Abstract
Objective
Distal pancreatectomy (DP) remains associated with significant morbidity, but little data is available about the clinical significance of drain contamination. We explored the incidence, risk factors, and association with surgical outcomes of positive drainage culture (PDC) after DP. In addition, the predictive capacity of early PDC for postoperative pancreatic fistula (POPF) was evaluated.
Methods
We retrospectively analyzed our prospectively collected database of patients who underwent DP between January 2005 and December 2015. Surveillance drainage cultures for microorganisms were conducted until drain removal or positive culture. The relationships between clinical variables and PDC were examined.
Results
Of 480 consecutive cases who underwent DP, 176 (36.7%) had PDC. One hundred twelve patients (23.3%) developed POPF according to the 2016 ISGPS definition, with the 90-day mortality rate of 0.2%. Staphylococcus spp. was the most frequent isolate. Thirty-eight (21.6%) patients had PDC within 3 days after surgery, and 129 (73.3%) within the first 7 days of operation. Body mass index (BMI) ≥ 25 kg/m2 and massive intraoperative blood loss were independent predictors for PDC. PDC had a negative impact on surgical outcomes, including POPF. Early PDC was identified as a newly independent risk factor for POPF. Compared with other microorganisms, those contaminated with Staphylococcus and Klebsiella had higher incidences of POPF.
Conclusions
PDC occurs commonly after DP and plays a critical role in the development of surgical morbidities including POPF. Extreme caution is warranted in patients involving contamination with specific types of microorganisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Distal pancreatectomy (DP) is a frequent intervention to treat various neoplastic diseases involving the pancreatic body and tail. The mortality rate after DP has decreased to as low as zero to 7.3%.1, 2 However, the morbidity rate remains high, ranging from 36.5 to 50.1% over the past decades,3,4 despite improvements in surgical techniques and perioperative management strategies. Postoperative pancreatic fistula (POPF) occurs more frequently after DP compared with pancreaticoduodenectomy (PD).4,5 Clinically relevant (CR) POPF (grade B/C), which has been reported to occur in 14.8–27.7% of patients, is the most challenging complication after DP.6,7 It has been demonstrated to be associated with several fatal complications, such as intra-abdominal abscess, hemorrhage, and sepsis, which can prolong the length of hospital stay and increase hospitalization costs. Infectious complications, mainly infected POPF, which occurred in one-quarter of patients received DP, have been shown a negative impact on surgical outcomes.4
With regard to DP, opinions differ as to the risk of POPF developing when routine drainage is used. Traditionally, it is thought that drains could help controlled evacuation of pancreatic secretions when leaks occur and early recognition of POPF or hemorrhage, thereby decreasing potential complications.3 Although prevalence of infection in abdominal discharge was frequent postoperatively, prophylactic intraperitoneal drains in DP could be effective for reducing fistula severity and preventing POPF from developing into lethal complications.8, 9 A recent prospective randomized trial comparing DP with and without intraperitoneal drainage showed that clinical outcomes were comparable between the two groups.6 However, several studies claimed that routine intraperitoneal drain placement was associated with a higher incidence of POPF following DP.3,8,10 Furthermore, delayed drain removal could promote the development of POPF.11 Our previous study demonstrated that positive drainage culture (PDC) was associated with postoperative complications, including POPF, hemorrhage, intra-abdominal abscess, major complications, and re-operation after PD.12 However, thus far, the relationship between PDC and postoperative complications after DP remains unclear.
Many factors such as age, obesity, hypoalbuminemia, intra-operative amylase concentration, and drain fluid amylase on postoperative day 1 (POD1) have been shown to be associated with the occurrence of POPF after DP.8,13,14,15 More recently, several studies showed that bacterial contamination of drain fluid induced the development of POPF after PD.16,17,18,19 However, there are no data available regarding the predictive value of early positive bacterial culture from drain fluid (POD1 to POD3) for POPF after DP. Therefore, this study was conducted to investigate the relationship between PDC and postoperative complications following DP; furthermore, we evaluated the predictive capacity of early bacterial contamination in abdominal discharge for the development of POPF.
Methods
A single-center retrospective analysis using prospectively collected data of consecutive cases of DP performed for benign or malignant tumors of the pancreatic body and tail at our institution between January 2005 and December 2015 was conducted. Eligible patients who underwent elective DP performed by pancreatic surgical specialists were enrolled in this study. The study was approved by the ethics committee of our institution.
Perioperative Management
The perioperative management has been described in a previous study.12 The difference is that pancreatic stump was closed using handsewn method (with or without suture ligation of the main pancreatic duct) or triple-row stapler without reinforcement. In cases of stapled closure, the closed pancreatic duct was oversewn as far as possible using 4–0 absorbable suture.20 Neither tissue patches nor biologic sealants for the pancreatic stump were employed during our operation. Two closed suction drains were placed along the superior and inferior borders of the pancreatic stump positioning in the bed of the resected pancreas near the transected margin. Another drain may be placed in the left subphrenic space from the left upper abdomen according to whether splenectomy had been performed (Supplementary Fig. 1).
Antibiotic prophylaxis consisting of cephalosporins (such as cephazolin, cefotiam, cefoxitin, and cefuroxime) was intravenously administered 30 min before skin incision, then redosed every 4 h until the end of the surgery. An additional short-term antibiotic course was used for about 3 days postoperatively. Whenever a patient had infectious complications, antibiotic treatment was started empirically (vancomycin for suspected gram-positive infection, carbapenems, and quinolones for suspected gram-negative infection)12 and adjusted according to the antimicrobiologic susceptibility results. Antibiotics were discontinued after confirmation of no symptoms of infection, and decrease of the patient’s serum inflammatory indicators including white blood cell count, C-reactive protein, and procalcitonin. Somatostatin anologues were used for prevention of POPF postoperatively. Blood glucose was routinely measured 3 to 4 times a day, and if high, insulin was subcutaneously administered with a target level set in the range of 110 to 150 mg/dl. Measurement of amylase level in the drain fluid was performed daily from POD1 to POD5, and then every other day until drains removed or patient discharged. Drain fluid culture for aerobic/anaerobic microorganisms was started on POD1 to POD3, and every 2 to 3 days thereafter until drains removed or positive cultured. Drains were removed when the drain fluid amylase value was less than 3 times the upper limit of the normal serum level (about 600 U/L) with imaging studies showing no peri-pancreatic fluid collection.
Data Collection and Definition of Variables
Clinicopathologic factors collected for data analysis included gender, age, body mass index (BMI), smoking history, preoperative comorbidity, American Society of Anesthesiologists (ASA) score, preoperative blood biochemical test results, preoperative chemoradiation, estimated intraoperative blood loss and transfusion, surgical procedure, operation time, vessel resection, pathological diagnosis, postoperative serum and drain amylase levels, and complications and results of drainage culture (including the date).
Both the 2005 International Study Group for Pancreatic Fistula (ISGPF) and 2016 International Study Group on Pancreatic Surgery (ISGPS) definition and grading system of POPF were used to define POPF.21,22 The definitions and grading systems of the ISGPS were used for other complications such as delayed gastric emptying (DGE) and postpancreatectomy hemorrhage (PPH).23,24 Intra-abdominal abscess was defined as intra-abdominal fluid collection with positive cultures detected by computed tomography or ultrasonography. The severity of surgical morbidity was graded according to the Clavien-Dindo classification.25,26 Complications of grade ≥ III were considered as major.27 The 90-day mortality was defined as any death that occurred in hospital or within 90 days of DP.4 Readmission was defined as admission to our hospital within 30 and 90 days of discharge home after surgery. Those who were readmitted more than once within the periods were counted only once.28
Statistical Analysis
Data were described as frequencies (percentages of population) and median (interquartile range). The Pearson Chi-square, Fisher’s exact, and Mann-Whitney U tests were used to identify univariate associations between baseline characteristics and outcome measures. Variables with a P value less than 0.05 were included in multiple logistic regression models. The optimal discriminator value for continuous variable was determined by the receiver operating characteristic (ROC) curve analysis. The optimal cut-off value was assessed using the Youden index.29 To display cumulative incidence of PDC after DP over time, Kaplan-Meier estimates of the time to first event were created and compared by the log-rank tests. All statistical analyses were performed using the SPSS Version 24.0 (SPSS Inc., Chicago, IL, USA), and P < 0.05 was considered statistically significant.
Results
Patient Characteristics and Perioperative Outcomes
Four hundred eighty patients ranged in age from 18 to 86 years (median 58 years) were included. There were 231 (48.1%) men and 249 (51.9%) women. Pancreatic carcinoma occurred in 211 (44.0%) patients. Among 266 (55.4%) patients with malignant disease, 11 (2.3%) had vessel resection. Eighty (16.7%) patients received spleen preserving DP. The mean operation time was 3.4 ± 1.2 h, and intra-operative red blood cell transfusion was needed in 125 (26.0%) patients. Major complications occurred in 27 (5.6%) patients, and a total of 112 patients (23.3%) developed POPF according to the 2016 ISGPS definition. When comparing with the 2005 scheme, grade B POPF increased from 21.3 to 22.3%, while grade C decreased from 2.1 to 1%. Figure 1 shows the POPF rates according to the 2005 ISGPF and 2016 ISGPS classifications and their distribution in terms of grade severity. The 90-day mortality was 0.2%, with re-operation rate of 2.5%. The median length of postoperative hospital stay was 11 days, with 30- and 90-day non-plan readmission rates of 5.8% and 6.9%, respectively.
Incidence, Bacteriology, and Time of PDC
Of the 480 patients, 176 (36.7%) had PDC during the postoperative period. Among them, a total of 259 isolates were yielded. A total of 106 (40.9%) were gram-positive bacteria, 143 (55.2%) gram-negative, and 10 (3.9%) fungi. The proportion of gram-positive to gram-negative cultures did not change over time (P = 0.249 for Period2005–2010 vs Period2011–2015). Distribution of isolated microorganisms is shown in Fig. 2 a. Staphylococcus spp. (29%) was the most frequent isolate, followed by acinetobacter spp. (19%) and pseudomonas spp. (13%). A total of 66 (37.5%) cases had poly-microbial infection. Gram-positive bacteria were found in 90 (51.1%) of 176 patients, gram-negative bacteria in 107 (60.8%), and fungi in 10 (5.7%) (Fig. 2 b). The cumulative rate of PDC was 100% versus 17.4% for those with and without 2016 POPF (P < 0.0001 by log-rank test). Thirty-eight (21.6%) patients developed PDC within 3 days after surgery, and 129 (73.3%) within the first 7 days of operation (Fig. 2 c).
Risk Factors for PDC
Four preoperative and intra-operative variables were shown to be associated with PDC by univariate analysis (Table 1). Patients with BMI ≥ 25 kg/m2, having combined colectomy, massive intraoperative blood loss (≥ 550 ml), or prolonged operation (≥ 5.5 h) had a greater frequency of PDC than those without. Multivariate analysis revealed that BMI ≥ 25 kg/m2 and massive intraoperative blood loss were independent predictors for PDC.
Impact of PDC on Surgical Outcomes
Patients with PDC had significantly higher incidences of overall morbidity, POPF, intra-abdominal abscess, major complications and reoperation, and subsequently longer hospital stays than those with negative drainage culture. However, PDC was not associated with incidences of DGE, PPH, mortality, and readmission (Table 2).
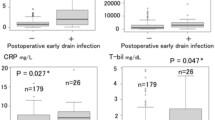
Association Between Early PDC and POPF
We hypothesized that bacteria from drain fluid during the early postoperative period might trigger the development of POPF after DP. To examine whether early detected bacteria were associated with POPF, we performed a separate analysis, in which PDC were stratified according to day of positive culture (early, ≤ 3 days vs late, > 3 days). Interestingly, late PDC had no significantly higher rates of complications than early PDC (all P > 0.05, Table 3), which suggested that the impact of PDC on postoperative complications including POPF was also significantly contributed by early bacterial contamination of drain fluid. Patients who developed POPF after DP often had higher BMI, and greater incidences of massive intraoperative blood loss and prolonged operation. Patients received combined colectomy had greater risks of POPF, while those with malignant disease had significantly fewer POPF. On the other hand, early PDC was significantly associated with POPF (P < 0.0001). Multivariable logistic regression revealed that BMI ≥ 25 kg/m2, benign disease, prolonged operation, and early PDC (odds ratio [OR] 5.300, 95% confidence interval [CI] 2.605 to 10.786) were independent predictors for POPF (Table 4).
Relationship Between Types of Microorganisms and 2016 POPF
The relationship between types of microorganisms and 2016 POPF was investigated. Among the total cohort, contamination with either gram-positive or gram-negative bacteria significantly correlated with POPF. Polymicrobial contamination also contributed to the occurrence of POPF. In addition, Staphylococcus, Enterococcus, Pseudomonas, Acinetobacter, Stenotrophomonas, E. coli, Klebsiella spp., and fungi were isolated significantly more frequently in patients with POPF. In a separate analysis restricted to those with PDC, contamination with gram-positive bacteria occurred significantly more often in the POPF group. Nevertheless, only Staphylococcus and Klebsiella were isolated more frequently in those with POPF (Table 5). These results indicate that specific types of microorganisms play critical roles in the development of POPF after DP.
Discussion
The incidence of infectious complications after DP has been revealed to be around 25%,4,30 most of which involved infected POPF. Although the mechanism is unclear, drain fluid microbial contamination is considered to play a potential role in turning an “innocent” leak into a POPF.31 Marchegiani et al.31 reported that the rate of drain fluid contamination after DP was 21.8%; however, they only conducted the microbiologic analysis on POD5. The positive rate of drain fluid culture in our series was 36.7%, which was similar to that after PD.12 The rate of PDC increased rapidly between POD3 and POD7, indicating a correlation between delayed drain removal and significant increase in PDC.
Consistent with previous reports,4,31 the present and our previous studies revealed that Staphylococcus spp. was isolated more frequently from intraperitoneal drainage after DP than PD.12 This indicated that the risk profile in terms of drain fluid contamination following DP was a little different from that following PD.4,30,31 PD is a relatively complex surgical procedure that involves biliary and enteric reconstructions, thus gut-derived bacteria are isolated predominantly after this operation. However, DP has no intestinal reconstruction. The high incidence of microorganisms from skin and mucous membranes indicates that development of drain fluid contamination after DP involves retrograde migration of bacteria along the drains.31 Taken together, this study support the current two “best practices” in pancreatic surgery—namely selective drain placement and early drain removal.
Many risk factors including prolonged surgery time, chronic steroid use, smoking, non-laparoscopic surgery, and blood transfusion have been reported for infectious complications after DP.4,30 However, up till now there have been no studies about risk factors for drain fluid contamination following DP, while this issue has been analyzed in PD.12,18,19 The present study demonstrated that BMI ≥ 25 kg/m2 and massive intraoperative blood loss were independent risk factors for PDC. Being aware of these factors could be useful for improved perioperative management, thus reducing the PDC rate. Recently, many studies have focused on concomitant colectomy in patients underwent DP.32,33 Although colectomy did not significantly correlate with PDC in our multivariate analysis, it is evident that colectomy increases the incidence of surgical morbidity and mortality. Hence, patients requiring combined colectomy should be well-planned preoperatively, maximally optimized, and referred to highly experienced team at specialty centers.
Several reports have shown that PDC was an independent risk factor for the occurrence of CR-POPF after PD.12,18,19 However, there are no data available regarding the effect of PDC on the development of postoperative complications following DP. The present study showed that PDC had a negative impact on surgical outcomes after DP, including not only POPF, but also other complications such as intra-abdominal abscess, major complications, and reoperation. These results indicate that drain fluid culture has an important clinical significance for prediction of postoperative complications after DP. The incidence of POPF after DP has been reported to be higher than that after PD,4,5 while the reason remains unknown. Considering that PDC correlates with POPF, we believe that the occurrence of PDC is one of the reasons leading to such high rates of POPF after DP. It is worth mentioning that patients with negative culture in our series had no incidence of CR-POPF. This result was in line with a most recent report from University of Heidelberg,34 which showed that sterile POPF occurred in less than 5% of patients underwent DP.
Although PDC following DP was shown to be correlated with worse outcomes, this finding is stuck in the rut of a “chicken or egg” conundrum. Is the presence of bacterial infection a driver of the problem or a reflection of it? We set out to clarify this issue by comparing the surgical outcomes between early and late PDC. Surprisingly, there were no significant differences between them, which indicated that early PDC also played a critical role in the development of POPF. Sometimes, it is difficult to determine whether the organisms cultured from drain fluid are pathogenic or simply contaminants. However, patients with positive bacterial culture of drain fluid are very few likely to be infectious in the early postoperative period. Therefore, the onset of POPF may be triggered by early bacterial contamination, and microbial culture during the early postoperative period is important to predict POPF.
Unlike PD, Soft Gland Texture and Small Pancreatic Duct Are Not Risk Factors for POPF Following DP35
Various factors including age, obesity, hypoalbuminemia, underlying disease, and intraoperative drainage have been shown to be associated with POPF after DP in previous reports8,13,14,15; however, no studies have evaluated the association between bacterial contamination of drain fluid and POPF. In this study, BMI ≥ 25 kg/m2, benign disease, prolonged operation, and early PDC were revealed as independent predictors of POPF after DP in multivariate analysis. To our knowledge, early PDC was identified as a newly independent risk factor for POPF after DP for the first time. Sugiura and coworkers17 showed that intraoperative bacterial contamination correlated with the development of CR-POPF following PD. These interesting findings make us want to know how early intraperitoneal bacterial contamination promotes the formation of POPF. Yamashita et al.18,36 demonstrated that Pseudomonas aeruginosa isolated from drain fluid could activate trypsinogen, resulting in significantly higher rate of CR-POPF than other bacteria. Although the mechanisms are worthy of further investigation, it can be considered that the coexistence of early bacterial contamination and leakage of pancreatic juice after DP is an initiating event in the development of POPF. The reason why we did not examine the value of late PDC to predict POPF is that late PDC is more likely to be a sequence of POPF, but not a risk factor.
What specific types of microorganisms cause POPF after DP has not been addressed in previous studies, we identified several types of bacteria related to POPF. The findings are important for the prevention of complications caused by these bacteria, and for the improvement of patient outcomes. When compared with other bacteria, Staphylococcus and Klebsiella spp. were found to be more closely related to POPF after DP. Staphylococcus spp. was the most commonly isolated microorganisms in drain fluid from our patients. Of these patients, 74.2% progressed to POPF. The high frequency of Staphylococcus cultured from intraperitoneal drainage suggests that retrograde migration of bacteria occur along the drains no matter how industrious to use an aseptic technique for drain care.4,12 Although Klebsiella spp. was isolated in only 2.9% of our cases, 92.9% of them progressed to POPFs. Klebsiella pneumoniae has been reported to able to cause acute obstructive suppurative pancreatic ductitis in intraductal papillary mucinous carcinoma, which in turn led to pancreatobiliary fistula formation37. Rogers and colleagues38 considered that POPF could involve Klebsiella generated cross-reactive antibodies that result in collagen degradation.
To our knowledge, this is the first report to evaluate the association between bacterial contamination in drain fluid and surgical complications after DP, providing positive findings. However, although drain fluid culture is non-invasive and convenient, it may not become a routine test as its evaluation of infection may be unreliable. Furthermore, routine drainage culture is expensive and may not be cost-effective. We are unable to draw an appropriate strategy for the use of drain fluid culture, but whether antibiotic prophylaxis based on the microorganisms isolated from surveillance drainage cultures could positively influence surgical outcomes is worthy for further research. Postoperative antibiotic therapy in the present study may be a deviation from many surgeons’ practice. However, until now there have been no studies evaluating the effect of extended administration of antibiotics on infectious complications after DP. A dose-dependent correlation between antibiotic administration and incisional surgical site infection has been identified39. Prophylactic antibiotics given for 3 days perioperatively, which was applied as a standard clinical practice after DP in a study from Japan11, has been shown to decrease the rate of methicillin-resistant Staphylococcus aureus isolated from postoperative infection sites, compared with antibiotics given within 1 day of surgery40. Considering that Staphylococcus was the most frequent isolate in our study, whether antibiotic administration for 3 days is more conducive to the reduction of PDC remains to be verified. Furthermore, studies are needed to evaluate the effect of preoperative chlorhexidine bathing on the theoretical drain migration of bacteria, as this measure is recommended to prevent surgical site infection41. Someone may argue the generalizability of our data due to the routine use of somatostatin analogues, which is not the case in the USA or elsewhere. However, although no randomized trial has reported the efficacy of prophylactic octreotide for DP, this strategy did not reduce the rate of POPF8, which significantly correlated with PDC in this study. Thus, we believe that the use of somatostatin analogues does not impact our results.
The main limitations of this study include the retrospective nature and a single-center study. Both of them are potential sources of bias. We routinely placed intra-abdominal drains at the time of DP, which may be considered not the optimal strategy. Nevertheless, management of drainage after this procedure still has no definitive evidence-based recommendations. Anyway, external validation is required in the future to confirm our results. Additionally, we only used closed suction drains (CSD) instead of open passive drains (OPD) in our clinical practice. The lack of OPD makes us wonder whether the results are applicable to patients managed using OPD. Recently, Marchegiani et al.31 showed that postoperative outcomes and spectrum of bacterial contamination were similar between CSD and OPD after major pancreatectomy. Therefore, the drain type may not affect our results.
In conclusion, bacterial contamination of intraperitoneal discharge occurs commonly after DP and plays a critical role in the development of surgical morbidities including POPF. Delayed drain removal increases the risk of retrograde migration of bacteria. Hence, early drain removal seems appropriate and may mitigate potential complications of drain placement in selected patients. Many risk factors of POPF following DP exist objectively, and only perioperative management and surgical techniques are changeable. Considering the correlation between early PDC and POPF, prophylactic control of intraperitoneal bacterial contamination is very important for outcome improvement.
References
Kawai M, Hirono S, Okada K, Sho M, Nakajima Y, Eguchi H, Nagano H, Ikoma H, Morimura R, Takeda Y, Nakahira S, Suzumura K, Fujimoto J, Yamaue H. Randomized Controlled Trial of Pancreaticojejunostomy versus Stapler Closure of the Pancreatic Stump During Distal Pancreatectomy to Reduce Pancreatic Fistula. Ann Surg. 2016;264(1):180–7.
Nimptsch U, Krautz C, Weber GF, Mansky T, Grützmann R. Nationwide In-hospital Mortality Following Pancreatic Surgery in Germany is Higher than Anticipated. Ann Surg. 2016;264(6):1082–1090.
Behrman SW, Zarzaur BL, Parmar A, Riall TS, Hall BL, Pitt HA. Routine drainage of the operative bed following elective distal pancreatectomy does not reduce the occurrence of complications. J Gastrointest Surg. 2015;19(1):72–9; discussion 79.
Okano K, Hirao T, Unno M, Fujii T, Yoshitomi H, Suzuki S, Satoi S, Takahashi S, Kainuma O, Suzuki Y. Postoperative infectious complications after pancreatic resection. Br J Surg. 2015;102(12):1551–60.
McMillan MT, Christein JD, Callery MP, Behrman SW, Drebin JA, Hollis RH, Kent TS, Miller BC, Sprys MH, Watkins AA, Strasberg SM, Vollmer CM Jr. Comparing the burden of pancreatic fistulas after pancreatoduodenectomy and distal pancreatectomy. Surgery. 2016;159(4):1013–22.
Van Buren G 2nd, Bloomston M, Schmidt CR, Behrman SW, Zyromski NJ, Ball CG, Morgan KA, Hughes SJ, Karanicolas PJ, Allendorf JD, Vollmer CM Jr, Ly Q, Brown KM, Velanovich V, Winter JM, McElhany AL, Muscarella P 2nd, Schmidt CM, House MG, Dixon E, Dillhoff ME, Trevino JG, Hallet J, Coburn NSG, Nakeeb A, Behrns KE, Sasson AR, Ceppa EP, Abdel-Misih SRZ, Riall TS, Silberfein EJ, Ellison EC, Adams DB, Hsu C, Tran Cao HS, Mohammed S, Villafañe-Ferriol N, Barakat O, Massarweh NN, Chai C, Mendez-Reyes JE, Fang A, Jo E, Mo Q, Fisher WE. A Prospective Randomized Multicenter Trial of Distal Pancreatectomy With and Without Routine Intraperitoneal Drainage. Ann Surg. 2017;266(3):421–431.
Hassenpflug M, Hinz U, Strobel O, Volpert J, Knebel P, Diener MK, Doerr-Harim C, Werner J, Hackert T, Büchler MW. Teres Ligament Patch Reduces Relevant Morbidity After Distal Pancreatectomy (the DISCOVER Randomized Controlled Trial). Ann Surg. 2016;264(5):723–730.
Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, Behrman SW, Dickson EJ, Callery MP, Christein JD, Drebin JA, Hollis RH, House MG, Jamieson NB, Javed AA, Kent TS, Kluger MD, Kowalsky SJ, Maggino L, Malleo G, Valero V 3rd, Velu LKP, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM Jr. Risk Factors and Mitigation Strategies for Pancreatic Fistula After Distal Pancreatectomy: Analysis of 2026 Resections From the International, Multi-institutional Distal Pancreatectomy Study Group. Ann Surg. 2019;269(1):143–149.
Yamashita S, Ishizawa T, Ichida A, Kaneko J, Aoki T, Sakamoto Y, Sugawara Y, Hasegawa K, Kokudo N. Advantages and Disadvantages of Prophylactic Abdominal Drainage in Distal Pancreatectomy. World J Surg. 2016;40(5):1226–35.
El Khoury R, Kabir C, Maker VK, Banulescu M, Wasserman M, Maker AV. Do Drains Contribute to Pancreatic Fistulae? Analysis of over 5000 Pancreatectomy Patients. J Gastrointest Surg. 2018;22(6):1007–1015.
Adachi T, Kuroki T, Kitasato A, Hirabaru M, Matsushima H, Soyama A, Hidaka M, Takatsuki M, Eguchi S. Safety and efficacy of early drain removal and triple-drug therapy to prevent pancreatic fistula after distal pancreatectomy. Pancreatology. 2015;15(4):411–6.
Yang F, Jin C, Li J, Di Y, Zhang J, Fu D. Clinical significance of drain fluid culture after pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2018;25(11):508–517.
Kawaida H, Kono H, Watanabe M, Hosomura N, Amemiya H, Fujii H. Risk factors of postoperative pancreatic fistula after distal pancreatectomy using a triple-row stapler. Surg Today. 2018;48(1):95–100.
Nahm CB, de Reuver PR, Hugh TJ, Pearson A, Gill AJ, Samra JS, Mittal A. Intra-Operative Amylase Concentration in Peri-Pancreatic Fluid Predicts Pancreatic Fistula After Distal Pancreatectomy. J Gastrointest Surg. 2017;21(6):1031–1037.
Maggino L, Malleo G, Bassi C, Allegrini V, Beane JD, Beckman RM, Chen B, Dickson EJ, Drebin JA, Ecker BL, Fraker DL, House MG, Jamieson NB, Javed AA, Kowalsky SJ, Lee MK, McMillan MT, Roses RE, Salvia R, Valero V 3rd, Velu LKP, Wolfgang CL, Zureikat AH, Vollmer CM Jr. Identification of an Optimal Cut-off for Drain Fluid Amylase on Postoperative Day 1 for Predicting Clinically Relevant Fistula after Distal Pancreatectomy: A Multi-Institutional Analysis and External Validation. Ann Surg. 2019;269(2):337–343.
Nagakawa Y, Matsudo T, Hijikata Y, Kikuchi S, Bunso K, Suzuki Y, Kasuya K, Tsuchida A. Bacterial contamination in ascitic fluid is associated with the development of clinically relevant pancreatic fistula after pancreatoduodenectomy. Pancreas. 2013;42(4):701–6.
Sugiura T, Mizuno T, Okamura Y, Ito T, Yamamoto Y, Kawamura I, Kurai H, Uesaka K. Impact of bacterial contamination of the abdominal cavity during pancreaticoduodenectomy on surgical-site infection. Br J Surg. 2015;102(12):1561–6.
Yamashita K, Kato D, Sasaki T, Shiwaku H, Ishii F, Naito S, Yamashita Y, Hasegawa S. Contaminated drainage fluid and pancreatic fistula after pancreatoduodenectomy: A retrospective study. Int J Surg. 2018;52:314–319.
Sato A, Masui T, Nakano K, Sankoda N, Anazawa T, Takaori K, Kawaguchi Y, Uemoto S. Abdominal contamination with Candida albicans after pancreaticoduodenectomy is related to hemorrhage associated with pancreatic fistulas. Pancreatology. 2017;17(3):484–489.
Yang F, Jin C, Di Y, He H, Hao S, Yao L, Li J, Fu D. Central pancreatectomy with external drainage of monolayer pancreaticojejunostomy for prevention of postoperative pancreatic fistula: A retrospective cohort study. Int J Surg. 2018;51:104–108.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138(1):8–13.
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M; International Study Group on Pancreatic Surgery (ISGPS). The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery. 2017;161(3):584–591.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142(5):761–8.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Büchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142(1):20–5.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
DeOliveira ML, Winter JM, Schafer M, Cunningham SC, Cameron JL, Yeo CJ, Clavien PA. Assessment of complications after pancreatic surgery: A novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 2006;244(6):931–7; discussion 937-9.
Braga M, Capretti G, Pecorelli N, Balzano G, Doglioni C, Ariotti R, Di Carlo V. A prognostic score to predict major complications after pancreaticoduodenectomy. Ann Surg. 2011;254(5):702–7; discussion 707-8.
Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, Maithel SK, Patel SH, Bentram DJ, Weber SM, Cho CS, Winslow ER, Scoggins CR, Martin RC, Kim HJ, Baker JJ, Merchant NB, Parikh AA, Kooby DA. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg. 2012;256(3):529–37.
Yang F, Yu X, Bao Y, Du Z, Jin C, Fu D. Prognostic value of Ki-67 in solid pseudopapillary tumor of the pancreas: Huashan experience and systematic review of the literature. Surgery. 2016;159(4):1023–31.
Kent TS, Sachs TE, Callery MP, Vollmer CM Jr. The burden of infection for elective pancreatic resections. Surgery. 2013;153(1):86–94.
Marchegiani G, Perri G, Pulvirenti A, Sereni E, Azzini AM, Malleo G, Salvia R, Bassi C. Non-inferiority of open passive drains compared with closed suction drains in pancreatic surgery outcomes: A prospective observational study. Surgery. 2018;164(3):443–449.
Paquette IM, Swenson BR, Kwaan MR, Mellgren AF, Madoff RD. Thirty-day outcomes in patients treated with en bloc colectomy and pancreatectomy for locally advanced carcinoma of the colon. J Gastrointest Surg. 2012;16(3):581–6.
Schwartz PB, Roch AM, Han JS, Vaicius AV, Lancaster WP, Kilbane EM, House MG, Zyromski NJ, Schmidt CM, Nakeeb A, Ceppa EP. Indication for en bloc pancreatectomy with colectomy: when is it safe? Surg Endosc. 2018;32(1):428–435.
Loos M, Strobel O, Legominski M, Dietrich M, Hinz U, Brenner T, Heininger A, Weigand MA, Büchler MW, Hackert T. Postoperative pancreatic fistula: Microbial growth determines outcome. Surgery. 2018;164(6):1185–1190.
Yang F, Jin C, Fu D. Pasireotide for postoperative pancreatic fistula. N Engl J Med. 2014;371(9):875.
Yamashita K, Sasaki T, Itoh R, Kato D, Hatano N, Soejima T, Ishii K, Takenawa T, Hiromatsu K, Yamashita Y. Pancreatic fistulae secondary to trypsinogen activation by Pseudomonas aeruginosa infection after pancreatoduodenectomy. J Hepatobiliary Pancreat Sci. 2015;22(6):454–62.
Nishie H, Okumura F, Fukusada S, Inoue T, Kachi K, Anbe K, Natsume M, Nishi Y, Yoshimura N, Mizushima T, Sano H, Kajikawa M, Harada A, Naitoh I, Hayashi K, Nakazawa T. A case of intraductal papillary mucinous carcinoma found with acute obstructive suppurative pancreatic ductitis and liver abscess, and associated with a pancreatobiliary fistula. Nihon Shokakibyo Gakkai Zasshi. 2013;110(7):1304–12. [In Japanese]
Rogers MB, Aveson V, Firek B, Yeh A, Brooks B, Brower-Sinning R, Steve J, Banfield JF, Zureikat A, Hogg M, Boone BA, Zeh HJ, Morowitz MJ. Disturbances of the Perioperative Microbiome Across Multiple Body Sites in Patients Undergoing Pancreaticoduodenectomy. Pancreas. 2017;46(2):260–267.
Fujita S, Saito N, Yamada T, Takii Y, Kondo K, Ohue M, Ikeda E, Moriya Y. Randomized, multicenter trial of antibiotic prophylaxis in elective colorectal surgery: single dose vs 3 doses of a second-generation cephalosporin without metronidazole and oral antibiotics. Arch Surg. 2007;142(7):657–61.
Kusachi S, Sumiyama Y, Nagao J, Arima Y, Yoshida Y, Tanaka H, Nakamura Y, Saida Y, Watanabe M, Watanabe R, Sato J. Prophylactic antibiotics given within 24 hours of surgery, compared with antibiotics given for 72 hours perioperatively, increased the rate of methicillin-resistant Staphylococcus aureus isolated from surgical site infections. J Infect Chemother. 2008;14(1):44–50.
Franco LM, Cota GF, Pinto TS, Ercole FF. Preoperative bathing of the surgical site with chlorhexidine for infection prevention: Systematic review with meta-analysis. Am J Infect Control. 2017;45(4):343–349.
Author information
Authors and Affiliations
Contributions
Feng Yang contributed to the conception and design of this paper, data acquisition, drafting and revising the article, and final approval of the version to be published; Sijie Hao contributed to the data acquisition and analysis, and revising the article; Chen Jin and Deliang Fu contributed to the conception and design of this paper, data analysis, and final approval of it.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supported by the National Key R&D Program of China No.2017YFC1308604 (Dr Yang).
Electronic supplementary material
Supplementary Figure 1
Schematic drawing of drainage placement after distal pancreatectomy in our center. (PNG 1766 kb)
Rights and permissions
About this article
Cite this article
Yang, F., Jin, C., Hao, S. et al. Drain Contamination after Distal Pancreatectomy: Incidence, Risk Factors, and Association with Postoperative Pancreatic Fistula. J Gastrointest Surg 23, 2449–2458 (2019). https://doi.org/10.1007/s11605-019-04155-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04155-7