Abstract
Purpose
The number of patients aged ≥ 90 years is increasing worldwide; however, the treatment guidelines for colorectal cancer in elderly patients remain unclear. This study aimed to investigate the clinical outcomes of patients with primary colorectal cancer aged ≥ 90 years.
Methods
We retrospectively reviewed the medical records of 100 patients (aged ≥ 90 years) with primary colorectal adenocarcinoma. Their demographic and clinical characteristics and surgical outcomes were assessed.
Results
The patients who underwent tumor resections (n = 71) showed longer overall and cancer-specific survival than those who underwent non-operative treatments (n = 29) (median overall survival time: 23.92 months vs. 2.99 months, P < 0.0001). Age, body mass index, performance status, advanced cancer stage (stages 3 and 4), and treatment strategy were identified as risk factors, prognostic factors, and predictors of overall survival. No significant differences in the postoperative morbidity rate, in-hospital mortality rate, and survival time were found between the elective laparoscopic (n = 27) and elective open (n = 37) surgery subgroups. However, the in-hospital mortality rate was 6.25% (4/64) in the patients who underwent elective open surgeries and 42.9% (3/7) in those who underwent emergent open surgeries (p = 0.0179).
Conclusions
In clinical practice, surgical treatment should not be denied to patients with primary colorectal cancer aged ≥ 90 years. However, the high complication and mortality rates for emergency surgeries act as a deterrent. Further studies to eliminate the bias between operative and non-operative groups may be needed to validate our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human’s life expectancy is increasing gradually; thus, the proportion of the elderly population is also increasing. In Taiwan, approximately 12% of the entire population was aged > 65 years; 1.37%, > 85 years; and 0.41%, > 90 years in 2014, and these proportions continue to increase.1,2 As a result, the proportion of the “old-old” population (i.e., age of ≥ 85 years) is expected to increase more than twofold from 2014 to 2061.3
Colorectal cancer (CRC) is one of the most common cancers worldwide. It occurs at any age; however, age remains one of its most important risk factors.4 The fact that most cancers of the colon and rectum evolve from isolated adenomatous polyps and villous adenomas has been known as the polyp-cancer sequence. The natural history of the polyp-cancer sequence is highly variable in patients. It happens never less than 5 years with an average of 10–15 years.5 Since the life expectancy is increasing, the number of elderly patients with CRC and various comorbidities is expected to increase accordingly.6
In the past, very old patients with CRC were treated less aggressively owing to concerns of age, physical conditions, comorbidities, and available surgical techniques.7 However, CRC can now be diagnosed via routine screening examinations early,8 and surgical techniques and postoperative medical care have improved dramatically. Thus, more aggressive treatment has recently been used in very old patients. In particular, laparoscopic colorectal resection has become the standard treatment for patients with CRC. It provides greater perioperative benefits in elderly patients than in younger patients.9 Hence, this study aimed to investigate the clinical outcomes of patients with CRC aged ≥ 90 years who underwent non-operative and operative treatments in the past 15 years.
Materials and Methods
We included patients aged ≥ 90 years with CRC diagnosed at the National Taiwan University Hospital and its Hsinchu Branch between January 2001 and September 2015. Patients treated with local excision and those with tumors of a non-glandular origin were excluded. A total of 100 patients with primary colorectal adenocarcinoma were enrolled in this study.
We collected the following patient information: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) score, performance status according to the Barthel index, preoperative comorbidities, tumor location, stage of presentation, type of surgical method, postoperative morbidity, postoperative hospital stay, in-hospital mortality, chemotherapy, radiotherapy, and survival by reviewing their medical records. Thereafter, the patients were divided into the non-operative and operative groups. Further, the patients in the operative group were subdivided into the laparoscopic and open surgery subgroups (including elective and emergent open surgeries). Emergent surgery was defined as surgery performed within 1 day after hospital admission. The preoperative comorbidities included cardiovascular diseases, respiratory diseases, renal disease, diabetes mellitus (DM), hypertension, cerebral infarction, and dementia or Alzheimer’s disease. Specifically, the cardiovascular diseases included coronary artery disease, arrhythmia, and heart failure; the respiratory diseases included lung emphysema and obstructive pulmonary disease. Renal disease was defined as a glomerular filtration rate (GFR) of < 60 ml/(min⋅1.73 m2). DM and hypertension were recorded if medical treatment for such was required. The Charlson comorbidity index was also calculated. The study was approved by the institutional review board of National Taiwan University Hospital (protocol no. 201410038RINB).
Statistical Analysis
Statistical analysis was performed using the R 3.2.3 software (R Foundation for Statistical Computing, Vienna, Austria). In statistical testing, two-sided P value ≤ 0.05 was considered statistically significant. The distributional properties of continuous variables were expressed by mean ± standard deviation (SD). Categorical variables were presented as frequencies and percentages. And, survival curves and the median survival times for time to death of any cause and time to death of cancer were estimated using the Kaplan-Meier method. In univariate analysis, the differences in the distributions of continuous variables and categorical variables among the four groups of patients with colorectal cancer (no surgery, laparoscopic surgery, elective open surgery, and emergent open surgery) were examined using Kruskal-Wallis rank-sum test or Fisher’s exact test. Similarly, the unadjusted effect of each potential risk factor, prognostic factor, and predictor of the two binary outcomes (i.e., death of any cause and death of cancer) was examined using Wilcoxon rank-sum test or Fisher’s exact test as appropriate.
Next, multivariate analysis was conducted by fitting Cox’s proportional hazards models to estimate the adjusted effects of risk factors, prognostic factors, and predictors of the two survival outcomes (i.e., time to death of any cause and time to death of cancer). Since the elderly patients were not randomized to one of the four treatment strategies, if a demographic or clinical characteristic was associated with the selection of the treatment strategy and it was also a risk factor of patient survival, then it could cause a selection bias in assessing the effect of a treatment strategy on patient survival. To tackle the potential selection bias due to the distributional differences in the baseline demographic and clinical characteristics among these four groups of patients, we performed a regression analysis, instead of a propensity score analysis, to examine the adjusted effects of surgical treatments on patient survival for comparing these groups in one multivariate analysis and minimizing the loss of subjects.
Results
Non-operative Treatment Versus Operative Treatment
The comparisons of the demographic and clinical characteristics among the four treatment strategies (no surgery, laparoscopic surgery, elective open surgery, and emergent open surgery) are shown in Table 1. The mean age of the 100 very old patients was 92.76 years (SD = 2.74). Among them, 29 patients did not undergo surgery, while 71 patients underwent one of the three operative treatments. As listed on the left panel of Table 1, no statistically significant differences were found in age, sex, tumor location, chemotherapy, and radiotherapy between the non-operative and operative groups. However, significant differences were detected in the BMI (20.18 ± 2.59 vs. 21.47 ± 2.93 kg/m2, P = 0.0374), performance status (38.10 ± 35.49 vs. 69.23 ± 31.37, P = 0.0001), dementia (17.2 vs. 4.2%, P = 0.0434), and cancer stage (P < 0.0001) between the non-operative and operative groups. And, the mortality rates were significantly different between the non-operative and operative groups (all deaths 96.6 vs. 63.4%, P = 0.0004; cancer deaths 86.2 vs. 32.4%, P < 0.0001).
Laparoscopic Surgery Versus Open Surgery (Elective or Emergent)
Moreover, as listed on the right panel of Table 1, 27 patients underwent laparoscopic surgery, and 44 patients underwent open surgery among the 71 patients in the operative group. None of the 27 laparoscopic surgeries were emergent, whereas 7 of the 44 open surgeries were emergent (6 patients had CRCs with obstructions, and 1 patient had massive bleeding). The 64 elective surgeries (27 laparoscopic surgeries and 37 open surgeries) were further analyzed. No statistically significant differences were found in age, sex, BMI, ASA score, performance status, tumor location, cancer stage, chemotherapy, radiotherapy, comorbidities, postoperative complications, and in-hospital mortality between the laparoscopic and elective open surgery groups. However, the patients who underwent emergent surgeries had a higher rate of postoperative respiratory complications than those who underwent laparoscopic or elective open surgeries (57.1 vs. 18.8%, P = 0.0411). Moreover, the patients who underwent emergent surgeries had a higher in-hospital mortality rate than those who underwent laparoscopic or elective open surgeries (42.9 vs. 6.3%, P = 0.0179). Specifically, in the 7 patients who underwent emergent open surgeries, 3 patients died, including 1 patient who died of pneumonia with respiratory failure and septic shock, 1 of aspiration pneumonia and shock-related multiple organ failure, and another of postoperative respiratory failure. By contrast, in the 64 patients who underwent laparoscopic or elective open surgeries, 4 patients died, including 1 patient who died of urosepsis, 1 of pneumonia with sepsis, 1 after undergoing laparoscopic surgery due to pulmonary congestion, and 1 of postoperative intracranial hemorrhage.
Conversion occurred in one patient owing to severe intra-abdominal adhesion. The operation was converted to open anterior resection immediately after the camera port was created, and severe adhesion was found. No conversion occurred because of cardiopulmonary compromise with insufflation.
Overall Survival and Cancer-Specific Survival
Next, univariate analyses of the demographic and clinical characteristics between the alive and dead patients, who died of any cause or died of cancer during the follow-up period, are shown in Table 2. No statistically significant associations with death of any cause were found in age, sex, tumor location, chemotherapy, radiotherapy, and comorbidity, but significant associations with death of any cause were detected in the BMI (alive 22.28 ± 3.11 kg/m2, dead 20.66 ± 2.69 kg/m2, P = 0.0159), performance status (alive 75.19 ± 31.3, dead 54.66 ± 35.43, P = 0.0095), cancer stage (P = 0.0346), surgery (dead/no surgery 96.6%, dead/surgery 63.4%, P = 0.0004), and treatment strategy (P = 0.0005). By contrast, no statistically significant associations with death of cancer were found in age, sex, BMI, tumor location, chemotherapy, radiotherapy, and comorbidity (except dementia), but significant associations with death of cancer were detected in the performance status (alive 70.00 ± 32.54, dead 49.58 ± 35.64, P = 0.0054), cancer stage (P < 0.0001), dementia (dead/dementia 100%, P = 0.0020), surgery (dead/no surgery 86.2%, dead/surgery 32.4%, P < 0.0001), and treatment strategy (P < 0.0001).
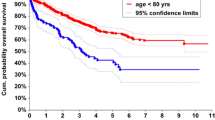
The median follow-up period of the 100 patients was 13.14 months (mean 24.01 months; range 0.23–170.58 months). As shown in Fig. 1a, the median overall survival time was 2.99 months (range 0.23–30.75 months) in the non-operative group as compared with 23.92 months (range 0.26–154.38 months) in the operative group. These two survival curves were statistically significantly different (P < 0.0001). As shown in Fig. 1b, after the patients who died of non-cancer-related causes were excluded, the survival curves of the non-operative and operative groups were still statistically significantly different (P < 0.0001).
a The long-term overall survival curves for elderly colorectal cancer patients (operative vs. non-operative). Solid line: patients who did not undergo surgery; dashed line: patients who underwent surgery. b The long-term cancer-specific survival curves for elderly colorectal cancer patients (operative vs. non-operative). Solid line: patients who did not undergo surgery; dashed line: patients who underwent surgery
However, as shown in Fig. 2, the overall survival and cancer-specific survival curves of the laparoscopic colectomy and elective open surgery groups were not statistically significantly different (P = 0.1138 and P = 0.6387, respectively). Specifically, the 5-year overall survival and cancer-specific survival rates in the operative group were 40.78 and 63.79%, respectively. The 5-year overall survival rates of the laparoscopic colectomy and elective open surgery groups were 61.85 and 30.01%, respectively. Moreover, the 5-year cancer-specific survival rates of the laparoscopic colectomy and elective open surgery groups were 75.38 and 57.28%, respectively.
a The long-term overall survival curves for elderly colorectal cancer patients (laparoscopic vs. elective open surgery). Solid line: patients who underwent elective open surgery; dashed line: patients who underwent laparoscopic surgery. b The long-term cancer-specific survival curves for elderly colorectal cancer patients (laparoscopic vs. elective open surgery). Solid line: patients who underwent elective open surgery; dashed line: patients who underwent laparoscopic surgery
Regression Analysis
As listed in Table 3, multivariate analyses of the risk factors, prognostic factors, and predictors for the time to death of any cause and time to death of cancer respectively were conducted by fitting stepwise Cox’s proportional hazard models with the available covariates in Tables 1 and 2 in our patients with CRC aged ≥ 90 years. We used the smoothing technique to detect nonlinear effects of continuous covariates and identify appropriate cut-off point(s) for discretizing continuous covariates, if necessary, during the stepwise variable selection procedure (not shown).
In the analysis of the risks for death of any cause, we found that older age (years), BMI < 22.19 kg/m2, performance status score < 78.48, and advanced cancer stage (stages 3 and 4) predicted the worse overall survival, but patients with ASA score ≤ 3 who underwent laparoscopic or elective open surgery had better overall survival. In other words, if two patients with CRC had the same old age, BMI, performance status score, and cancer stage, and their ASA scores ≤ 3, then the one who underwent laparoscopic or elective open surgery would live longer than the other one who did not undergo surgery or underwent emergent open surgery. Technically speaking, after adjusting for the effects of age, BMI < 22.19 kg/m2, performance status score < 78.48, and advanced cancer stage (stages 3 and 4), the hazard rates of the patients with ASA scores ≤ 3 who underwent laparoscopic or elective open surgeries would be 26.18% (95% confidence interval [CI] 12.45–55.08%, P = 0.0004) or 57.91% (95% CI 33.80–99.22%, P = 0.0467) of the hazard rate of the patients with ASA score ≤ 3 who did not undergo surgery or underwent emergent open surgery and those with ASA score > 3. The proportional hazard assumptions were not violated. And, the adjusted generalized R2 = 0.471 > 0.15 and the estimated area under the receiver operating characteristic (ROC) curve (standard error, se) = 0.7672 (0.0387) > 0.7 indicated a good fit.
By contrast, in the analysis of the risks for death of cancer, we found that older age (years), advanced cancer stage (stages 3 and 4), and non-surgical treatment predicted the worse cancer-specific survival, but the patients with higher performance status scores had a better cancer-specific survival. In other words, if two patients with CRC had the same old age, cancer stage, and performance status score, then the one who did not undergo surgery would have a shorter cancer-specific survival than the other one who underwent laparoscopic or open surgeries. Technical speaking, after adjusting for the effects of age, advanced cancer stage (stages 3 and 4), and performance status score, the hazard rate of the patients who did not undergo surgery would be 2.64 (95% CI 1.28–5.45, P = 0.0084) times of the hazard rate of the patients who underwent laparoscopic or open surgeries. The proportional hazards assumptions were not violated. And, the adjusted generalized R2 = 0.432 > 0.15 and the estimated area under the ROC curve (se) = 0.7961 (0.0460) > 0.7 indicated a good fit.
Discussion
The incidence of colon and rectal cancers is known to increase with age. As the life expectancy is increasing, the number of elderly patients with CRC and various comorbidities is also expected to increase worldwide. However, the relatively high risks of complications, postoperative sequelae, and in-hospital mortality in very old patients with CRC undergoing cancer surgery have led to the refusals of screening examinations and aggressive treatments. Similar to the natural end cancer concept by Kitagawa et al. in 1998,10 some people even consider that no treatment is the best treatment for the elderly to let them die peacefully without suffering.
Nevertheless, laparoscopic colectomy has gradually become a popular surgical option since 2000.11 It leads to shorter hospital stays and lower complication rates than open colorectal surgery.9,12,13,14,15 Similar to the finding of Valls et al.,16 we did not observe statistically significant differences in the length of hospital stay, postoperative complication rate, in-hospital mortality, and survival between laparoscopic colectomy and elective open surgeries in the patients with CRC aged ≥ 90 years. The tissues of the aged are weak, fragile, and more easily traumatized, and tissue healing and blood supply are known to be worse in elderly patients. This may be the reason why we did not observe the benefits of laparoscopic surgery in the very old patients in this study. Hence, the surgical procedure should be performed more gently in elderly patients to reduce the risks of tissue damages and complications. In our experience, the dissection plane in the elderly patients was loose with a lower tissue strength, and the dissection was difficult owing to the loss of elasticity in older tissues. Avoiding excessive manipulations in the surgical techniques was extremely important.
The postoperative complication rates in patients with CRC aged > 80 years have been reported to be 21–46.4%17,18,19 with perioperative mortality rates of 1.1–15.6%.4,17,18,19,20,21,22,23 In this study, the postoperative complication, major postoperative complication, and in-hospital mortality rates of elective open surgery in the patients with CRC aged ≥ 90 years were 45.3, 20.3, and 6.25%, respectively, which were not higher than those reported by other studies on elderly patients. By contrast, the postoperative complication rate was higher in the elderly patients who underwent emergent open surgeries. The mortality rate of emergent surgery in elderly patients has been reported to range from 27.6 to 81%.4,21,23,24,25,26 In our study, 4 of the 7 patients (57.1%) who underwent emergent open surgeries experienced major postoperative complications. Among these 4 patients who experienced major postoperative complications, 3 patients (42.9%) died in hospital due to postoperative sequelae.
In this study, we found statistically significant differences in the distributions of the BMI, performance status score, dementia, and cancer stage between the operative and non-operative groups. In fact, the patients with CRC with lower BMI, dementia, poor performance status, and advanced cancer stage were more likely to receive conservative treatments. Nevertheless, after controlling for the selection bias in our multivariate analyses, the important risk factors, prognostic factors, and predictors of overall survival and cancer-specific survival were identified by fitting stepwise Cox’s proportional hazard models, respectively. Specifically, older age, lower BMI, lower performance status score, and advanced cancer stage predicted the worse overall survival, but the patients with CRC and ASA score ≤ 3 who underwent laparoscopic colectomy or elective open surgery showed better overall survival. By contrast, older age (years), advanced cancer stage (stages 3 and 4), and non-surgical treatment predicted the worse cancer-specific survival, but patients with higher performance status scores showed better cancer-specific survival. These findings suggested that given the same baseline demographic and clinical characteristics, the patients who underwent surgery properly would have better overall survival and cancer-specific survival than those who did not. Hence, curative surgical treatments should be considered in patients with CRC aged ≥ 90 years, although their risks of postoperative morbidity and mortality are relatively high. However, there are still some biases in this study. To minimize these biases, it is better to compare patients with the same conditions.
In our study, patients who underwent surgery showed longer overall survival and cancer-specific survival than those who did not. However, the complication rates were relatively high in elderly patients who underwent emergency operations. The current colorectal cancer screening protocol in Taiwan is immunochemical fecal occult blood testing (iFOBT) every 2 years in patients between 50 and 74 years old. Therefore, our work suggests that colorectal screening in these extremely old patients (> 75 years old) may still be needed, not only because the cancer treatment results were acceptable, but also to reduce the rate of emergency operation, which has relatively high complication and mortality rates.
Elderly patients are usually unable to recover quickly from surgery owing to their decreased physiological reserve. Many studies have shown that prehabilitation can result in excellent recovery of functional outcomes in elderly patients undergoing elective colorectal surgery.27,28 A prehabiliation program should be customized according to each patient’s condition, the type of surgery, and the disease status. This is particularly true in elderly patients who are prone to have decreased functional reserve, more comorbidities, and increased possibility of medical and surgical interventions. Currently, no consensus has been reached about the duration of prehabilitation, especially for extremely old patients with colorectal cancer. For elective colorectal cancer surgery, prehabilitation programs with a duration of 3–6 weeks have been reported.29 Future studies with larger sample sizes are needed to explore more issues with regard to the duration of prehabilitation programs for elderly patients with colorectal cancer.
Although colorectal cancer surgery is steadily increasingly being performed in elderly patients aged 90 years or older, the decision-making of surgical treatment for these extremely old patients is still difficult owing to the possibility of negative influences on the quality of life, the limited functional capability of these patients, and the disposition of nursing facilities after the operation. The challenge is increasing because the population of elderly is rapidly growing. For many patients, their family, and physicians, quality of life and ability to perform activities of daily living after the operation is more important than extending life alone. Several reports have shown that elderly patients with colorectal cancer have a quality of life comparable to that of younger patients in most respects.30,31 For the treatment of colorectal cancer, age is not a contraindication for surgery. Furthermore, surgery is still useful in colorectal cancer even as a palliative treatment to prevent emergency surgery and to extend the comfortable life of patients. However, further prospective investigation with more enrolled patients that evaluates survival outcomes, quality of life, and functional status should be done, not only to extend the life expectancy but also to improve the quality of life.
The National Health Insurance (NHI) plan of Taiwan covers > 98% of Taiwan’s population, and enrollees enjoy almost free access to health care. Taiwan’s NHI was associated with a reduction of deaths of causes amenable to health care, particularly among those age groups (< 20 and ≥ 65 years) that were previously uninsured in the beginning.32 The appropriate management for colorectal cancer might be hindered by the high cost of cancer treatment. These economic barriers were eliminated after the implementation of NHI. Especially, the effect was more prominent because the proportion of elderly populations is increasing steadily in Taiwan.
This study has three limitations. First, it was difficult to perform a propensity score analysis in this study to reduce selection bias because there were four treatment groups (non-operative, laparoscopic surgery, elective open surgery, and emergent open surgery) to be compared in our multivariate analyses. And, it is infeasible to conduct randomized clinical trials in patients with CRC aged ≥ 90 years owing to ethical concerns. Second, 73 of the 100 patients died during the follow-up period, but the data on the patients’ post-discharge medical care and quality of life could not be collected retrospectively. Third, this study had a relatively small sample size of 100 so that statistically non-significant findings, including differences in the length of hospital stay, morbidity, and mortality between the laparoscopic and elective open surgery groups, might appear owing to the lack of statistical power. Hence, further studies with larger sample sizes are needed to verify these results and to explore more issues.
Conclusion
In summary, surgical treatment should not be denied to patients with primary CRC aged ≥ 90 years in clinical practice. With good preoperative preparation and postoperative care, such elderly patients who undergo surgical treatment could have good oncological outcomes similar to those in younger patients. However, the high complication and mortality rates for emergency surgeries act as a deterrent for such, and in such cases, palliative surgery should be considered rather than curative resection for emergency operations. Further research eliminating the bias between operative and non-operative groups is required to conclude that such very old patients with CRC could benefit from aggressive surgical treatment.
References
Taiwan Health and Welfare Report. Ministry of Health and Welfare, Executive Yuan, Taiwan, 2015. Available from: http://www.mohw.gov.tw/MOHW_Upload/doc/book/web20160111/files/flash/flippingbook.swf
Statistical Annual Report. Ministry of the Interior, Taiwan, 2014. Available from: http://sowf.moi.gov.tw/stat/year/103年內政統計年報電子書.pdf
Population Projections for R.O.C. (Taiwan). Taiwan National Development Council, Executive Yuan, Taiwan. 2014; 2014–2060.
Heriot AG, Tekkis PP, Smith JJ, Cohen CR, Montgomery A, Audisio RA, et al. Prediction of postoperative mortality in elderly patients with colorectal cancer. Dis Colon Rectum 2006;49:816–24.
Morson B. President’s address. The polyp-cancer sequence in the large bowel. Proc R Soc Med 1974;67:451–7.
Rabeneck L, Davila JA, Thompson M, El-Serag HB. Outcomes in elderly patients following surgery for colorectal cancer in the veterans affairs health care system. Aliment Pharmacol Ther 2004;20:1115–24.
Hardiman KM, Cone M, Sheppard BC, Herzig DO. Disparities in the treatment of colon cancer in octogenarians. Am J Surg 2009;197:624–8.
Nascimbeni R, Di Fabio F, Di Betta E, Salerni B. The changing impact of age on colorectal cancer surgery: A trend analysis. Colorectal Dis 2009;11:13–8.
Frasson M, Braga M, Vignali A, Zuliani W, Di Carlo V. Benefits of laparoscopic colorectal resection are more pronounced in elderly patients. Dis Colon Rectum 2008;51:296−300.
Kitagawa T, Hara M, Sano T, Sugimura T. The concept of Tenju-gann, or “natural-end cancer”. Cancer 1998;83:1061–5.
Liang JT, Huang KC, Lai HS, Lee PH, Jeng YM. Oncologic results of laparoscopic versus conventional open surgery for stage II or III left-sided colon cancers: A randomized controlled trial. Ann Surg Oncol 2007;14:109–17.
Nakamura T, Mitomi H, Onozato W, Sato T, Ikeda A, Naito M, et al. Oncological outcomes of laparoscopic surgery in elderly patients with colon cancer: A comparison of patients 64 years or younger with those 75 years or older. Hepatogastroenterology 2011;58:1200–4.
She WH, Poon JT, Fan JK, Lo OS, Law WL. Outcome of laparoscopic colectomy for cancer in elderly patients. Surg Endosc 2013;27:308–12.
The clinical outcome of surgical therapy (COST) study. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–9.
Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg 2004;91:1111–24.
Vallribera Valls F, Landi F, Espín Basany E, Sánchez García JL, Jiménez Gómez LM, Martí Gallostra M, et al. Laparoscopy-assisted versus open colectomy for treatment of colon cancer in the elderly: Morbidity and mortality outcomes in 545 patients. Surg Endosc 2014;28:3373–8.
Ong ES, Alassas M, Dunn KB, Rajput A. Colorectal cancer surgery in the elderly: Acceptable morbidity? Am J Surg 2008;195:344–8.
Smith JJ, Lee J, Burke C, Contractor KB, Dawson PM. Major colorectal cancer resection should not be denied to the elderly. Eur J Surg Oncol 2002;28:661–6.
Vignali A, Di Palo S, Tamburini A, Radaelli G, Orsenigo E, Staudacher C. Laparoscopic vs. open colectomies in octogenarians: A case-matched control study. Dis Colon Rectum 2005;48:2070–5.
Barrier A, Ferro L, Houry S, Lacaine F, Huguier M. Rectal cancer surgery in patients more than 80 years of age. Am J Surg 2003;185:54–7.
Violi V, Pietra N, Grattarola M, Sarli L, Choua O, Roncoroni L, et al. Curative surgery for colorectal cancer: Long term results and life expectancy in the elderly. Dis Colon Rectum 1998;41:291–8.
Stewart BT, Stitz RW, Lumley JW. Laparoscopically assisted colorectal surgery in the elderly. Br J Surg 1999;86:938–41.
Arnaud JP, Schloegel M, Ollier JC, Adloff M. Colorectal cancer in patients over 80 years of age. Dis Colon Rectum 1991;34:896–8.
Basili G, Lorenzetti L, Biondi G, Preziuso E, Angrisano C, Carnesecchi P, et al. Colorectal cancer in the elderly. Is there a role for safe and curative surgery? ANZ J Surg 2008;78:466–70.
Kesisoglou I, Pliakos I, Sapalidis K, Deligiannidis N, Papavramidis S. Emergency treatment of complicated colorectal cancer in the elderly. Should the surgical procedure be influenced by the factor ‘age’? Eur J Cancer Care (Engl) 2010;19:820–6.
Leong QM, Aung MO, Ho CK, Sim R. Emergency colorectal resections in Asian octogenarians: Factors impacting surgical outcome. Surg Today 2009;39:575–9.
Boereboom CL, Williams JP, Leighton P, Lund JN; Exercise Prehabilitation in Colorectal Cancer Delphi Study Group. Forming a consensus opinion on exercise prehabilitation in elderly colorectal cancer patients: a Delphi study. Tech Coloproctol. 2015;19:347–5
Chen BP, Awasthi R, Sweet SN, Minnella EM, Bergdahl A, Santa Mina D, et al. Four-week prehabilitation program is sufficient to modify exercise behaviors and improve preoperative functional walking capacity in patients with colorectal cancer. Support Care Cancer. 2017;25:33–40.
Carli F, Charlebois P, Stein B, Feldman L, Zavorsky G, Kim DJ, et al. Randomized clinical trial of prehabilitation in colorectal surgery. Br J Surg. 2010;97:1187–97.
Mastracci TM, Hendren S, O'Connor B, McLeod RS. The impact of surgery for colorectal cancer on quality of life and functional status in the elderly. Dis Colon Rectum. 2006;49:1878–84.
Amemiya T, Oda K, Ando M, Kawamura T, Kitagawa Y, Okawa Y, et al. Activities of daily living and quality of life of elderly patients after elective surgery for gastric and colorectal cancers. Ann Surg. 2007;246:222–8.
Lee YC, Huang YT, Tsai YW, Huang SM, Kuo KN, McKee M, et al. The impact of universal National Health Insurance on population health: the experience of Taiwan. BMC Health Serv Res 2010;10:225.
Acknowledgments
The authors would like to thank Professor Fu-Chang Hu for his guidance in data analysis and statistical editing.
The Contribution of Each Author
Tzu-Chun Chen, the first author, is responsible for the writing, data collection, and analysis for this article; Tung-Cheng Chang, the second author, supplied partial clinical patients and was involved the design and conduction of this study; Jin-Tung Liang, the corresponding author, supervised the analysis of the clinical data, study design, and writing of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, TC., Liang, JT. & Chang, TC. Should Surgical Treatment Be Provided to Patients with Colorectal Cancer Who Are Aged 90 Years or Older?. J Gastrointest Surg 22, 1958–1967 (2018). https://doi.org/10.1007/s11605-018-3843-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3843-5