Abstract
Background
In pancreaticoduodenectomy (PD), the approach to superior mesenteric artery (SMA) is a critical process that supports adequate surgical margins and radicality for pancreatic tumors. In most of the reports on laparoscopic PD, the right-sided approach in which the jejunum is pulled out to the right side for peri-SMA dissection is used, since the left side of the SMA is difficult to dissect, and the only way to do this is to dissect the vein first.
Methods
We devised a method to simplify and safely perform peri-SMA dissection by reversing the process, starting from the left side of the SMA. The first step involves the mobilization of the pancreatic head, which allows for rotation around the SMA. The second step involves the dissection of the left side of the SMA and transection of the jejunum. The key point is to change the incision line between the anterior and posterior mesojejunum. The third process includes the inferior pancreatoduodenal artery (IPDA) and first jejunal artery (J1A) dissection, which can be easily performed from the left side because the SMA rotates by simply continuing the dissection along the previously exposed SMA, and the IPDA/J1A are safely dissected at the root because they are drawn to the left side. The remaining processes are performed on the right side.
Results
This method was performed in 16 cases, and in most cases IPDA/J1A were divided from the left side.
Conclusion
The technique for SMA dissection from the left posterior side was described with illustrations and video. Our method allows safe oncologic dissection around SMA avoiding anatomical misorientation during laparoscopic PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In pancreaticoduodenectomy (PD) for periampullary malignancies, superior mesenteric artery (SMA) dissection is a critical step in obtaining an appropriate surgical margin length and complete clearance of lymph nodes. While various operative approaches for SMA dissection have been described to improve operative safety and oncologic clearance, most are suitable for open surgery [1,2,3]. In laparoscopic surgery, since the first PD case was reported in 1994 [4], many surgical/oncological results have been reported and reviewed [5, 6], but specific techniques/approaches for SMA dissection have rarely been discussed [7,8,9]. In this short report, we describe our technique (named the ‘left posterior approach’) for SMA dissection during laparoscopic PD for periampullary tumors and its short-term outcomes.
Methods
Indication
For the benign tumors including IPMN without high risk stigmata, lymph node dissection can be partially omitted. In terms of dissection around SMA, the principle of the procedure is the same regardless of the disease. Patients with pancreatic cancer with concern for vascular invasion (SMA/PV) were not selected for laparoscopic PD.
Operative procedure
Preoperative preparation and exposure of the SMV
First, we cannot emphasize enough the importance of meticulous preoperative assessment of precise vascular anatomy using thin-slice contrast-enhanced computed tomography scans. Surgeons must be well-aware of the anatomical details of all named/unnamed branches of the SMA and celiac artery (CA), and specifically, the location of the roots of the inferior pancreatoduodenal artery (IPDA) and jejunal arteries (by “o’clock” position or distance from the SMA root and other landmarks) is critical for operative planning.
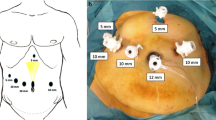
Five ports are placed in a standard fashion, and the liver is retracted superioanteriorly with a Nathanson liver retractor to expose the porta hepatis (Fig. 1). The gastrocolic ligament is incised, and the lesser sac is opened widely. The superior mesenteric vein (SMV) is identified at the inferior border of the pancreas, and the superior right colic vein is ligated and/or clipped, and divided. The transverse mesocolon is retracted inferiorly and dissected from the pancreatic head. When the third portion of the duodenum becomes visible, the SMV above this level is exposed widely, with the gastrocolic trunk not yet divided, to avoid congestion of the pancreatic head. The second portion of the duodenum is kocherized well to completely free the duodenum from the retroperitoneum. The purpose of these initial steps are to mobilize the vascular pedicle including SMA and facilitate the SMA dissection and identification of its major branches (IPDA and J1A).
Dissection of the anterior side of the mesojejunum
In order to dissect the SMA (left posterior approach), the transverse mesocolon is retracted cephalad with the Nathanson liver retractor, and the mesojejunum is pulled caudad. The anterior side of the mesojejunum is incised along with the SMA at the 3 o’clock position, and the neural plexus around the SMA is exposed. During dissection along with the neural plexus directed to the root of the SMA, the ligament of Treitz is detached and divided. The first and second jejunal arteries (J1A and J2A) are identified in the mesojejunum, and the anterior plane of the mesojejunum is incised along J2A with communicating branches to J1A divided (Fig. 2). The jejunum is then divided at the end of the mesojejunal incision line (Fig. 3). In obese patients, the roots of the jejunal arteries from the SMA are not necessarily easy to find because of the thick fat in the mesentery, and it is not safe to dissect the tissue near the SMA without clear anatomical orientation. Therefore, in these patients, we recommend dissecting the mesojejunum in the reverse direction. As the communication arcade can be easily found at the rim of the mesentery once the jejunum is transected, the distal J2A can be identified by following the distal side of the arcade, and it is easy and safe to then incise the anterior side of the mesentery along with J2A toward the SMA.
Cutline of the anterior side of the mesojejunum. The transverse mesocolon is retracted cephalad, and the anterior surface of the mesentery is incised along with the SMA, exposing the surrounding nerve tissue. The mesojejunum is then incised with J2A toward the jejunum. MCA middle colic artery, SMA superior mesenteric artery, J1A first jejunal artery, J2A second jejunal artery
After dissection of the anterior plane of the mesojejunum. The communicating arcade between J1A and J2A was divided, and the jejunum was transected using an endo-stapler. The posterior side of the mesentery was not incised. The ligament of Treitz can be divided either in this step or later. MCA middle colic artery, SMA superior mesenteric artery, J1A first jejunal artery, J2A second jejunal artery
Dissection of the posterior plane of the mesojejunum
The jejunum is retracted anteriorly and the posterior side of the mesojejunum is exposed. The posterior peritoneal attachment is incised, and the duodenum is dissected free from the retroperitoneum (Fig. 4, line A). When the ligament of Treitz is divided, the duodenum to the proximal jejunum is mobile around the SMA axis. To remove all the soft tissue, including the uncinate process and lymph nodes around the SMA enbloc, the division line of the posterior plane of the mesojejunum should not be parallel to the anterior division line but must be directed to the inferior border of the third portion of the duodenum (Fig. 4, line B). The surface of the posterior mesojejunum is incised.
Cut line of the posterior plane of the mesojejunum. A The jejunal loop was elevated anteriorly, and the peritoneal attachment between the duodenum and retroperitoneum is incised. B It should be noted that the dissection line for the posterior mesojejunum was not the same as the incision line on the anterior side. The superficial layer of the mesentery was incised toward the proximal duodenum. MCA middle colic artery, J2A second jejunal artery
When the distal jejunum loop is elevated anteriorly and the proximal jejunal stump is pulled posteriorly, countertraction between the future resected specimen (including the uncinate process and proximal mesojejunum) and preserved structures (SMA, J2A, or more distal branches and distal mesojejunum) is created. This retraction also facilitates the outline of the SMA pedicle. Thereafter, the rest of the procedure involves placing all tissues other than the mesenteric vessels down posteriorly to the specimen side (Fig. 5). For patients with jejunal veins running anterior to the SMA, the SMA with the surrounding nerve plexus should be used as the landmark for the dissection layer, and for those with jejunal veins running posterior to the SMA, the second jejunal vein and SMV trunk should be the landmarks for the dissection layer. The landmark vessel is exposed in the direction from distal to proximal, with all arterial and venous branches toward the specimen side divided. Subsequently, dissection of the soft tissue around the SMA, including its branches, allows rotation of the SMA to the left side, and subsequently, the IPDA branching off from the posterior side can be securely ligated and divided. After these process, uncinate process and soft tissue including lymph nodes is detached enbloc from the SMA. In another case, in which the IPDA branches from the right side, it should be divided at a later stage of the procedure after the proximal jejunal stump is pulled out to the right. Finally, the division of soft tissue around the root of the SMA completes the “SMA dissection.” The proximal jejunum was passed under the SMA/SMV pedicle and pulled to the right (Supplementary Video).
The concept of the laparoscopic left posterior approach. The distal jejunal loop and its mesojejunum were elevated anteriorly, and the proximal jejunum to be resected was pulled posterolaterally. Along with the dissection, the SMA rotates to the left, and IPDA/J1A can be isolated and ligated. SMA superior mesenteric artery, IPDA inferior pancreaticoduodenal artery, JVT jejunal venous trunk, SMV superior mesenteric vein
Pitfall
When the proximal jejunum is retracted to the left, with the distal jejunum and the SMA being elevated anteriorly, the uncinate process of the pancreas is withdrawn to the left with the mesopancreas by SMA rotation. As the tissue between the uncinate process and the duodenum is relatively loose, dissection can easily go in the wrong direction behind the uncinate process (Fig. 6A). In the case of disorientation, it is safe to intentionally expose the surface of the uncinate process and adjust the dissection line appropriately (Fig. 6B). Nonetheless, the best way to avoid disorientation is to continue the dissection close to the SMA during the entire procedure (Fig. 6C). The head-down position can facilitate the exposure of the operative field by excluding the distal jejunum loops from the area left and posteriorly to the SMA. Intraoperative photographs are shown in Fig. 7.
Variations in the left posterior approach. A Incorrect dissection plane. If the dissection progresses along with the jejunum, the plane is easily misdirected under the pancreas. B To return to the appropriate plane, the uncinate process is exposed, and the tissue between the SMA and pancreas is divided. C To avoid such misdirection and to assure the clearance of soft tissue around the SMA, we recommend staying close to the SMA
Snapshots of the surgical procedure. A Preparation of the left posterior approach from anterior view. B The J1A + IPDA transection by left posterior view C dissection of the SMA from right side by anterior view D after resection by right side view. SMV; superior mesenteric vein, SMV superior mesenteric vein, MCA middle colic artery, MCV middle colic vein, IPDA inferior pancreaticoduodenal artery, PV portal vein, CA celiac artery
Division of the stomach/duodenum
The division line is determined based on tumor location and surgeon preference. The right gastric and right gastroepiploic vessels are divided, and the antrum of the stomach or proximal duodenum is divided using an endo-stapler.
Dissection at the superior boarder of the pancreas
The anterior surface of the common hepatic artery (CHA) is exposed above the pancreas, and the surrounding lymph nodes/soft tissues are dissected proximally and distally. The CHA and proper hepatic artery are circumferentially dissected. The gastroduodenal artery (GDA) is isolated and divided after testing.
Dissection of the hepatoduodenal ligament
The gallbladder is detached from the liver bed, and the peritoneal surface of the hepatoduodenal ligament is incised. The common bile duct is dissected free of the right hepatic artery (RHA) and encircled. After the distal RHA is exposed on the right side, the common bile duct is divided.
The steps described above are completed by the operator standing on the patient’s left side. At this point, the operator moves to the right of the patient and performs the rest of the procedure.
Division of the pancreas
A tunnel between the head of the pancreas and the SMV/PV is created. As the dissection of the superior pancreas is already completed at this point, the forceps can easily pass under the pancreas which is then divided.
Division of pancreas head nerve plexus from the right side
The jejunum and uncinate processes are pulled to the right. At this point, the left to posterior side of the SMA is dissected free, and the major inflow to the pancreas via the GDA and IPDA is already gone. The gastrocolic trunk is divided, as well as other small right branches of the PV. With the specimen retracted to the right, only the right-side plexus around the SMA remains. The nerve fibers are dissected along the SMA; the fibers directed to the pancreas are divided, while the fibers running parallel to the SMA are left behind. The IPDA branches on the right side of the SMA should be divided at this stage (Fig. 7C). After the plexus behind the CHA is dissected along with the CA, the specimen can be taken en bloc with the lymph nodes at the superior border of the pancreas. Finally, the soft tissue in the hepatoduodenal ligament is incised along the hepatic arteries and portal vein, and the resection is completed (Fig. 7D).
Reconstruction for the intestinal continuity
Pancreaticojejunostomy, choledochojejunostomy, and gastrojejunostomy/duodenojejunostomy are performed either via mini-laparotomy or laparoscopy. Pancreatic and biliary stents are placed as required.
This retrospective study was approved by the Cancer Institute Hospital Ethics Committee (approval number 2019-GA-1095), and the written consents were obtained from all the patients.
Results
From January 2020, when we performed initial laparoscopic PD with this left posterior approach, through to March 2022, we performed this procedure on 16 patients (Table 1). In all but one patient (n = 12) with IPDA branching at the left side (3–7 o’clock position), the IPDA (+ J1A) was divided from the left side. In three patients with IPDA branching from the right side (8–11 o’clock position), isolation of the root of the IPDA from the left side was not possible, and the IPDA was divided from the right side during the later step. The operations tended to be more difficult in obese male patients. Table 2 shows pathological findings. Eight cases (50%) were diagnosed with malignancy. Median harvested lymph nodes was 20, and median size of the tumor was 19 mm.
Postoperative complications of Clavien–Dindo grade ≥ 3a occurred in one patient who underwent laparotomy for an intra-abdominal abscess. Pancreatic fistula of ISGPF grade B or greater occurred in one patient (6.2%). Operative mortality was not observed.
Discussion
In this short report, we describe our technique for laparoscopic PD, in which SMA dissection can be completed safely in a systematic manner using the mesenteric vessels as landmarks for dissection. Although various techniques for SMA dissection and their oncologic implications have been described in open PD for pancreatic cancer [1,2,3, 10, 11], the limitations in operative view angle and mobility of surgical instruments make a similar approach difficult to translate into the laparoscopic procedure, and the details for SMA dissection have rarely been addressed in technical reports for laparoscopic PD [7, 9, 12, 13]. Despite the advantages of laparoscopic surgery, such as less blood loss and shorter recovery time [5, 14], the priority for cancer patients is the radicality for oncologic clearance; thus, the oncologic principles used in the open approach should not be compromised in the laparoscopic approach. Among the limited number of technical reports regarding the SMA approach in laparoscopic PD, most described an approach to the SMA from the right side [7]. In our experience, we found this approach technically demanding because SMA exposure and rotation completely relies on the assistant’s hands. The problem was that assistants did not always have adequate laparoscopic skills. When we started left posterior approach, we did it at a first step. However, it’s difficult to complete the IPDA dissection due to the angle limitations of the forceps except in the less visceral fat patients. While changing the order of the surgical steps, we noticed that the soft tissue including uncinate process rotated well around the SMA after the dissection around the pancreatic head. In our left posterior approach, the assistant only needed to grasp the mesojejunum and not the mesenteric vessels, including the SMA or SMV. Thus, the operation could be performed with the trainee surgeon as an assistant.
Our technique described here is a combination of the previously described knowledge of surgical anatomy for SMA dissection techniques [3, 10, 11] with the basic dissection techniques for lymph nodes around major vessels that have been established in laparoscopic gastrectomy [15, 16].
The advantage of this technique over the traditional laparoscopic PD are as follows. The first is operative safety. In traditional SMA dissection from the right side, the operating surgeon needs to retract the proximal jejunum and pancreas to the right for appropriate exposure of the SMA, and only one hand can be used for dissection; thus, in cases of bleeding from the branches of the SMA or SMV, suturing or ligation would be difficult or even impossible because both hands cannot be used. In contrast, our left posterior approach, in which the SMA is retracted anteriorly by the assistant’s forceps with the duodenum/proximal jejunum being pulled down posteriorly by gravity, the operating surgeon is allowed to use both hands for dissection as well as for bleeding control with sutures, as needed.
The second advantage is the blood inflow/outflow to the pancreatic head. In our left posterior approach, all inflow arteries (IPDA, J1A, GDA) were divided prior to the division of outflow veins (gastrocolic trunk, anterior/posterior superior pancreaticoduodenal veins [ASPDV/PSPDV], and others), and congestion of the pancreas was avoided. In the right approach, the division of major SMV branches is necessary for the exposure of the SMA, and when the arterial inflow remains intact, venous congestion of the pancreatic head can occur even if ASPDV is left alone. On the left side, SMA exposure and subsequent IPDA/J1A ligation are possible without division of the SMV branches; thus, we did not have to struggle with annoying venous oozing from the congested pancreas head during the rest of the procedure.
The third advantage is the ease of orienting the dissection line. The vascular anatomy in the mesojejunum/mesopancreas is usually quite complex owing to its embryonic rotation, and disorientation or misdirection can occur during dissection in this area. As the dissection progresses along with the landmark vessels in our approach, such problems are unlikely to occur, even in obese patients in whom the mesenteric vessels are not visible from the mesenteric surfaces.
The last and most important advantage is the security of oncologic clearance. Our approach allows for the safe dissection of the SMA to its root and complete clearance of the nodes on its left posterior side. In the traditional right-side approach, the tissue at the left posterior side of the SMA must be withdrawn to the right side by rotating the SMA. Although this maneuver is possible in open surgery, it is technically demanding in laparoscopic surgery with instruments of limited mobility and is likely to result in incomplete clearance with some soft tissue/lymph nodes left behind. Specifically, because of the difficulty in SMA rotation near its root, in contrast to the greater mobility of the distal SMA, it is not easy to remove the left-side tissue around the root from the right. In this context, we believe that the left-sided approach is technically reasonable. While IPDA branching from the right of the SMA cannot be taken initially from the left in our approach, it can be divided from the right in the final step of the procedure. Obviously, the simplest and safest principle is to remove the tissue on the left from the left and the tissue on the right from the right. Rather than sticking to either the left or the right, approaching from the direction that is easy to do will make the surgery better. A video paper was recently published summarizing various approaches to the SMA [9]. Unfortunately, they do not recommend a left approach. However, the main value of their report is that it gives us a chance to know every approach. That will allow surgeons to make better choices in difficult situations during MIS-PD.
Despite these technical and oncological advantages, we have also recognized some issues with this technique. While it could be performed quite safely, as shown in the results, we found it difficult to expose the SMA from the left side in some cases, including patients with morbid obesity and a history of pancreatitis. In these cases, we needed to be flexible for the selection of the left or right approach according to the specific patient condition and vascular anatomy, as well as the location and extent of the tumor. This series excludes patients with SMA and/or SMV involvement. If MIS-PD is planned for more advanced pancreatic cancer, other approach, a mesenteric approach or extensive dissection from Treitz ligament, or combination of approaches from multiple directions may be necessary.
Conclusion
The technique for SMA dissection from the left posterior side was described with illustrations and videos. Our method allows safe oncologic dissection around SMA avoiding anatomical misorientation during laparoscopic PD. The operative principle and surgical anatomy should be applicable to robot-assisted PD, and further evaluation is warranted.
Abbreviations
- PD:
-
Pancreaticoduodenectomy
- SMA:
-
Superior mesenteric artery
- CA:
-
Celiac artery
- IPDA:
-
Inferior pancreatoduodenal artery
- SMV:
-
Superior mesenteric vein
- J1A and J2A:
-
First and second jejunal arteries
- CHA:
-
Common hepatic artery
- GDA:
-
Gastroduodenal artery
- RHA:
-
Right hepatic artery
References
Weitz J, Rahbari N, Koch M, Buchler MW (2010) The “artery first” approach for resection of pancreatic head cancer. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2009.10.019
Sanjay P, Takaori K, Govil S, Shrikhande SV, Windsor JA (2012) ‘Artery-first’ approaches to pancreatoduodenectomy. Br J Surg. https://doi.org/10.1002/bjs.8763
Nagakawa Y, Yi SQ, Takishita C, Sahara Y, Osakabe H, Kiya Y, Yamaguchi H, Miwa Y, Sato I, Tsuchida A (2020) Precise anatomical resection based on structures of nerve and fibrous tissue around the superior mesenteric artery for mesopancreas dissection in pancreaticoduodenectomy for pancreatic cancer. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.725
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. https://doi.org/10.1007/BF00642443
Kendrick ML, van Hilst J, Boggi U, de Rooij T, Walsh RM, Zeh HJ, Hughes SJ, Nakamura Y, Vollmer CM, Kooby DA, Asbun HJ, Minimally Invasive Pancreatic Resection Organizing C (2017) Minimally invasive pancreatoduodenectomy. HPB (Oxford). https://doi.org/10.1016/j.hpb.2017.01.023
Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D’Angelica MI, Balduzzi A, Bassi C, Bjornsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG, International Study Group on Minimally Invasive Pancreas S (2020) The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg. https://doi.org/10.1097/SLA.0000000000003590
Nagakawa Y, Watanabe Y, Kozono S, Boggi U, Palanivelu C, Liu R, Wang SE, He J, Nishino H, Ohtsuka T, Ban D, Nakata K, Endo I, Tsuchida A, Nakamura M, Study group of Precision Anatomy for Minimally Invasive Hepato-Biliary-Pancreatic s (2022) Surgical approaches to the superior mesenteric artery during minimally invasive pancreaticoduodenectomy: a systematic review. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.905
Honda G, Kurata M, Okuda Y, Kobayashi S, Sakamoto K, Takahashi K (2013) Laparoscopic pancreaticoduodenectomy: taking advantage of the unique view from the caudal side. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2013.08.019,Dec2013
Ielpo B, Anselmo A, Masuda Y, Xuan MYH, Burdio F, De Blasi V, Sanchez-Velazquez P, Giuliani A, Azagra JS, Viola GM, Podda M, Pellino G, Rosso E (2023) Superior mesenteric artery first approach for minimally invasive pancreaticoduodenectomy: a step-by-step surgical technique video. Ann Surg Oncol. https://doi.org/10.1245/s10434-022-12743-2
Inoue Y, Saiura A, Yoshioka R, Ono Y, Takahashi M, Arita J, Takahashi Y, Koga R (2015) Pancreatoduodenectomy with systematic mesopancreas dissection using a supracolic anterior artery-first approach. Ann Surg. https://doi.org/10.1097/SLA.0000000000001065
Inoue Y, Saiura A, Oba A, Kawakatsu S, Ono Y, Sato T, Mise Y, Ishizawa T, Takahashi Y, Ito H (2019) Optimal extent of superior mesenteric artery dissection during pancreaticoduodenectomy for pancreatic cancer: balancing surgical and oncological safety. J Gastrointest Surg. https://doi.org/10.1007/s11605-018-3995-3
Nagakawa Y, Nakagawa N, Takishita C, Uyama I, Kozono S, Osakabe H, Suzuki K, Nakagawa N, Hosokawa Y, Shirota T, Honda M, Yamada T, Katsumata K, Tsuchida A (2021) Reconsideration of the appropriate dissection range based on japanese anatomical classification for resectable pancreatic head cancer in the era of multimodal treatment. Cancers (Basel). https://doi.org/10.3390/cancers13143605
Nagakawa Y, Hosokawa Y, Sahara Y, Takishita C, Hijikata Y, Osakabe H, Nakajima T, Shirota T, Katsumata K, Nakamura M, Tsuchida A (2018) Approaching the superior mesenteric artery from the right side using the proximal-dorsal jejunal vein preisolation method during laparoscopic pancreaticoduodenectomy. Surg Endosc. https://doi.org/10.1007/s00464-018-6118-z
Palanivelu C, Senthilnathan P, Sabnis SC, Babu NS, Srivatsan Gurumurthy S, Anand Vijai N, Nalankilli VP, Praveen Raj P, Parthasarathy R, Rajapandian S (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg. https://doi.org/10.1002/bjs.10662
Kanaya S, Haruta S, Kawamura Y, Yoshimura F, Inaba K, Hiramatsu Y, Ishida Y, Taniguchi K, Isogaki J, Uyama I (2011) Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Endosc. https://doi.org/10.1007/s00464-011-1792-0
Shibasaki S, Suda K, Nakauchi M, Nakamura T, Kadoya S, Kikuchi K, Inaba K, Uyama I (2018) Outermost layer-oriented medial approach for infrapyloric nodal dissection in laparoscopic distal gastrectomy. Surg Endosc. https://doi.org/10.1007/s00464-018-6111-6
Funding
No funding associated with this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Takafumi Sato, Yosuke Inoue, Atsushi Oba, Yoshihiro Ono, Hiromichi Ito and Yu Takahashi have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 334072 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sato, T., Inoue, Y., Oba, A. et al. Laparoscopic dissection around the superior mesenteric artery by left posterior approach during pancreaticoduodenectomy. Surg Endosc 37, 8871–8878 (2023). https://doi.org/10.1007/s00464-023-10417-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10417-y