Abstract
Background
Early recurrence after liver resection of hepatocellular carcinoma (HCC) has a great effect on the survival of patients. The aims of this study were to identify risk factors for early recurrence and to clarify whether early recurrence is related to patient survival rate.
Methods
We identified a total of 1010 patients with HCC recurrence after hepatic resection between 2009 and 2014 in Samsung Medical Center and Seoul National University Hospital. Inclusion criteria were preoperative solitary tumor Child-Pugh class A and curative hepatectomy. Early recurrence was defined as HCC recurrence < 1 year after surgery.
Results
A total of 628 patients were included in this study: 302 with early recurrence and 326 with late recurrence. Multivariate analysis showed that HCC grade 3 or 4, tumor size > 3 cm, and microvascular invasion were closely associated with early recurrence after liver resection for solitary HCC. When HCC recurred, the early recurrence group had large tumor size, increased tumor numbers and AFP levels, and high incidence of diffuse intrahepatic recurrence compared with the late recurrence group. The overall survival curve for the early recurrence group was lower than that for the late recurrence group (P < 0.001). Multivariate analysis demonstrated early recurrence was closely associated with patient survival.
Conclusions
Patients with early recurrence had different characteristics compared to patients with late recurrence after hepatic resection in solitary HCC. Early detection of recurrence is necessary through active postoperative surveillance in hepatectomy patients with poor prognostic factors.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Liver resection (LR) is considered to be a curative treatment for solitary hepatocellular carcinoma (HCC) in Eastern Asia because of the shortage of liver grafts from deceased donors.1,2 However, the incidence of intrahepatic recurrence after LR is about 50% at 5 years for patients with solitary HCC.3,4 Understanding and predicting HCC recurrence is important for improving the prognosis of hepatectomy patients because of the rate of high recurrence after curative LR.
The time interval between LR and HCC recurrence is reported to influence patient survival. Therefore, early recurrence is considered when predicting poor survival of HCC patients who have undergone LR.5,6,7,8,9,10 Numerous studies have identified important predictive factors for early recurrence after curative LR. Previous multiple studies reported that risk factors for early recurrence were associated with tumor factors, host factors, and surgical factors.5,6,7,8,9,10 Tumor factors included tumor size, number, differentiation grade, and preoperative tumor markers. Hepatitis activity, presence of cirrhosis, and hepatitis viral load were considered as host factors.5,6,7,8,9,10
Consequently, analysis of factors carrying a high risk of recurrence may improve the selection of patients for surgery, leaving those with the worst prognosis for other less-invasive treatments. The aim of this study was to identify prognostic factors for patients with solitary HCC that influence early recurrence within 1 year after LR and their survival rate.
Materials and Methods
Patients
This study was performed on patients who underwent LR for solitary HCC at Samsung Medical Center (SMC) (n = 1382) or Seoul National University Hospital (SNUH) (n = 938) between January 2005 and December 2011 based on preoperative radiological images. HCC was histologically confirmed after LR. Patients with recurrent HCC after LR in the two centers were included (n = 1010). This study was approved by the Samsung Medical Center Institutional Review Board (SMC 2013-05-013) and Seoul National University Hospital Institutional Review Board (H-1303-061-474).
Inclusion criteria included performance status of 0–1, solitary HCC in the preoperative images, no extrahepatic metastasis, primary curative LR, and Child-Pugh class A. Multiple HCC in the preoperative images (n = 174); Child-Pugh class B (n = 51); re-resection (n = 40); extrahepatic metastasis or invasion (n = 9); and the history of locoregional therapies such as radiation, transarterial chemoembolization (TACE), radiofrequency ablation (RFA), or percutaneous ethanol injection (PEI) (n = 11), R1 resection (n = 67), and incomplete data or loss to follow-up after LR (n = 30), were excluded in present study.
Demographic data, preoperative laboratory findings, and pathologic data collected from electronic medical records were retrospectively reviewed. None of the patients received postoperative adjuvant therapy prior to HCC recurrence. A total of 628 patients were selected (Fig. 1).
Early recurrence group was defined as HCC recurrence within 1 year after LR. Patients who experienced recurrence after more than 1 year were defined as the late recurrence group.
Surgery and Surveillance
Surgical procedure and surveillance after LR in two centers were previously described.3,4,11,12 Four surgeons in SMC and four surgeons in SNUH performed LR for HCC. All patients were followed at 1-month postoperatively and then every 2 or 3 months. Follow-up duration was the time from surgery to final follow-up or death.
Therapy in Recurrent HCC
Patients with intrahepatic recurrences were treated with liver re-resection (RR), RFA, PEI, TACE, living donor liver transplantation (LDLT), or combined TACE and RFA (TACE-RFA). When feasible, RR, PEI, and RFA were considered as first-choice treatments. RR was performed based on the same criteria as initial resection, including Child A patients with solitary or oligonodular (≤ 3 nodules < 3 cm) recurrence in one or two adjacent segments, preserved liver function, and sufficient liver volume without severe portal hypertension. Patients whose recurrent HCC lesions were small (≤ 3 cm in diameter) and accessible for percutaneous RFA or PEI and in whom RR would be risky were treated with RFA in SMC or PEI in SNUH. Patients who did not fulfill the aforementioned criteria underwent TACE if the serum total bilirubin level was < 2 mg/dL. Salvage LDLT was considered when they had potential living liver donors, otherwise when RR, PEI, and RFA were not possible owing to tumor location and/or poor liver functional reserve. Patients with small HCC (3 cm) infeasible for US-guided RFA were referred for combined TACE-RFA in SMC. Target therapy or systemic chemotherapy was not given as the treatment choice at the first recurrence.
Statistical Analysis
All statistical analyses were performed using SPSS ver. 22.0 (SPSS, Inc., Chicago, IL, USA). Continuous variables are described as medians with ranges. Categorical variables are expressed as numbers and percentage of subjects. Chi-square test or Fisher’s exact test was conducted to evaluate differences in frequencies of categorical variables between groups. The significant cutoff value of AFP level was drawn from the significant continuous variables using receiver operating characteristic (ROC) curves. Cumulative survival time was calculated using the Kaplan–Meier method and compared by log-rank test. All significant predictors of early recurrence in univariate analysis were analyzed in a binary logistic regression model to show independent values by multivariate analysis. Factors that were significant (P < 0.05) for the prediction of patient survival in a univariate survival analysis were selected for a multivariate survival model. Confidence intervals (CIs) and odds ratios (ORs) were calculated. All tests were two-sided, and statistical significance was defined as P < 0.05.
Results
Baseline Characteristics
Among 1010 patients, records for 628 were analyzed. All patients were classified as Child-Pugh class A and had solitary HCC without extrahepatic metastasis at surgery. The early recurrence group had 302 patients (48.1%) and the late recurrence group had 326 patients (51.9%). Median disease-free survival was 6.1 months for the early recurrence group and 33.9 months for the late recurrence group (Fig. 1).
Comparison Early and Late Recurrence
Cumulative patient survival rates for 3, 5, and 7 years were 71.7%, 58.7%, and 51.9% for the early recurrence group, respectively, and 97.5%, 88.7%, and 86.9% for the late recurrence group (Fig. 2). Patient survival was longer in the late recurrence group than the early recurrence group (P < 0.001).
Mean age was younger in the early recurrence group than the late recurrence group (54 years vs. 56 years; P = 0.041), and mean platelet counts were higher in the early recurrence group than the late recurrence group (164,010/mL vs. 149,428/mL; P = 0.013). Preoperative mean AFP level was significantly higher in the early recurrence group than the late recurrence group (7961 ± 33,577 ng/mL vs. 1915 ± 12,092 ng/mL; P < 0.001) (Table 1). Total bilirubin, creatinine, and ICG-R15 were significantly different in the early recurrence group compared to the late recurrence group, but values were within the normal ranges.
Mean tumor size was larger in the early recurrence group than the late recurrence group (5.6 ± 3.7 cm vs. 4.1 ± 2.7 cm; P < 0.001). The incidence of tumor size > 3 cm, grade 3 or 4, pathological necrosis, microvascular invasion, and macrovascular invasion was significantly higher in the early recurrence group than the late recurrence group (P < 0.001). Major LR, multiple tumor numbers, pathologic hemorrhage, and intrahepatic metastasis were not different between the two groups (Table 2).
Prediction of Early Recurrence after Hepatic Resection
On multivariate analysis, statistically significant factors predicting early HCC recurrence were grade 3 or 4 (OR, 2.882; 95% CI, 1.667–4.975; P < 0.001), tumor size >3 cm (OR, 2.242; 95% CI, 1.362–3.690; P = 0.001), and microvascular invasion (OR, 2.110; 95% CI, 1.319–3.378; P = 0.002) at surgery.
We compared patient survival according to number of risk factors which were related with early HCC recurrence after LR. Patient survival at 5 years was 89.4% for patients without risk factors, 80.2% for patients with one risk factor, 68.4% for patients with two risk factors, and 62.6% for patients with three risk factors. The lower the number of risk factors, the greater the survival rate of patients with recurrent HCC (Fig. 3).
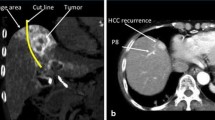
Management of Recurrent HCC
When recurrent HCC was diagnosed, tumor size and tumor numbers and AFP and PIVKA-II levels were higher in the early recurrence group than in the late recurrence group (Table 3). Incidence of extrahepatic recurrence did not reach a significant level, but diffuse intrahepatic recurrence more than ten intrahepatic nodules in the early recurrence group was higher than the late recurrence group (10.9% vs. 0.9%; P < 0.001). TACE was commonly used in the early and late recurrence groups (65.6% vs. 45.4%), but RFA was higher in the late recurrence group than the early recurrence group (34.0% vs. 21.2%).
Risk Factors for Patient Survival
Univariate analysis showed that increased in age, total bilirubin level, INR, tumor size, pathologic hemorrhage, microvascular invasion, macrovascular invasion, long hospitalization, and early recurrence were closely associated with patient survival. Multivariate analysis demonstrated that increased in age, albumin, total bilirubin, long hospitalization, grade 3 or 4, pathologic hemorrhage, macrovascular invasion, and early recurrence were predisposing factors for patient survival (Table 4).
Discussion
Time after recurrence is an important prognostic factor. Therefore, early HCC recurrence appears to be associated with worse survival rates, compared with those with later recurrence.5,6,7,8,9,10 In this study, risk factors for early and late recurrence were assessed for hepatectomy patients with solitary HCC. Early recurrence was a main cause of poor prognosis after curative hepatic resection in patients with solitary HCC. Our study confirmed that early HCC recurrence was associated with adverse tumor factors including large tumor size, grade 3 or 4, and microvascular invasion. In addition, early recurrence developed in 50% of HCC patients with recurrent HCC who underwent curative LR for solitary HCC in a 5-year period.
The definition of early recurrence is still controversial. There are two studies that refer to early recurrence based on 1-year postoperative without sufficient explanation.13 Other studies defined early recurrence based on 6-months postoperative.7,10 Another study reported that HCC recurrence within 2 years after LR is defined as early recurrence because of an early peak for recurrence at approximately 1 postoperative year and a second peak at 4 years after surgery.14 Early recurrence (within 2 years) is associated with tumor-related factors including presence of microvascular invasion and satellite lesion. Late recurrence (after 2 years) seems to be related to background liver disease conditions such as hepatic inflammation and liver damage.14
In this study, we defined early recurrence as within 1 year after LR as an arbitrary cutoff. Our study demonstrated that unfavorable factors such as tumor size, tumor grade, and microvascular invasion were predisposing factors for early HCC recurrence after curative LR. When none of these factors was present, the outcome was particularly good with a risk of recurrence of about 10%. Previously, different studies reported risk factors for early recurrence include AFP, PIVKA-II, intrahepatic metastases, tumor size, tumor number, positive resection margin, venous invasion, tumor rupture, tumor differentiation, and serum alanine transferase level.5,6,7,8,9,10,15,16 However, previous studies have reported conflicting results about which factors predict recurrence. Much debate still exists because enrolled patients were heterogeneous in clinicopathological characteristics and management-related factors.5,6,7,8,9,10,15,16
Our study showed that increased AFP level before surgery was associated with early recurrence. AFP level was higher in the early recurrence group compared to the late recurrence group when HCC recurrence was diagnosed after LR. However, serum AFP level did not demonstrate early recurrence in multivariate analysis. This factor might have revealed a likely wide variation in values inherent in our patient population.
Proteins induced by vitamin K absence or antagonist-II (PIVKA-II) or positron emission tomography (PET) uptake were closely associated prognostic factors after LR.4,17,18 However, we could not identify the effect of PIVKA-II or PET uptake as prognostic factor in hepatectomy patients because many patients did not undergo such evaluations.
The high early recurrence rates seen of patients with HCC and unfavorable characteristics suggest microscopic intrahepatic dissemination beyond the resection field, so simple tumor removal would be insufficient.19 Microvascular invasion is related to multinodular diffuse, which is considered metastasis.9,19 Neither preoperative characteristics nor intraoperative factors correlated with early HCC recurrence after LR. These prognostic factors are not known until the final pathology report. If poor prognostic factors are known before surgery, physicians or surgeons should consider limiting the indication or relative contraindications to LR. These predictors would not be suggested by preoperative liver biopsy and therefore do not support the use of routine biopsy before surgery.20 Identification, prevention, or early detection of early HCC recurrence should be emphasized until molecular profiling is available for HCC. In patients with a high risk of early recurrence after initial LR for HCC, early detection through close postoperative surveillance is necessary. Patients with unfavorable factors on pathologic review should be closely monitored in the first year after LR of HCC, and strong consideration should be given to preemptive adjuvant therapy. Although prophylactic liver transplantation is controversial, it should be considered.
HCC recurrence must not be considered a definitive failure of the therapeutic program in patients initially addressed with curative LR. Recurrence may be treated with curative intent, and a long survival may result from an aggressive treatment of the recurrent lesion. Re-resection, RFA, and PEI have been shown to be curative treatments for recurrent HCC.16 In our study, 32.7% of patients with early recurrence and 50.8% of patients with late recurrence were suitable for such treatment approaches.
Our study has several limitations. First, it was retrospective. Second, selection bias was inevitable and may have influenced the analysis because we selected only patients who had undergone LR. Third, HBV is the most common cause of HCC in Korea, which is not the case in most Western countries. Fourth, the treatment of recurrent HCC does not have any guidelines. Therefore, recurrent HCC was treated based on physician preference or multidisciplinary team approach.
In conclusion, the survival rate in a late recurrence group was significantly better than that of an early recurrence group after curative hepatic resection in patients with solitary HCC. Patients with large tumor size, microvascular invasion, and grade 3 or 4 on pathologic examination should be actively and closely monitored to detect early HCC recurrence. We hope that our findings will help identify patients with a high possibility of recurrence after surgery to improve survival by early detection of recurrent HCC. Therefore, a strict follow-up protocol and treatment strategies should be established for early detection and intervention of recurrence.
References
Lee JM, Park JW, Choi BI. 2014 KLCSG-NCC Korea Practice Guidelines for the management of hepatocellular carcinoma: HCC diagnostic algorithm. Dig Dis 2014;32:764–777.
Yu SJ. A concise review of updated guidelines regarding the management of hepatocellular carcinoma around the world: 2010-2016. Clin Mol Hepatol 2016;22:7–17.
Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, Paik SW, Park CK, Yoo BC. Outcomes after curative hepatectomy in patients with non-B non-C hepatocellular carcinoma and hepatitis B virus hepatocellular carcinoma from non-cirrhotic liver. J Surg Oncol 2014;110:976–981.
Kim JM, Kwon CH, Joh JW, Park JB, Lee JH, Kim SJ, Paik SW, Park CK, Yoo BC. Differences between hepatocellular carcinoma and hepatitis B virus infection in patients with and without cirrhosis. Ann Surg Oncol 2014;21:458–465.
Hong YM, Cho M, Yoon KT, Chu CW, Yang KH, Park YM, Rhu JH. Risk factors of early recurrence after curative hepatectomy in hepatocellular carcinoma. Tumour Biol 2017;39:1010428317720863.
Lim KC, Chow PK, Allen JC, Siddiqui FJ, Chan ES, Tan SB. Systematic review of outcomes of liver resection for early hepatocellular carcinoma within the Milan criteria. Br J Surg 2012;99:1622–1629.
Hirokawa F, Hayashi M, Asakuma M, Shimizu T, Inoue Y, Uchiyama K. Risk factors and patterns of early recurrence after curative hepatectomy for hepatocellular carcinoma. Surg Oncol 2016;25:24–29.
Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GA, Giulini SM. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg 2006;243:229–235.
Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, Taylor BR, Grant DR, Vollmer CM. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg 2006;202:275–283.
Lu X, Zhao H, Yang H, Mao Y, Sang X, Miao R, Xu Y, Du S, Xu H, Chi T, Yang Z, Zhong S, Huang J. A prospective clinical study on early recurrence of hepatocellular carcinoma after hepatectomy. J Surg Oncol 2009;100:488–493.
Han SR, Kim JM, Choi GS, Park JB, Kwon CH, Kim SJ, Joh JW. Protrusion of hepatocellular carcinoma is a predictor of early recurrence in hepatectomy patients after spontaneous rupture. Ann Surg Treat Res 2016;91:17–22.
Kim JM, Kwon CH, Joh JW, Park JB, Ko JS, Lee JH, Kim SJ, Park CK. The effect of alkaline phosphatase and intrahepatic metastases in large hepatocellular carcinoma. World J Surg Oncol 2013;11:40.
Hayashi M, Shimizu T, Hirokawa F, Inoue Y, Komeda K, Asakuma M, Miyamoto Y, Takeshita A, Shibayama Y, Tanigawa N. Clinicopathological risk factors for recurrence within one year after initial hepatectomy for hepatocellular carcinoma. Am Surg 2011;77:572–578.
Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, Sugawara Y, Minagawa M, Takayama T, Kawasaki S, Makuuchi M. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol 2003;38:200–207.
Wu JC, Huang YH, Chau GY, Su CW, Lai CR, Lee PC, Huo TI, Sheen IJ, Lee SD, Lui WY. Risk factors for early and late recurrence in hepatitis B-related hepatocellular carcinoma. J Hepatol 2009;51:890–897.
Li T, Fan J, Qin LX, Zhou J, Sun HC, Qiu SJ, Ye QH, Wang L, Tang ZY. Risk factors, prognosis, and management of early and late intrahepatic recurrence after resection of primary clear cell carcinoma of the liver. Ann Surg Oncol 2011;18:1955–1963.
Kim JM, Hyuck C, Kwon D, Joh JW, Lee JH, Paik SW, Park CK. Protein induced by vitamin K antagonist-II (PIVKA-II) is a reliable prognostic factor in small hepatocellular carcinoma. World J Surg 2013;37:1371–1378.
Kim JM, Kwon CHD, Joh JW, Sinn DH, Choi GS, Paik SW. Prognosis of preoperative positron emission tomography uptake in hepatectomy patients. Ann Surg Treat Res 2018;94:183–189.
Lim KC, Chow PK, Allen JC, Chia GS, Lim M, Cheow PC, Chung AY, Ooi LL, Tan SB. Microvascular invasion is a better predictor of tumor recurrence and overall survival following surgical resection for hepatocellular carcinoma compared to the Milan criteria. Ann Surg 2011;254:108–113.
Levy I, Greig PD, Gallinger S, Langer B, Sherman M. Resection of hepatocellular carcinoma without preoperative tumor biopsy. Ann Surg 2001;234:206–209.
Funding
This work was funded by the Korean Liver Cancer Association.
Author information
Authors and Affiliations
Contributions
Sung Mi Jung: literature search, data analysis and interpretation and writing
Jong Man Kim: design, literature search, data acquisition, analysis, and interpretation and writing
Jae-Won Joh: design and data interpretation
Nam Joon Yi, Gyu-Seong Choi, Choon Hyuck David Kwon, Kwang-Woong Lee, and Kyung-Suk Suh: acquisition and analysis of data
Corresponding author
Ethics declarations
This study was approved by the Samsung Medical Center Institutional Review Board (SMC 2013-05-013) and Seoul National University Hospital Institutional Review Board (H-1303-061-474).
Rights and permissions
About this article
Cite this article
Jung, SM., Kim, J.M., Choi, GS. et al. Characteristics of Early Recurrence After Curative Liver Resection for Solitary Hepatocellular Carcinoma. J Gastrointest Surg 23, 304–311 (2019). https://doi.org/10.1007/s11605-018-3927-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3927-2