Abstract
Background
Actual predictors of survival and recurrence for rectal cancer patients undergoing curative resection mostly come from pathological data of surgical specimen. Recently, novel blood biomarkers have been proposed as useful tools in cancer patient management, but few and conflicting data have been reported in rectal cancer. We evaluated the prognostic relevance of preoperative platelet-to-lymphocyte (P/L) ratio and neutrophil-to-lymphocyte (N/L) ratio on survival and recurrence in patients undergoing laparoscopic curative resection for rectal cancer.
Methods
All consecutive patients who referred for primary rectal disease to the Department of General Surgery in Cittadella (Italy) from June 2005 to September 2015 were retrospectively evaluated. Patients with metastatic disease at surgery were excluded. P/L and N/L ratios were calculated. For patients undergoing neoadjuvant chemo-radiotherapy, pre-treatment data were considered. Follow-up data were updated at December 2016.
Results
One hundred fifty-two patients were included in the study, 49 (32%) received neoadjuvant chemo-radiotherapy. Both P/L and N/L ratios showed poor discriminative performance on 5-year OS and DFS. Time-dependent ROC curves showed no improvements in discriminative performance of P/L and N/L ratios when considering different time endpoints. Multivariable analysis identified CEA—rather than P/L or N/L ratios—as independent predictor of OS and DFS, adjusting for age, tumor stage, and postoperative morbidity.
Conclusion
Neither P/L nor N/L ratios were associated with survival after rectal cancer surgery. Further studies on large series might provide insights on the role of these inexpensive blood biomarkers in rectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rectal cancer is one of the most common neoplasms worldwide.1 Results of treatment for rectal cancer have significantly improved in the last 30 years thanks to the introduction of and the adherence to the oncological principles of total mesorectal excision (TME): removal of the mesorectum to allow for minimal pelvic recurrence.2,3 In patients with local-advanced rectal cancer, TME combined with neoadjuvant chemo-radiotherapy has improved survival rate from 50% to over 70% in the last 30 years, and has reduced recurrence rate from 40% to less than 10%.4,5
In the last few years, several studies aimed to identify the subgroup of rectal cancer patients with unfavorable prognosis in term of survival and recurrence.6,7 An important but controversial topic is the definition of markers that could be associated with those patients who might benefit from adjuvant therapy.8 Most of the tools used by the clinicians to define “high-risk” rectal cancer patients rely on pathological examination of the surgical specimen, as depth of tumor invasion, nodal involvement, presence of distant metastases, perineural and lymphovascular invasion.9,10,11 However, the main drawback is that these markers can only be assessed after surgery.
Peripheral blood biomarkers, such as platelet-to-lymphocyte ratio (P/L ratio) and neutrophil-to-lymphocyte ratio (N/L ratio), have been used to preoperatively assess the prognosis in some gastrointestinal solid cancers, emphasizing on the effect of inflammatory response in tumor growth and metastatic diffusion.12,13,14,15,16,17,18,19,20 The precise role of cellular components of host inflammation (including platelets, lymphocytes, and neutrophils) in promoting/containing tumor progression is clearly not fully understood. However, the relationship between inflammation and cancer has been widely explored.21 A few mechanisms of host-tumor-inflammation relationship have been suggested, involving platelets (having protumor/neoangiogenetic effect), neutrophils (reflecting host response to systemic inflammation), and lymphocytes (reflecting host antitumor forces). Therefore, the ratios platelets/lymphocytes and neutrophils/lymphocytes might express the equilibrium between protumor (inflammatory pathway) and antitumor (immune response) forces.18,22
Although several studies already published on the prognostic role of P/L and N/L ratios, they investigated heterogeneous events (overall survival, disease-free survival, time to recurrence) and reported conflicting results. Moreover, few data have been made available specifically on rectal cancer, so far.23
The aim of this study was to evaluate the role of P/L and N/L ratios as prognostic biomarkers of oncological outcomes—namely, overall and disease-free survival—after laparoscopic resection with curative intent of non-metastatic rectal cancer (LCRRC).
Materials and Methods
Patients
We evaluated all consecutive patients who referred for primary rectal adenocarcinoma to the Department of General Surgery in Cittadella (Italy) from June 2005 to September 2015. Data were retrospectively retrieved from a prospectively collected dedicated database. We excluded from this study patients not operated on by laparoscopy, those not operated with curative intent, those with metastatic disease at surgery, and those with rectal resection as part of pelvic exenteratio due to other non-rectal primary malignancies.
Preoperative Staging and Treatment
Preoperative cancer staging included endoscopic ultrasound, abdominal CT scan, and/or pelvic MRI. All patients with locally advanced tumor (cT3-4 and/or N+) of the mid/low rectum on preoperative examinations received a long course of neoadjuvant chemo-radiotherapy (CRT) with continuous venous infusion of 5-FU or capecitabine and radiation treatment directed to the pelvis (4500 cGy). Surgery usually followed 8 weeks after completing the treatment. Standard oncological principles of TME were applied for rectal cancer resection. The rectal dissection was carried out at least 5 cm below the lower edge of the tumor with partial mesorectal resection for high-rectal tumors (rectal anterior resection, RAR), while in case of mid-/low-rectal tumors the dissection was extended to the pelvic floor and a complete mesorectal resection was accomplished (low anterior resection, LAR). A diverting ileostomy or colostomy was performed in patients who had received preoperative CRT for a locally advanced mid-/low-rectal tumor and underwent a total mesorectal excision.
Variables
Platelets, neutrophils, and lymphocytes were analyzed in routine blood tests. Blood samples from each patient were obtained within 1 week prior to surgery, during preoperative evaluation tests. For patients undergoing neoadjuvant CRT, pre-treatment hematologic data (1 week prior to CRT) were considered. Platelet-to-lymphocyte ratio was calculated as the absolute count of platelets divided by the absolute lymphocyte count. The neutrophil-to-lymphocyte ratio was calculated as the absolute count of neutrophil divided by the absolute lymphocyte count. Patient comorbidities were assessed using the American Society of Anesthesiologists (ASA) score24 and the Charlson Comorbidity Index (CCI).25 CCI calculation includes major comorbidities with different weight (1, 2, 3, or 6) according to their clinical relevance.
Follow-up
Patients were followed up routinely by the operating surgeon and seen at least once after discharge at 4 weeks after surgery and subsequently for oncological follow-up, on a regular basis, by the surgeon and/or oncologist with a combination of clinical examination, laboratory data, and radiological imaging. In the first 5 years after surgery, patients were seen every 6 months with CEA levels measured and thereafter yearly. Colonoscopy was performed at 12 and 48 months after surgery; abdominal CT scans and/or abdominal ultrasound every 6 months and then at 48 and 60 months; chest X-rays every 12 months for the first 5 years; chest CT scans every 12 months for the first 5 years.
Statistical Analysis
Continuous data were expressed as median and interquartile range (IQR). The correlation between continuous data was evaluated using Spearman rank correlation. The study endpoints were overall survival (OS) and disease-free survival (DFS), that were calculated according to proposed guidelines on cancer endpoints.26 DFS and relapse-free survival (RFS) overlapped in the present study, because no second primary cancers occurred during follow-up.27 Time-dependent receiver operating characteristic (ROC) curve analysis was used to assess the performance of P/L and N/L ratio in predicting survival outcomes.28 A subgroup analysis was performed to evaluate the performance of P/L ratio and N/L ratio according to neoadjuvant therapy, adjuvant therapy, age, and tumor stage. Time-dependent ROC curve analysis was also used to assess the performance of potentially relevant hematologic data (CEA and CA19.9) and of single components of P/L ratio and N/L ratio (lymphocyte, neutrophil, and platelet count) in predicting survival outcomes. Two Cox regression model were estimated to identify independent predictors of 5-year OS and of 5-year DFS among P/L ratio, N/L ratio, CEA, and CA 19.9, adjusting for age, CCI, neoadjuvant treatment, pTMN stage, and postoperative morbidity. Time-dependent ROC curves were estimated using R package “survival ROC”.28 Statistical analysis was performed using R 3.3.2 software (R Foundation for Statistical Computing, Vienna, Austria).29
Ethics
The study was conducted according to the Helsinki Declaration and patients gave their consent to have their data collected for scientific purposes. The study was approved by the local Ethics Committee (4131/U15/17).
Results
Patient Characteristics
One hundred and fifty-nine patients who underwent laparoscopic resection of primary rectal cancer with curative intent were retrospectively evaluated. Seven patients were excluded, due to incomplete hematologic data on clinical charts (6 patients) or idiopathic thrombocytopenic purpura (1 patient with Werlhof’s disease), thus 152 patients were included in the study. Patient characteristics are presented in Table 1. Median age was 70 years (IQR 59–76). One third of the patients received neoadjuvant CRT, 36 (23.7%) adjuvant chemotherapy. The completeness of TME was achieved in 143 out of 152 patients (94.1%), while the margin of the specimen was positive only in one patient (0.7%). Postoperative surgical complications occurred in 17 patients (11.2%), including ileus (6 patients), anastomotic leak (4 patients), abdominal collection (2 patients), colonic ischemia (2 patients), hemorrhage (1 patient), ileal volvulus (1 patient), and substenosis of the ileostomy (1 patient).
Hematologic Data
Hematologic data are presented in Table 2. Platelet and neutrophil count were correlated (rho 0.23, p < 0.0001), as well as P/L ratio and N/L ratio (rho 0.58, p < 0.0001). Age was not correlated with hematologic data (lymphocyte count: rho − 0.08, p = 0.35; neutrophil count: rho − 0.04, p = 0.63; platelet count: rho − 0.03, p = 0.67; N/L ratio: rho 0.02, p = 0.81; P/L ratio: rho 0.07, p = 0.41).
Survival
The 5-year OS was 78% and the 5-year DFS was 74%, with a median follow-up of 59 months (IQR 33–76). Nineteen patients (12.5%) had distant recurrence alone, and 7 patients (4.6%) had both local and distant recurrence.
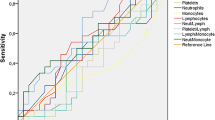
Both P/L ratio and N/L ratio showed poor discriminative performance regarding 5-year OS (AUC: 0.45 and 0.47, respectively) and 5-year DFS (AUC: 0.48 and 0.47, respectively) (Fig. 1). Time-dependent ROC curves showed no improvements in discriminative performance of P/L ratio and N/L ratio regarding different time endpoints (1, 2, 3, 4, and 5 years; Fig. 2). AUCs of ROC curves are reported in Supplementary Table 1.
In addition, the single components of P/L ratio and N/L ratio had poor discriminative performance regarding 5-year OS (AUC: lymphocyte count 0.52, neutrophil count 0.47, platelet count 0.41) and 5-year DFS (AUC: lymphocyte count 0.52, neutrophil count 0.52, platelet count 0.42).
The discriminative performance of P/L ratio, N/L ratio, CEA, and CA 19.9 was compared in 119 patients who had complete hematologic data. All the hematologic parameters showed low discrimination regarding both 5-year OS and 5-year DFS (AUCs < 0.70; Fig. 3). Multivariable analysis identified CEA—rather than P/L ratio, N/L ratio, or CA 19.9—as independent predictor of both OS and DFS (Table 3), adjusting for age, Charlson Comorbidity Index, neoadjuvant treatment, pTMN stage, and postoperative morbidity.
Subgroup Analysis
The discriminative performance of P/L ratio and N/L ratio regarding 5-year OS and 5-year DFS was assessed in subgroups of patients according to neoadjuvant therapy, adjuvant therapy, age, and tumor stage (Supplementary Table 2). The discriminative performance of P/L ratio and N/L ratio was low in any subgroup (Fig. 4).
Discussion
The present study aimed to assess the role of P/L and N/L ratios as prognostic markers after laparoscopic resection with curative intent of non-metastatic rectal cancer patients. These blood biomarkers are inexpensive and readily available as preoperative assessment in any rectal cancer patient.
Previous studies suggested a relationship between peripheral blood biomarkers, inflammatory pathway, and immune response.18 In addition, these biomarkers might provide some advantages over the pathological prognostic evaluation (i.e., tumor invasion, nodal involvement, presence of distant metastases, perineural and lymphovascular invasion), because the latter is more expensive and can only be assessed after surgery.8,9,10,11 The prognostic role of P/L ratio and N/L ratio has been investigated in gastrointestinal solid cancers12,13,14,15,16,17,18,19,20, but few data and conflicting findings have been reported in rectal cancer.23
In our series, the discrimination of both P/L ratio and N/L ratio was poor regarding both 5-year OS and 5-year DFS. The analysis at different time points (1, 2, 3, 4, and 5 years) confirmed such poor discrimination even at short term. In addition, the single components of P/L ratio and N/L ratio (lymphocyte count, neutrophil count, and platelet count) showed poor discrimination as well. Multivariable analysis identified CEA as independent predictor of survival; nevertheless, CEA had low discrimination as showed by ROC curve analysis.
Our findings add to the few data available for P/L and N/L ratios in rectal cancer patients undergoing curative surgery and to the conflicting results of larger heterogeneous studies in which the subgroup of rectal cancer patients are usually less than 20%.20
To our knowledge, only two studies evaluated the prognostic effect of both P/L and N/L ratios in rectal cancer patients undergoing resection. Carruthers et al.30 analyzed 115 UK patients undergoing preoperative chemo-radiotherapy and found that only N/L ratio (≥ 5) was significantly associated with OS, DFS, and time to local recurrence, with a nearly 3-fold difference in median survival between patients with and without elevated N/L ratio. Toiyama et al.31 reported on 89 Japanese patients with locally advanced rectal cancer who underwent neoadjuvant chemoradiation treatment followed by TME surgery. Platelets and N/L ratio predicted OS, while platelets were the only biomarker independently predicting DFS and recurrence, along with lymph node involvement. In our series, subgroups analysis according to neoadjuvant therapy, adjuvant therapy, age, and tumor stage confirmed the poor discrimination of both P/L ratio and N/L ratio.
A recent systematic review reported the findings of four studies from Eastern countries that showed an association between N/L ratio and OS in rectal cancer,23 but a recent Chinese study on 202 rectal cancer patients showed no prognostic role at all for N/L ratio.32 In addition, a recent systematic review on P/L ratio did not find any significant association between P/L ratio and survival in rectal cancer patients.20
The limitations of the study include the retrospective design and the single institution series. However, selection bias has been avoided by the inclusion of all consecutive LCRRC that were performed during the study period. Moreover, the completeness of data has been achieved by standardized surveillance program with prospective collection of data in an electronic database and by updating follow-up information before the analysis, thus mitigating the common weakness of retrospective studies.
The strengths of this study rely in the inclusion of only rectal cancer patients, thus avoiding the analysis of a miscellaneous colorectal cohort, and in the sample size, which is one of the largest so far. In addition, all patients had a close clinical/radiological follow-up to properly assess survival and recurrence. Despite the two previous studies on rectal cancer included only patients receiving neoadjuvant therapy,30,31 we included both patients with and without neoadjuvant treatment, in order to provide a “real” picture of the role of the biomarkers. For patients receiving preoperative CRT, we considered pre-treatment hematological values, to avoid the effects of systemic treatments on patient immunological status and on blood counts. Similarly, we included all stage III patients receiving adjuvant chemotherapy, because this treatment has become the standard of care for stage III patients. P/L ratio and N/L ratio have been evaluated as continuous variables without suggesting any cutoffs, in order to avoid the risk of dichotomizing continuous variable.33 Finally, we performed a sub-analysis that confirmed the main findings in subgroups of patients according to neoadjuvant therapy, adjuvant therapy, age, and tumor stage. Our data confirmed the heterogeneity of findings on this topic in literature, with lack of agreement regarding the optimal cutoff value and the prognostic effect of P/L and N/L ratios. Interestingly, all but one of the previous studies were from Eastern populations (China, Korea, or Japan) and overall included less than 1000 patients, altogether. This might explain—at least in part—the differences with our results, but to date, it represents just a speculation.
Conclusions
In conclusion, we reported one of the few and largest experience on the role of both P/L and N/L ratios as potential prognostic blood biomarkers for patients undergoing laparoscopic curative TME rectal cancer resection. Neither of these ratios significantly contributed as independent predictor of OS and DFS. Tumor features and postoperative pathological cancer staging system currently remain the “gold” standard in defining prognosis and in suggesting postoperative management and surveillance programs in rectal cancer. Future studies on large series of rectal cancer patients might provide further knowledge on this topic and help clinicians in treatment decision making with the use of inexpensive blood biomarkers.
References
Torre LA, et al. (2015). Global cancer statistics, 2012. CA Cancer J Clin 65:87–108.
Heald RJ, et al. (1982) The mesorectum in rectal cancer surgery: the clue to pelvic recurrence? Br J Surg 69:613–616.
Rutten HJ, et al. (2008) Controversies of total mesorectal resection for rectal cancer in elderly patients. Lancet Oncol 9:494–501.
Slaney G. (1971) Results of treatment of carcinoma of the colon and rectum. Mod Trends Surg 3:69–89.
Kapiteijn E, et al. (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345:638–646.
Kusters M, et al. (2010) Patterns of local recurrence in rectal cancer; a study of the Dutch TME trial. Eur J Surg Oncol 36:470–476.
Marks JH, et al. (2016) Outcomes in 132 patients following laparoscopic total mesorectal excision (TME) for rectal cancer with greater than 5-year follow-up. Surg Endosc 30:307–314.
Breugom AJ, et al. (2015) Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol 16:200–207.
Edge S, et al. (2010) AJCC cancer staging manual, 7th ed. New York: Springer.
Nagtegaal ID, et al. (2002) Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol 26:350–7.
Cienfuegos JA, et al. (2015) Impact of perineural and lymphovascular invasion on oncological outcomes in rectal cancer treated with neoadjuvant chemoradiotherapy and surgery. Ann Surg Oncol 22:916–923.
Feng JF, et al. (2013) Clinical significance of preoperative neutrophil lymphocyte ratio versus platelet lymphocyte ratio in patients with small cell carcinoma of the esophagus. Scientific World Journal 2013:504365.
Gunaldi M, et al. (2015) Prognostic impact of platelet/lymphocyte and neutrophil/lymphocyte ratios in patients with gastric cancer: a multicenter study. Int J Clin Exp Med 8:5937–5942.
Kinoshita A, et al. (2012) Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer 107:988–993.
Smith RA, et al. (2009) Preoperative platelet-lymphocyte ratio is an independent significant prognostic marker in resected pancreatic ductal adenocarcinoma. Am J Surg 197:466–472.
Kwon HC, et al. (2012) Clinical significance of preoperative neutrophil-lymphocyte ratio versus platelet-lymphocyte ratio in patients with operable colorectal cancer. Biomarkers 17:216–222.
Szkandera J, et al. (2014) The elevated preoperative platelet to lymphocyte ratio predicts decreased time to recurrence in colon cancer patients. Am J Surg 208:201–214.
Li MX, et al. (2014) Prognostic role of neutrophil-to-lymphocyte ratio in colorectal cancer: a systematic review and meta-analysis. Int J Cancer 134:2403–2413.
Choi WJ, et al. (2015) Preoperative neutrophil-to-lymphocyte ratio is a better prognostic serum biomarker than platelet-to-lymphocyte ratio in patients undergoing resection for non-metastatic colorectal cancer. Ann Surg Oncol 22:S603–616.
Gu X, et al (2016) Elevated platelet to lymphocyte ratio is associated with poor survival outcomes in patients with colorectal cancer. PLoS One Sep 22;11(9):e0163523.
Grivennikov SI, et al. (2010) Immunity, inflammation, and cancer. Cell 140:883–899.
Sierko E, et al. (2004) Platelets and angiogenesis in malignancy. Semin Thromb Hemost 30:95–108.
Dong YW, et al. (2016) Prognostic significance of neutrophil-to-lymphocyte ratio in rectal cancer: a meta-analysis. Onco Targets Ther 9:3127–3134.
Al-Homoud S, et al. (2004) Evaluating operative risk in colorectal cancer surgery: ASA and POSSUM-based predictive models. Surg Oncol 13:83–92.
Charlson M, et al. (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245–51.
Punt CJ, et al. (2007) Endpoints in adjuvant treatment trials: a systematic review of the literature in colon cancer and proposed definitions for future trials. J Natl Cancer Inst 99:998–1003.
Birgisson H, et al. (2011) Survival endpoints in colorectal cancer and the effect of second primary other cancer on disease free survival. BMC Cancer 11:438.
Heagerty PJ, et al. (2013). Survival ROC: time-dependent ROC curve estimation from censored survival data. R package version 1.0.3. URL https://CRAN.R-project.org/package=survivalROC
R Core Team (2016). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
Carruthers R, et al. (2012) Systemic inflammatory response is a predictor of outcome in patients undergoing preoperative chemoradiation for locally advanced rectal cancer. Colorectal Dis 14:e701-e707.
Toiyama Y, et al. (2015) Elevated platelet count as predictor of recurrence in rectal cancer patients undergoing preoperative chemoradiotherapy followed by surgery. Int Surg 100:199–207.
Shen J, et al. (2017) Prognostic role of neutrophil-to-lymphocyte ratio in locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Med Sci Monit 23:315–324.
Cavallin F, et al. (2013) The effect of dichotomizing age in outcomes assessment of the surgical management of esophageal cancer. Ann Thorac Surg 95:2210–2211.
Author information
Authors and Affiliations
Contributions
- Conception and design: G Portale, A Valdegamberi, F Cavallin, F Frigo, V Fiscon
- Acquisition of data: G Portale, A Valdegamberi, F Cavallin
- Analysis and interpretation of data: G Portale, F Cavallin, A Valdegamberi, F Frigo, V Fiscon
- Drafting of the manuscript: G Portale, F Cavallin, A Valdegamberi, F Frigo, V Fiscon
- Revising of the manuscript: G Portale, F Frigo, V Fiscon
Corresponding author
Ethics declarations
Conflict of Interest
None of the authors has conflict of interest to disclose
Electronic supplementary material
ESM 1
(DOC 52 kb)
Rights and permissions
About this article
Cite this article
Portale, G., Cavallin, F., Valdegamberi, A. et al. Platelet-to-Lymphocyte Ratio and Neutrophil-to-Lymphocyte Ratio Are Not Prognostic Biomarkers in Rectal Cancer Patients with Curative Resection. J Gastrointest Surg 22, 1611–1618 (2018). https://doi.org/10.1007/s11605-018-3781-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3781-2