Abstract
Background
The rate of early (< 30 days) complications after bariatric surgery has been reported to be 0.4–27.4%. Although the incidence of serious adverse events has decreased with time and experience, controversy regarding how they are reported persists, and the current literature is heterogeneous.
Methods
Data from patients, who underwent primary bariatric surgery (gastric bypass and sleeve gastrectomy) at a single institution between 2012 and 2018, were retrospectively reviewed. Any deviation from a “normal” postoperative course (< 30 days) was identified, and a comparative analysis of early complications according to five models was performed: modified Clavien-Dindo; Longitudinal Assessment of Bariatric Surgery (LABS); Bariatric Surgery Centers of Excellence (BSCOE); American Society for Metabolic and Bariatric Surgery (ASMBS); and Li (major/minor).
Results
A total of 788 patients (83.7% gastric bypass), of whom 8.8% deviated from a “normal” postoperative course, were included. After applying the five classifications, the results were as follows: Clavien-Dindo, 8.8%; LABS, 2.3%; BSCOE, 0.4%; ASMBS, 9.9%; and Li, 11.2%. The incidence of major/severe/adverse outcomes were as follows: Clavien-Dindo, 2.4%; LABS, 2.3%; BSCOE, 0.4%; ASMBS, 6.9%; and Li 9.2%. Minor complications were as follows: Clavien-Dindo, 6.5%; ASMBS, 3%; and Li, 2%. There was no mortality.
Conclusion
Germane heterogeneity was found in reporting of early complications after bariatric surgery. Incidence varied according to classification system applied, and Clavien-Dindo demonstrated accuracy as a reporting model. To avoid bias, standardized reporting should be mandatory, and a more stringent and homogeneous reporting system should be established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Bariatric and metabolic surgery has yielded proven health benefits, such as weight loss, weight loss maintenance, and resolution of comorbidities associated with obesity 1 For > 50 years, Roux-en-Y gastric bypass (RYGB) was the most common bariatric procedure worldwide. More recently, however, RYGB has been displaced by sleeve gastrectomy (SG) due to its increasing popularity as a primary bariatric procedure 2,3. Both procedures, nevertheless, have resulted in significant weight loss and resolution of comorbidities 4,5,6,7,8,9,10,11,12.
Historically, bariatric surgery was considered to be a high-risk procedure with severe morbidity (≥ 10%) in the era of open surgery13. This field has been revolutionized with the advent of laparoscopy as the standard of care, and the implementation of standardized techniques and management algorithms in the past few decades, reflected by a decrease in complication rates 14,15,16. However, there is a lack of consensus regarding the definition of a surgical complication; as such, recommendations have been made for the classifications used to address this topic 17. Complications are classified according to the time of presentation—early (≤ 30 days) and late (> 30 days) (5)—however, there is heterogeneity in the description of the type of such complications. There is a tendency to divide complications according to severity; however, several discrepancies exist among classifications and authors. Consequently, complication rates after bariatric surgery have been reported to be between 0.4% and 27.4% 7,10,14,15,18,19,20. Such radical differences are related to the classification or model used to describe events. The objective of the present analysis, therefore, was to characterize this variability in reporting complications by applying different models/classifications reported in the literature.
Methods
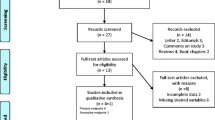
A retrospective study (using prospectively collected data) of patients, who underwent primary bariatric surgery (RYGB or SG) at a single institution between 2012 and 2018, was performed. The primary objective was to identify differences in the incidence of early complications (< 30 days) based on the classification used to report them. First, an analysis to identify any event that deviated from a “normal” postoperative course in the first 30 days was performed. All patients identified were considered to have an early complication. Second, every event was re-classified according to five models/classifications used in the bariatric surgery literature, including: modified Clavien-Dindo21; Longitudinal Assessment of Bariatric Surgery (LABS)15; Bariatric Surgery Centers of Excellence (BSCOE)14; American Society for Metabolic and Bariatric Surgery (ASMBS)17; and major and minor complications described by Li et al. 22. The detailed models/classifications are reviewed in Supplement 1. A descriptive analysis of each model/classification, including overall morbidity and minor and major or severe complications, was performed. For re-classification purposes, only patients that fulfilled SOFA criteria 23 for sepsis were considered in the classifications that include or mention this condition.
Models and Classifications
Modified Clavien-Dindo
This classification was first reported in 1992 and modified in 2004, and can be used in any given surgical series to report complications and their severity. It grades complications from I to V according to severity. Grades III and IV have subclassifications (IIIa, IIIb, IVa, and IVb) depending on whether re-intervention was performed with or without general anesthesia (IIIb and IIIa, respectively), or if one or multiple organ failures are present (IVa and IVb, respectively) 21.
LABS
The LABS was used by Flum et al. (LABS consortium) to report 30-day outcomes in a cohort study in 2009. It accounts for death, venous thromboembolism, reintubation, reintervention (endoscopic, percutaneous, or surgical), and failure to discharge after 30 days. No other complications were reported 15.
BSCOE
The BSCOE program reporting system, as described by Pratt et al., was used when the Surgical Review Committee (SRC) presented a summary of key statistics of patient data collected and entered into a national database of centers participating in the BSCOE program using two separate definitions for complications: serious and others. Serious complications include death, deep venous thrombosis, stroke/cerebrovascular accident, heart attack, pulmonary embolus, heart failure or pulmonary edema, renal failure, liver failure, multi-system organ failure, sepsis from a leak, and systemic inflammatory response syndrome. The remaining complications are bundled, as in other studies 14,17.
ASMBS
Suggested by Brethauer et al. in their 2015 article bariatric surgery reporting standards, the ASMBS divides complications into early (≤ 30 days) and late (> 30 days), and further into major and minor. The authors defined major complications that resulted in prolonged hospital stay (> 7 days) or any adverse event that led to reoperation or reintervention, such as venous thromboembolism, requiring anticoagulant or embolectomy, anastomotic leak requiring reoperation, reintervention, percutaneous drainage or stent placement, and gastrointestinal hemorrhage requiring transfusion or intervention (Supplement 1). Minor complications included everything that was not included under major, such as marginal ulcer diagnosed using upper endoscopy but not requiring endoscopic intervention, nausea, and vomiting requiring intravenous fluids, among others (Supplement 1) 17. This is a flexible classification system.
Li et al. (major/minor)
In this single-institution multicenter regional cohort, used as a standardized means of reporting complications, Li et al. described 30-day and 1-year adverse events including reoperation, readmission, and death, dividing them into minor and major adverse events. A specific definition for minor adverse events was not specified; however, wound problems or infection, nausea and vomiting not requiring readmission, and abdominal pain that did not require readmission, were considered to be minor (Supplement 1).
Major adverse events were defined as any complication requiring readmission, intervention, intensive care unit stay, or reoperation, including anastomotic leak, staple line leak or abscess, gastric or intestinal perforation, postoperative hemorrhage, or gastrointestinal bleeding requiring transfusion, reoperation, or intervention. Death is also included in this category 22 (Supplement 1).
Statistical analysis
Data are expressed using descriptive statistics as mean and standard deviation (± SD) or percentage (%) where applicable. All data were grouped and analyzed using SSPS version 25.0 (IBM Corporation, Armonk, NY, USA).
Results
In a 6-year period, 805 patients underwent bariatric surgery, of whom 17 were excluded due to revisional surgery. Of the remaining 788 patients, 668 (83.7%) underwent RYGB. Females comprised 80.7% of all cases, which had a mean age of 38.8 ± 9.7 years. Baseline demographic information and patient characteristics are summarized in Table 1. A total of 69 (8.8%) patients experienced a deviation from a “normal” postoperative course (Table 2). After re-classification, the following morbidity rates were observed: Clavien-Dindo, 8.8% (6.4% mild/minor and 2.4% major/severe) (Table 3) REV1 COM2; LABS, 2.3% (all of which were classified as major/severe) (Table 4); BSCOE, 0.4% (all of which were considered to be major/severe) (Table 5); ASMBS, 9.9% (6.9% major/severe and 3% mild/minor) (Table 6); and Li et al. reported that 11.2% (9.2% major/severe and 2% mild/minor) (Table 7). When comparing the performance of all five classifications, the global morbidity rate ranged from 0.4 to 11.2%, with a wide range of mild/minor (2–6.5%) and severe/major (0.4–9.2%) complications (Table 8).
Discussion
In this retrospective study, including 788 patients who underwent primary bariatric surgery (RYGB and SG) in a 6-year period at a single institution, we observed an early complication rate that was similar to international reports, including reference centers in highly industrialized countries.
With the advent of minimally invasive techniques in the early 1990s, morbidity and mortality in bariatric surgery have dramatically improved. In the late 1990s, mortality associated with bariatric surgery was reported to be 0.5–1.0%, which persisted into the early 2000s due to translation of laparoscopic techniques to bariatric surgery and the inexperience of surgeons performing these new procedures 24. Since then, mortality associated with bariatric procedures has decreased several-fold and has been reported to be as low as 0.1–0.3%, making these procedures extremely safe compared to mortality associated with colorectal surgery (1–3%)24,25,26 and similar to that of common general surgical procedures such as anti-reflux surgery or laparoscopic cholecystectomy 26,27.
Evidence suggests that any given bariatric procedure can be safe and effective (i.e., lower morbidity and mortality) in the hands of many surgeons over the long term if a defined sequence between operative steps is performed. In 2018, the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) called for a meeting of experts comprising panelists from all over the world in New Delhi, India (the first such gathering) to reach consensus regarding standardization of bariatric surgery techniques to ensure uniformity in comparisons and facilitate the development of the safest and most effective procedures to treat obesity and metabolic disorders 28. Our results demonstrated that when applying any given classification system or reporting method, early morbidity can vary significantly in the same group of patients (0.4–11.2%), and be sub-reported or over-reported.
When compared with other series, we observed that overall morbidity (8.8%) was similar 10,11,29 or lower 30,31 than the reported complications in randomized controlled trials. The reoperation rate (1.1%) was also similar to that reported in a meta-analysis of early complications by Osland et al. (1.5%) 32. Finally, in our series, gastrointestinal bleeding and leak/fistula were the two most common early complications (2.2% and 2.0%, respectively). This differs from the bleeding rate reported by Helmio et al. 30 which was twice as high (4.2%), and the rate reported by Zhang et al. 31 (3.1%); however, this is similar to the fistula/leak rate (1.6% and 1.5% respectively) in both SG and RYGB patients in their randomized controlled trials. The lower gastrointestinal bleeding rate in our group of patients was probably due to selective—rather than routine—use of chemical thromboprophylaxis.
According to Dindo et al. in their original classification 21, minor complications were events that did not require therapy other than analgesia, antipyresis, antiemesis, or antibiotics for lower urinary infection (Grade I), and all other complications were regarded to be potentially life-threatening and, thus, severe or major (≥ Grade II). The modified classification in the same report, which was used in this review, considers the mentioned minor complications and now divides them into Grade I and II depending on whether pharmacological therapy was used, and the life-threatening complications (previously Grade II) were graded as III and higher. Consistent with these thoughts and for the purpose of this study, Clavien-Dindo Grade I and II were regarded as minor or mild, and Grade IIIa, IIIb, IVa, and IVb as major or severe. Some authors, however, find this classification inflexible and cumbersome 17. When applying this classification to the study group, a global morbidity rate of 8.8% was observed, in concordance with the 8.8% morbidity reported in the study group. It is noteworthy that 2 (0.2%) patients experienced > 1 early complication, and only the most severe complication was coded in this classification. In addition, it is also worth noting that only 2.4% of the complications were coded as severe, while 6.4% were mild. This differs greatly from the results observed for all the other four classifications.
According to Flum et al. (LABS consortium) 15, all adverse outcomes reported were those that required reintervention or were life-threatening in nature. In this review, all events reported in the LABS classification were considered to be major or severe. When re-classifying our cohort into this classification, a 2.3% global morbidity rate was observed, which cannot be divided into major or severe complications because all complications listed in their report are life-threatening and, thus, considered to be severe. If we compare this rate (2.3%) to the severe/major complications observed with modified Clavien-Dindo (2.4%), we notice that it is similar; thus, it can be assumed that it neglects and does not report minor/other complications (6.7%), creating significant variability in the morbidity rate reported/observed.
Pratt et al. (BSCOE) 14,17 defined all 30-day complications as severe adverse outcomes. Therefore, all events reported in this study in the BSCOE classification were considered to be major or severe. It used two separate definitions for complications: serious and others. Considering only the listed complications (deep venous thrombosis, cerebral vascular accident, acute myocardial infarction, pulmonary embolism, heart failure, pulmonary edema, renal failure, liver failure, multiple organ failure, sepsis due to leak or death), we obtained a 0.4% morbidity (and 0.4% severe complications) rate; thus, the classification leaves the majority of complications (8.5% for the study group) unclassified and unaccounted for.
In 2015, Brethauer et al. 17 proposed a standardized method for reporting bariatric surgery outcomes, including complications, which takes into account the time frame as early (< 30 days) or late (> 30 days) and severity; major complications and minor complications without definitions of each but thoroughly describing each group. In this review, the ASMBS classification was used as described in the document. After application, a 9.9% morbidity rate was observed with a 6.9% rate of severe/major and 3% of mild/minor complication rates. A higher morbidity rate was observed because the classification includes “and reoperation’’ (includes surgery, percutaneous drainage or bedside procedure) as major complications; as such, a patient who was readmitted to the hospital and surgically intervened because of a leak, codes three times in this classification. Therefore, it is not surprising that because of double and triple coding, a higher rate of severe/major complications was obtained using this classification.
Finally, in 2015, Li et al. 22 described another way of reporting adverse bariatric surgery outcomes, grouping them as minor adverse events and major adverse events. For this review, their classification was applied “as is” to our patient group. After application, 11.2% morbidity was observed with a 9.2% severe major and 2% mild/minor complication rate. Again, in their classification, they include “and reoperation” as major complications and not as therapeutic actions to deal with a complication. It differs from the ASMBS including sepsis and multiple organ failure as major complication; thus, a septic patient that is readmitted and reoperated because a gastrointestinal leak can code several times into this classification. Thus, the more specific the classification, the higher the morbidity it tends to reveal; therefore, a higher morbidity (compared with the group’s and modified Clavien-Dindo) was observed with a disproportionately high severe/major complication rate. The most frequent early complications in bariatric surgery include bleeding from any source and gastrointestinal leaks/fistulae, accounting for more than one-half of major early complications and the cause of most reoperations or interventions (i.e., endoscopy, percutaneous drainage, and transfusion) 9,10,29,30,31,32. In our patient series, such complications accounted for 59.4% of all early complications.
We observed that, for unknown reasons, there is a tendency not to use the modified Clavien-Dindo classification when reporting morbidity in the American literature (North, Central, and South America). However, we found it to be the most representative classification (and easier to apply) of actual complications, taking into account the severity of the complication and the therapeutic measures taken to treat such complications. We consider that every event should be reported, just as Pierre-Alain Clavien and Daniel Dindo stated: every event can be classified. An example is the way to report sepsis, since none of the original articles used to classify complications clearly defines it. The previous underrates the estimation of real adverse events following surgery. For example, we considered a fistula as major complication despite being treated conservatively (no sepsis and non-invasive treatment). It is important to know the real anastomotic leak rate even if sepsis was not present.
In summary, this is the first analysis (to our knowledge) addressing the disparity while reporting complications in this specific surgical field. There were limitations to the present study, the first of which were its retrospective and descriptive design, and that it considered only two procedures (i.e., RYGB and SG). Furthermore, the RYGB to SG ratio was 7 to 1 and, finally, that it was a single-center rather than a multicenter experience. Future efforts should focus on developing consensus to standardize reporting of adverse events.
Conclusions
There is germane heterogeneity in the reporting of early complications following bariatric surgery. After applying five different classifications within the same group of patients, a wide range of overall minor and major complications was observed. The modified Clavien-Dindo is the broadest and most punctual classification. Standardization may avoid—or at least mitigate—bias when adverse events are reported, and a more stringent and homogeneous reporting system should be established.
References
Marcotte E, Chand B. Management and prevention of surgical and nutritional complications after bariatric surgery. Surg Clin North Am 2016;96:843–56. https://doi.org/10.1016/j.suc.2016.03.006.
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, et al. Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes Surg 2017;27:2279–89. https://doi.org/10.1007/s11695-017-2666-x.
Phillips BT, Shikora SA. The history of metabolic and bariatric surgery: development of standards for patient safety and efficacy. Metabolism 2018;79:97–107. https://doi.org/10.1016/j.metabol.2017.12.010.
Sharples AJ, Mahawar K. Systematic review and meta-analysis of randomised controlled trials comparing long-term outcomes of roux-en-y gastric bypass and sleeve gastrectomy. Obes Surg 2020;30:664–72. https://doi.org/10.1007/s11695-019-04235-2.
Mingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, et al. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet 2015;386:964–73. https://doi.org/10.1016/S0140-6736(15)00075-6.
Chen Y, Corsino L, Shantavasinkul PC, Grant J, Portenier D, Ding L, et al. Gastric bypass surgery leads to long-term remission or improvement of type 2 diabetes and significant decrease of microvascular and macrovascular complications. Ann Surg 2016;263:1138–42. https://doi.org/10.1097/SLA.0000000000001509.
Vidal P, Ramón JM, Goday A, Benaiges D, Trillo L, Parri A, et al. Laparoscopic gastric bypass versus laparoscopic sleeve gastrectomy as a definitive surgical procedure for morbid obesity. Mid-term results. Obes Surg 2013;23:292–9. https://doi.org/10.1007/s11695-012-0828-4.
Lim DM, Taller J, Bertucci W, Riffenburgh RH, O’Leary J, Wisbach G. Comparison of laparoscopic sleeve gastrectomy to laparoscopic Roux-en-Y gastric bypass for morbid obesity in a military institution. Surg Obes Relat Dis 2014;10:269–76. https://doi.org/10.1016/j.soard.2012.08.012.
Boza C, Gamboa C, Salinas J, Achurra P, Vega A, Pérez G. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: a case-control study and 3 years of follow-up. Surg Obes Relat Dis 2012;8:243–9. https://doi.org/10.1016/j.soard.2011.08.023.
Peterli R, Borbély Y, Kern B, Gass M, Peters T, Thurnheer M, et al. Early results of the swiss multicentre bypass or sleeve study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg 2013;258:690–5. https://doi.org/10.1097/SLA.0b013e3182a67426.
Kehagias I, Karamanakos SN, Argentou M, Kalfarentzos F. Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI<50 kg/m 2. Obes Surg 2011;21:1650–6. https://doi.org/10.1007/s11695-011-0479-x.
Shoar S, Saber AA. Long-term and midterm outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass: a systematic review and meta-analysis of comparative studies. Surg Obes Relat Dis 2017;13:170–80. https://doi.org/10.1016/j.soard.2016.08.011.
Grundy SM, Barondess JA, Bellegie NJ, Fromm H, Greenway F, Halsted CH, et al. Gastrointestinal surgery for severe obesity. Ann Intern Med 1991;115:956–61. https://doi.org/10.7326/0003-4819-115-12-956.
Pratt GM, Learn CA, Hughes GD, Clark BL, Warthen M, Pories W. Demographics and outcomes at American Society for metabolic and bariatric surgery centers of excellence. Surg Endosc Other Interv Tech 2009;23:795–9. https://doi.org/10.1007/s00464-008-0077-8.
Flum DR, Belle SH, Longitudinal Assessment of Bariatric Surgery (LABS) consortium. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 2009;361:445–54. https://doi.org/10.1056/nejmoa0901836.
Lancaster RT, Hutter MM. Bands and bypasses: 30-day morbidity and mortality of bariatric surgical procedures as assessed by prospective, multi-center, risk-adjusted ACS-NSQIP data. Surg Endosc Other Interv Tech 2008;22:2554–63. https://doi.org/10.1007/s00464-008-0074-y.
Brethauer SA, Kim J, El Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Relat Dis 2015;11:489–506. https://doi.org/10.1016/j.soard.2015.02.003.
DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American society for metabolic and bariatric surgery-designated bariatric surgery centers of excellence using the bariatric outcomes longitudinal database. Surg Obes Relat Dis 2010;6:347–55. https://doi.org/10.1016/j.soard.2009.11.015.
Stenberg E, Szabo E, Ågren G, Näslund E, Boman L, Bylund A, et al. Early complications after laparoscopic gastric bypass surgery: results from the scandinavian obesity surgery registry. Ann Surg 2014;260:1040–7. https://doi.org/10.1097/SLA.0000000000000431.
MacIejewski ML, Winegar DA, Farley JF, Wolfe BM, Demaria EJ. Risk stratification of serious adverse events after gastric bypass in the Bariatric Outcomes Longitudinal Database. Surg Obes Relat Dis 2012;8:671–7. https://doi.org/10.1016/j.soard.2012.07.020.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Li RA, Fisher DP, Dutta S, O’Brien RM, Ackerson LM, Sorel ME, et al. Bariatric surgery results: reporting clinical characteristics and adverse outcomes from an integrated healthcare delivery system. Surg Obes Relat Dis 2015;11:1119–25. https://doi.org/10.1016/j.soard.2015.03.002.
Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis. JAMA 2016;315:762. https://doi.org/10.1001/jama.2016.0288.
Nguyen NT, Vu S, Kim E, Bodunova N, Phelan MJ. Trends in utilization of bariatric surgery, 2009–2012. Surg Endosc 2016;30:2723–7. https://doi.org/10.1007/s00464-015-4535-9.
Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis, 2003-2012. JAMA Surg 2014;149:275–87. https://doi.org/10.1001/jamasurg.2013.3654.
Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol 2017;14:160–9. https://doi.org/10.1038/nrgastro.2016.170.
Villamere J, Gebhart A, Vu S, Nguyen NT. Utilization and outcome of laparoscopic versus robotic general and bariatric surgical procedures at Academic Medical Centers. Surg Endosc 2015;29:1729–36. https://doi.org/10.1007/s00464-014-3886-y.
Bhandari M, Fobi MAL, Buchwald JN, Abbass A, Abu Dayyeh BK, Alamo M, et al. Standardization of bariatric metabolic procedures: world consensus meeting statement. Obes Surg 2019;29:309–45. https://doi.org/10.1007/s11695-019-04032-x.
Yang J, Wang C, Cao G, Yang W, Yu S, Zhai H, et al. Long-term effects of laparoscopic sleeve gastrectomy versus roux-en-Y gastric bypass for the treatment of Chinese type 2 diabetes mellitus patients with body mass index 28–35 kg/m2. BMC Surg 2015;15. https://doi.org/10.1186/s12893-015-0074-5.
Helmiö M, Victorzon M, Ovaska J, Leivonen M, Juuti A, Jaser N, et al. SLEEVEPASS: a randomized prospective multicenter study comparing laparoscopic sleeve gastrectomy and gastric bypass in the treatment of morbid obesity: preliminary results. Surg Endosc 2012;26:2521–6. https://doi.org/10.1007/s00464-012-2225-4.
Zhang Y, Zhao H, Cao Z, Sun X, Zhang C, Cai W, et al. A randomized clinical trial of laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy for the treatment of morbid obesity in China: a 5-year outcome. Obes Surg 2014;24:1617–24. https://doi.org/10.1007/s11695-014-1258-2.
Osland E, Yunus RM, Khan S, Alodat T, Memon B, Memon MA. Postoperative early major and minor complications in laparoscopic vertical sleeve gastrectomy (LVSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) procedures: a meta-analysis and systematic review. Obes Surg 2016;26:2273–84. https://doi.org/10.1007/s11695-016-2101-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All procedures performed involving human participants were in accordance with the ethical standards of the institution and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Heterogeneity exists when reporting bariatric surgical complications.
• Incidence of complications varies according to classification system applied.
• Claviend-Dindo classification demonstrates accuracy as a reporting model.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Flores, J.E., Berrones, R., Guilbert, L. et al. Complications Rate Variability after Bariatric Surgery and the Importance of Standardization of a Reporting System. J Gastrointest Surg 26, 1154–1161 (2022). https://doi.org/10.1007/s11605-022-05280-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05280-6