Abstract
Background
Intraductal papillary neoplasm of the bile duct (IPNB) has a wide range of histopathology and intra- and extrahepatic tumor locations.
Methods
This retrospective single-center study evaluated the clinicopathological features and long-term outcomes of 146 patients with IPNB of the liver (IPNB-L) who underwent hepatic resection between January 2002 and June 2019.
Results
The 146 patients included 97 (66.4%) men and 49 (33.6%) women, of mean age 64.3 ± 8.0 years. Seventy-two (49.3%) patients were incidentally diagnosed, with no specific symptoms, and 18 (12.3%) were found to have hepatolithiasis. Sixty-one (41.8%) and two (1.4%) patients underwent concurrent bile duct resection and pancreaticoduodenectomy, respectively, and 130 (89.0%) underwent R0 resection. Low-grade and high-grade intraepithelial neoplasia, and invasive carcinoma were identified in 26 (17.8%), 50 (34.2%), and 70 (47.9%) patients, respectively. Five-year tumor recurrence and patient survival rates were 8.4% and 93.9%, respectively, in patients with high-grade neoplasia; and 41.5% and 72.3%, respectively, in patients with invasive carcinoma. CA19-9 > 37 U/mL and R1 resection were independent risk factors for tumor recurrence and reduced survival in patients with carcinoma. The combination of hypermetabolic fluorodeoxy-glucose-positron emission tomography (FDG-PET) or elevated CA19-9 showed a sensitivity of 91.8% and a specificity of 61.9% for the prediction of IPNB-L with high-grade neoplasia and carcinoma.
Conclusions
IPNB-L is a rare type of intrahepatic biliary neoplasm that can range histologically from benign disease to invasive carcinoma. Surgical curability is the most important prognostic factor, thus aggressive resection is highly recommended to achieve R0 resection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraductal papillary neoplasm of the bile duct (IPNB) is a rare disease, accounting for 4–38% of all bile duct tumors.1,2,3,4 In 2010 and 2019, the World Health Organization classified IPNB as a distinct clinical and pathological entity, being the biliary counterpart of intraductal papillary mucinous neoplasm (IPMN) of the pancreas. 5,6,7,8 IPNB is regarded as precursor to cholangiocarcinoma. Histologically, IPNB can range widely and has been classified as low-grade and high-grade intraepithelial neoplasias, and invasive carcinoma.7 The pathological features of IPNBs also differ markedly and can include various types of intrahepatic and extrahepatic lesions. IPNB should be differentiated from other similar diseases, including intrahepatic and perihilar cholangiocarcinomas, biliary papillomatosis, biliary intraepithelial neoplasia, and mucinous cystic neoplasm. The clinicopathological features of IPNB are different in patients with intrahepatic and extrahepatic IPNBs.7 The present study evaluated the clinicopathological features and long-term outcomes of 146 patients who underwent hepatic resection for intrahepatic IPNBs, also called as IPNB of the liver (IPNB-L).
Materials and Methods
Patient Selection
The primary purpose of this retrospective single-center study was to assess the long-term postoperative outcomes of patients with IPNB-L according to histological grade. The secondary purpose was to identify a preoperative diagnostic method that could distinguish IPNBs with high-grade intraepithelial neoplasia and invasive carcinoma from IPNBs with low-grade intraepithelial neoplasia.
The database of our institution was searched for patients with IPNB-L who underwent hepatic resection between January 2002 and December 2019. Patients with intrahepatic cholangiocarcinoma (ICC) of intraductal tumor growth pattern were excluded, as were patients with extrahepatic IPNB alone and the two patients who died within 2 months of the operation due to non-surgical complications (unexpected cardiovascular and cerebrovascular event in each one patient). Finally, the study group included 146 patients. All patients were followed up until July 2021 or patient death. Institutional medical records were reviewed to determine tumor recurrence and patient survival, with the database of the National Health Insurance Service of Korea reviewed to confirm patient survival.
The study protocol was approved by the Institutional Review Board of our institution (IRB No. 2021–1347), which waived the requirement for informed consent due to the retrospective nature of this study. This study was performed in accordance with the ethical guidelines of the World Medical Association Declaration of Helsinki 2013.
Preoperative Imaging Evaluation
Routine preoperative imaging studies included abdominal and chest computed tomography (CT), liver magnetic resonance imaging (MRI) with magnetic resonance cholangiopancreatography (MRCP), and fluoro-deoxy-glucose-positron emission tomography (FDG-PET). Diagnostic modalities for bile duct evaluation included endoscopic retrograde cholangiopancreatography (ERCP), MRCP, and percutaneous transhepatic cholangioscopy.
Surgical Procedures
The extent of hepatic resection was primarily determined by measuring the post-surgical volume of the liver remnant, with consideration of tumor-free resection margins and hepatic functional reserve. Hepatic resection was classified as anatomical or non-anatomical hepatectomy. Anatomical hepatectomy included resection of one or more adjacent hepatic segments along the hepatic vasculature. Patients having tumors thought to involve the resection margins of the hilar bile duct underwent concurrent bile duct resection (BDR), along with caudate lobectomy.
Histologic Grading
Tissue specimens stained with haematoxylin and eosin were reviewed by pathologists and categorized as IPNB with low-grade or high-grade intraepithelial neoplasia or IPNB with invasive carcinoma, according to the World Health Organization 2019 classification.7 IPNB with low-grade intraepithelial neoplasia was generally regarded as benign IPNBs, whereas IPNB with high-grade intraepithelial neoplasia and invasive carcinoma were classified as malignant IPNBs.
IPNB-L with invasive carcinoma showed various growth patterns, similar to those of ICC, including intraductal-growing, mass-forming, periductal infiltrating, or mixed tumor growth patterns. Although the eight edition of the American Joint Committee on Cancer (AJCC) staging system is valid for all ICCs except for those with intraductal growth pattern,9 the AJCC tumor staging system was applied to all IPNB-L patients with invasive carcinoma regardless of tumor growth pattern.
Postoperative Surveillance and Treatment of Tumor Recurrence
Patients were followed up every 2–4 months during the first year after surgery, depending on pathology and tumor stage; thereafter, the follow-up interval was adjusted on a case-by-case basis. For patients with malignant IPNB-L, the interval between follow-up examinations was set at every 3–4 months for 5 years and thereafter prolonged to every 6–8 months until 10 years. The general principles of treatment of ICC were applied to the patients with IPNB-L with carcinoma.10
Statistical Analysis
Categorical variables were compared by the chi-square test or Fisher’s exact test. Continuous variables were compared by Student’s t-test or analysis of variance, depending on their distribution. Survival curves were estimated by the Kaplan–Meier method and compared by the log-rank test. Cox proportional hazard regression analysis was used to calculate the hazard ratio (HR) and 95% confidence intervals (CIs). A p-value < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 22 (IBM, New York, NY, USA) and MedCalc version 20.010 (Ostend, Belgium).
Results
Demographic Data and Clinical Characteristics
The 146 patients with IPNB-L identified in the present study included 97 (66.4%) men and 49 (33.6%) women. Mean patient age was 64.3 ± 8.0 years (range: 37–83 years). Initial clinical manifestations were abdominal pain or discomfort in 46 (31.5%), gastrointestinal symptoms in 10 (6.9%), fever in nine (6.2%), pruritus and jaundice in nine (6.2%). Another 72 (49.3%) had no specific symptoms and were diagnosed incidentally. Thirteen (8.9%) patients had undergone prior cholecystectomy for gallstone diseases. In addition, 34 (23.3%) were diagnosed with diabetes mellitus and 62 (42.5%) with hypertension. Intrahepatic duct stones were detected in 18 (12.3%) patients at the time of IPNB-L diagnosis, with five (3.4%) and one (0.7%) having a history of hepatitis B and C virus infections, respectively, and three (2.1%) having a history of Clonorchis sinensis. Twelve (8.2%) patients with incidentally detected intraductal masses were followed up by imaging modalities for more than 1 year prior to operation (Supplementary Fig. 1). The median serum concentration of carcinoembryonic antigen (CEA) was 2.0 ng/mL (range: 0.4–178.0 ng/mL); and the median serum concentration of carbohydrate antigen 19–9 (CA19-9) was 12.5 U/mL (range: 0.6–567.9 U/mL). The relationship between serum CA19-9 concentration and histological grade is shown in Fig. 1.
Preoperative Imaging Findings
All patients underwent preoperative radiological examinations, including abdominal ultrasonography, abdominal CT scan, and MRCP; 45 (30.8%) were evaluated by ERCP; 11 (7.5%) were evaluated by percutaneous transhepatic cholangioscopy; and 118 (80.8%) were evaluated by FDG-PET. MRCP was useful for determining the gross sizes of the involved intraductal lesions, enabling the extent of hepatic resection to be determined before surgery. Of the 118 (80.8%) patients evaluated by FDG-PET scanning, 95 (80.5%) showed hypermetabolic FDG uptake (Table 1).
Surgical Procedures and Oncological Curability
All patients underwent hepatic resection with or without concurrent BDR. The extent of liver resection is summarized in Table 2. Sixty-one (41.8%) and two (1.4%) patients underwent concurrent BDR and pancreaticoduodenectomy, respectively, to obtain tumor-free bile duct resection margins. Six (4.1%) patients underwent right hepatectomy after preoperative portal vein embolization. Of the 146 patients, 143 (97.9%) underwent anatomical hepatic resection, with only three (2.1%) undergoing non-anatomical hepatic resection. Resection was curative (R0 resection) in 130 (89.0%) patients (Table 3), with the other 16 (11.0%) patients having tumor-positive resection margins (R1 resection). Sites of tumor-positive resection margins included the distal bile duct or remnant liver hepatic duct in 11 patients who had undergone hepatectomy with BDR, and the hilar bile duct in five patients who had undergone hepatectomy alone (Supplementary Fig. 2).
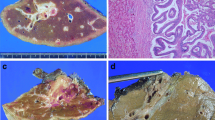
Histopathological Findings
Histologic grading of IPNB-L showed low-grade intraepithelial neoplasia in 26 (17.8%) patients, high-grade intraepithelial neoplasia in 50 (34.2%), and invasive carcinoma in 70 (47.9%), with mean tumor diameters of 3.2 ± 2.8, 4.0 ± 2.3 cm, and 3.0 ± 2.0 cm, respectively (p = 0.013). Mucin pool formation was detected in seven (4.8%) patients, and multiple tumors in 13 (8.9%). The clinicopathological findings according to the histological grades are summarized in Table 1.
Of the 70 IPNB-L patients with invasive carcinoma, 41 (58.6%), 17 (24.3%), and eight (11.4%) had well-, moderately, and poorly differentiated tumors, respectively, with the grade of tumor differentiation being unclassified in four (5.7%) patients due to the nature of microinvasive tumors.
Tumor Recurrence and Patient Survival
Of the 26 patients with low-grade intraepithelial neoplasia followed up for a median 79 months, only one showed tumor recurrence at 94 months. Four of the 50 patients with high-grade intraepithelial neoplasia, all of whom had undergone R0 resection, showed tumor recurrence during a median follow-up period of 48 months. By contrast, of the 70 patients with invasive carcinoma, 32 patients, including seven of the 10 patients who had undergone R1 resection, showed tumor recurrence during a median follow-up period of 47 months (p < 0.001; Fig. 2A).
Two patients in the low-grade intraepithelial neoplasia groups died of causes other than IPNB recurrence after 96 months and 158 months, respectively.
The 1-, 3-, 5-, and 10-year patient survival rates were 100%, 100%, 100% and 88.9%, respectively, in the low-grade intraepithelial neoplasia group; 96.0%, 93.9%, 93.9%, and 82.8%, respectively, in the high-grade intraepithelial neoplasia group; and 100%, 87.0%, 72.3%, and 49.3%, respectively, in the invasive carcinoma group (p = 0.003; Fig. 2B).
Risk Factor Analysis for Postoperative Outcomes
Because only one patient in the low-grade intraepithelial neoplasia group experienced IPNB recurrence and none died of IPNB recurrence-associated causes, this group was excluded from risk factor analysis.
The 1-, 3-, 5-, and 10-year tumor recurrence rates in the high-grade intraepithelial neoplasia group were 2.0%, 4.2%, 8.4%, and 16.8%, respectively (Fig. 2A). Univariate analysis showed that serum CA19-9 > 37 U/mL (p = 0.042) and mucin pool formation (p < 0.001) were significantly associated with tumor recurrence, but neither was significant on multivariate analysis. Only mucin pool formation (p = 0.004) was significantly associated with patient survival on univariate analysis, but not on multivariate analysis (Table 3).
The 1-, 3-, 5-, and 10-year tumor recurrence rates in the carcinoma group were 12.9%, 28.5%, 41.5%, and 54.4%, respectively (Fig. 2A). Univariate analysis revealed that CA19-9 > 37 U/mL (p = 0.033), perineural invasion (p = 0.005), and R1 resection (p = 0.015) were significantly associated with tumor recurrence, with CA19-9 > 37 U/mL (HR = 2.17; p = 0.040) and R1 resection (HR = 2.92; p = 0.016) remaining significantly associated with tumor recurrence on multivariate analysis. Both univariate and multivariate analyses showed that CA19-9 > 37 U/mL (HR = 2.43; p = 0.032) and R1 resection (HR = 4.74; p = 0.001) were significantly associated with patient survival (Table 4).
The median post-recurrence survival period after R0 resection was 30 months, and the median overall patient survival period after R1 resection was 39 months (p = 0.595; Fig. 3), indicating that the prognostic impact of R1 resection was similar to postoperative tumor recurrence.
Preoperative Prediction of Diagnosis of High-grade Intraepithelial Neoplasia and Invasive Carcinoma
Preoperative finding was found unable to differentiate patients with high-grade intraepithelial neoplasia and invasive carcinoma from those with low-grade intraepithelial neoplasia (Table 1). Of the 118 patients who underwent preoperative FDG-PET, 21 (17.8%) had IPNB-L with low-grade intraepithelial neoplasia (benign IPNB-L group) and 97 (82.2%) had IPNB-L with high-grade intraepithelial neoplasia or invasive carcinoma (malignant IPNB-L group).
Hypermetabolic FDG-PET uptake was detected in 8 of the 21 (38.0%) benign IPNB-L lesions and 87 of the 97 (89.7%) of the malignant IPNB-L lesions (p < 0.001). Serum CA19-9 concentration was > 37 U/mL in 3 of 21 (14.7%) patients with benign IPNB-L lesions and 27 of 97 (27.8%) with malignant IPNB-L lesions (p = 0.272). A receiver operating characteristic curve analysis for predicting malignant IPNB-L revealed that a CA19-9 cutoff of 37 U/mL had a sensitivity of 25.8% and a specificity of 90.5%, with area under the curve of 0.604 (p = 0.110; Supplementary Fig. 3).
The combination of hypermetabolic FDG-PET uptake and/or serum CA19-9 > 37 U/mL was detected in 89 of 97 (91.8%) patients with malignant IPNB-L. By contrast, the combination of non-hypermetabolic FDG-PET uptake and serum CA19-9 ≤ 37 U/mL was detected in 13 of 21 (61.9%) patients with benign IPNB-L. The combination of hypermetabolic FDG-PET uptake and/or CA19-9 concentration > 37 U/mL had a sensitivity of 91.8%, a specificity of 61.9%, a positive predictive value of 91.8%, and a negative predictive value of 61.9% for the preoperative prediction of malignant IPNB-L.
Discussion
IPNB, proposed as a new disease entity in 2010 WHO classification,5 has been reported sporadically around the world and shown to be a precursor of invasive carcinoma.1,11,12 The incidence of IPNB is higher in Far East Asian countries than in Western countries.13,14 IPNB accounts for 9.9–30% of bile duct tumors in Asian countries,15,16 compared with 7–11% in Western countries.6,17 Analysis of our institutional database found that IPNB-L accounted for approximately 13% of intrahepatic bile duct tumors undergone hepatic resection.
Accurate preoperative diagnosis of IPNB-L is usually difficult in clinical practice. The most common clinical manifestations observed in patients with IPNB-L in the present study were abdominal pain, acute cholangitis, and obstructive jaundice, although about half of these patients did not present with any specific symptoms. Intrahepatic duct dilatation was the most frequent abnormal finding on preoperative imaging in patients with IPNB-L. Patients lacking an intraductal mass on ultrasonography or CT scan were initially diagnosed with the conditions such as benign biliary stricture, intrahepatic stone or clonorchiasis. ERCP is useful in diagnosis of IPNB-L, with characteristic findings including multiple filling defects and serrated irregularities of the bile duct walls. However, copious mucin production hinders opacification of the entire biliary tract, especially within the intrahepatic bile ducts, resulting in suboptimal evaluation of the tumor extent.18 MRCP appears to be the most useful imaging modality to delineate the actual extents of IPNB-L.19 Therefore, patients in our center have routinely undergone MRCP for evaluation of nearly all liver tumors involving the intrahepatic bile ducts.
The extent of IPNB varies widely, resulting in various classifications.20,21,22,23 For example, a Korean multi-center study proposed that IPNB could be radiologically classified into three types.23 In the extrahepatic type, the main lesions are confined to the common bile duct and common hepatic duct. Patients with this type were intentionally excluded from the present study because this type is not regarded as IPNB-L. In the intrahepatic type, the main lesions are located at the periphery beyond the first confluence of the intrahepatic duct. Most patients in the present study had this type. In the diffuse type, the main lesions are located throughout the intrahepatic and extrahepatic ducts. A small number of patients in the present study who had undergone hepatectomy with BDR might be classified as this type of lesion. In practice, it is difficult to define radiological types based solely on imaging findings, not only because the morphology and extent of dilated bile ducts are highly variable, but also because the microscopic extent of mucosal lesions is much wider than their macroscopic extent, as determined by gross findings.
Of the IPNB-L lesion in the present study, 82.2% were regarded to be malignant, whereas only 17.8% were considered to be benign. IPNBs that differ in malignant potential can be ultimately diagnosed as low-grade or high-grade intraepithelial neoplasia, or invasive carcinomas,7 indicating that the spectrum of IPNB represents a continuum of intraductal neoplastic progression along the adenoma–carcinoma sequence. Thus, IPNB-L should not be regarded as a benign disease with malignant potential but as a premalignant lesion with high malignant potential.24
In practice, it is difficult to differentiate benign from malignant IPNB-L based on morphological imaging using CT and MRI. Of the benign and malignant IPNB-L groups in the present study, 38.0% and 89.7%, respectively, showed hypermetabolic FDG-PET uptake. High expression of serum CA19-9 was closely associated with malignant IPNB-L. The combination of hypermetabolic FDG-PET uptake and/or CA19-9 > 37 U/mL showed a sensitivity of 91.8%, a specificity of 61.9%, a positive predictive value of 91.8%, and a negative predictive value of 61.9% in the prediction of malignant IPNB-L. A Japanese study reported that maximum standardized uptake values (SUVmax) of FDG-PET were significantly higher in patients with invasive IPNB and papillary ICC than in patients with non-invasive IPNB.25 Based on the diagnostic importance of FDG-PET, nearly all patients with liver mass in our center have been routinely evaluated by FDG-PET during the past 10 years. However, in the present study, we did not provide FDG-PET SUVmax to define whether to be hypermetabolic or not because the reports of FDG-PET taken before year 2010 provided only simple description on hypermetabolic uptake instead of SUVmax. Our additional retrospective analysis revealed that the cutoff values of SUVmax for diagnosing hypermetabolic uptake in IPNB-L were greater than 3.0 (unpublished data).
The post-resection prognosis has been reported better in patients having IPNB-L with invasive carcinoma than in those with usual ICC.3,24,26 The results of the present study found that the 5-year tumor recurrence rate was 41.5%, and the 5-year patient survival rate was 72.3%.
The carcinogenesis mechanism of IPNB is still poorly characterized. An European multicenter study assessed common oncogenic pathways.27 Molecular and immunohistochemical analysis revealed mutated KRAS, overexpression of TP53 and loss of p16 in low-grade intraepithelial neoplasia, whereas loss of SMAD4 was found in late phases of tumor development. Alterations of HER2, EGFR, β-catenin and GNAS were rare events. Patients with IPNB showed a slightly better overall survival than patients with cholangiocarcinoma. The development of IPNB follows an adenoma-carcinoma sequence that correlates with the stepwise activation of common oncogenic pathways.27 These mechanisms may be associated less aggressive tumor biology of IPNB-L, compared with ICC.
High serum concentration of CA19-9 and R1 resection were independent risk factors for both tumor recurrence and reduced patient survival. Furthermore, the median post-recurrence survival period after R0 resection was found to be 30 months, whereas the median overall patient survival period after R1 resection was 39 months. The major components of tumor staging, such as tumor size and number, were not significant prognostic factors in the present study. These findings suggest that the tumor biology of IPNB-L with invasive carcinoma is similar to that of ICC with intraductal tumor growth, being less invasive than usual ICC. Therefore, surgical R0 resection is highly recommended as the first-choice treatment for patients with IPNB-L without distant metastasis. Five patients in the present study who underwent hepatectomy alone had tumor-positive hilar bile duct margins. Had these patients undergone concurrent BDR, the likelihood of achieving R0 resection would likely have increased. Even if concurrent BDR does not guarantee R0 resection, we still recommend performing concurrent BDR because tumor progression at the level of the proximal bile duct is often intractable. Additional caudate lobectomy during BDR, along with hepatectomy to remove the primary tumor, helps to secure tumor-free bile duct resection margins, as in resection for perihilar cholangiocarcinoma. Two patients in the present study underwent concurrent pancreaticoduodenectomy to achieve R0 resection because the distal bile duct resection margins were repeatedly tumor-positive on frozen-section biopsies even after deep excavation of the intrapancreatic bile duct.28
Regional lymphadenectomy is an important component of surgical procedures for malignant IPNB-L, as for ICC. In the present study, only 8.6% of IPNB-L patients with carcinoma were positive for lymph node metastasis. This relatively low proportion may be attributed to the less aggressive biological behavior of IPNB-L with invasive carcinoma and partially to the lack of sufficient lymph node sampling. The absence of enlarged lymph nodes at the hepatoduodenal ligament and celiac axis may be responsible for the lack of sufficient lymph node sampling. Nevertheless, to avoid tumor under-staging, patients with IPNB-L should routinely undergo extensive lymph node dissection, similar to patients with ICC.29,30 This is especially necessary for IPNB-L patients with hypermetabolic uptake on FDG-PET and/or high serum concentration of CA19-9, such that the extent of lymph node dissection in these patients should be the same as for usual ICC.
The present study had several limitations, including a retrospective design and inclusion of data from a single center. Long-term tumor recurrence could not be fully assessed because some patients were lost to follow-up. However, their survival outcomes could be determined completely, based on data collected through the national health insurance database in Korea. In addition, this study only included patients with IPNB-L; thus, patients with extrahepatic IPNB were not assessed. FDG-PET SUVmax was not available in a considerable number of patients, thus a cutoff value for diagnosing hypermetabolic uptake was not calculated. The tumor size was based on the pathology reports, thus the sizes of the IPNB and invasive carcinoma portions were not assessed separately.
In conclusion, IPNB-L is a rare type of biliary neoplasm that can range histologically from benign disease to invasive carcinoma. Surgical curability is the most important prognostic factor, thus aggressive surgery should be performed to achieve R0 resection.
Data availability
Data available on request due to privacy/ethical restrictions.
References
Nakanuma Y, Sato Y, Harada K, Sasaki M, Xu J, Ikeda H. Pathological classification of intrahepatic cholangiocarcinoma based on a new concept. World J Hepatol 2010;2:419–427.
Jang KT, Hong SM, Lee KT, Lee JG, Choi SH, Heo JS, et al. Intraductal papillary neoplasm of the bile duct associated with Clonorchis sinensis infection. Virchows Arch 2008;453:589–598.
Itatsu K, Zen Y, Ohira S, Ishikawa A, Sato Y, Harada K, et al. Immunohistochemical analysis of the progression of flat and papillary preneoplastic lesions in intrahepatic cholangiocarcinogenesis in hepatolithiasis. Liver Int 2007;27:1174–1184.
Zen Y, Fujii T, Itatsu K, Nakamura K, Minato H, Kasashima S, et al. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology 2006;44:1333–1343.
Nakanuma Y. A novel approach to biliary tract pathology based on similarities to pancreatic counterparts: is the biliary tract an incomplete pancreas? Pathol Int 2010;60:419–429.
Rocha FG, Lee H, Katabi N, DeMatteo RP, Fong Y, D'Angelica MI, et al. Intraductal papillary neoplasm of the bile duct: a biliary equivalent to intraductal papillary mucinous neoplasm of the pancreas? Hepatology 2012;56:1352–1360.
WHO Classification of Tumours Editorial Board. WHO classification of tumours, digestive system tumours. 5th ed. International Agency for Research on Cancer; Lyon, France: 2019. pp. 279–282.
Jung G, Park KM, Lee SS, Yu E, Hong SM, Kim J. Long-term clinical outcome of the surgically resected intraductal papillary neoplasm of the bile duct. J Hepatol 2012;57:787–793.
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK, Washington MK, et al. eds. AJCC cancer staging manual. 8th ed. New York: Springer; 2017.
Hwang S, Lee YJ, Song GW, Park KM, Kim KH, Ahn CS, et al. Prognostic impact of tumor growth type on 7th AJCC staging system for intrahepatic cholangiocarcinoma: a single-center experience of 659 cases. J Gastrointest Surg 2015;19:1291–1304.
Wu SD, Lu CD, Lu CJ, Huang J, Zhou J. Mucin-producing intrahepatic biliary papillomatosis. Surg Today 2010;40:845–850.
Nakanuma Y, Zen Y, Harada K, Ikeda H, Sato Y, Uehara T, et al. Tumorigenesis and phenotypic characteristics of mucin-producing bile duct tumors: an immunohistochemical approach. J Hepatobiliary Pancreat Sci 2010;17:211–222.
Wan XS, Xu YY, Qian JY, Yang XB, Wang AQ, He L, et al. Intraductal papillary neoplasm of the bile duct. World J Gastroenterol 2013;19:8598–604.
Park HJ, Kim SY, Kim HJ, Lee SS, Hong GS, Byun JH, et al. Intraductal papillary neoplasm of the bile duct: clinical, imaging, and pathologic features. Am J Roentgenol 2018;211:67–75.
Yeh CN, Jan YY, Yeh TS, Hwang TL, Chen MF. Hepatic resection of the intraductal papillary type of peripheral cholangiocarcinoma. Ann Surg Oncol 2004;11:606–611.
Onoe S, Shimoyama Y, Ebata T, Yokoyama Y, Igami T, Sugawara G, et al. Prognostic delineation of papillary cholangiocarcinoma based on the invasive proportion: a single-institution study with 184 patients. Surgery 2014;155:280–291.
Barton JG, Barrett DA, Maricevich MA, Schnelldorfer T, Wood CM, Smyrk TC, et al. Intraductal papillary mucinous neoplasm of the biliary tract: a real disease? HPB (Oxford) 2009;11:684–691.
Yang J, Wang W, Yan L. The clinicopathological features of intraductal papillary neoplasms of the bile duct in a Chinese population. Dig Liver Dis 2012;44:251–256
Lee S, Kim MJ, Kim S, Choi D, Jang KT, Park YN. Intraductal papillary neoplasm of the bile duct: assessment of invasive carcinoma and long-term outcomes using MRI. J Hepatol 2019;70:692–699.
Kim JR, Jang KT, Jang JY, Lee K, Kim JH, Kim H, et al. Clinicopathologic analysis of intraductal papillary neoplasm of bile duct: Korean multicenter cohort study. HPB (Oxford) 2020;22:1139–1148.
Kubota K, Jang JY, Nakanuma Y, Jang KT, Haruyama Y, Fukushima N, et al. Clinicopathological characteristics of intraductal papillary neoplasm of the bile duct: a Japan-Korea collaborative study. J Hepatobiliary Pancreat Sci 2020;27:581–597.
Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci 2014;21:176–185.
Kim JR, Lee KB, Kwon W, Kim E, Kim SW, Jang JY. Comparison of the clinicopathologic characteristics of intraductal papillary neoplasm of the bile duct according to morphological and anatomical classifications. J Korean Med Sci 2018;33:e266.
Kim WJ, Hwang S, Lee YJ, Kim KH, Park KM, Ahn CS, et al. Clinicopathological features and long-term outcomes of intraductal papillary neoplasms of the intrahepatic bile duct. J Gastrointest Surg 2016;20:1368–1375.
Ikeno Y, Seo S, Yamamoto G, Nakamoto Y, Uemoto Y, Fuji H, et al. Usefulness of preoperative (18)F-FDG-PET in detecting invasive intraductal papillary neoplasm of the bile duct. Anticancer Res 2018;38:3677–3682.
Nakanuma Y, Sato Y, Ojima H, Kanai Y, Aishima S, Yamamoto M, et al; Hepatolithiasis Subdivision of Intractable Hepatobiliary Diseases Study Group of Japan. Clinicopathological characterization of so-called "cholangiocarcinoma with intraductal papillary growth" with respect to "intraductal papillary neoplasm of bile duct (IPNB)". Int J Clin Exp Pathol 2014;7:3112–3122.
Schlitter AM, Born D, Bettstetter M, Specht K, Kim-Fuchs C, Riener M, et al. Intraductal papillary neoplasms of the bile duct: stepwise progression to carcinoma involves common molecular pathways. Mod Pathol 2014;27:73–86.
Lee SJ, Hwang S, Ha TY, Kim KH, Ahn CS, Moon DB, et al. Technical knacks and outcomes of extended extrahepatic bile duct resection in patients with mid bile duct cancer. Korean J Hepatobiliary Pancreat Surg 2013;17:109–112.
Ruzzenente A, Conci S, Viganò L, Ercolani G, Manfreda S, Bagante F, et al. Role of lymph node dissection in small (≤ 3 cm) intrahepatic cholangiocarcinoma. J Gastrointest Surg 2019;23:1122–1129.
Morine Y, Shimada M. The value of systematic lymph node dissection for intrahepatic cholangiocarcinoma from the viewpoint of liver lymphatics. J Gastroenterol 2015;50:913–927.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: SH.
(II) Administrative support: SH.
(III) Provision of study materials or patients: CSA, DBM, TYH.
(IV) Collection and assembly of data: GSW, DHJ, SMH.
(V) Data analysis and interpretation: JMY, SH.
(VI) Manuscript writing – 1st: SH, JMY.
(VII) Manuscript writing—revision: All authors.
(VIII) Final approval of manuscript: All authors.
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Youn, J.M., Hwang, S., Ahn, CS. et al. Clinicopathological Features and Long-Term Outcomes of Intraductal Papillary Neoplasms of the Bile Duct of the Liver: Single-Institution Experience with 146 Patients. J Gastrointest Surg 26, 1394–1405 (2022). https://doi.org/10.1007/s11605-022-05268-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05268-2