Abstract
Purpose
We assessed emergency department (ED) utilization in patients with colorectal cancer to identify factors associated with ED visits and subsequent admission, as well as identify a high-risk subset of patients that could be targeted to reduce ED visits.
Methods
Data from Optum Labs Data Warehouse, a national administrative claims database, was retrospectively analyzed to identify patients with colorectal cancer from 2008 to 2014. Multivariable logistic regression was used to identify factors associated with ED visits and ED “super-users” (3+ visits). Repeated measures analysis was used to model ED visits resulting in hospitalization as a logistic regression based on treatments 30 days prior to ED visit.
Results
Of 13,466 patients with colorectal cancer, 7440 (55.2%) had at least one ED visit within 12 months of diagnosis. Factors associated with having an ED visit included non-white race, advancing age, increased comorbidities, and receipt of chemotherapy or radiation. 69.2% of patients who visited the ED were admitted to the hospital. A group of 1834 “super-users” comprised 13.6% of our population yet accounted for 52.1% of the total number of ED visits and 32.3% of admissions.
Conclusions
Over half of privately insured patients undergoing treatment for colorectal cancer will visit the ED within 12 months of diagnosis. Within this group, we identify common factors for a high-risk subset of patients with three or more ED visits who account for over half of all ED visits and a third of all admissions. These patients could potentially be targeted with alternative management strategies in the outpatient setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
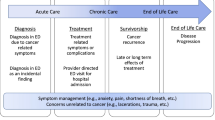
Multidisciplinary cancer care is a complex endeavor that occurs in a variety of inpatient and outpatient settings. Delivery of care itself can be challenging as it involves transitions between different specialists and phases of treatment. Often, this results in fragmentation of care and either delayed or inappropriate utilization of health care resources.1,2,3 This “system in crisis” was acknowledged by the Institute of Medicine in the report, “Delivering High Quality Care”.4 For patients navigating a cancer treatment plan, the emergency department (ED) represents a safety net that provides access to care that may not be otherwise available. However, the appropriate role of the ED in the management of cancer patients remains largely unknown.5,6
Clinical experience suggests that many of the ED visits made by patients during active cancer treatment may represent non-preventable use. However, it is also likely that a significant proportion is due to potentially avoidable problems. Furthermore, in the spectrum of cancer patients, there is likely a subset that is at risk of visiting the ED more than others.
In this study, we sought to better characterize the use of the ED in delivering care to patients with an initial diagnosis of colorectal cancer. Our primary goal is to quantify utilization of the ED and to identify factors associated with ED use following diagnosis of colorectal cancer and therefore identify high-risk subsets of patients that can be targeted to reduce ED use. As a secondary goal, we identify factors associated with hospital admission following a visit to the ED as well as common reasons for ED presentation.
Materials and Methods
Data Source
A retrospective analysis using Optum Labs Data Warehouse (OLDW) was performed for this study. OLDW is an administrative claims database consisting of privately insured and Medicare Advantage enrollees throughout the USA.7 The database covers more than 100 million enrollees from all regions of the USA, with greatest representation from the South and Midwest. The plan provides fully insured coverage for inpatient, outpatient, and pharmacy services. Medical claims include ICD-9-CM (international classification of diseases, ninth revision, clinical modification) diagnosis codes; ICD-9 procedure codes; Current Procedural Terminology, version 4 (CPT-4) procedure codes; Healthcare Common Procedure Coding System (HCPCS) procedure codes; site of service codes; and provider specialty codes.8 As all data in OLDW are deidentified, our study was exempted from Institutional Research Board review.
Case Selection
Any patient (> 18 years) with a diagnosis of colorectal cancer from 2008 to 2014 comprised our study cohort. ICD-9 diagnosis codes were used to identify the diagnosis of colorectal cancer (Supplemental Table 1), and all ED visits within 12 months of the initial diagnosis were counted as events. Initial diagnosis was defined as the first diagnosis colorectal cancer claim for each patient from 2008 to 2014. A validated algorithm of only including patients with five or more claims related to the primary claim was used.9 Causes for presentation to the ED were identified from primary diagnoses and limited to the day the patient presented to the ED; in cases where the primary diagnosis for the ED visit was colorectal cancer, the first non-CRC diagnosis was used. Only patients enrolled continuously for the year before the index diagnosis date and 12 months post diagnosis were included. The Charlson-Deyo comorbidity index10 was calculated using all primary and secondary non-colorectal cancer ICD-9 diagnosis codes on claims within 12 months prior to the index diagnosis date (baseline). Active treatment was identified using CPT codes for surgery, chemotherapy, and radiation within 30 days prior to ED visit (Supplemental Table 1).
Statistical Analysis
Categorical variables were compared using chi-squared analyses and continuous variables using t tests as appropriate. Covariates for all models included age (18–44, 45–54, 55–64, 65–74, 75+ years), race (non-white, white), gender, year of diagnosis, Charlson index (0, 1–2, 3+), surgery (no/yes), chemotherapy (no/yes), and radiation (no/yes). Multivariable analysis was performed using logistic regression to identify factors associated with one or more ED visits. A negative binomial model was constructed to identify factors associated with the total number of ED visits. A multivariable logistic regression was again used to identify factors associated with ED “super-users” (3+ visits). In addition, repeated measures analysis was performed modeling ED visits resulting in hospitalization as a logistic regression based on treatments 30 days prior to ED visit. Although socioeconomic status (SES) data is limited in the OLDW, information on patient income level is available. Using income as a proxy for SES, we also performed sensitivity analyses by incorporating income into our regression models. All tests were two-sided; significance levels were set at p < 0.05 and confidence intervals at 95%. Statistical analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC) software.
Results
Overall Rates of ED Evaluation and Admission
Our study population consisted of 13,446 patients, of whom 7440 (55.2%) had at least one ED visit in the 12 months after the diagnosis of colorectal cancer (Table 1). Of the 7440 patients with an ED visit, 5147 (69.2%) were subsequently admitted to the hospital. The mean age of patients who visited the ED was 67.3 years (SD 13.0); 50.4% were male, and the most common race was white (72.1%). Although most patients who utilized the ED did so only once (51.5%), many had two (23.9%) or three or more ED visits (24.7%). This last group of 1834 “super-users” comprised 13.6% of our total population of 13,446 patients, yet accounted for 52.1% of the total number of ED visits (8039) and 32.3% of the admissions from the ED (3907).
Bivariate Comparisons of Patients with an ED Visit and Those with No ED Visit (Table 1)
Compared to patients with no ED visit, patients who visited the ED at least once in the 12 months following diagnosis of colorectal cancer tended to be older (mean age 67.3 vs. 64.5, p < 0.001, with 36% of the patients with an ED visit being 75+ vs. 25.1% of the patients with no ED visit), more likely to have had chemotherapy (24.5 vs. 18.1%, p < 0.001) and had more comorbidities (Charlson score 3+ 29.8 vs. 20.3%, p < 0.001) (Table 1). Although patients who were non-white were also statistically more likely to visit the ED (27.9 vs. 25.6%, p = 0.003), but with a difference of only 2.3%, this finding may not be clinically meaningful.
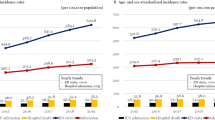
Trends in ED Visits (Fig. 2)
Utilization of the ED showed a linear increase from 11.6% in 2008 to 17.3% in 2014 (p < 0.001) (Fig. 1). The number of patients who utilized the ED only once decreased during this time period. The increase in total utilization was driven by repeat users (Fig. 2).
Factors Associated with an ED Visit Within 12 Months of Diagnosis (Table 2)
In multivariable analyses, the strongest factors associated with an ED visit were advancing age (75+ age group: OR 1.44, 95% CI 1.22–1.69), increased comorbidities (Charlson 3+: OR 1.64, 95% CI 1.49–1.80), chemotherapy (OR 1.57, 95% CI 1.44–1.72), and radiation (OR 1.15, 95% CI 1.05–1.26) (Table 2).
More recent year of diagnosis was also a factor in ED utilization, in keeping with the trends seen in Figs. 1 and 2. The most common diagnoses for ED visits were intestinal obstruction (5.33%), fluid and electrolyte disorders (5.25%), anemia (4.39%), gastrointestinal hemorrhage (3.69%), and abdominal pain (3.46%) (Supplemental Table 2).
“Super-users” (3+ ED Visits Within 12 Months of Diagnosis)
A group of 1834 “super-users” comprised 13.6% of our patient population yet accounted for 52.1% of the total number of ED visits (8039) and 32.3% of the admissions (3907). Factors associated with high ED use were non-white race (OR 1.16, 95% CI 1.04–1.30), older age (75+: OR 1.27, 95% CI 1.00–1.62), increased comorbidities (Charlson 3+: OR 2.27, 95% CI 1.98–2.59; Charlson 1–2: OR 1.36, 95% CI 1.20–1.55), chemotherapy (OR 1.44, 95% CI 1.27–1.62), and radiation (OR 1.27, 95% CI 1.11–1.44) (Table 3).
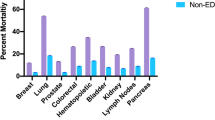
Factors Associated with ED Visits That Result in Subsequent Hospitalization
Of the 15,422 ED visits made by the 7440 patients in our study, 12,105 resulted in a hospital admission (78.5%). Hospital admission from the ED was associated with non-white race (OR 1.20, 95% CI 1.07–1.35), advanced age (75+ age group: OR 2.20, 95% CI 1.75–2.76), increased comorbidities (Charlson 3+: OR 1.29, 95% CI 1.13–1.48), and having had surgery (OR 4.04, 95% CI 3.60–4.53), radiation (OR 1.67, 95% CI 1.38–2.02), or chemotherapy (OR 2.22, 95% CI 1.90–2.58) in the 30 days before the ED visit (Table 2). The most common diagnoses leading to admission following an ED visit were colon cancer (25.4%), cancer of rectum and anus (9.9%), other gastrointestinal disorders (5.4%), complications of surgical procedures or medical care (4.9%), and intestinal obstruction (4.14%) (Supplemental Table 3).
Discussion
In this study, we show that 55% of colorectal cancer patients visit the ED in the first 12 months following diagnosis: a period of active treatment for most patients. Of the patients who visit the ED, 69.2% are subsequently admitted to the hospital. Patients who are older, have more comorbidities, and who receive radiation or chemotherapy in the 30 days prior are more likely to visit the ED. We also identify a high-risk subset of patients with three or more ED visits (“super-users”) who comprise 13.6% of our population, yet account for over half of all ED visits and a third of admissions from the ED.
The role of the ED as a safety net in the delivery of healthcare in the USA is well known.11 Over the last decade, the growth in utilization of ED services has outpaced growth in the general population, despite a reduction in the number of emergency rooms nationally.12 We see a similar trend in our data, with increasing utilization during the time of the study. Although not currently recognized as one of the leading causes of ED visits, the increasing incidence and prevalence of cancer in the general population will likely lead to worsening of the burden on EDs, both during active treatment and the surveillance phase. End-of-life care for many cancer patients often includes one or more visits to the ED, and in many cases, these are potentially avoidable.13,14 Some researchers have identified alternative strategies such as increased home-based nursing, telephone-based interventions, and multidisciplinary care to help prevent such ED visits.15,16,17
The largest study to date looking at utilization of the ED by cancer patients used The North Carolina Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT) to analyze 37,760 ED visits.18 Patients with colorectal cancer comprised 7.7% of total ED visits in their study, and the most common reasons for presentation were related to pain, respiratory distress, and GI issues. Our study found that intestinal obstruction, fluid and electrolyte disorders, and anemia were the top three diagnoses for visiting the ED. It is important to note that the NC DETECT analysis used the chief complaint listed for each ED visit. The OLDW database does not include chief complaint but does include diagnosis codes for each ED visit, which we grouped using Clinical Classifications Software (CCS) categories. This explains why our percentages of reasons for presentation are smaller than the NC DETECT analysis, as overall there were over 200 CCS categories represented using the primary diagnosis code for the 15,422 ED visits in our study.
The fact that patients who undergo chemotherapy or radiation are more likely to visit an ED and subsequently be admitted to the hospital is not surprising. Both modalities can potentially be associated with toxicity needing medical attention.19 However, 32% of patients receiving chemotherapy and 37% of patients receiving radiation who visited the ED were not admitted to the hospital, suggesting that some of the issues related to active treatment may have been treatable in a lower acuity setting. The use of chemotherapy did significantly increase from 18.8% of patients with colorectal cancer in 2008 to 24.4% in 2014 (p = 0.005), while the use of radiation significantly decreased from 21.6% in 2008 to 16.6% in 2014 (p = 0.001). This increase in chemotherapy use could be contributed to an increase in ED use. The current NCCN chemotherapy recommendations are well-established regimens that were approved for the treatment of colorectal cancer prior to our study period. These guidelines recommend regimens combining fluorouracil, leucovorin, and oxaliplatin (FOLFOX) or capecitabine and oxaliplatin (CAPEOX) as adjuvant treatment after surgical resection. For metastatic disease, FOLFOX, CAPEOX, or FOLFIRI (leucovorin, fluorouracil, and irinotecan) with or without bevacizumab is recommended.20,21,22 Except for the growing shift from adjuvant to neoadjuvant use of radiation in rectal cancer patients, there were also no major changes seen in recommendations for radiation therapy during the time frame of our study.23 Unfortunately, we do not have access to clinical details such as staging information in this dataset, so we are unable to further investigate which patient subsets saw an increase in the use of chemotherapy.
Having surgery was not a factor associated with an ED visit but was a factor associated with a hospital admission following an ED visit, suggesting that ED visits within 30 days of surgery may have had higher acuity. The finding that surgery was not a factor associated with an ED visit may be related to the fact that these patients have a postoperative inpatient stay where they are assessed for many complications before they are discharged. They also routinely have early follow-up appointments, which represent additional opportunities to address any problems in an outpatient setting.
Looking at the total number of ED visits (15,422) instead of the number of patients (7440), 78.5% of all ED visits result in admission, but “super-users” admission rate after an ED visit was much lower, 32.3% (RR 0.41, 95% CI (0.40, 0.42). This translates to 4132 ED visits that did not lead to admissions, again suggesting that these visits were potentially avoidable. The multivariable analysis did show these patients tended to be non-white, older, and higher comorbidity patients undergoing active treatment with radiation and/or chemotherapy. However, the C-statistic of our model was only 0.64, suggesting these variables are only moderately predictive and there are likely other factors associated with an ED visit that we cannot account for using this dataset. This is particularly applicable to socioeconomic variables, of which only patient income was available to us. In our sensitivity analysis, after incorporating patient income into our models, race was no longer associated with an ED visit or with being a “super-user.” This suggests that the differences in ED use seen between races are likely due to SES, which is consistent with previously published literature.24 We believe our findings lay a solid foundation for further research to better define a predictive model that can be used to identify a subset of “super-users.”
Some limitations to our study must be acknowledged. The data is retrospective and hence subject to misclassification, selection, and information bias. Although the OLDW database gives us a large sample size with the ability to conduct robust analyses, this comes at the expense of clinical detail. Detailed information on ED presentation or the circumstances and decision-making behind inpatient admission cannot be gleaned from administrative data. We limited capture of ED events to 12 months after diagnosis. While this should include the majority of patients undergoing active colorectal cancer treatment, it is possible there are patients still undergoing treatment and visiting the ED more than 12 months after diagnosis. Since a pre-condition for hospital admission in our study was an ED visit, direct admissions to the hospital were not captured and the true rate of admissions in our study cohort may be higher. Furthermore, although we used a validated algorithm to identify patients with colorectal cancer from claims data,9 it is possible that some misclassification bias exists. We do not have specific staging information for the colorectal cancers; hence, stage-specific analyses reflecting disease burden could not be conducted. The time of day and day of the week for ED presentation were not available to us using this dataset. Where care was actually delivered, e.g., outpatient clinic or multidisciplinary cancer center was not identifiable using our current dataset. Finally, we would like to point out that a proportion of ED visits by this patient population are likely appropriate and represent reasonable use of health care resources for acute problems. Our focus is less aimed toward the appropriateness of ED visits, and more toward quantifying this burden and identifying a group of “super-users” who could potentially be targeted to receive care in more suitable settings.
Conclusion
In conclusion, we show that 55% of privately insured patients undergoing treatment for colorectal cancer will visit an ED in the first 12 months following diagnosis and also identify the most common reasons for such a visit. Within this group, we define a high-risk subset of patients with three or more ED visits who account for over half of ED visits, but less than one third of admissions. This suggests these patients could potentially be treated in an outpatient setting with alternative management strategies such as improving patient education, increasing communication between patients and their multidisciplinary team via phone or electronic medical systems, or more frequent outpatient visits. Similar strategies could be applied to other patients undergoing multidisciplinary care to potentially offset the burden of patients with cancer in the ED who could have received appropriate care in an alternative setting.
References
Hussain, T., et al., Fragmentation in specialist care and stage III colon cancer. Cancer, 2015. 121(18): p. 3316–24.
Skolarus, T.A., Y. Zhang, and B.K. Hollenbeck, Understanding fragmentation of prostate cancer survivorship care: implications for cost and quality. Cancer, 2012. 118(11): p. 2837–45.
Graboyes, E.M., et al., Postoperative care fragmentation and thirty-day unplanned readmissions after head and neck cancer surgery. Laryngoscope, 2017. 127(4): p. 868–874.
Herzog, T., et al., Complicated sigmoid diverticulitis—Hartmann’s procedure or primary anastomosis? Acta Chir Belg, 2011. 111(6): p. 378–83.
Jelinek, G.A., et al., Caught in the middle: tensions around the emergency department care of people with advanced cancer. Emerg Med Australas, 2013. 25(2): p. 154–60.
Ahn, S., et al., Emergency department cancer unit and management of oncologic emergencies: experience in Asan Medical Center. Support Care Cancer, 2012. 20(9): p. 2205–10.
Wallace, P.J., et al., Optum Labs: building a novel node in the learning health care system. Health affairs, 2014. 33(7): p. 1187–94.
Levack, M.M., et al., Sigmoidectomy syndrome? Patients’ perspectives on the functional outcomes following surgery for diverticulitis. Dis Colon Rectum, 2012. 55(1): p. 10–7.
McClish, D.K., et al., Ability of Medicare claims data and cancer registries to identify cancer cases and treatment. Am J Epidemiol, 1997. 145(3): p. 227–33.
Deyo, R.A., D.C. Cherkin, and M.A. Ciol, Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol, 1992. 45(6): p. 613–9.
Costi, R., et al., Challenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with a nonoperative treatment. Surg Endosc, 2012. 26(7): p. 2061–71.
Tang, N., et al., Trends and characteristics of US emergency department visits, 1997-2007. JAMA, 2010. 304(6): p. 664–70.
Barbera, L., C. Taylor, and D. Dudgeon, Why do patients with cancer visit the emergency department near the end of life? CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne, 2010. 182(6): p. 563–8.
Henson, L.A., et al., Emergency department attendance by patients with cancer in their last month of life: a systematic review and meta-analysis. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 2015. 33(4): p. 370–6.
Wang, S.M., et al., Effects of multidisciplinary team care on utilization of emergency care for patients with lung cancer. The American journal of managed care, 2014. 20(8): p. e353–64.
Alkema, G.E., et al., Reduced mortality: the unexpected impact of a telephone-based care management intervention for older adults in managed care. Health services research, 2007. 42(4): p. 1632–50.
Seow, H., et al., Does Increasing Home Care Nursing Reduce Emergency Department Visits at the End of Life? A Population-Based Cohort Study of Cancer Decedents. Journal of pain and symptom management, 2015. 51(2): p. 204–12.
Mayer, D.K., et al., Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 2011. 29(19): p. 2683–8.
Burke, T.A., T. Wisniewski, and F.R. Ernst, Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer, 2011. 19(1): p. 131–40.
Benson, A.B., 3rd, et al., Metastatic colon cancer, version 3.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw, 2013. 11(2): p. 141–52; quiz 152.
Benson, A.B., 3rd, et al., Colon Cancer, Version 1.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw, 2017. 15(3): p. 370–398.
Benson, A.B., 3rd, et al., Rectal Cancer, Version 2.2015. J Natl Compr Canc Netw, 2015. 13(6): p. 719–28; quiz 728.
Ma, B., et al., What has preoperative radio(chemo)therapy brought to localized rectal cancer patients in terms of perioperative and long-term outcomes over the past decades? A systematic review and meta-analysis based on 41,121 patients. Int J Cancer, 2017. 141(5): p. 1052–1065.
Hong, R., B.M. Baumann, and E.D. Boudreaux, The emergency department for routine healthcare: race/ethnicity, socioeconomic status, and perceptual factors. J Emerg Med, 2007. 32(2): p. 149–58.
Funding
This publication was made possible by funding from the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Author information
Authors and Affiliations
Contributions
All authors meet all of the criteria for the definition of authorship: substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Rights and permissions
About this article
Cite this article
Weidner, T.K., Kidwell, J.T., Etzioni, D.A. et al. Factors Associated with Emergency Department Utilization and Admission in Patients with Colorectal Cancer. J Gastrointest Surg 22, 913–920 (2018). https://doi.org/10.1007/s11605-018-3707-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3707-z