Abstract
Introduction
The role of laparoscopic TME for rectal cancer is still questioned as a safe and adequate cancer operation. Currently, multicenter randomized prospective trials are underway to evaluate this. We analyze our long-term results using laparoscopic TME in the treatment of rectal cancer to evaluate its oncologic outcomes.
Methods
A prospective laparoscopic database was queried to identify all patients operated upon for rectal cancer from April 1997 to September 2007. In total, 151 patients were identified. Metastatic disease excluded 19 patients, leaving 132 patients to be analyzed for perioperative and 5-year oncologic outcomes. Procedures included LAR, n = 35; transanal abdominal transanal proctosigmoidectomy, n = 77; and APR, n = 20. All surgeries were TME or pTME.
Results
Laparoscopic TME was performed on 89 men (67 %), mean age 61 (22–85). Preoperative chemoradiation was administered in 119 (90.2 %) with median dose of 5500 cGy (3800–10,080). Mean EBL was 300 ml, and 4.5 % were transfused. Seven patients (5.3 %) underwent conversion, 5 to lap-assisted, with a 1.5 % conversion rate to open. Pathologic stage of disease: complete response: 24 %; I: 36 %; II: 22 %; III: 18 %. There were no mortalities. Overall morbidity was 23.5 %, with no anastomotic leaks and 5 (3.8 %) delayed anastomotic stricture/fistula. There were no port site recurrences. Mean follow-up was 69.4 months (7.6–168.0). Overall LR was 5.3 % (n = 7). There was only one isolated LR (0.8 %). Mean time to local recurrence was 13.9 months. Metastatic rate was 18.2 %. By stage, disease-specific survival was: CR 86.3 %; I: 87.4 %; II: 86.4 %; III: 77.4 %. Overall, 5-year survival was 84.8 %.
Conclusion
The long-term data confirm that laparoscopic TME can be performed with lasting low local recurrence (5.3 %) and excellent 5-year survival (84.8 %). This report’s importance stems from it representing one of the largest experiences of rectal cancer treated by laparoscopic TME with greater than 5-year follow-up reported in the literature.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Total mesorectal excision (TME) is the gold standard for rectal cancer resection. Its adoption has led to improved oncologic outcomes. Initially described by Professor Heald in 1986, TME has been largely studied in open surgery and is properly regarded as the standard of care for operative approach in rectal cancer. It is defined as sharp dissection and “complete removal of the lymph node bearing mesorectum along with its intact enveloping fascia.” Sharp scissor dissection is used to stay within the avascular plane between visceral and somatic structures, thus avoiding tearing into “fragile tumour planes” which can compromise cancer clearance [1–3]. In the Norwegian rectal cancer trial published in 2002, the adoption of TME demonstrated a reduction in local recurrence from 12 to 6 % with improvement in 4-year survival rates from 60 to 73 %. This suggested that improved surgical technique can positively affect outcomes which were further aided with the implementation of chemoradiotherapy [4–7]. However, the ability to recreate these results using a laparoscopic approach has been questioned.
The advent of minimally invasive surgical technique has demonstrated clear advantages in many fields of surgery. Decreased pain, faster return of bowel function, less blood loss, and shorter length of stay with similar complication rates to open surgery have been consistent findings in the literature [8, 9]. The laparoscopic treatment of colon cancer has gained acceptance as being comparable, if not superior oncologically to open surgery, while retaining these same advantages. From an oncologic standpoint, the COSTSG trial, as well as other trials, has demonstrated a laparoscopic approach to colon cancer is equally as safe and effective as open surgery. With outcomes including time to recurrence, disease-free survival, overall survival, and complications studied, none were inferior using a laparoscopic approach [10–14]. However, utilization of laparoscopy in rectal cancer has been challenged due to the inherent difficulty of rectal cancer surgery. The steep learning curve and challenges in working in the narrow confines of the pelvis have created these barriers and raise questions whether adequate TME can be performed laparoscopically [15–17]. There are several excellent experiences reported in the literature demonstrating the safety of laparoscopic TME and its short-term oncologic outcome [18–23]. However, there is a paucity of long-term data, with 5-year follow-up, regarding the laparoscopic approach implementing TME. To date, studies with shorter follow-up or surrogate markers for oncologic outcome, such as completeness of TME, have been reported.
There are several ongoing prospective randomized trials underway designed to definitively address whether rectal cancer can effectively be performed laparoscopically. The UK MRC CLASICC trial raised initial concerns regarding the adequacy of a laparoscopic approach in rectal cancer as there was an increased pathologic circumferential margin (CRM) positivity within the laparoscopic anterior resection group, which while not statistically significant was high at 16 versus 14 % in the open group (p = 0.8) [24]. This, however, did not translate into a difference in local recurrence, disease-free survival, and overall survival at 3 and 5 years between the laparoscopic and open groups [25, 26]. The recently closed American College of Surgeons Oncology Group (ACOSOG)-Z6051 trial is testing the hypothesis that a laparoscopic approach is not inferior to open resection in patients with Stage IIA, IIIA, or IIIB rectal cancer treated with neoadjuvant therapy. Rather than wait for the long-term data to mature, the study is designed using surrogates for cancer outcomes with CRM >1 mm, distal resection margin >2 cm, and completeness of TME to evaluate the efficacy of the laparoscopic approach. Among its secondary outcomes are local pelvic recurrence and disease-free survival rates at 2 years [27]. The European colon cancer laparoscopic or open resection (COLOR) II trial is an international, multi-institutional study also using the pathologic completeness and quality of TME as a surrogate for outcome with its primary endpoint as locoregional recurrence at 3 years [28]. Furthermore, if a TME performed laparoscopically is proved noninferior, can it be inferred that other platforms such as robotics, with its stereoscopic view and more meticulous dissection, can also be utilized or even enhance outcomes? [29] While ultimately these trials will give the surgical community important information regarding long-term oncologic outcomes, it will take many years for the final results to be available.
To address the question of long-term oncologic outcomes for rectal cancer treated by laparoscopic TME, we report our experience in patients operated on 5 or more years ago.
Methods
Patient selection
A query of a prospective database of laparoscopic colorectal surgeries performed by a single colorectal surgeon from April 1997 to September 2012 identified 1522 consecutive laparoscopic cases. From April 1997 to September 2007, 151 rectal cancers with laparoscopic total or partial mesorectal excisions were performed. Nineteen patients were excluded due to metastatic disease, leaving 132 patients available for oncologic review with a 5-year follow-up. Follow-up was performed in an ongoing fashion and recorded in the database via prospective chart review, consulting health-care providers, and direct patient contact for disease status.
These patients were treated as part of an ongoing rectal cancer management program. As part of our rectal cancer management pathway, the need for neoadjuvant chemoradiation was determined by T stage on presentation, tumor location, and tumor fixity. Preoperative tumor location was measured as distance from the anorectal ring with distal third defined as 0–2.9 cm, middle third as 3–6.9 cm, and proximal third 7 cm and higher. Patients were staged with endorectal ultrasound and MRI as well as clinically. Those with unfavorable cancers, defined as T3 or N+, at any level in the rectum, as well as all cancers located in the distal 1/3 of the rectum, received neoadjuvant therapy. Chemotherapy consisted of 5FU continuous venous infusion (CVI) or capecitabine. Radiation therapy comprised of high-dose radiation dosed to a preferred goal of 5580, 4500 cGy delivered to the pelvis followed by a boost of 1080 cGy to the tumor and the presacral hollow [30, 31]. To allow maximal tumor regression, final assessment for the consideration of sphincter preservation was performed after an 8- to 12-week interval. All decisions on sphincter preservation were based on the postirradiated stage of the rectal cancer. Sphincter preservation surgery (SPS) was performed on all cancers except those that remained fixed in the distal third of the rectum. Diverting stomas were utilized for all patients with cancers in the distal third of the rectum and those who underwent neoadjuvant chemoradiation. All stapled anastomoses were performed laparoscopically with an EEA stapler intracorporally.
Data review
Preoperative demographics, perioperative data points, and postoperative factors were compared. Preoperative factors included age, gender, ASA, body mass index, prior abdominal surgery, and prior incisions. Perioperative factors included estimated blood loss, operative time, need for conversion, need for blood transfusion, number of incisions, and longest incision length. A case was considered a conversion if a hand-assist port or open laparotomy was performed. Postoperative factors included time to bowel function and diet advancement, hospital length of stay, immediate and delayed morbidity, and 30-day mortality. Major morbidities included anastomotic leaks, strictures, or fistulas, return to the operating room, wound infections, prolonged ileus or obstruction, and port site recurrences. Minor morbidities included postoperative arrhythmias, hernias, and urinary tract retention.
Tumor characteristics were recorded before and after chemoirradiation based on level from the anorectal ring, position, fixity, radiographic and clinical stage, neoadjuvant radiation and dosage, and ypTN stage. A successful TME is determined by the surgeon as well as pathologic evaluation of the resected specimen. Local and distant failures are identified by clinical examination, laboratory evaluation, and imaging. Primary oncologic outcomes were measured in local recurrence, distant metastasis, disease-specific survival, and overall survival.
Patients were closely followed with a cancer surveillance protocol through a combined modality of clinical examinations, laboratory data, and radiographic imaging. In the first 2 years after surgery, patients were seen every 3 months with CEA levels measured. During years 3 and 4, this was extended to every 4 months, then every 6 months in year 5. Either a flexible sigmoidoscopy or colonoscopy was performed at 6-month interval for the first 2 years followed by yearly thereafter. After 5 years, patients were followed yearly. CAT scans are performed at 6 months, then 1 year postoperatively, and then yearly.
Data analysis
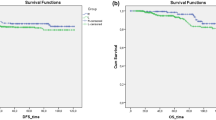
Statistical analysis was performed using the Chi-square test, and survival measured using the Kaplan–Meier 5-year survival curves.
Results
Demographics
During the 10-year study period, 132 patients underwent laparoscopic TME for rectal cancer. Of these, 67 % were men. Mean age was 61 (22–85) years old, and mean BMI was 25.9 (15.6–39.5). This included 73 patients (55 %) with BMI over 25, and 24 patients (18.1 %) with BMI >30. ASA class was III or IV in 49.2 %. There were 36 patients (27.3 %) with prior abdominal surgery, of which 15 (11.4 %) involved prior pelvic surgeries. Two additional patients had prior abdominal incisions from abdominoplasties. Please see Table 1 for demographic summary.
Preoperative tumor characteristics
The tumor was located in the distal third in 71 % of cases. Tumor fixity was assessed clinically with 47.6 % mobile lesions, 36.2 % tethered, and 16.2 % fixed lesions. Preoperative T staging was as follows: T1: 1.9 %, T2: 23.1 %, T3: 74 %, and T4: 0.96 %.
Mean CEA was 2.21 (0.4–32.1) and mean albumin 3.8 (2.0–4.8) (Table 2).
Procedures performed
Using our rectal cancer selection algorithm, sphincter preservation was achieved in 84.8 % of patients. Laparoscopic LAR was performed in 35 patients (26.5 %), TATA in 77 (58.3 %), and APR in 20 patients (15.1 %). Preoperative radiation was administered in 119 (90.2 %) patients with mean dose 5535 cGy (3800–10,080) (Table 2).
Clinical outcomes
Mean operative time was 391 (91–730) min. Median estimated blood loss was 300 cc (25–5000 cc) with six patients (4.5 %) requiring perioperative blood transfusions. In total, 60.6 % of patients had a handsewn coloanal anastomosis. Conversion rate was 5.3 % with five patients being converted to laparoscopic assisted and 1.5 % (n = 2) to an open laparotomy. The mean largest incision length was 4.1 cm (1.2–9.2 cm) with the exclusion of the patients with open laparotomy. Reasons for conversion to open were secondary to bleeding in one and a low cancer with the lack of progression in an obese patient in the second. The mean specimen length was 32.9 cm. Mean number of lymph nodes harvested was 11.7 (1–93).
Postoperative course reveals the median time to flatus and bowel movement was 2 and 2 days, respectively. The median time to clears and house diet was 1 and 3 days, respectively. Patients were discharged at a median of 5 days postoperatively (Table 3).
Overall morbidity was 23.5 % with the majority (15.1 %) of these representing minor morbidities. There was a 1.5 % wound infection rate, and 6.8 % had ileus or small bowel obstruction. There were no clinically apparent anastomotic leaks; however, there was a 3.8 % rate of delayed anastomotic stricture or fistula.
Specifically, prolonged ileus/small bowel obstruction occurred in 9 patients (6.8 %), wound infection in 2 (1.5 %), arrhythmia in 5 (3.8 %), urinary retention in 4 (3.0 %), wound separation in 1 (0.8 %), right arm neuropraxia in 5 (3.8 %), and other in 4 (3.0 %) . There was 1 intraperitoneal bleed (0.8 %). There was no need for return to the operating room. There were no port site recurrences. There were no perioperative mortalities (Table 4).
There were 25 (18.9 %) delayed morbidities including abscess/wound infection and hernia each in 4 patients (3.0 %), anastomotic stricture/fistula in 5 (3.8 %), rectal prolapse in 5 (3.8 %), DVT/thrombosis in 2 (2.5 %), and other in 5 (3.8 %) (Table 4).
Oncologic outcomes
Mean length of follow-up was 69.4 months (7.6–168.0 mo.). Pathologic staging was as follows: Stage 0: 24 %, Stage I: 36 %, Stage II: 24 %, Stage III: 17 %. Overall, local recurrences occurred in 7 patients (5.3 %) with 6 (4.5 %) presenting with concurrent distant metastasis. Only 1 patient (0.8 %) had isolated local recurrence discovered on vaginal examination 1.5 years after APR. By stage, there were no local failures in 24 % of patients who had achieved complete pathologic response. Those with Stage I disease had a 4.3 % local recurrence rate. Those with Stage II disease had a 9.7 % local recurrence rate. Stage III disease patients were found to have a 8.7 % local recurrence rate. Between stages, there was no statistical significance except between Stage 0 and Stage III (Table 5). Mean time to local recurrence was 13.9 months. By level, all local recurrences were found in those with tumors in the distal third of the rectum with the highest recurrence of 15 % in those who required APR (Table 5). With SPS, local recurrence was 3.6 % which was not statistically significant compared with APR (p = 0.31).
Metastatic disease rate was 18.2 %. By stage, distant metastasis rate increased with increasing stage. Stage III patients did statistically worse compared with all other stages with its higher metastatic failure (p = 0.0008–0.027). By procedure, distant metastasis was greatest in those undergoing APR at 30 %. There was no statistical difference in local recurrence or metastasis by procedure (p = 0.32–0.61). There were 18 patients (13.6 %) presenting with distant metastasis alone (Table 5).
Overall, disease-specific survival was 84.8 %. This was similar at ~87 % among those with complete response, Stage I, and Stage II. Those with nodal disease had decreased survival at 77.4 % at 5 years which was not statistically significant (p = 0.38). Overall survival was 85 % at 60 months (Table 5).
Discussion
With 5-year follow-up, laparoscopic TME for rectal cancer can be performed safely with low morbidity and mortality, low local recurrence rates of 5.3 %, and distant metastatic rate of 18.2 %. We found excellent 5-year disease-specific survival of 84.8 % and overall survival of 85 %. This is comparable to that of open TME which has local recurrence rates of 4–8 % and cancer-specific survival rates of 70–80 % at 5 years [32, 33].
Our study demonstrates the technical feasibility of performing a successful TME laparoscopically despite challenges inherent in working in the pelvic confines. There have been concerns regarding high conversion rates ranging from 11 % in the Barcelona trial to as high as 29 % in the MRC CLASICC trial which was even higher at 34 % in the rectal arm [24, 34]. We demonstrate a low conversion rate of 5.3 %, with an open conversion of only 1.5 %. This much lower rate is in keeping with other single-center experiences doing high-volume rectal work whose conversion rates range from 3.0 to 15.1 % [20, 35, 36]. Proponents of laparoscopic TME maintain the preservation of TME principles commonly with the placement of five trocars to perform sharp pelvic dissection in the avascular plane separating the parietal layer of pelvic fascia and the visceral fascia of the mesorectum. This technique preserves the autonomic nerves with en-bloc removal of the rectum and its associated mesorectum with uninvolved circumferential and distal resection margins. High ligation of the IMA is performed [20, 29, 34]. An advantage to laparoscopy is the improved visualization of critical urologic, and neurovascular structures permitting facilitation of the sharp dissection required with TME. Certainly, expertise comes hand in hand with experience and the learning curve associated with it, but with adequate training, technical feasibility is attainable. The technically challenging aspect of laparoscopic TME has led many to propose robotic and now bottoms-up approaches; however, it will be some time until long-term results are available in this patient population.
Our morbidity rate of laparoscopic TME of 23.5 % is comparable to that of other published studies which range from 18 to 37 % [20, 35]. Even with over 70 % of our patient population with cancers in the distal 1/3 of the rectum, we were able to maintain a low anastomotic leak rate of 3.8 %. This compares favorably with that of reported open studies including that from Dr. Heald’s group of 11 % as well as the Dutch Colorectal Cancer Group Trial of 12 %. Proximal diversion for low rectal cancers was routinely performed, likely contributing to our low leak rates. Perhaps, there were subclinical leaks that were evident only through secondary sequelae such as stricture or abscess on delayed imaging studies.
The question driving this study was: Can TME be safely and effectively performed laparoscopically without compromising oncologic outcomes? The paucity of long-term data regarding the laparoscopic approach implementing TME for rectal cancer and whether exposure in the pelvis is truly adequately performed to attain complete tumor and mesorectal resection has bred the prospective trials that are currently underway in Europe, Asia, and the USA.
Early long-term results of laparoscopic TME for rectal cancer support the use of laparoscopic TME for rectal cancer. Our finding of local recurrence of 5.3 % and disease-specific survival of 84.8 % is similar to other studies. Leroy et al. described the successful application in 102 consecutive unselected patients over a 9-year period with a 3 % conversion rate to open. Forty percent of patients were treated to 4500 cGy, and surgery performed 4–6 weeks after the completion of neoadjuvant therapy. Their overall morbidity rate of 27 % was similar to our rate of 23.5 %. Their 30-day mortality rate of 2 % was higher than that in our study group. With at least 6-month follow-up and a mean follow-up of 36 months, Leroy et al. [20] achieved at least comparable oncologic outcomes to that reported in open TME with a 6 % local recurrence and cancer-specific survival of 75 % at 5 years.
More recent comparative data have shown similar long-term and cancer-free survival between open and laparoscopic surgery. Laurent et al. published their 5-year data with a median follow-up of 52 months with nonsignificant morbidity rates of 37.7 % in the open cases versus 32.0 % in the laparoscopic arm. Their laparoscopic local recurrence rate was slightly lower than ours at 3.9 % and cancer-free survival comparable at 82 %. However, their conversion rate of 15 % was much higher than ours of 5.3 %. Converted cases were not found to adversely affect oncologic outcomes [36].
Our results are comparable to the conclusions of the recently published CLASICC long-term 5-year data where patients undergoing laparoscopic rectal cancer surgery had a median overall survival was 82.7 (67.3–97.6) months and disease-free survival of 70.8 (52.1–90.0) months. There was a trend toward improved overall survival in the laparoscopic group compared with open surgery, though this was only significant in early survival. They concluded that this finding “should encourage surgeons to use laparoscopic surgery in patients with rectal cancer” [37]. By procedure, those undergoing an APR were associated with worse DFS than anterior resection (p = 0.005), though there was no difference by randomized procedure approach. Local recurrence was found to be 10.9 % for all colorectal patients with no significant differences observed between anterior resection (9.9 %) and APR (15.3 %) (p = 0.078). Distant recurrence was found to be higher in those undergoing APR (37.7 %) compared with anterior resection (24.3 %) though there was no difference whether it was performed open, laparoscopic, or a converted procedure [37]. Hence, the factors necessitating an APR as the resection type contributed more to one’s oncologic outcomes and survival than the operative approach itself. We also noted this trend in APRs though it did not reach significance. Early concerns regarding laparoscopic TME leading to higher positive circumferential resection margins as well as intraoperative conversions did not translate into differences in long-term overall survival and DFS, again similar to our findings.
There are several limitations of this descriptive study. One, all cases were performed by a single surgeon with advanced laparoscopic training and expertise. Thus, the reproducibility of the results of this study among those with less experience may initially vary until proficiency is reached. Second, in comparison with published reports, our practice employs a high-dose neoadjuvant radiation regime contributing to our high sphincter preservation rates. There is also variability in imaging surveillance protocols, radiation oncologic protocols with improved chemotherapeutic agents, and minor variances in laparoscopic TME technique as would be expected during the 10-year study period. Also our study did not stratify patients into laparoscopic versus open approaches by the same surgeon; thus, direct comparative outcomes were not measured. In later years, this was done as part of the ACOSOG trial. Finally, this is a retrospective review of a prospectively maintained database and suffers the drawbacks inherent in this arrangement.
In summary, our single-institution experience with laparoscopic TME suggests that the procedure is safe and has similar morbidity and tumor-free survival compared with published open TME experience. The strength of this report is that this is actual 5-year follow-up for all patients and does not rely on other surrogates, such as TME completeness, as predictors for outcome. Furthermore, no rectal cancer patient operated on laparoscopically without metastatic disease during this period was excluded in the LR or survival data. While we all await the results of the large prospective trials such as the ACOSOG Z6051 trial, this study represents one of the largest experience of rectal cancer treated by laparoscopic TME with greater than 5-year follow-up and demonstrates excellent long-term oncologic outcomes. As these randomized studies reach maturity, greater adoption of minimally invasive approaches to rectal cancer is to be expected. We are hopeful that the above-presented long-term data on laparoscopic TME coupled with the randomized trial results will generate more widespread adoption of minimally invasive surgical approaches for rectal cancer patients.
References
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1:1479–1482
Nogueras JJ (2012) Open low anterior resection. In: Wexner SD, Fleshman JW, Fischer JE (eds) Master techniques in general surgery: colon and rectal surgery: abdominal operations. Lippincott Williams & Wilkins, Philadelphia, pp 127–131
Wibe A, Møller B, Norstein J, Carlsen E, Wiig JN, Heald RJ, Langmark F, Myrvold HE, Søreide O (2002) A national strategic change in treatment policy for rectal cancer—implementation of total mesorectal excision as routine treatment in Norway. A national audit. Dis Colon Rectum 45(7):857–866
Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H, Steup WH, Wiggers T, Kranenbarg EK, Leer JW (2002) Cooperative Investigators of the Dutch Colorectal Cancer Group. Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 20(3):817–825
Kapiteijn E, Kranenbarg EK, Steup WH, Taat CW, Rutten HJ, Wiggers T, van Krieken JH, Hermans J, Leer JW, van de Velde CJ (1999) Total mesorectal excision (TME) with or without preoperative radiotherapy in the treatment of primary rectal cancer: prospective randomised trial with standard operative and histopathological techniques: Dutch ColoRectal Cancer Group. Eur J Surg 165(5):410–420
Peeters KC, Marijnen CA, Nagtegaal ID, Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius B, Leer JW, van de Velde CJ (2007) Dutch Colorectal Cancer Group. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 246(5):693–701
The MRC Laparoscopic Groin Hernia Trial Group (1999) Laparoscopic versus open repair of groin hernia: a randomised comparison. The Lancet 354(9174):185–190
Stauffer JA, Rosales-Velderrain A, Goldberg RF, Bowers SP, Asbun HJ (2013) Comparison of open with laparoscopic distal pancreatectomy: a single institution’s transition over a 7-year period. HPB 15(2):149–155
The Clinical Outcomes of Surgical Therapy Study Group (2004) A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Fleishman J, Sargent DJ, Green E et al (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST study group trial. Ann Surg 246:655–664
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM (2005) COlon cancer Laparoscopic or Open Resection Study Group (COLOR). Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6(7):477–484
Lacy AM, Delgado S, Castells A, Prins HA, Arroyo V, Ibarzabal A, Pique JM (2008) The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248(1):1–7
Lacy AM, García-Valdecasas JC, Piqué JM, Delgado S, Campo E, Bordas JM, Taurá P, Grande L, Fuster J, Pacheco JL et al (1995) Short-term outcome analysis of a randomized study comparing laparoscopic vs open colectomy for colon cancer. Surg Endosc 9(10):1101–1105
Tekkis PP, Senagore AJ, Delaney CP, Fazio VW (2005) Evaluation of the learning curve in laparoscopic colorectal surgery: comparison of right-sided and left-sided resections. Ann Surg 242:83–91
Wexner SD, Cohen SM, Ulrich A, Reissman P (1995) Laparoscopic colorectal surgery—Are we being honest with our patients? Dis Colon Rectum 38(7):723–727
Künzli BM, Friess H, Shrikhande SV (2010) Is laparoscopic colorectal cancer surgery equal to open surgery? An evidence based perspective. World J Gastrointest Surg 2(4):101–108
Bretagnol F, Lelong B, Laurent C, Moutardier V, Rullier A, Monges G, Delpero JR, Rullier E (2005) The oncological safety of laparoscopic total mesorectal excision with sphincter preservation for rectal carcinoma. Surg Endosc 19(7):892–896
Laurent C, Leblanc F, Gineste C, Saric J, Rullier E (2007) Laparoscopic approach in surgical treatment of rectal cancer. Br J Surg 94(12):1555–1561
Leroy J, Jamali F, Forbes L, Smith M, Rubino F, Mutter D, Marescaux J (2004) Laparoscopic total mesorectal excision (TME) for rectal cancer surgery: long-term outcomes. Surg Endosc 18(2):281–289
Arezzo A, Passera R, Scozzari G, Verra M, Morino M (2013) Laparoscopy for rectal cancer reduces short-term mortality and morbidity: results of a systematic review and meta-analysis. Surg Endosc 27(5):1485–1502
Gong J, Shi DB, Li XX, Cai SJ, Guan ZQ, Xu Y (2012) Short-term outcomes of laparoscopic total mesorectal excision compared to open surgery. World J Gastroenterol 18(48):7308–7313
Ying X, Li Z, Shen Y, Ye P, Pan W, Chen H, Zhang L (2013) Total mesorectal excision for rectal cancer: laparoscopic versus open approach. Tumori 99(2):154–158
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM et al (2005) MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASSICC trial): multicentre, randomized controlled trial. Lancet 365:1718–1726
Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM et al (2007) UK MRC CLASICC Trial Group. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Fleshman J. American College of Surgeons Oncology Group (ACOSOG)-Z6051. A phase III prospective randomized trial comparing laparoscopic-assisted resection versus open resection for rectal cancer. http://clinicaltrials.gov/ct2/show/NCT00726622. Accessed 15 Nov 2014
Color II Study Group, Buunen M, Bonjer HJ, Hop WC, Haglind E, Kurlberg G, Rosenberg J, Lacy AM, Cuesta MA, D’Hoore A, Fürst A, Lange JF, Jess P, Bulut O, Poornoroozy P, Jensen KJ, Christensen MM, Lundhus E, Ovesen H, Birch D, Iesalnieks I, Jäger C, Kreis M, Van riet Y, Van der Harst E, Gerhards MF, Bemelman WA, Hansson BM, Neijenhuis PA, Prins HA, Balague C, Targarona E, Luján Mompeán JA, Franco Osorio JD, Garcia Molina FJ, Skullman S, Läckberg Z, Kressner U, Matthiessen P, Kim SH, Poza AA (2009) COLOR II: a randomized clinical trial comparing laparoscopic and open surgery for rectal cancer. Dan Med Bull 56(2):89–91
Kim NK, Kang J (2010) Optimal total mesorectal excision for rectal cancer: the Role of robotic surgery from an expert’s view. J Korean Soc Coloproctol 26(6):377–387
Marks G, Mohiuddin M, Goldstein SD (1988) Sphincter preservation for cancer of the distal rectum using high dose preoperative radiation. Int J Radiat Oncol Biol Phys 15(5):1065–1068
Mohiuddin M, Marks G (1991) High dose preoperative irradiation for cancer of the rectum, 1976–1988. Int J Radiat Oncol Biol Phys 20(1):37–43
Murty M, Enker WE, Martz J (2000) Current status of total mesorectal excision and autonomic nerve preservation in rectal cancer. Semin Surg Oncol 19:321–328
Enker WE, Thaler HT, Cranor ML, Polyak T (1995) Total mesorectal excision in the operative treatment of carcinoma of the rectum. J Am Coll Surg 181:335–346
Lacy AM, Garcia-Valdescasas JC, Delgado S et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomized trial. Lancet 359(9325):2224–2229
Morino M, Parini U, Giraudo G, Salval M, Brachet Contul R, Carrone C (2003) Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg 237:335–342
Laurent C, Leblanc F, Wütrich P, Scheffler M, Rullier E (2009) Laparoscopic versus open surgery for rectal cancer: long-term oncologic results. Ann Surg 250(1):54–61
Green BL, Marshall HC, Collinson F, Quirke P, Guillou P, Jayne DG, Brown JM (2013) Long-term follow-up of the Medical Research Council CLASICC trial of conventional versus laparoscopically assisted resection in colorectal cancer. Br J Surg 700:75–82
Disclosures
Drs. John H Marks and Renee Huang, Ms. McKeever, and Ms. Greenfield have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marks, J.H., Huang, R., McKeever, D. et al. Outcomes in 132 patients following laparoscopic total mesorectal excision (TME) for rectal cancer with greater than 5-year follow-up. Surg Endosc 30, 307–314 (2016). https://doi.org/10.1007/s00464-015-4210-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4210-1