Abstract
Introduction
Use of central vascular ligation during dissection around the superior mesenteric artery (SMA) in pancreaticoduodenectomy (PD) for periampullary malignancies has rarely been documented.
Methods
We developed the SMA hanging technique (SHT) to facilitate central vascular ligation during PD. Briefly, SMA dissection was initiated using the supracolic anterior approach, followed by left-sided dissection. The SMA was taped under finger guidance immediately after right-sided dissection. The ligament of Treitz was detached from the SMA during left-sided dissection, facilitating adequate lymph node dissection while preserving the nerve plexus around the SMA. Forty-seven consecutive patients who underwent PD for periampullary malignancies were divided into two groups: 23 underwent SHT and 24 underwent conventional dissection. Patients’ clinical results were assessed to evaluate the feasibility and validity of SHT.
Results
Blood loss volume, operation duration, and the incidence of bleeding during SMA dissection were significantly lower in the SHT group than in the conventional group. The short-term and oncological results were similarly acceptable in both groups.
Conclusions
SHT is a feasible and safe technique with acceptable short-term outcomes. We propose the use of this procedure to standardize en bloc dissection around the SMA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In bloc resection of the cancer and cancer-bearing regions including lymph nodes and organ parenchyma has been advocated when treating cancers of the gastrointestinal system such as those of the stomach,1–3 colon,4 rectum,5 and liver.6 Although the oncological benefit of this method has been proven in only a limited number of reports,3 , 7 the principle has gained popularity among surgeons worldwide. Particularly for colonic cancers, en bloc resection of the cancer-bearing intestine and mesocolon with high ligation of the supplying arteries of corresponding regions is termed central vascular ligation.4
Central vascular ligation has seldom been discussed in pancreaticoduodenectomy (PD), where margin-negative resection often depends on adequate dissection around the superior mesenteric artery (SMA),8–13 even though a standardized method of appropriate dissection has not been established. Dissection between the pancreas head and SMA ahead of the point of no return (such as pancreas transection or bile duct division) has been proposed, and several different approaches have been described.14–25 However, most of these reports describe the initial approach for SMA dissection; descriptions of the entire procedure for SMA dissection are rare. A safe, easily performed dissection method around the SMA is required for standardization.
We describe the complete sequence for SMA dissection using the “SMA hanging technique” following the supracolic anterior artery-first approach, to facilitate central vascular ligation. This technique is based on the anatomical features surrounding the SMA and ligament of Treitz and is a promising proposed technique for standardized dissection during PD.
Materials and Methods
Concept of Central Vascular Ligation in the Periampullary Region
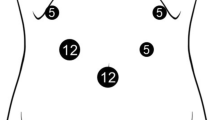
Figure 1a shows a conceptual schema of the vascular anatomy of the digestive system with the components arranged in a single plane. Central vascular ligation represents en bloc resection of the tumor-bearing region with high ligation of supplying arteries, e.g., the inferior mesenteric artery for sigmoid colectomy or the ileocolic, right colic, and right branch of the middle colic artery for right hemicolectomy. The pancreas head is connected to the SMA system, celiac ganglion, and celiac axis system. When performing central vascular ligation, the arteries that supply the pancreas head, namely the inferior pancreatoduodenal artery (IPDA) and gastroduodenal artery, should be ligated at their origin (Fig. 1b, c). Because the IPDA usually has a common trunk with the first or second jejunal artery,25 central vascular ligation extends to the origin of the corresponding jejunal artery. This concept has been described as level 2 dissection in PD with systematic mesopancreas dissection (SMD-PD)25 and involves en bloc mesopancreas dissection including both sides of the SMA, with staged dissection. The technique is indicated for diseases requiring systematic lymph node dissection of the mesopancreas such as for ampullary, distal bile duct, and duodenal cancers. If the hemi-circumferential nerve plexus of the SMA (plSMA) is also dissected, the dissection is classified as level 3, indicated for cancers with invasive growth or with perineural spread such as in pancreatic ductal cancer. Our new method can be applied to level 2 or 3 dissection according to this classification.
Conceptual schema of the vascular anatomy of the digestive system. a Entire system. Each component is arranged in a single plane. Central vascular ligation covers the tumor-bearing region with high ligation of supplying arteries; e.g., sigmoid colectomy (black dashed line) or right hemicolectomy (black solid line). b Magnified view of the mesopancreas area. GDA gastroduodenal artery, IPDA inferior pancreatoduodenal artery, JA jejunal artery, SMA superior mesenteric artery, MCA middle colic artery, pl-PH-I(II) first (second) nerve plexus of the pancreas head. c Conceptual schema of en bloc resection of the pancreas head and mesopancreas
SMA Hanging Technique Surgical Procedure
Following Kocher’s maneuver, the gastrocolic fascia is dissected to open the omental bursa. The superior right colic vein is ligated routinely, followed by further dissection along the same plane to expose the middle colic artery, which is exposed to its origin to identify the SMA and to dissect the lymph nodes above the SMA. The superior mesenteric vein (SMV) is then taped at the level of the transverse portion of the duodenum.
In level 2 dissection without SMV co-resection, branches such as the gastrocolic trunk of Henle, which usually arises from the anterior aspect of the SMV26 or the first jejunal vein, are first divided to free the SMV from the pancreas head. A diamond-shaped window is then created by retracting the SMV rightward, the transverse mesocolon caudally, the SMA leftward, and the pancreas neck cranially (Fig. 2a, b). If the middle colic vein obstructs the view, it can be ligated and divided. The right and dorsal aspects of the SMA are dissected within this field using the supracolic anterior approach while preserving the circumferential plSMA.25
Schema during right dorsal dissection of the superior mesenteric artery (SMA) by the supracolic anterior approach. a Frontal view of level 2 dissection. The diamond-shaped field is created by cross-directional retraction of the superior mesenteric vein (SMV), the SMA, pancreatic neck, and transverse mesocolon, including the pedicle of the middle colic artery. b Transverse view of level 2 dissection. Dissection from the right side should extend to the left side of the SMA. c Frontal view of level 3 dissection. The nerve plexus around the SMA is peeled off the artery. Dissection around the SMV is limited to maintain good tumor margins. d Transverse view of level 3 dissection. The second nerve plexus of the pancreas head is dissected hemicircumferentially from the SMA. Lymph nodes, fat, connective tissue, and the SMV around the tumor are untouched to maximize the resection margins
In level 3 dissection, wherein the cancer has invaded the mesopancreas and SMV, the connective tissue around the SMV is not detached from the SMV. The middle colic vein is routinely ligated and divided, and the hemicircumferential plSMA in the corresponding direction is resected to gain an optimal margin (Fig. 2c, d).
In both level 2 and 3 dissection, the jejunal vein running behind the SMA should be adequately separated from the SMA, i.e., up to 1 cm left of the SMA (Fig. 2b, d). The origin of the IPDA or the common trunk of the IPDA and first jejunal artery is exposed, ligated, and cut at this stage. We then convert the procedure to left-sided dissection of the SMA. At this stage, we can easily identify the origin of the second jejunal artery (preserved). The surgeon inserts a left finger behind the SMA from the right side at a point just proximal to the second jejunal artery. Under the guidance of the surgeon’s fingers, the serosa of the mesentery is opened, connecting the right and left dissection spaces (Fig. 3a, b). A tape for hanging is placed through this hole, encircling the dorsal aspect of the SMA. The transverse colon is then reflected cranially, and the left side of the SMA is dissected so that the previous opening is enlarged toward the origin of the SMA, preserving the plSMA (Fig. 4a). This procedure can be performed bloodlessly because the origin of the first jejunal artery has already been ligated and cut, and the jejunal vein has been separated from the SMA during the previous supracolic anterior approach. The mesentery of the first jejunal artery is divided from the remnant, and the corresponding jejunum is cut. Dissection of the left side then progresses, and the ligament of Treitz is identified as a membranous layer composed of smooth muscle that narrows cranially (Fig. 4b).27,28 The ligament is dissected from the SMA, then ligated, and cut at the level of the SMA origin. The left side of the SMA is thus fully dissected while preserving the plSMA (Fig. 4c). Once the stump of the jejunum is reflected rightward, the SMV is retracted to the left, and the upper portion of the mesopancreas is dissected. Once the right-sided dissection reaches the origin of the SMA, en bloc dissection around the SMA is completed. Division of the pancreas neck, common bile duct, stomach, or duodenum is then performed. We performed intraoperative frozen section analysis for the pancreas stump, bile duct stump, and para-aortic lymph nodes for all cases in this study. When the pancreatic or bile duct stump was judged to be cancer positive, additional resection was considered.
Schema of connecting the dissection planes. a Frontal view of connecting the planes. Under finger guidance, the serosa of the mesojejunum is opened adjacent to the superior mesenteric artery. b Transverse view of connecting the planes. Under finger guidance, a thin Kelly clamp is inserted from the left side, and tape is applied
Schema of dissection of the left side of the superior mesenteric artery (SMA). a Initial dissection. The dissection begins from the point at which the tape is applied and progresses toward the origin of the SMA, preserving the nerve plexus of the SMA, enlarging the window to the right-sided dissection plane. b Middle dissection. The mesojejunum is divided along the future-preserved jejunal artery pedicle. Left-sided dissection is then extended, identifying the ligament of Treitz as a membranous muscular layer. c Final dissection. The ligament is detached from the SMA, ligated, and cut beyond the left renal vein. At this stage, complete dissection of the left side of the superior mesenteric artery is achieved while preserving this side of the nerve plexus of the superior mesenteric artery
Conventional SMA Dissection During SMD-PD
In conventional SMA dissection during SMD-PD, right-sided dissection is similarly performed using a supracolic anterior approach, followed by dissection of the left side of the SMA. Conventional dissection is initiated by dividing the jejunum at the estimated point of resection, and the mesojejunum is then transected toward the SMA from the periphery.25 Thereafter, left-sided dissection of the SMA continues along the SMA with connection of the right and left dissection spaces achieved during the final stage of the dissection.
Patients
Between January 2013 and August 2015, the first author performed 47 elective PDs for malignant diseases using the SMD-PD method; the first 24 patients underwent PD with the conventional technique (conventional group), and the latter consecutive 23 underwent PD with the SMA hanging technique (SMA hanging technique group). The institutional review board of the Cancer Institute Hospital, Tokyo, Japan, approved this retrospective study with waived informed consent.
In all operations, immediately after resection, the specimen was macroscopically explored, and the regional lymph nodes were identified, numbered, and isolated by the attending surgeon. The lymph nodes surrounding the main tumor were left untouched and simply noted. Pathological R0 resection was defined as no exposure of cancer cells in the dissection plane.
The total amount of intraoperative blood loss was estimated from the total volume of blood aspirated or absorbed by gauze, which was recorded by a nurse in the operating theater. All clinical, surgical, and pathological data were collected from a prospectively accumulated database. The definition of postoperative pancreatic fistula in this report was that proposed by the International Study Group on Pancreatic Fistula.29 The definition of delayed gastric emptying was that proposed by the International Study Group of Pancreatic Surgery.30 Other postoperative complications were defined according to the Clavien-Dindo classification system,31,32, and the final diagnosis was determined based on the pathological findings.
Feasibility and Efficacy of the SMA Hanging Technique
The feasibility of the SMA hanging technique was evaluated based on patients’ prospectively accumulated surgical records. A successful dissection procedure was defined as that completed without conversion to the conventional method because of uncontrollable bleeding or loss of orientation during dissection. Bleeding was defined as active hemorrhage during dissection around the SMA requiring coagulation, compression, or suturing; minor oozing was excluded.
Statistical Analysis
All continuous data are expressed as the median with range. Quantitative and categorical variables were compared using the generalized Wilcoxon’s rank-sum test and Fisher’s exact test, respectively. A p value <0.05 was considered statistically significant. Statistical analysis was performed using JMP software (version 10; SAS Institute Inc., Cary, NC).
Results
Patient Demographics
No significant differences in patient demographics were present between the two groups (Table 1). All patients with invasive pancreatic cancer excluding two patients with pancreatic groove cancer located away from the SMA and one with high systemic risk underwent level 3 dissection of the mesopancreas including hemicircumferential plSMA dissection. The remaining patients underwent level 2 dissection.
Perioperative Outcomes
The SMA hanging technique was feasible in all 23 patients, and Table 1 shows the perioperative outcomes in both groups. The intraoperative blood loss volume (420 vs. 625 ml, p = 0.027), operation duration (401 vs. 486 min, p = 0.042), and incidence of bleeding events during SMA dissection (4 vs 29 %, p = 0.047) were significantly lower in patients in the SMA hanging technique group. The incidence of blood transfusion tended to be lower in the SMA hanging technique group, although the difference between groups did not reach statistical significance. The rate of postoperative complications, including postoperative pancreatic fistula and delayed gastric emptying, and the hospital stay duration were similar between the groups. Although the rate of diarrhea was comparable between the groups and successfully controlled by medication, most patients who required an opioid antidiarrheal had undergone level 3 dissection. Among 16 patients with opioid administration, opioid was discontinued or converted to non-opioid antidiarrheal drugs in seven patients. One patient in the conventional group died of acute interstitial pneumonia of unknown cause with secondary multiple organ failure. Among 27 patients with pancreatic cancer, 21 patients underwent adjuvant chemotherapy using 5-fluorouracil derivative (TS-1) or gemcitabine (13 in the SMA hanging technique group and 8 in the conventional group). Two patients in the SMA hanging technique group and one in the conventional group were not candidates for adjuvant therapy because of advanced age or comorbidity. Three patients in the conventional group underwent therapeutic chemotherapy for early recurrence.
Oncological Outcomes
The number of patients with positive lymph nodes was 18 (78 %) in the SMA hanging technique group and 16 (67 %) in the conventional group with no significant difference (p = 0.52). The total number of dissected lymph nodes (31 (range, 19–50) vs. 29 (range, 11–68), SMA hanging technique vs. conventional group, respectively; p = 0.27) was similar between the groups. Margin-negative resection was achieved in 20 patients (87 %) in the SMA hanging technique group and 22 (92 %) in the conventional group, with no significant difference between groups (p = 0.67). Both groups included two patients with a positive margin in the medial dissection plane of the mesopancreas, whereas one patient in the SMA hanging technique group had a positive margin at the pancreas neck stump.
Discussion
In this preliminary report, we proposed further developments in the technique for en bloc dissection around the SMA following the supracolic anterior approach. Although en bloc resection around the SMA is desirable, a standardized technique for widespread use should be universally applicable regardless of patient factors such as disease type, anatomy, and possible obesity. Inoue et al.25 recently proposed a novel technique termed SMD-PD with en bloc mesopancreas dissection including both sides of the SMA. The SMA hanging technique described in the current article is supplemental to and an adaptation of SMD-PD, potentially ensuring precise and bloodless dissection around the SMA, as our results have shown.
Our technique includes two new points derived from anatomical features around the SMA. The first point is a safe connection of both sides of the dissection space around the SMA. As was described previously, the supracolic anterior approach allows for dissection of the right dorsal aspect of the SMA with a clear view.25 At this stage, the dissection level for preserving or resecting the plSMA (corresponding to level 2 or 3, respectively) or the longitudinal range of dissection along the SMA (which branches should be resected) is adjusted while judging resectability. Previous reports of pancreatic cancer have reported the SMA aspect as the most frequent point of R1 resection.8,9,33,34 Therefore, a logical strategy includes dissection of this part first to establish the maximum cancer margin or judge resectability with respect to the SMA margin. Also, because most jejunal veins run behind the SMA,25 primary dissection between the jejunal vein and SMA facilitates bloodless dissection in the left aspect. In the SMA hanging technique, finger-guided penetration of the mesentery enables atraumatic connection of the dissection space, and a hanging tape works as an entrance landmark for left-sided dissection, which also corresponds to the distal end of the longitudinal SMA dissection. This approach facilitates bloodless dissection because of the primary right-sided dissection of the jejunal vein from the SMA and ventral retraction to facilitate dissection between the artery and the mesopancreas. The second new point in this article is setting an optimal dissection layer on the left side of the SMA by identifying the ligament of Treitz27,28,35,36 as the membranous muscular tissue forming the duodenojejunal junction. Detaching the ligament from the SMA exposes the left surface of the plSMA. This technique is reasonable and useful because in most pancreatic head tumors, the left-sided plSMA is usually intact and should be preserved to avoid severe postoperative diarrhea.
A standardized method of en bloc resection of the supplying artery and its associated lymph nodes in patients with gastric cancer was proposed approximately 50 years ago and was termed “D2 dissection” in the 1980s.1 Also, the efficacy of lymph node dissection in promoting long-term survival was proven after more than 50 years of performing lymph node dissection.2,3 A similar principle has been proposed for total mesorectal excision or complete mesocolic excision in patients with colorectal cancer, and the validity of this technique has been accepted worldwide.4,5,7,37 En bloc resection of the cancer-bearing area together with a corresponding inflow vessel has also been applied in the treatment of hepatocellular carcinoma.6 Wide and accurate resection of regional lymph nodes during PD has been advocated in several series for precise disease staging;38–40 however, clear descriptions of en bloc resection regarding the SMA are lacking. Also, in several randomized trials comparing “extended dissection” and “standard dissection,”32,41–43 the definition of standard dissection was not established, and there remains no standardized technique. Therefore, the true benefit of wide and en bloc lymph node dissection around the SMA remains unclear. Our technique could become part of a widespread safe and comprehensible SMA dissection method, with surgeons at different institutes performing it with similar quality.
Our report has certain limitations. First, related to the preliminary retrospective design, comparison of the long-term outcomes was omitted. Second, the true efficacy of the SMA hanging technique remains to be confirmed. Results from comparisons between non-concurrent groups from a single institution without randomization should be interpreted carefully regarding technical bias or a learning curve effect. Although our series showed significantly reduced blood loss in the SMA hanging technique group, to draw reproducible and definitive conclusions, well-controlled randomized trials are needed to compare this technique with a conventional method. Third, our study involved exclusively Japanese patients, who tend to have a lower BMI. Although Japanese people have genetically different fat distribution characterized by higher amounts of visceral fat compared with people in other regions,44,45 extremely obese patients are rare in Japanese society. Therefore, the feasibility and efficacy of the SMA hanging technique remain unclear in higher BMI or obese patients in western countries. Despite these limitations, this preliminary report achieved its major aims of describing the complete SMA dissection sequence and the concept of central vascular ligation in PD, with acceptable perioperative and oncological outcomes.
During the last decade, “artery-first” and “mesopancreas dissection” have been hot topics potentially leading to standardized SMA dissection in PD. However, to our knowledge, there are no reported objective and reproducible evaluations of the outcomes of these techniques that exclude the learning curve effect or selection bias. We hope that our proposed technique will help further the discussion of central vascular ligation in PD among surgeons worldwide, serving as an impetus for a randomized study to confirm the superiority of any technique in a larger cohort.
Conclusion
We described the details of the SMA hanging technique for en bloc resection around the SMA, with acceptable perioperative outcomes. We believe that this technique is feasible for surgeons with average skill performing conventional pancreatic surgery. We advocate this procedure as a promising option for PD.
Abbreviations
- PD:
-
Pancreaticoduodenectomy
- SMA:
-
Superior mesenteric artery
- IPDA:
-
Inferior pancreatoduodenal artery
- SMD-PD:
-
Pancreaticoduodenectomy with systematic mesopancreas dissection
- plSMA:
-
Nerve plexus around the superior mesenteric artery
- SMV:
-
Superior mesenteric vein
References
Kajitani T. The general rules for the gastric cancer study in surgery and pathology. Part I. Clinical classification. Jpn J Surg 1981;11:127-139.
Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, van Elk P, Obertop H, Gouma DJ, Taat CW, van Lanschot J, Meyer S, de Graaf PW, von Meyenfeldt MF, Tilanus H. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet 1995;345:745-748.
Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439-449.
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P. Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol. 2010;28:272-278.
Heald RJ, Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet. 1986;1:1479–1482.
Makuuchi M, Hasegawa H, Yamazaki S. Ultrasonically guided subsegmentectomy. Surgery, gynecology & obstetrics. 1985;161:346-350.
Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, O’Callaghan C, Myint AS, Bessell E, Thompson LC, Parmar M, Stephens RJ, Sebag-Montefiore D; MRC CR07/NCIC-CTG CO16 Trial Investigators; NCRI Colorectal Cancer Study Group. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009;373:821-828.
Esposito I, Kleeff J, Bergmann F, Reiser C, Herpel E, Friess, H Schirmacher P, Büchler MW. Most pancreatic cancer resections are R1 resections. Ann Surg Oncol. 2008;15:1651-1660.
Buchler MW, Werner J, Weitz J. R0 in pancreatic cancer surgery: surgery, pathology, biology, or definition matters? Ann Surg. 2010;251:1011-1012.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Tajima H, Miwa K. Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer. Ann Surg. 1999;229:76-83.
Kayahara M, Ohta T. Gross appearance of the ampullary tumor predicts lymph node metastasis and outcome. Dig Surg. 2000;27:127-131.
Ito K, Ito H, Allen PJ, Gonen M, Klimstra D, D’Angelica MI, Fong Y, DeMatteo RP, Brennan MF, Blumgart LH, Jarnagin WR. Adequate lymph node assessment for extrahepatic bile duct adenocarcinoma. Ann Surg. 2010;251:675-681.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Miyazaki I. Surgical strategy for carcinoma of the papilla of Vater on the basis of lymphatic spread and mode of recurrence. Surgery. 1997;121:611-617.
Ohigashi H, Ishikawa O, Eguchi H, Yamada T, Sasaki Y, Noura S, Takachi K, Miyashiro I, Murata K, Doki Y, Imaoka S. Early ligation of the inferior pancreaticoduodenal artery to reduce blood loss during pancreaticoduodenectomy. Hepatogastroenterology. 2004;51:4-5.
Pessaux P, Varma D, Arnaud JP. Pancreaticoduodenectomy: superior mesenteric artery first approach. J Gastrointest Surg. 2006;10:607-611.
Popescu I, David L, Dumitra AM, Dorobantu B. The posterior approach in pancreaticoduodenectomy: preliminary results. Hepatogastroenterol. 2007;54:921–926.
Horiguchi A, Ishihara S, Ito M, Nagata H, Shimizu T, Furusawa K, Kato R, Katada K, Miyakawa S. Pancreatoduodenectomy in which dissection of the efferent arteries of the head of the pancreas is performed first. J Hepatobiliary Pancreat Surg. 2007;14:575–578.
Weitz J, Rahbari N, Koch M, Buchler MW. The “artery first” approach for resection of pancreatic head cancer. J Am Coll Surg. 2010;210:e1–4.
Dumitrascu T, David L, Popescu I. Posterior versus standard approach in pancreatoduodenectomy: a case-match study. Langenbecks Arch Surg. 2010;395:677-684.
Hackert T, Werner J, Weitz J, Schmidt J, Buchler MW. Uncinate process first--a novel approach for pancreatic head resection. Langenbecks Arch Surg. 2010;395:1161-1164.
Popescu I, Dumitrascu T. Total meso-pancreas excision: key point of resection in pancreatic head adenocarcinoma. Hepatogastroenterol. 2011;58:202-207.
Dumitrascu T, Popescu I. Posterior approach pancreaticoduodenectomy: does it really improve long-term survival in pancreatic head cancer? JOP. 2011;12:491-492; author reply 493-494.
Kurosaki I, Minagawa M, Takano K, Takizawa K, Hatakeyama K. Left posterior approach to the superior mesenteric vascular pedicle in pancreaticoduodenectomy for cancer of the pancreatic head. JOP. 2011;12:220-229.
Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, Takahashi Y, Koga R. Pancreatoduodenectomy With Systematic Mesopancreas Dissection Using a Supracolic Anterior Artery-First Approach. Ann Surg. 2015;262:1092-1101.
Nagakawa Y, Hosokawa Y, Osakabe H, Sahara Y, Takishita C, Nakajima T, Hijikata Y, Kasahara K, Kazuhiko K, Saito K, Tsuchida A. Pancreaticoduodenectomy with right-oblique posterior dissection of superior mesenteric nerve plexus is logical procedure for pancreatic cancer with extrapancreatic nerve plexus invasion. Hepatogastroenterology. 2014;61:2371-2376.
Miyazawa M, Kawai M, Hirono S, Okada K, Shimizu A, Kitahata Y, Yamaue H. Preoperative evaluation of the confluent drainage veins to the gastrocolic trunk of Henle: understanding the surgical vascular anatomy during pancreaticoduodenectomy. J Hepatobiliary Pancreat Sci. 2015;22:386-91.
Alford WC, Jr. WENZEL TREITZ: the man and his “ligament”. Surgery. 1963;53:556-562.
Jit I. The development and the structure of the suspensory muscle of the duodenum. The Anatomical record. 1952;113:395-407.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13.
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW, Yeo CJ, Büchler MW. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196.
Jang JY, Kang MJ, Heo JS, Choi SH, Choi DW, Park SJ, Han SS, Yoon DS, Yu HC, Kang KJ, Kim SG, Kim SW. A prospective randomized controlled study comparing outcomes of standard resection and extended resection, including dissection of the nerve plexus and various lymph nodes, in patients with pancreatic head cancer. Ann Surg. 2014;259:656-664.
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg. 2006;93:1232-1237.
Jamieson NB, Foulis AK, Oien KA, Going JJ, Glen P, Dickson EJ, Imrie CW, McKay CJ, Carter R. Positive mobilization margins alone do not influence survival following pancreatico-duodenectomy for pancreatic ductal adenocarcinoma. Ann Surg. 2010;251:1003-1010.
Treitz W. Uber einen neuen Muskel am Duodenum des Menchen, uber elstische Sehenen und einige andere anastomische Verhaltnisse. Vierteljahrschr Prakt Heilk. 1953;37:113. (in German)
Kim SK, Cho CD, Wojtowycz AR. The ligament of Treitz (the suspensory ligament of the duodenum): anatomic and radiographic correlation. Abdominal imaging. 2008;33:395-397.
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P. Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol. 2012;30:1763-1769.
Schwarz RE, Smith DD. Extent of lymph node retrieval and pancreatic cancer survival: information from a large US population database. Ann Surg Oncol. 2006;13:1189-200.
Tomlinson JS, Jain S, Bentrem DJ, Sekeris EG, Maggard MA, Hines OJ, Reber HA, Ko CY. Accuracy of staging node-negative pancreas cancer: a potential quality measure. Arch Surg. 2007;142:767-23; discussion 73-4.
Pawlik TM, Gleisner AL, Cameron JL, Winter JM, Assumpcao L, Lillemoe KD, Wolfgang C, Hruban RH, Schulick RD, Yeo CJ, Choti MA. Prognostic relevance of lymph node ratio following pancreaticoduodenectomy for pancreatic cancer. Surgery. 2007;141:610-8.
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, Coleman J, Abrams RA, Hruban RH. Pancreaticoduodenectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg. 2002;236:355-366.
Farnell MB, Pearson RK, Sarr MG, DiMagno EP, Burgart LJ, Dahl TR, Foster N, Sargent DJ; Pancreas Cancer Working Group. A prospective randomized trial comparing standard pancreatoduodenectomy with pancreatoduodenectomy with extended lymphadenectomy in resectable pancreatic head adenocarcinoma. Surgery. 2005;138:618-628.
Kimura W. Strategies for the treatment of invasive ductal carcinoma of the pancreas and how to achieve zero mortality for pancreaticoduodenectomy. J Hepatobiliary Pancreat Surg. 2008;15:270-277.
Tanaka S, Horimai C, Katsukawa F. Ethnic differences in abdominal visceral fat accumulation between Japanese, African-Americans, and Caucasians: a meta-analysis. Acta diabetologica. 2003;40 Suppl 1:S302-4.
Haldar S, Chia SC, Henry CJ. Body Composition in Asians and Caucasians: Comparative Analyses and Influences on Cardiometabolic Outcomes. Advances in food and nutrition research. 2015;75:97-154.
Acknowledgments
We thank Mr. Koki Tazoe (a freelance graphic designer, Nerima-ku, Tokyo) for designing the schemata in this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Inoue, Y., Saiura, A., Tanaka, M. et al. Technical Details of an Anterior Approach to the Superior Mesenteric Artery During Pancreaticoduodenectomy. J Gastrointest Surg 20, 1769–1777 (2016). https://doi.org/10.1007/s11605-016-3214-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3214-z