Abstract
Background
Peroral endoscopic myotomy (POEM) is a novel operation for the treatment of achalasia and other esophageal motility disorders. While POEM has shown excellent short-term safety and efficacy, the long-term symptomatic outcomes after the procedure are unknown.
Methods
Patients from a single center that underwent POEM for treatment of esophageal motility orders and were greater than 5 years removed from their operation were studied. Patients were contacted to assess current symptoms and encouraged to undergo repeat endoscopy for objective follow-up.
Results
Thirty-six patients underwent POEM from October, 2010 to February, 2012 and current symptom scores were obtained from 29 patients at median 65-month follow-up. In the 23 patients with achalasia, Eckardt scores were significantly improved from preoperative baseline (mean current 1.7 vs. preoperative 6.4, p < 0.001). Nineteen patients (83%) with achalasia had a symptomatic success (Eckardt ≤3) and none required retreatment for symptoms. Eckardt scores were dramatically improved at 6 months and maintained at 2 years; however, there was a small but significant worsening of symptoms between 2 and 5-years. Of the five patients with EGJ outflow obstruction, all had current Eckardt scores ≤3 but two needed reintervention for persistent or recurrent symptoms, one with a laparoscopic Heller myotomy and another with an endoscopic cricomyotomy and proximal esophageal myotomy extension. At 6-month follow-up, repeat manometry showed decreased EGJ relaxation pressures and esophagram demonstrated improved emptying. 24-h pH monitoring showed abnormal distal esophageal acid exposure in 38% of patients. Fifteen patients underwent endoscopy at 5-years, revealing erosive esophagitis in two (13%), new hiatal hernia in two, and new non-dysplastic Barrett’s esophagus in one. The patient with Barrett’s underwent a subsequent laparoscopic hiatal hernia repair and Toupet fundoplication.
Conclusions
POEM resulted in a successful palliation of symptoms in the majority of patients after 5 years, though these results emphasize the importance of long-term follow-up in all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achalasia is a disease of primary esophageal dysmotility that results from an immune-mediated loss of neurons in the esophageal myenteric plexus. This causes a failure of both swallow-induced lower esophageal sphincter (LES) relaxation and esophageal peristalsis, leading to symptoms of dysphagia, regurgitation, and chest pain [1]. Treatment is aimed at disrupting the LES in order to reduce esophageal outflow resistance and thus improve passive emptying of food boluses. Two interventional therapies have comprised the standard-of-care treatment for achalasia for more than twenty years: laparoscopic Heller myotomy with partial fundoplication (LHM) and endoscopic pneumatic dilation (PD). Both procedures result in a dramatic initial improvement in symptoms in approximately 75–95% of patients [2], although PD often requires a series of several dilations to achieve an adequate clinical effect [3] and meta-analyses have shown better overall efficacy after LHM [2, 4]. While this palliation remains durable in many patients, a substantial number will experience recurrent symptoms in the years following either LHM or PD with more than half requiring reintervention in some series [5, 6].
A novel operation, peroral endoscopic myotomy (POEM), has been introduced as alternative treatment for achalasia and other disorders of esophageal motility. First performed by Inoue in 2008 [7], POEM combines many of the theoretical advantages of both LHM and PD, by creating a controlled surgical myotomy across the esophagogastric junction (EGJ) via a completely endoscopic approach. Outcomes after POEM have been encouraging, with excellent short-term results in early published series that appear comparable to LHM and PD [8, 9]. Due to the relatively recent clinical introduction of POEM, longer term outcomes are limited to a handful of series. Studies examining patients with greater than two-year follow-up have found a durability of symptomatic relief ranging 79–92% [10,11,12], suggesting there may be a degradation of treatment efficacy after POEM commensurate with that following LHM and PD. As of yet, no POEM series have reported outcomes at greater than three years.
In this study, we examined the outcomes of patients who underwent POEM at our institution and were greater than five years removed from their operation. We sought to evaluate the durability of symptomatic relief after POEM, as well findings on repeat upper endoscopy in order to better understand the long-term outcomes of the procedure.
Methods
Preoperative evaluation and patient selection
Patients who had undergone POEM by surgeons in a single practice and were greater than 5 years removed from their operation were included in this study. All patients were part of an Institutional Review Board approved longitudinal outcomes study. Preoperatively, patients underwent history and physical exam, including a symptom assessment using the Eckardt score [13] (Table 1). All patients were evaluated with upper endoscopy, timed barium esophagram (TBE), and high-resolution manometry (HRM) to establish a diagnosis according to the Chicago Classification of esophageal motility disorders [14]. Inclusion criteria for POEM were age ≥18 years and a manometrically confirmed diagnosis of achalasia. Patients with other esophageal motility disorders (including EGJ outflow obstruction (EGJOO), distal esophageal spasm (DES), and jackhammer esophagus) that the patient’s treating physician determined would benefit from EGJ myotomy were also included. Exclusion criteria were inability to tolerate general anesthesia, uncorrectable coagulopathy, and esophageal varices. During the study period, such patients were counseled regarding the available treatment options including PD, LHM, and POEM, and chose to undergo POEM in consultation with their physicians. All patients underwent informed and written consent for POEM per an Institutional Review Board approved research protocol.
POEM procedure
Our operative technique for POEM has been previously described in detail [15] and is similar to the procedure as originally performed by Inoue [7]. Briefly, POEM is performed under general anesthesia with endotracheal intubation. A high-definition flexible gastroscope with CO2 insufflation is used, with an overtube in place. An upper endoscopy is performed and, in a retroflexed position in the stomach, blue dye is injected on the anterior-lesser curve approximately 3 cm distal the EGJ in order to mark the end point of the dissection. The scope is then fitted with a transparent dissecting cap and a submucosal injection is performed to create a wheal in the anterior-right esophageal wall. A longitudinal incision is made in the mucosa overlying the injection and the scope is navigated through this mucosotomy and into the submucosal space. A longitudinal submucosal tunnel is then created, ending 3 cm beyond the EGJ at the point marked by the prior blue dye injection. A selective myotomy of the circular muscle layer is then performed starting proximal to the dysfunctional EGJ and ending at the distal extent of the tunnel, 2–3 cm distal to the EGJ. The myotomy is started further proximally in some patients with DES and EGJOO in order to ablate the entire spastic segment of esophagus. After completion of the myotomy, the mucosotomy is closed using endoscopic clips.
Perioperative management
Patients were kept nil per os and underwent a contrast esophagram on the first postoperative day. If negative for leak, they were started on a liquid diet and discharged the same day if progressing as expected. They were allowed to gradually advance from a puree to soft food diet over the following two weeks. The patients involved in this study were not routinely placed on proton pump inhibitors (PPI) or H2 antagonists (H2A) in the initial postoperative period.
Follow-up symptom and physiologic assessment
At 6-months postoperatively, patients had repeat symptom assessment using the Eckardt score and underwent upper endoscopy, HRM, TBE, and 24-h pH monitoring to assess for iatrogenic gastroesophageal reflux (GER). Patients with elevated distal esophageal acid exposure on 24-h pH were advised to begin anti-secretory therapy. At 2 years, patients were again assessed using the Eckardt score.
Patients who were greater than 5 years removed from their POEM procedure at the time of the current study were contacted via telephone to obtain a current Eckardt score. Symptomatic “success” was defined as a current Eckardt score ≤3 and freedom from reintervention for persistent or recurrent symptoms, in line with prior studies [16]. Additionally, a GerdQ score was obtained, with a score >7 considered indicative of symptomatic GER in line with prior usage of the questionnaire [17]. Patients were encouraged to have a repeat upper endoscopy at 5 years post-POEM. During endoscopy, esophagitis was graded according to the Los Angeles (LA) classification.
Statistical analysis
Data analysis was performed using SPSS software (version 23; IBM, Armonk, NY). For continuous variables, comparisons were performed using an independent or paired t test as appropriate. A two-tailed p-value of <0.05 was used to determine statistical significance in all cases. Values throughout are presented as mean ± standard deviation unless otherwise specified.
Results
Preoperative patient characteristics and perioperative outcomes
Thirty-six patients underwent POEM from October 2010 to February 2012 and were included in the study. The operations were performed by one of three surgeons (LLS, CMD, and KMR) and these patients represent the initial cases in the institutional experience. Twenty patients (56%) were female and the median age was 55 years (range 20–88 years). The preoperative diagnosis was achalasia type I in 10 patients, achalasia type II in 17, EGJOO in 7 and DES in 2. Eighteen patients (50%) had either preoperative pneumatic dilation or botulinum toxin injection for treatment of achalasia prior to undergoing POEM.
Median operative time was 130 min (range 60–220 min). Median length of stay was 1 day (range 1–2 days) and 32 patients (89%) were discharged postoperative day 1. There was one complication (Clavien Dindo Grade IIIa), a patient who was readmitted with gastrointestinal bleeding from a gastric ulceration just distal to the EGJ. This was treated successfully with upper endoscopy and clip placement.
Symptomatic outcomes and reinterventions
Current symptom scores were obtained from 29 patients (81%) at a median follow-up interval of 65 months (range 60–76 months). Of these patients, 23 had a preoperative diagnosis of achalasia (8 type I, 15 type II), 5 had EGJOO, and 1 DES. Four patients were lost to follow-up and 3 were deceased, all due to causes unrelated to achalasia or POEM. In achalasia patients with greater than 5-year follow, Eckardt scores were significantly improved from preoperative baseline (mean current 1.7 ± 1.7 vs. preoperative 6.4 ± 2.6, p < 0.001). Nineteen achalasia patients (83%) had a symptomatic success at current follow-up (Eckardt ≤3) and none required reintervention for persistent or recurrent symptoms. Table 2 shows the change in each symptom component of the Eckardt score, and Table 3 shows the change in total Eckardt scores according to diagnosis subtype. There was a significant decrease in all four symptom domains, but the degree of improvement was somewhat less for chest pain.
In the five patients with EGJOO, all had current Eckardt scores ≤3 but two required repeat interventions after POEM. One patient had persistent dysphagia and elevated relaxation pressures on repeat HRM and underwent a LHM with partial fundoplication 11 months after her initial POEM. Another patient with EGJOO had symptomatic relief after POEM but more than two years later had a recurrence of chest pain and developed new cervical dysphagia. She was found to have a hypertensive upper esophageal sphincter and a spastic segment of esophagus proximal to where the POEM myotomy had been performed. She was treated with an endoscopic cricomyotomy with myotomy extension to disrupt the spastic segment. Both patients’ reoperations were successful, resulting in current Eckardt scores ≤2. The one patients with DES had a symptomatic success at current follow-up.
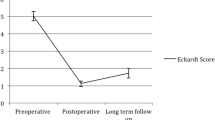
Prospective symptom assessment at all three postoperative time points (6 months, 2 years, and 5 years) was available for 23 patients, whose Eckardt scores over time are shown in Fig. 1. Eckardt scores were dramatically improved at 6 months postoperatively (mean 0.6 ± 0.7 vs. 6.4 ± 2.6 preoperatively, p < 0.001) and maintained at 2 years (0.7 ± 1.1, p = n.s. vs. 6 months), but there was a significant worsening of Eckardt scores at 5 years (1.7 ± 1.7, p = 0.01 vs. 2 years). All four patients with current Eckardt scores >3 in the study cohort had scores ≤1 at the 2-year postoperative timepoint. Dysphagia was the primary recurrent symptom in these patients, with all four complaining of dysphagia daily or with every meal. Only two of the four had occasional regurgitation (i.e., less frequently than daily) and none had weight loss. One of these patients does not currently desire further treatment and the other three are in the process of being evaluated for potential reintervention.
Eckardt symptom score progression of the 23 patients with prospectively collected symptom evaluations at all four time points. The bold line represents the mean Eckardt score at each time point. Mean scores were dramatically decreased at 6-months postoperatively and this improvement was maintained at 2 years. There was a slight, but significant, worsening of scores between 2- and 5-year postoperatively
At greater than 5-year follow-up, 6 patients (21%) had symptoms suggestive of GER (i.e., GerdQ score >7) and 8 patients (26%) were taking a daily PPI or H2A therapy. One patient with EGJOO underwent a laparoscopic hiatal hernia repair and Toupet fundoplication for treatment-refractory GER, 5 years after his initial POEM. The patient had developed a 4 cm Type I hiatal hernia that was not present on pre-POEM esophagram, HRM, or endoscopy.
Of the seven patients who were deceased or lost to follow-up, the mean Eckardt score at last follow-up was 1.7 ± 1 (median postoperative interval of 12 months, range 6–30 months) and all would have been considered therapeutic successes (i.e., Eckardt ≤3) at last follow-up.
Postoperative physiologic and anatomic evaluation
Table 4 shows the results of pre- and postoperative physiologic and anatomic studies. On repeat HRM at 6 months postoperatively (n = 25), EGJ relaxation pressures were significantly decreased from baseline (pre 23 ± 15 mmHg vs. post 9 ± 7 mmHg, p < 0.01) and percent esophageal emptying on timed barium esophagram (n = 29) was increased (pre 50 ± 36% vs. post 92 ± 23%, p < 0.001). At 6 months, a 24-h pH monitoring study was performed in 29 patients, demonstrating abnormal distal esophageal acid exposure (i.e., DeMeester score >14.7) in 11 patients (38%). Twenty-three patients had a 6-month upper endoscopy which showed esophagitis in 9 patients (39%, 5 LA A, 4 LA B). At 5-year follow-up, 16 patients had a repeat upper endoscopy which demonstrated esophagitis in 2 patients (13%, 1 LA A, 1 LA B), hiatal hernia in 2 patients (13%, both Type I) and new non-dysplastic Barrett’s esophagus in one patient (who subsequently underwent laparoscopic hiatal hernia repair and Toupet fundoplication, as described above).
Discussion
The main finding of this study was that POEM for treatment of achalasia resulted in durable long-term symptomatic relief for 83% of patients without the need for reintervention. While patients’ current symptoms were dramatically improved at 5 years compared with their preoperative baseline, there did appear to be a slight worsening of symptoms between two and five years following the operation. All four achalasia patients in this study with symptomatic failures after POEM had an excellent initial treatment response, but developed recurrent symptoms during this period. Delayed symptomatic regression in some patients appears to be part of the natural history of post-treatment achalasia after POEM, as well as following LHM and PD. Early reports of the short-term outcomes after POEM demonstrated near-resolution of symptoms in 90–95% of patients, whereas more recent publications of 2–3-year outcomes have shown success rates in the range of 79–92% [10,11,12]. The same pattern of symptom recurrence occurs after both LHM and PD. The recent European achalasia trial randomized patients to either LHM or PD, resulting in treatment success rates at two years of 90 and 86%, respectively [16]. However, at 5-year follow-up from this trial, these success rates had decreased to 84 and 82% [3]. There is wide variation in the reported long-term success rates of both LHM and PD in prior single-center series, ranging from 47 to 87% for LHM and as low at 0% for PD [5, 6, 18]. While this degree of variance makes comparison to historic results difficult, the findings of our current study add to the growing body of evidence that suggests POEM results in equivalent treatment efficacy and durability when compared with the current standard-of-care interventions for achalasia.
A particular early concern regarding POEM was that it would result in high rates of iatrogenic GER, given it does not include creation of an anti-reflux barrier as is typically performed during LHM. In the current study, 38% of patients had pathologic GER on routine 24-h pH monitoring study, a number that is consistent with other POEM series [10]. The rate of iatrogenic GER after LHM with partial fundoplication has varied greatly between studies, but the most recent randomized trials have reported frequencies in the range of 21–42% [16, 19]. We found that at 6-month upper endoscopy, 39% of patients had reflux esophagitis; however, during our initial POEM experience we did not routinely place patients on anti-secretory therapy postoperatively. After follow-up endoscopy and pH monitoring, patients were placed on medical therapy if they had evidence of pathologic GER, and on repeat endoscopy at 5-years only 13% had esophagitis. This finding demonstrates that although POEM resulted in GERD, a substantial minority of patients can successfully be treated with PPIs or H2As. It should be noted that one patient was found to have new non-dysplastic Barrett’s esophagus 5 years after POEM. In the interval since his initial operation, he had also developed a 4 cm Type I hiatal hernia and had LA B esophagitis despite medical therapy. He subsequently underwent a laparoscopic hiatal hernia repair and Toupet fundoplication and is currently doing well with an Eckardt score of 0 and no GER symptoms.
When taken in total, these results emphasize the importance of careful evaluation and surveillance of patients before and after POEM. Ours and other's studies have shown severe GER after POEM in patients with hiatal hernia [10], and our current recommendation is that patients with significant hiatal hernia should be offered LHM with concurrent hernia repair rather than POEM. Multiple studies have demonstrated that after myotomy for achalasia (either LHM or POEM), typical symptoms, such as heartburn and bitter-tasting regurgitation, are poor correlates of objective distal esophageal acid exposure as measured by 24-h pH monitoring [20, 21]. This discordance, combined with a 30–40% incidence of post-POEM GER, makes routine postoperative 24-h pH monitoring mandatory. Our current practice is to place all patients on anti-secretory therapy postoperatively and then tailor the need for extended therapy based on the results of pH monitoring performed at 6–12 months after surgery.
In addition to GER, the progression of achalasia symptoms needs to be carefully monitored and evaluated. The two patients with EGJOO in our series who required reinterventions had markedly different presentations. The first had only transient and partial symptomatic improvement after POEM and had a persistently elevated EGJ relaxation pressure on repeat HRM. She likely had an incomplete initial myotomy and was treated to good effect with a subsequent LHM. The second patient had an excellent initial symptomatic response after POEM, but years later developed recurrent chest pain and new cervical dysphagia. On repeat HRM, she had low EGJ pressures, but had a hypertensive upper esophageal sphincter and a spastic segment in the proximal esophagus. A repeat endoscopic myotomy was performed, dividing the cricopharyngeal muscle with extension through the upper esophagus, which resulted in resolution of these symptoms. Although two of five patients with EGJOO in our series required reintervention, symptomatic results after PD in other series have also been poor [22]. EGJOO is a relatively new categorization in the Chicago Classification with evolving diagnostic criteria. The optimal treatment algorithm for such patients is as yet unknown and further evaluation of outcomes is needed [23].
Through contacting patients for this study, four achalasia patients with recurrent symptoms were identified and they are currently undergoing physiologic reevaluation. These examples stress the need for life-long monitoring of patients after POEM, as well as the importance of a detailed evaluation of persistent or recurrent symptoms using endoscopy, HRM, TBE, and pH monitoring in order to tailor the optimal reintervention to patient-specific pathophysiology.
This study has some limitations. Most important of these are the small sample size of the study which may affect both the validity and generalizability of the results. These patients represent our initial experience with POEM, an operation that our group and others have shown to have a learning curve that is tied to intraoperative and short-term patient outcomes [24, 25]. It is possible that with increased experience, long-term symptomatic outcomes after the procedure will improve. Additionally, although we stress the importance of long-term surveillance with our patients, some were lost to follow-up and a minority underwent repeat endoscopy at 5 years. This may have introduced unintended selection bias to the findings.
In conclusion, POEM resulted in a sustained long-term palliation of symptoms in a majority of patients and the need for reintervention was rare. There appears to be a slight worsening of overall symptoms between 2 and 5 years postoperatively, on par with that seen after both LHM and PD. Overall, these results encourage the continued use of POEM for the treatment of achalasia and other esophageal motility disorders.
References
Boeckxstaens GE, Zaninotto G, Richter JE (2014) Achalasia. Lancet 383:83–93
Yaghoobi M, Mayrand S, Martel M, Roshan-Afshar I, Bijarchi R, Barkun A (2013) Laparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trials. Gastrointest Endosc 78:468–475
Moonen A, Annese V, Belmans A, Bredenoord AJ, Bruley des Varannes S, Costantini M, Dousset B, Elizalde JI, Fumagalli U, Gaudric M, Merla A, Smout AJ, Tack J, Zaninotto G, Busch OR, Boeckxstaens GE (2016) Long-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomy. Gut 65:732–739
Schoenberg MB, Marx S, Kersten JF, Rosch T, Belle S, Kahler G, Vassiliou MC, Luth S, von Renteln D (2013) Laparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysis. Ann Surg 258:943–952
Sawas T, Ravi K, Geno DM, Enders F, Pierce K, Wigle D, Katzka DA (2017) The course of achalasia one to four decades after initial treatment. Aliment Pharmacol Ther 45:553–560
Vela MF, Richter JE, Khandwala F, Blackstone EH, Wachsberger D, Baker ME, Rice TW (2006) The long-term efficacy of pneumatic dilatation and Heller myotomy for the treatment of achalasia. Clin Gastroenterol Hepatol 4:580–587
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL (2014) A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 259:1098–1103
von Renteln D, Inoue H, Minami H, Werner YB, Pace A, Kersten JF, Much CC, Schachschal G, Mann O, Keller J, Fuchs KH, Rosch T (2012) Peroral endoscopic myotomy for the treatment of achalasia: a prospective single center study. Am J Gastroenterol 107:411–417
Hungness ES, Sternbach JM, Teitelbaum EN, Kahrilas PJ, Pandolfino JE, Soper NJ (2016) Per-oral endoscopic myotomy (POEM) after the learning curve: durable long-term results with a low complication rate. Ann Surg 264:508–517
Werner YB, Costamagna G, Swanstrom LL, von Renteln D, Familiari P, Sharata AM, Noder T, Schachschal G, Kersten JF, Rosch T (2016) Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 65:899–906
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264
Eckardt VF (2001) Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am 11:281–292
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, International High Resolution Manometry Working G (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Swanstrom LL, Rieder E, Dunst CM (2011) A stepwise approach and early clinical experience in peroral endoscopic myotomy for the treatment of achalasia and esophageal motility disorders. J Am Coll Surg 213:751–756
Boeckxstaens GE, Annese V, des Varannes SB, Chaussade S, Costantini M, Cuttitta A, Elizalde JI, Fumagalli U, Gaudric M, Rohof WO, Smout AJ, Tack J, Zwinderman J, Zaninotto G, Busch OR, European Achalasia Trial I (2011) Pneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasia. N Engl J Med 364:1807–1816
Jones R, Junghard O, Dent J, Vakil N, Halling K, Wernersson B, Lind T (2009) Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther 30:1030–1038
Zaninotto G, Costantini M, Rizzetto C, Zanatta L, Guirroli E, Portale G, Nicoletti L, Cavallin F, Battaglia G, Ruol A, Ancona E (2008) Four hundred laparoscopic myotomies for esophageal achalasia: a single centre experience. Ann Surg 248:986–993
Rawlings A, Soper NJ, Oelschlager B, Swanstrom L, Matthews BD, Pellegrini C, Pierce RA, Pryor A, Martin V, Frisella MM, Cassera M, Brunt LM (2012) Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: results of a multicenter, prospective, randomized-controlled trial. Surg Endosc 26:18–26
Familiari P, Gigante G, Marchese M, Boskoski I, Tringali A, Perri V, Costamagna G (2016) Peroral endoscopic myotomy for esophageal achalasia: outcomes of the first 100 patients with short-term follow-up. Ann Surg 263:82–87
Gholoum S, Feldman LS, Andrew CG, Bergman S, Demyttenaere S, Mayrand S, Stanbridge DD, Fried GM (2006) Relationship between subjective and objective outcome measures after Heller myotomy and Dor fundoplication for achalasia. Surg Endosc 20:214–219
Okeke FC, Raja S, Lynch KL, Dhalla S, Nandwani M, Stein EM, Chander Roland B, Khashab MA, Saxena P, Kumbhari V, Ahuja NK, Clarke JO (2017) What is the clinical significance of esophagogastric junction outflow obstruction? evaluation of 60 patients at a tertiary referral center. Neurogastroenterol Motil. doi:10.1111/nmo.13061
Perez-Fernandez MT, Santander C, Marinero A, Burgos-Santamaria D, Chavarria-Herbozo C (2016) Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol Motil 28:116–126
Teitelbaum EN, Soper NJ, Arafat FO, Santos BF, Kahrilas PJ, Pandolfino JE, Hungness ES (2014) Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM). J Gastrointest Surg 18:92–98 discussion 8–9
Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanstrom LL (2013) Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc 77:719–725
Acknowledgements
The authors would like to acknowledge Angie Gill, RN, and Lisa Leeth for their help coordinating the clinical aspects of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Reavis is a consultant for Boston Scientific, Endogastric Solutions, and Stryker, and receives teaching or advisory honoraria from Ethicon, Mederi, Gore, and Apollo. Dr. DeMeester is a consultant for Bard. Dr. Swanstrom is on the scientific advisory boards of Olympus and Boston Scientific. These disclosures are not related to the current study. Drs. Teitelbaum, Dunst, Sharata, and Ward have no disclosures or conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Teitelbaum, E.N., Dunst, C.M., Reavis, K.M. et al. Clinical outcomes five years after POEM for treatment of primary esophageal motility disorders. Surg Endosc 32, 421–427 (2018). https://doi.org/10.1007/s00464-017-5699-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5699-2