Abstract
Background
There is limited data on long-term outcomes of per-oral endoscopic myotomy (POEM). In this study, we aim to evaluate the efficacy of POEM in patients who completed a minimum follow-up of 5 years.
Methods
Data of patients who underwent POEM and completed ≥ 5-year follow-up were analyzed, retrospectively. Primary outcome of study was clinical success (Eckardt ≤ 3) at ≥ 5 years after POEM. Secondary outcomes included predictors of dysphagia and symptomatic gastroesophageal reflux disease (GERD) on long-term follow-up.
Results
Three hundred nineteen patients (males 182, mean age 40.5 ± 14.2 years) completed a median of 73-(60–89) month follow-up. Esophageal motility disorders included idiopathic achalasia (type I 26.6%, type II 60.8%, type III 5.6%) and Jackhammer esophagus or distal esophageal spasm (2.8%). POEM was technically successful in 307 (96.2%) patients. Long-term success was 92.6% (overall), 92.1% (type I), 94.7% (type II), 87.5% (type III), and 75% (Jackhammer esophagus/distal esophageal spasm). Symptomatic GERD and reflux esophagitis were detected in 28.9% and 35.3% patients, respectively. On multivariate analysis, young age and female gender were independent risk factors for recurrent dysphagia (p = 0.037) and symptomatic GERD after POEM (p = 0.025), respectively. Lower post-POEM lower esophageal sphincter pressure was an independent predictor for reflux esophagitis (p = 0.016).
Conclusion
POEM is an effective and durable treatment for achalasia and non-achalasia spastic motility disorders. Young patients and females may be at higher risk for recurrent dysphagia and symptomatic GERD, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Per-oral endoscopic myotomy (POEM) is an established treatment modality for achalasia with excellent safety profile and short-term clinical success rates. Since achalasia is a progressive disease, relapses are known to occur irrespective of the treatment modality used. Therefore, it is imperative to evaluate the durability of POEM in achalasia as well as allied esophageal motility disorders. POEM is a relatively new treatment and the first series of POEM was published about a decade ago. Consequently, there are limited studies regarding the long-term outcomes of POEM compared to pneumatic dilatation (PD) and Heller’s myotomy (HM) [1,2,3,4,5].
In this study, we evaluated the outcomes of POEM in a large cohort of cases with achalasia and non-achalasia spastic motility disorders who completed a minimum of 5 years of follow-up.
Methods
The data of patients who underwent POEM from Jan 2013 to Dec 2020 for various esophageal motility disorders and completed at least 5-year follow-up were analyzed from a prospectively maintained database (Fig. 1). The study was approved by the institutional review board committee (AIG/AHF IRB: 34/2015).
Inclusion Criteria
-
a)
Patients with treatment naïve or previously treated cases with achalasia and non-achalasia motility disorders including Jackhammer esophagus (JHE) and diffuse Esophageal spasm (DES)
-
b)
Age ≥ 18 years
-
c)
Minimum follow-up of 5 years
Exclusion Criteria
-
a)
Follow-up < 5 years
-
b)
Refusal for written informed consent
Pre-POEM Evaluation
A standard set of evaluation was performed in all the cases including high resolution esophageal manometry (HRM), timed barium esophagogram, and upper gastrointestinal endoscopy. The height of barium column at 5 min was recorded. We have described the manometry evaluation in our previous study [6]. During HRM, following parameters were recorded: type of esophageal motility disorder, lower esophageal sphincter (LES) pressures, and integrated relaxation pressures.
POEM Technique
All the POEM procedures were performed by three operators (MR, ZN, and DNR) by standard technique described in previous studies [6, 7]. In brief, anterior route of POEM (1–2 o’clock) was preferred as we began performing POEM procedures via this route. Posterior route was chosen in cases with a history of Heller’s myotomy. Post procedure, oral contrast study was performed on the second post-operative day before initiating oral diet.
Follow-up Protocol
All patients were followed at pre-defined intervals i.e. 3 months, 6 months, 1 year, and annually thereafter. Evaluation at 3 and 6 months included symptom assessment for achalasia (Eckardt score) as well as gastroesophageal reflux (heartburn and regurgitation). Objective assessment was done at 3-months and 1 year including endoscopy, timed barium esophagogram, and HRM. At subsequent annual visits, symptom assessment was performed.
Management of Gastroesophageal Reflux Disease
Proton pump inhibitors (PPIs) were prescribed to all the patients for about 3 months after POEM. Objective assessment of gastroesophageal reflux disease (GERD) was performed at 3 months using endoscopy, 24-h pH study, and symptom assessment (heartburn or regurgitation). PPIs were prescribed in cases with symptomatic GERD or increased esophageal acid exposure or erosive esophagitis (LA ≥ B). Subsequently, GERD was assessed (symptom and gastroscopy) at annual visits. In those with severe symptoms or reflux esophagitis (LA grade C or D), early assessment (3–6 months) was advised to document resolution of symptoms or healing of esophagitis. Further evaluation with esophageal manometry and timed barium esophagogram was planned in cases with persistent symptoms (especially regurgitation) without significant reflux esophagitis to differentiate GERD from recurrence of primary disease i.e. achalasia.
Primary Outcome
The primary outcome of the study was clinical efficacy at ≥ 5-year follow-up. Clinical success was defined using Eckardt score which is a composite score consisting of sub-scores for dysphagia (0–3), regurgitation (0–3), chest pain (0–3), and weight loss (0–3). The minimum and maximum possible scores are 0 and 12, respectively. Clinical success was defined as Eckardt score ≤ 3. The outcomes were recorded during annual follow-up visits. All the patients who completed ≥ 5 year and could not come for physical visits were contacted by telephonic questionnaire for clinical success and symptomatic GERD.
Secondary Outcomes
The secondary outcomes included the prevalence and predictors of dysphagia, symptomatic GERD, and reflux esophagitis after POEM. The symptoms of GERD were evaluated using a standardized questionnaire including 16 Likert-type questions, with responses ranging from 0 (no symptoms) to 5 (worst symptoms) to each question was used to calculate GERD-HRQL score [8]. The total score was calculated by summing the individual scores to questions 1–15. The heartburn and regurgitation severity scores were calculated by summing the individual scores to questions 1 to 6 and 10 to 15, respectively. The greatest possible total score (worst symptoms) was 75 and the worst possible symptom score for each symptom was 30 [9]. Reflux esophagitis was graded according to the Los Angeles classification system (LA grade A to D) [10].
Statistics
The continuous data were expressed as mean (standard deviation) and compared with independent sample t test and the categorical data as frequencies and compared with chi-square test unless otherwise specified. The comparison of Eckardt score between pre- and post-POEM (at 1 and 5 years) was done using repeated measure analysis of variance (ANOVA). Multivariate analysis was performed using binominal logistic regression to ascertain the effects of age, gender, type of achalasia, Eckardt score (pre- and post-POEM), LES pressures (pre- and post-POEM) on recurrence of dysphagia, symptomatic GERD, and reflux esophagitis at long-term. Linearity of the continuous variables with respect to the logit of the dependent variable was assessed via the Box-Tidwell procedure. All the tests of significance were two tailed and a p value of < 0.05 was considered to indicate statistical significance.
Results
A total of 1,230 patients underwent POEM for achalasia and non-achalasia esophageal motility disorders during the study period. Of these, 319 patients (males 182, mean age 40.5 ± 14.2 years) completed ≥ 5-year [median 73 months (range 60–89)] follow-up and were included in the study. The spectrum of motility disorders included type I achalasia (26.6%), type II achalasia (60.8%), type III achalasia (5.6%), and JHE/DES (2.8%). A history of prior treatment was present in 142 (45.5%).
POEM was technically successful in 307 (96.2%) patients. POEM could not be completed in 12 (3.8%) patients due to severe submucosal fibrosis (n = 9) and extension of mucosal incision (n = 3). Baseline Eckardt score, manometry parameters, and intra-operative details including length and orientation of myotomy have been outlined in Table 1.
Primary outcome
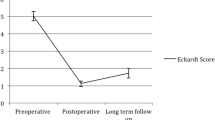
The data regarding efficacy and clinical GERD were available in 283 (88.4%) and 270 (84.6%) patients, respectively. Clinical success was recorded in 262 (92.6%) patients who successfully underwent POEM and were available for final follow-up. In intention to treat analysis (including technical failures (3.8%) and lost to follow-up (7.5%)), the clinical success in the overall group was observed in 262/319 (82.1%). The clinical success according to the type of achalasia and motility disorders were as follows: type I (92.1%), type II (94.7%), type III (85.7%), and JHE/DES (75%) (Fig. 2). There was significant reduction in the mean Eckardt scores at 1 and 5 years compared to baseline (p < 0.001); however, there was no significant difference in the mean Eckardt score between various indications of POEM (p = 0.098) (Fig. 3). There was no impact of prior interventions on the long-term clinical outcome after POEM (naïve 94.1% vs prior treatment 90.7%; p = 0.276).
Change in mean Eckardt score. Significant reduction in the mean Eckardt score was observed at 1 and 5 years after POEM compared to baseline. There was no significant difference in the mean Eckardt score between various indications of POEM at baseline and long-term follow-up (POEM, per-oral endoscopic myotomy; JH, Jackhammer esophagus; DES, distal esophageal spasm)
Secondary Outcome
Dysphagia
The information on recurrence of dysphagia was available in 270 (84.6%) patients. Dysphagia of any degree (1–3) was noticed in 114 (42.2%) patients at ≥ 5 years. Majority (78.5%) had occasional dysphagia equivalent to Eckardt score of one. On univariate and multivariate analysis, young age was the only predictive factor for dysphagia recurrence on long-term follow-up. The baseline Eckardt score, type of achalasia, length and orientation of myotomy, baseline manometry parameters, and history of prior treatment had no significant impact on the recurrence of dysphagia after POEM (Table 2).
Gastroesophageal Reflux Disease
Clinical symptoms of GERD were present in 78 (28.9%) patients. On univariate and multivariate female sex was a significant predictor of GERD (Table 3). Other factors including the type of achalasia, age, gender, length and orientation of myotomy, post-POEM LES pressures, and history of prior treatment had no significant impact on the incidence of symptomatic GERD at ≥ 5-year follow-up.
The data on reflux esophagitis was available in 119 (42%) patients. Of these, 26 (21.8%) patients were on regular PPIs and another 9 (7.6%) on demand PPIs. Erosive esophagitis was detected in 42 (35.3%) of which majority (97.5%) had mild (LA grade A and B) esophagitis. Only 3 (2.5%) patients had severe (LA grade C) esophagitis. On univariate analysis, a higher post treatment Eckardt score and lower post-POEM LES pressures were significant predictors of reflux esophagitis (Fig. 4). The mean difference in the post-POEM LES pressures in the two groups (with and without reflux esophagitis) was 2.45 (95%CI 0.65–4.25) mmHg. On multivariate analysis, a lower post-POEM LES pressure was the only significant predictor of reflux esophagitis (p = 0.016) (Table 4).
Outcomes in Clinical Failures
Overall, clinical failure were recorded in 21 (7.4%) patients at a median follow-up of 16 (3–40) months. Majority (14, 66.7%) of the clinical failures occurred within 2 years of POEM procedure. The proportion of relapses was higher among the first half of the study cohort compared to the latter half (9.3% vs 4.1%; p = 0.072). A re-intervention was performed in ten cases including one or more sessions of pneumatic dilatation (n = 6), re-POEM via alternate route (n = 3), and esophagectomy (n = 1). Clinical response (Eckardt ≤ 3) was documented in four cases who underwent pneumatic dilatation and all the three cases who underwent re-POEM. The remaining eleven cases refused (n = 7) for further interventions or lost to follow-up (n = 4).
Discussion
In this study, we found POEM to be an effective and durable treatment modality for achalasia and non-achalasia spastic motility disorders of the esophagus. Symptomatic GERD was uncommon and detected in less than 1/3rd patients beyond 5-year follow-up.
The safety and short-term efficacy of POEM have been recognized in multiple studies. POEM has been shown to be superior to pneumatic dilatation and non-inferior to laparoscopic Heller’s myotomy with fundoplication [11, 12]. Consequently, the updated societal guidelines have incorporated POEM into the management algorithm of achalasia [13,14,15,16]. Unlike pneumatic dilatation and Heller’s myotomy, there is limited data on the long-term outcomes of POEM in achalasia. Since achalasia is a progressive disease, long-term outcomes are crucial to establish the durability of POEM in esophageal achalasia.
In this study, we evaluated the outcomes of POEM including clinical success and symptomatic GERD in cases who completed at least 5-year follow-up. Overall, clinical success was recorded in 93% of the patients at ≥ 5-year follow-up. Our results are concordant with previous studies with clinical success in upto 95% cases at a median follow-up ranging from 3 to 7 years [1,2,3, 5, 17,18,19,20,21,22]. Therefore, it is reasonable to conclude that POEM is a durable treatment modality for achalasia and other spastic esophageal motility disorders.
In our study, majority of the clinical failures occurred in the first half of the study cohort. Besides, nearly two-thirds of the relapses were encountered within 2 years of POEM procedure. Early relapses and preponderance of the failures in the initial cohort likely represent the learning curve effect. Since the number of clinical failures was too small, we analyzed the risk factors for recurrent dysphagia on long-term follow-up. Majority of the cases with dysphagia had occasional difficulty in swallowing equivalent to Eckardt score of one. Among various factors assessed, young age was found to be an independent risk factor for dysphagia of any severity at ≥ 5 years. However, it is important to note that young age was just a predictor of dysphagia and not clinical failure. Whether these cases develop relapse (Eckardt ≥ 3) over subsequent years remains to be seen.
Clinical success was better in non-spastic achalasia (type I and type II) when compared to spastic esophageal motility disorders including type III achalasia, JHE, and DES. However, the difference did not reach statistical significance presumably due to small number of patients in the latter group. We have previously published the short- and long-term outcomes in cases with type III achalasia and other spastic esophageal motility disorders. The clinical success at short-term (≤ 3 years) follow-up in type III achalasia, Jackhammer esophagus, and distal esophageal spasm were 92.7%, 83.3%, and 90%, respectively [23]. In agreement to our results, some of the recent studies reveal a relatively lower clinical success (82–90%) in cases with spastic esophageal motility disorders at a median follow-up ranging from 6 to 48 months [24,25,26].
Clinical GERD and reflux esophagitis was detected in 29% and 35.3% of the patients, respectively. In previous studies, symptomatic GERD been documented in 20–37% patients at a median follow-up ranging from two to four years indicating that symptomatic GERD is relatively less common after POEM when compared to reflux esophagitis at short-term and long-term follow-up [2, 4, 5, 21, 22]. Among various factors analyzed, female gender was an independent risk factor for symptomatic GERD. The association between female gender and pH positive GERD has been concluded in a previous multicenter study by Kumbhari et al. (odds ratio 1.69, 95% confidence interval 1.04–2.74) [27]. Some population-based studies indicate that women report significantly higher frequency of symptoms corresponding with GERD suggesting that gender difference might exist in the perception and reporting of symptoms [28]. In the absence of objective evaluation, we acknowledge that these results may be interpreted with caution since the symptoms of achalasia like regurgitation, heartburn, and chest pain mimic those of GERD as well as functional heartburn, esophageal hypersensitivity, and non-cardiac chest pain. Therefore, in cases with persistent symptoms on PPI and without objective evidence of GERD (pH study or LA grade C or D), further evaluation with timed barium esophagogram and or high resolution manometry may be performed to rule out relapse of the primary disease. On the other hand, a lower post-POEM LES pressure was an independent risk factor for reflux esophagitis and female gender was not found to be a predictor for erosive esophagitis after POEM. It is important to note that there was substantial overlap in the post-POEM LES pressures between the two groups i.e. those with and without erosive esophagitis. Multicenter studies are required to substantiate the correlation of LES pressures with reflux esophagitis.
The incidence of reflux esophagitis in our study was lower at ≥ 5 years (35%) compared to that at 3 months (48%) in our previously published study [29]. In other studies, the incidence of reflux esophagitis after POEM ranges from 40 to 60% during short-term follow-up (3–4 months) [12, 29, 30]. The results of our study indicate that the incidence of reflux esophagitis may reduce with time after POEM. Our results are in concordance with the landmark randomized trial by Werner and colleagues where the incidence of post-POEM reflux esophagitis was lower at 24 months compared to 3 months (44% vs 57%) [12]. In a recent study, esophageal acid exposure and compliance of gastroesophageal junction reduced on follow-up after POEM [30].
There are several strengths of our study. To the best of our knowledge, this is one of the largest studies evaluating the long-term outcomes of POEM (≥ 5 years). The number of cases who lost to follow-up was within acceptable range (< 10%). In addition, our study presents with new findings with respect to the risk factors for dysphagia, reflux esophagitis, and symptomatic GERD in long-term. We acknowledge certain limitations. First, endoscopic assessment of GERD could be done in only 42% of patients in long-term. The possibility of selection bias cannot be excluded as symptomatic patients are more likely to agree for objective evaluation of GERD. Nevertheless, the available data indicates that there is poor correlation between symptoms and erosive esophagitis. Therefore, it is less likely (albeit not impossible) that GERD was grossly underdiagnosed or overdiagnosed to a substantial extent. Second, some of risk factors for clinical failure and GERD like disease duration, esophageal dilatation, and BMI could not be analyzed due to incomplete information.
Conclusion
POEM is a durable treatment option for achalasia and non-achalasia spastic motility disorders. In long-term, young age may predispose to recurrent dysphagia. Female gender and lower post-POEM LES pressures are risk factors for symptomatic GERD and reflux esophagitis, respectively.
Data Availability
The original anonymous dataset is available on request from the corresponding author at zaheernabi1978@gmail.com.
References
Guo H, Yang H, Zhang X, Wang L, Lv Y, Zou X, Ling T (2017) Long-term outcomes of peroral endoscopic myotomy for patients with achalasia: a retrospective single-center study. Dis Esophagus 30:1-6
Li QL, Wu QN, Zhang XC, Xu MD, Zhang W, Chen SY, Zhong YS, Zhang YQ, Chen WF, Qin WZ, Hu JW, Cai MY, Yao LQ, Zhou PH (2018) Outcomes of per-oral endoscopic myotomy for treatment of esophageal achalasia with a median follow-up of 49 months. Gastrointest Endosc 87:1405-1412 e1403
Teitelbaum EN, Dunst CM, Reavis KM, Sharata AM, Ward MA, DeMeester SR, Swanstrom LL (2018) Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc 32:421-427
He C, Li M, Lu B, Ying X, Gao C, Wang S, Ma C, Jin C (2019) Long-Term Efficacy of Peroral Endoscopic Myotomy for Patients with Achalasia: Outcomes with a Median Follow-Up of 36 Months. Dig Dis Sci 64:803-810
Brewer Gutierrez OI, Moran RA, Familiari P, Dbouk MH, Costamagna G, Ichkhanian Y, Seewald S, Bapaye A, Cho JY, Barret M, Eleftheriadis N, Pioche M, Hayee BH, Tantau M, Ujiki M, Landi R, Invernizzi M, Yoo IK, Roman S, Haji A, Hedberg HM, Parsa N, Mion F, Fayad L, Kumbhari V, Agarwalla A, Ngamruengphong S, Sanaei O, Ponchon T, Khashab MA (2020) Long-term outcomes of per-oral endoscopic myotomy in achalasia patients with a minimum follow-up of 4 years: a multicenter study. Endosc Int Open 8:E650-E655
Ramchandani M, Nageshwar Reddy D, Darisetty S, Kotla R, Chavan R, Kalpala R, Galasso D, Lakhtakia S, Rao GV (2016) Peroral endoscopic myotomy for achalasia cardia: Treatment analysis and follow up of over 200 consecutive patients at a single center. Dig Endosc 28:19-26
Nabi Z, Ramchandani M, Chavan R, Kalapala R, Darisetty S, Rao GV, Reddy N (2017) Per-oral endoscopic myotomy for achalasia cardia: outcomes in over 400 consecutive patients. Endosc Int Open 5:E331-E339
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20:130-134
Karyampudi A, Nabi Z, Ramchandani M, Darisetty S, Goud R, Chavan R, Kalapala R, Rao GV, Reddy DN (2021) Gastroesophageal reflux after per-oral endoscopic myotomy is frequently asymptomatic, but leads to more severe esophagitis: A case-control study. United European Gastroenterol J 9:63–71
Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ, Tytgat GN, Wallin L (1999) Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45:172-180
Ponds FA, Fockens P, Lei A, Neuhaus H, Beyna T, Kandler J, Frieling T, Chiu PWY, Wu JCY, Wong VWY, Costamagna G, Familiari P, Kahrilas PJ, Pandolfino JE, Smout A, Bredenoord AJ (2019) Effect of Peroral Endoscopic Myotomy vs Pneumatic Dilation on Symptom Severity and Treatment Outcomes Among Treatment-Naive Patients With Achalasia: A Randomized Clinical Trial. JAMA 322:134-144
Werner YB, Hakanson B, Martinek J, Repici A, von Rahden BHA, Bredenoord AJ, Bisschops R, Messmann H, Vollberg MC, Noder T, Kersten JF, Mann O, Izbicki J, Pazdro A, Fumagalli U, Rosati R, Germer CT, Schijven MP, Emmermann A, von Renteln D, Fockens P, Boeckxstaens G, Rosch T (2019) Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med 381:2219-2229
Jung HK, Hong SJ, Lee OY, Pandolfino J, Park H, Miwa H, Ghoshal UC, Mahadeva S, Oshima T, Chen M, Chua ASB, Cho YK, Lee TH, Min YW, Park CH, Kwon JG, Park MI, Jung K, Park JK, Jung KW, Lim HC, Jung DH, Kim DH, Lim CH, Moon HS, Park JH, Choi SC, Suzuki H, Patcharatrakul T, Wu JCY, Lee KJ, Tanaka S, Siah KTH, Park KS, Kim SE, Korean Society of N, Motility (2020) 2019 Seoul Consensus on Esophageal Achalasia Guidelines. J Neurogastroenterol Motil 26:180-203
Khashab MA, Vela MF, Thosani N, Agrawal D, Buxbaum JL, Abbas Fehmi SM, Fishman DS, Gurudu SR, Jamil LH, Jue TL, Kannadath BS, Law JK, Lee JK, Naveed M, Qumseya BJ, Sawhney MS, Yang J, Wani S (2020) ASGE guideline on the management of achalasia. Gastrointest Endosc 91:213-227 e216
Oude Nijhuis RAB, Zaninotto G, Roman S, Boeckxstaens GE, Fockens P, Langendam MW, Plumb AA, Smout A, Targarona EM, Trukhmanov AS, Weusten B, Bredenoord AJ (2020) European guidelines on achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J 8:13-33
Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT (2020) ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol 115:1393-1411
McKay SC, Dunst CM, Sharata AM, Fletcher R, Reavis KM, Bradley DD, DeMeester SR, Muller D, Parker B, Swanstrom LL (2021) POEM: clinical outcomes beyond 5 years. Surg Endosc 35:5709–5716
Zhang WG, Chai NL, Zhai YQ, Linghu EQ, Li HK (2020) Long-term outcomes of peroral endoscopic myotomy in achalasia patients with a minimum follow-up of 7 years. Chin Med J (Engl) 133:996-998
Tefas C, Boros C, Ciobanu L, Surdea-Blaga T, Tantau A, Tantau M (2020) POEM: Five Years of Experience in a Single East European Center. J Gastrointestin Liver Dis 29:323-328
Onimaru M, Inoue H, Fujiyoshi Y, Abad MRA, Nishikawa Y, Toshimori A, Shimamura Y, Tanabe M, Sumi K, Ikeda H (2021) Long-term clinical results of per-oral endoscopic myotomy (POEM) for achalasia: First report of more than 10-year patient experience as assessed with a questionnaire-based survey. Endosc Int Open 9:E409-E416
Campagna RAJ, Cirera A, Holmstrom AL, Triggs JR, Teitelbaum EN, Carlson DA, Pandolfino JE, Hungness ES (2021) Outcomes of 100 Patients More Than 4 Years After POEM for Achalasia. Ann Surg 273:1135-1140
Modayil RJ, Zhang X, Rothberg B, Kollarus M, Galibov I, Peller H, Taylor S, Brathwaite CE, Halwan B, Grendell JH, Stavropoulos SN (2021) Peroral endoscopic myotomy: 10-year outcomes from a large, single-center U.S. series with high follow-up completion and comprehensive analysis of long-term efficacy, safety, objective GERD, and endoscopic functional luminal assessment. Gastrointest Endosc 94:930–942
Nabi Z, Chavan R, Ramchandani M, Basha J, Jagtap N, Karyampudi A, Darisetty S, Tandan M, Goud R, Rao GV, Reddy DN (2021) Long-term Outcomes of Per-oral Endoscopic Myotomy in Spastic Esophageal Motility Disorders: A Large, Single-Center Study. J Clin Gastroenterol 55:594-601
Filicori F, Dunst CM, Sharata A, Abdelmoaty WF, Zihni AM, Reavis KM, Demeester SR, Swanstrom LL (2019) Long-term outcomes following POEM for non-achalasia motility disorders of the esophagus. Surg Endosc 33:1632-1639
Bernardot L, Roman S, Barret M, Vitton V, Wallenhorst T, Pioche M, Chaussade S, Gonzalez JM, Ponchon T, Prat F, Barthet M, Vergniol J, Chabrun E, Zerbib F (2020) Efficacy of per-oral endoscopic myotomy for the treatment of non-achalasia esophageal motor disorders. Surg Endosc 34:5508–515
Zhang W, Linghu EQ (2017) Peroral Endoscopic Myotomy for Type III Achalasia of Chicago Classification: Outcomes with a Minimum Follow-Up of 24 Months. J Gastrointest Surg 21:785-791
Kumbhari V, Familiari P, Bjerregaard NC, Pioche M, Jones E, Ko WJ, Hayee B, Cali A, Ngamruengphong S, Mion F, Hernaez R, Roman S, Tieu AH, El Zein M, Ajayi T, Haji A, Cho JY, Hazey J, Perry KA, Ponchon T, Kunda R, Costamagna G, Khashab MA (2017) Gastroesophageal reflux after peroral endoscopic myotomy: a multicenter case-control study. Endoscopy 49:634-642
Kim YS, Kim N, Kim GH (2016) Sex and Gender Differences in Gastroesophageal Reflux Disease. J Neurogastroenterol Motil 22:575-588
Nabi Z, Ramchandani M, Kotla R, Tandan M, Goud R, Darisetty S, Rao GV, Reddy DN (2020) Gastroesophageal reflux disease after peroral endoscopic myotomy is unpredictable, but responsive to proton pump inhibitor therapy: a large, single-center study. Endoscopy 52:643-651
Modayil RJ, Zhang X, Rothberg B, Kollarus M, Galibov I, Peller H, Taylor S, Brathwaite CE, Halwan B, Grendell JH, Stavropoulos SN (2021) Peroral endoscopic myotomy: 10-year outcomes from a large, single-center U.S. series with high follow-up completion and comprehensive analysis of long-term efficacy, safety, objective GERD, and endoscopic functional luminal assessment. Gastrointest Endosc 94:930-942
Author information
Authors and Affiliations
Contributions
Zaheer Nabi, Pradev Inavolu, and Mohan Ramchandani were involved in conception of the study. Jahangeer Basha, Rajesh Goud, and Radhika Chavan were involved in acquisition and analysis of the data. Arun Karyampudi, Santosh Darisetty, and D. Nageshwar Reddy were involved in revising the manuscript for important intellectual content. All the authors agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study was reviewed and approved for publication by our Institutional Reviewer.
Consent to Participate
All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nabi, Z., Karyampudi, A., Ramchandani, M. et al. Predictors of Long-Term Outcomes, Recurrent Dysphagia, and Gastroesophageal Reflux After Per-oral Endoscopic Myotomy in Esophageal Motility Disorders. J Gastrointest Surg 26, 1352–1361 (2022). https://doi.org/10.1007/s11605-022-05330-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05330-z