictions (INMHA) to PreVAiL (Centre for Research Development in Gender, Mental Health and Violence across the Lifespan). Michael Boyle is Canada Research Chair in the Social Determinants of Child Health. Marilyn Ford-Gilboe holds the Women’s Health Research Chair in Rural Health from the Ontario Ministry of Health and Long-Term Care. Harriet MacMillan holds the David R. (Dan) Offord Chair in Child Studies.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the special issue “Violence and Health: Implications of the 2030 Agenda for South-North Collaboration”.
Rights and permissions
About this article
Cite this article
Wathen, C.N., Tanaka, M., MacGregor, J.C.D. et al. Trajectories for women who disclose intimate partner violence in health care settings: the key role of abuse severity. Int J Public Health 61, 873–882 (2016). https://doi.org/10.1007/s00038-016-0852-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-016-0852-6