Abstract
Purpose
Perioperative blood transfusions are costly and linked to adverse clinical outcomes. We investigated the factors associated with variation in blood transfusion utilization following upper gastrointestinal cancer resection and its association with infectious complications.
Methods
The Statewide Planning and Research Cooperative System was queried for elective esophagectomy, gastrectomy, and pancreatectomy for malignancy in NY State from 2001 to 2013. Bivariate and hierarchical logistic regression analyses were performed to assess the factors associated with receiving a perioperative allogeneic red blood cell transfusion. Additional multivariable analysis examined the relationship between transfusion and infectious complications.
Results
Among 14,875 patients who underwent upper GI cancer resection, 32 % of patients received a perioperative blood transfusion. After controlling for patient, surgeon, and hospital-level factors, significant variation in transfusion rates was present across both surgeons (p < 0.0001) and hospitals (p < 0.0001). Receipt of a blood transfusion was also independently associated with wound infection (OR = 1.68, 95% CI = 1.47 and 1.91), pneumonia (OR = 1.98, 95% CI = 1.74 and 2.26), and sepsis (OR = 2.49, 95% CI = 2.11 and 2.94).
Conclusion
Significant variation in perioperative blood transfusion utilization is present at both the surgeon and hospital level. These findings are unexplained by patient-level factors and other known hospital characteristics, suggesting that variation is due to provider preferences and/or lack of standardized transfusion protocols. Implementing institutional transfusion guidelines is necessary to limit unwarranted variation and reduce infectious complication rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nearly 14 million units of allogeneic red blood cells (RBCs) are transfused each year in the USA, and at least 20 % of these transfusions are administered perioperatively to surgical patients.1 While blood transfusions may be vital in improving oxygen delivery to tissues in some circumstances, there has been increasing evidence that there may be adverse postoperative outcomes associated with their use.2 Many of these complications have been attributed to transfusion-related immunomodulation (TRIM) resulting in a higher risk of postoperative infectious complications and cancer recurrence following oncologic resection.3 – 8 Because of this growing concern for post-transfusion adverse outcomes, a lack of benefit for using liberal transfusion strategies, and a goal of reducing consumption of a scarce resource, blood transfusion guidelines favoring restrictive transfusion triggers with a hemoglobin threshold between 7 and 8 g/dL for most patients have been developed to limit unnecessary utilization.2 , 8 , 9
Despite the existence of general practice guidelines for the use of RBC transfusions over the past few decades, numerous studies have demonstrated wide variation in blood transfusion utilization following surgical procedures. Over 20 years ago, Goodnough et al. demonstrated large variation in the rate of perioperative transfusion of RBCs (range = 17–100 %), plasma (range = 0–97 %), and platelets (range = 0–80 %) between hospitals for coronary artery bypass graft surgery despite controlling for patient and surgical practice factors.10 Since then, additional studies have further confirmed those results for cardiac surgery.11 , 12 Similar hospital variability has been shown for orthopedic surgery with significant differences in RBC transfusion practices between hospitals following total hip and knee replacement.13 – 15 However, there is a paucity of data examining contemporary blood transfusion utilization for procedures outside of cardiac and orthopedic surgery.
Given these limitations in the literature, the aim of this study was to investigate patient, surgeon, and hospital-level factors associated with perioperative allogeneic RBC transfusion in patients undergoing elective upper gastrointestinal cancer resection using a large, population-based database. Furthermore, the study analyzes the variation in blood transfusion utilization at both the surgeon and hospital level and assesses the association between perioperative RBC transfusion and the postoperative infectious complications of deep wound infection, pneumonia, and sepsis.
Materials and Methods
Study Population
The Statewide Planning and Research Cooperative System (SPARCS), a hospital discharge database established by the New York Department of Health, was utilized for this study. SPARCS includes patient-level data for all hospital admissions, ambulatory surgery procedures, and emergency department visits within New York State and has been used extensively for research purposes, both on their own and as part of the Healthcare Cost and Utilization Project (HCUP) databases.16 , 17 These data are abstracted from medical records by trained medical records personnel, verified for accuracy by the Department of Health, and include a unique patient identifier, patient demographics, up to 25 diagnostic codes with present-on-admission indicators, up to 15 procedures codes, and unique hospital and surgeon identifiers. The data are also linked to New York State Vital Records to obtain mortality information.
Inclusion/Exclusion Criteria
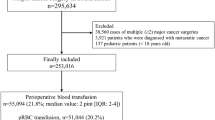
The SPARCS inpatient file was queried for all elective admissions for esophagectomy, gastrectomy, or pancreatectomy for malignancy using International Classification of Diseases, Ninth Revision (ICD-9) codes. From these claims, patients at least 18 years old with a primary or secondary diagnosis of esophageal cancer (ICD-9 = 150.0–151.0) who underwent esophagectomy (ICD-9 = 42.40–42.42), gastric cancer (ICD-9 = 151.0–151.9) who underwent partial gastrectomy (ICD-9 = 43.5–43.7, 43.81–43.89) or total gastrectomy (ICD-9 = 43.91–43.99), or hepatobiliary cancer (ICD-9 = 152.0, 156.1–156.8, 157.0–157.9) who underwent distal pancreatectomy (ICD-9 = 52.52) or pancreaticoduodenectomy (ICD-9 = 52.7) between January 1, 2001 and December 31, 2013 were selected. Patients who had non-elective admission to the hospital or who had a missing unique surgeon identifier were excluded. In addition, because the date of blood transfusion is not captured for many patients in SPARCS, patients who were admitted prior to the date of surgery were necessarily excluded to ensure that blood transfusions were not administered preoperatively (Fig. 1).
Outcome Measures
The primary outcome was the receipt of a perioperative (intraoperative or postoperative) allogeneic red blood cell transfusion. The receipt of a blood transfusion was captured either through ICD-9 procedural coding (ICD-9 = 99.03, 99.04) or ancillary revenue codes for red blood cell products (code = 0381, 0382) and transfusion (code = 0391). Because the number of units of blood product is not captured in SPARCS, the receipt of a blood transfusion was only characterized as a dichotomous outcome.
Secondary outcome measures included the postoperative infectious complications of deep wound infection, pneumonia, and sepsis. These adverse outcomes were captured using secondary diagnosis codes categorized as “not present-on-admission.” The inclusion and exclusion criteria and corresponding ICD-9 coding for these complications were previously described and validated by Silber et al.18
Patient-Level Factors
Patient factors considered for the analyses were age, sex, race, insurance type, active tobacco use, and the 30 comorbidities included in the Elixhauser Comorbidity Index, including several factors that would influence the likelihood of receiving a blood transfusion, such as anemia, congestive heart failure, end-stage renal disease, and coagulation disorders. These patient comorbidities were extracted from the current claim as well as all claims up to 1 year prior to the index operation based upon ICD-9 diagnostic codes using the Elixhauser Comorbidity Index method.19
Surgeon-Level Factors
Procedure-specific individual surgeon procedure volumes were calculated as the total number of esophagectomies, gastrectomies, or pancreatectomies for cancer performed during that calendar year by that individual surgeon using the unique surgeon identifier. Because individual surgeon volumes fluctuated over the years, surgeon volumes were calculated for each individual calendar year. Volume was then categorized into procedure-specific tertiles. The volume categories for esophagectomy were low (1–3 cases/year), medium (4–9 cases/year), and high (≥10 cases/year). The volume categories for gastrectomy were low (1–2 cases/year), medium (3–5 cases/year), and high (≥6 cases/year). The volume categories for pancreatectomy were low (1–4 cases/year), medium (5–19 cases/year), and high (≥20 cases/year).
Hospital-Level Factors
Procedure-specific individual hospital procedure volumes were calculated as the total number of esophagectomies, gastrectomies, or pancreatectomies for cancer performed during that calendar year by that individual hospital using the unique hospital identifier. Because individual hospital volumes fluctuated over the years, hospital volumes were calculated for each individual calendar year. Volume was then categorized into procedure-specific tertiles. The volume categories for esophagectomy were low (1–9 cases/year), medium (10–29 cases/year), and high (≥30 cases/year). The volume categories for gastrectomy were low (1–7 cases/year), medium (8–24 cases/year), and high (≥25 cases/year). The volume categories for pancreatectomy were low (1–14 cases/year), medium (15–39 cases/year), and high (≥40 cases/year).
In addition to facility volume, hospital characteristics included major academic status based upon Council of Teaching Hospitals (COTH) designation and facility location (urban or rural). The American Hospital Association Annual Survey was used to identify facilities considered to be major academic centers.
Propensity Score Analysis
Because of the observational nature of the data and potential for selection bias with respect to which patients received a blood transfusion for the secondary analysis involving infectious complications, a propensity score for each patient was estimated to determine the probability of receiving a perioperative blood transfusion. The propensity score was estimated using the same multivariable model used to assess the factors associated with the primary outcome of receipt of a blood transfusion. In order to avoid reduction in study size, the propensity score was used as a continuous variable and entered as a covariate in the multivariable models as has been previously described.20 – 24
Statistical Analysis
Patient, operative, surgeon, and hospital characteristics were assessed using Pearson’s chi-square test, Mann–Whitney U test, and Cochrane-Armitage test for trend as appropriate to the data. Clinically appropriate variables with a p value of less than 0.1 were manually entered in multivariable analysis. To account for clustering of outcomes among surgeons and hospitals, a three-level mixed-effects logistic regression model was used for the primary outcome of perioperative blood transfusion, as well as the secondary outcomes of deep wound infection, pneumonia, and sepsis. The models estimated random effects for each individual surgeon and hospital identifier.
To identify individual surgeons and hospitals who were significant outliers with regard to blood transfusion utilization, exact Poisson 95 % confidence intervals (CI) were calculated for the risk-adjusted observed/expected (O/E) ratios for each surgeon and hospital. The observed represents the total number of patients who received a blood transfusion, and the expected was calculated by summing the probability of receiving a blood transfusion across all patients. Only surgeons and hospitals that performed at least 10 cases over the 2001 to 2013 study period were included in this analysis. Low outliers (low blood transfusion utilization) were defined as surgeons or hospitals with an O/E ratio significantly less than one, and high outliers (high blood transfusion utilization) were those with an O/E ratio significantly greater than one.
For the mixed-effects models, the glmer function in the lme4 package was used in R version 3.1.0 (R Foundation for Statistical Computing). All other analyses were performed using SAS, Version 9.3 (SAS Institute, Cary, NY, USA). The study was approved by both the University of Rochester (IRB #00054886) and the New York State Department of Health institutional review boards.
Results
Population Characteristics
Out of 21,608 patients who underwent esophagectomy, gastrectomy, or pancreatectomy for malignancy between 2001 and 2013 in New York State, 14,875 patients met inclusion criteria. Of the 6733 patients who were excluded, 5061 patients had a non-elective admission for the index hospital stay, 5 had a missing unique surgeon identifier, and 1667 were admitted to the hospital prior to the date of surgery (Fig. 1). Patient, surgeon, and facility characteristics are presented in Table 1. For the procedure type, 14 % of the cohort underwent esophagectomy, 49 % underwent partial or total gastrectomy, and 37 % underwent distal pancreatectomy or pancreaticoduodenectomy.
Blood Transfusion
The overall rate of perioperative red blood cell transfusion was 32 %. The unadjusted blood transfusion rate varied according to procedure type from 22 % for esophagectomy to as high as 41 % for total gastrectomy. Among individual surgeons and hospitals that performed at least 10 cases during the study period, large variation in transfusion utilization was seen across both surgeons and hospitals. Unadjusted blood transfusion rates ranged from 0 to 82 % for individual surgeons and 0 to 64 % for individual hospitals. Using a test for trend, there was no significant change in the overall rate of transfusion observed over the 2001 to 2013 study period (p = 0.57).
Bivariate results of factors associated with blood transfusion are presented in Table 2. In addition to patient-level factors, several surgeon and hospital-level factors, including low surgeon procedure volume, low hospital procedure volume, non-academic hospital status, and rural hospital location, were significantly associated with higher blood transfusion utilization. After controlling for relevant covariates in a hierarchical mixed-effects multivariable analysis, the hospital-level factors of procedure volume, academic status, and location were no longer significant (Table 3). Low-volume surgeons were associated with 16 % higher odds of blood transfusion compared to high-volume surgeons.
After adjusting for these patient, surgeon, and hospital-level factors in the multivariable analysis, significant variation was still present among individual surgeons (p < 0.0001) and hospitals (p < 0.0001). Only 2 % of the surgeon-level variation was explained by surgeon procedure volume, and only 11 % of the hospital-level variation was explained by the hospital characteristics of hospital procedure volume, academic status, and hospital location. Of the remaining variation not explained by the multivariable model, 42 % was due to surgeon-level factors and 58 % due to hospital-level factors. After excluding 939 surgeons and 72 hospitals that performed less than 10 cases over the study period to reduce random statistical variation, 223 surgeons and 99 hospitals were evaluated for status as outliers using risk-adjusted observed/expected ratios. Among surgeons, 28 % were low outliers, 59 % were non-outliers, and 13 % were high outliers (Fig. 2). Among hospitals, 24 % were low outliers, 61 % were non-outliers, and 15 % were high outliers (Fig. 3).
Propensity Analysis
The propensity score for receipt of a blood transfusion had good predictive ability with a c-statistic of 0.74 (area under the receiver operating characteristic curve). All of the variables included in the propensity score model are listed in Table 3.
Infectious Complications
The overall rates of deep wound infection, pneumonia, and sepsis were 7.7, 8.2, and 4.5 %, respectively, for the entire study cohort. Receipt of a perioperative blood transfusion was associated with significantly higher unadjusted rates of each of the infectious complications, including deep wound infection (10.7 vs. 6.4 %), pneumonia (12.2 vs. 6.4 %), and sepsis (7.8 vs. 3.0 %). After adjusting for patient, operative, surgeon, and hospital factors as well as the propensity score during multivariable analysis, perioperative blood transfusion was independently associated with increased odds of deep wound infection (odds ratio [OR] = 1.64, 95 % CI = 1.43, 1.89), pneumonia (OR = 1.93, 95 % CI = 1.69, 2.22), and sepsis (OR = 2.34, 95 % CI = 1.96, 2.78) (Table 4).
Discussion
This study demonstrated that marked variation in perioperative RBC transfusion utilization persists across both surgeons and hospitals following elective upper gastrointestinal cancer resection. Thirteen percent of surgeons and 15 % of hospitals were considered high outliers for blood transfusion utilization. Furthermore, surgeon volume accounted for only 2 % of the variation between surgeons, and known hospital characteristics explained only 11 % of the variation between hospitals. In addition, no change in the overall rate of transfusion was observed over the 2001 to 2013 study period. These findings suggest that the wide variation in transfusion practices is most likely due to provider preferences or lack of standardized transfusion protocols. Unfortunately, this surgeon and hospital variation were not without major consequences to patients as blood transfusions were independently associated with postoperative deep wound infection, pneumonia, and sepsis.
Despite the creation of general practice guidelines by various healthcare organizations for the use of RBC transfusions several decades ago, several recent large studies investigating perioperative transfusion rates continue to show marked variation across hospitals in the USA.25 In fact, in a study by Bennett-Guerrero et al. including over 80,000 cases at 408 different institutions, a 7.7-fold difference in perioperative RBC transfusion usage between hospitals in 2008 was observed for coronary artery bypass graft surgery patients even after adjusting for patient risk factors.26 Similarly, Qian et al. demonstrated dramatic variation in RBC, fresh frozen plasma, and platelet transfusion utilization between 77 academic hospitals following approximately 80,000 cases of total hip replacement, colectomy, or pancreaticoduodenectomy performed between 2006 and 2010.27
Aside from the study by Qian et al., the current study is one of the first to investigate the variation in blood transfusion usage for surgical procedures outside of cardiac and orthopedic surgery. Furthermore, it is one of the first studies to analyze both surgeon and hospital-level variation. While most previous studies have focused solely on hospital-level variability, the current study found that 42 % of the unexplained variation in blood transfusion utilization resided at the surgeon level. To date, only small, single-hospital studies have specifically investigated surgeon variation in blood transfusion usage in the USA. Several studies by Ejaz et al. using an institutional prospective database have demonstrated variability between surgeons regarding perioperative blood transfusion utilization, indication for transfusion (“trigger”), and transfusion goal (“target”) in patients undergoing major gastrointestinal surgery.28 – 30 Using data from 2010 to 2013, the authors found that one in four patients who received an intraoperative blood transfusion had a hemoglobin level of 10 g/dL or more.28 Furthermore, they found significant differences in the mean hemoglobin level trigger and target across surgical services and individual surgeons for perioperative transfusion usage.29
Unfortunately, this wide variation is present despite the existence of numerous national evidence-based blood transfusion guidelines supporting restrictive use of RBC transfusions.2 , 9 , 31 These guidelines are largely based on multiple randomized clinical trials that have demonstrated equivalent or superior outcomes for restrictive use of blood transfusion with a hemoglobin threshold between 7 and 8 g/dL compared to liberal use protocols that utilize higher hemoglobin level transfusion triggers.32 – 36 In fact, some have argued for clinical trials using an even lower hemoglobin threshold of 5 or 6 g/dL.37 This push toward restrictive blood transfusion usage is due to a growing body of literature regarding adverse outcomes secondary to TRIM.
The immunologic effects of blood transfusions were first discovered in the late 1970s when Opelz and Terasaki described an improvement in kidney transplant graft survival in patients who received an increased number of blood transfusions.38 Since then, the paradigm of “blood must be good” has been seriously called into question as studies have begun establishing a causative mechanism between blood transfusions and infectious complications as a result of TRIM.39 – 41 The current study further establishes this association between blood transfusions and postoperative infections as RBC transfusions were independently associated with deep wound infection, pneumonia, and sepsis. A large study by Bernard et al. including over 125,000 general surgery patients from the National Surgical Quality Improvement Program (NSQIP) database had similar findings.3 The authors reported that intraoperative transfusion of packed RBCs was associated with increased rates of morbidity, surgical site infection, pneumonia, sepsis, and 30-day mortality. An even larger study by Ferraris et al. using NSQIP that included 941,496 noncardiac surgical cases demonstrated that even intraoperative transfusion of only 1 unit of packed RBCs was associated with increased odds of postoperative wound problems, pulmonary complications, renal dysfunction, sepsis, length of stay, and mortality.7
Given the strong association between blood transfusions and infectious complications, numerous studies have attempted to elucidate the exact mechanism behind this immunomodulatory phenomenon. Proposed reasons include decreases in the helper/suppressor T-lymphocyte ratio, killer cell function, efficacy of antigen presentation, or delayed-type hypersensitivity, suppression of blastogenesis, and the development of tolerance to specific antigens.39 , 42 , 43 While the exact mechanism remains unknown, randomized controlled trials have shown that modification of stored red blood cells, such as leukoreduction, can improve inflammatory responses and reduce the adverse effects of RBC transfusion.4 These trials have demonstrated a reduction in the incidence of postoperative infection by 30–71 % with the use of white blood cell reduction prior to the transfusion of packed RBCs in surgical patients.44 – 46 However, despite this evidence, there has been strong opposition by some physicians from academic blood banks against the Food and Drug Administration’s proposed plan for a universal leukocyte reduction mandate due to the high medical costs of leukoreduction.47 As a result, policies regarding white blood cell reduction remain at the institutional level. Furthermore, there is some evidence to suggest that other non-leukocyte mechanisms may also be involved in the development of TRIM.48
For these reasons, limiting unwarranted variation in blood transfusion usage through the adoption and implementation of institutional perioperative blood transfusion protocols remains the most effective method of reducing TRIM and subsequent risk of postoperative infection. According to the most recent National Blood Collection and Utilization Survey Report in 2011, only 27 % of reporting hospitals had institutional guidelines in place promoting restrictive use of postoperative transfusions.1 Future work should focus on adopting new quality improvement initiatives focusing on the creation of blood conservation programs at these institutions. This strategy would not only protect a scarce, life-saving resource when used appropriately but also reduce the risk of postoperative infectious complications.
Despite its potentially impactful findings, this study is not without limitations. First, the SPARCS database is comprised of administrative data that lacks detailed clinical information related to surgical technique, a comprehensive list of medical comorbidities, provider decision-making, and patient preferences. An additional limitation is that preoperative anemia was captured using administrative coding instead of from laboratory hemoglobin or hematocrit levels. Without preoperative laboratory values available, it is not known whether the provider was utilizing appropriate transfusion triggers consistent with the current evidence-based practice guidelines. Other pathologic- or tumor-related factors that might affect the need for blood transfusions are also not available in the database. Furthermore, while the data is abstracted from medical records by trained personnel, the possibility of ICD-9 miscoding error does exist. The date of transfusion and number of units of RBCs transfused are also not captured making it difficult to know whether the blood transfusion preceded the infectious complication or whether a dose–response relationship existed between the amount of blood transfused and the rate of infectious complications. However, previous studies have already established a causal mechanism and dose–response relationship between allogeneic blood transfusions and infectious complications.40 , 41 In addition, we utilized a propensity score to reduce potential selection bias with regard to which patients received a blood transfusion and their risk of an infectious complication.
Notwithstanding these limitations, this is one of the first studies to examine both surgeon-level and hospital variation using a large population-based database. Previous studies have either been single-institution studies or only investigated hospital-level variability in blood transfusion utilization. It is also one of the few large studies that have looked at variation in transfusion practices outside of cardiac and orthopedic surgery. Furthermore, the study is population-based which provides real world data regarding current transfusion practices at all non-Veteran Administration hospitals across New York State.
Conclusion
Significant variation in perioperative blood transfusion utilization following elective upper gastrointestinal cancer resection is present across both surgeons and hospitals. This variation is not explained by patient-level factors, surgical volume, or other known hospital characteristics, suggesting that it is largely due to provider preferences or lack of standardized transfusion protocols. The adoption and implementation of perioperative blood transfusion guidelines aimed at limiting unwarranted variation in transfusion practices are necessary to reduce the risk of infectious complications.
References
The 2011 National Blood Collection and Utilization Survey Report. Washington, DC: US Department of Health and Human Services; 2011.
Napolitano LM, Kurek S, Luchette FA, Corwin HL, Barie PS, Tisherman SA, Hebert PC, Anderson GL, Bard MR, Bromberg W, Chiu WC, Cipolle MD, Clancy KD, Diebel L, Hoff WS, Hughes KM, Munshi I, Nayduch D, Sandhu R, Yelon JA, American College of Critical Care Medicine of the Society of Critical Care M, Eastern Association for the Surgery of Trauma Practice Management W. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. Crit Care Med. 2009 Dec;37(12):3124–57.
Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009 May;208(5):931–7, 7 e1-2; discussion 8–9.
Grimshaw K, Sahler J, Spinelli SL, Phipps RP, Blumberg N. New frontiers in transfusion biology: identification and significance of mediators of morbidity and mortality in stored red blood cells. Transfusion. 2011 Apr;51(4):874–80.
Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R, Salloum R, Meredith UW, Osler TM. Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology. 2011 Feb;114(2):283–92.
Al-Refaie WB, Parsons HM, Markin A, Abrams J, Habermann EB. Blood transfusion and cancer surgery outcomes: a continued reason for concern. Surgery. 2012 Sep;152(3):344–54.
Ferraris VA, Davenport DL, Saha SP, Austin PC, Zwischenberger JB. Surgical outcomes and transfusion of minimal amounts of blood in the operating room. Arch Surg. 2012 Jan;147(1):49–55.
Cata JP, Wang H, Gottumukkala V, Reuben J, Sessler DI. Inflammatory response, immunosuppression, and cancer recurrence after perioperative blood transfusions. Br J Anaesth. 2013 May;110(5):690–701.
Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, Holcomb JB, Illoh O, Kaplan LJ, Katz LM, Rao SV, Roback JD, Shander A, Tobian AA, Weinstein R, Swinton McLaughlin LG, Djulbegovic B, Clinical Transfusion Medicine Committee of the A. Red blood cell transfusion: a clinical practice guideline from the AABB*. Ann Intern Med. 2012 Jul 3;157(1):49–58.
Goodnough LT, Johnston MF, Toy PT. The variability of transfusion practice in coronary artery bypass surgery. Transfusion Medicine Academic Award Group. JAMA. 1991 Jan 2;265(1):86–90.
Stover EP, Siegel LC, Parks R, Levin J, Body SC, Maddi R, D’Ambra MN, Mangano DT, Spiess BD. Variability in transfusion practice for coronary artery bypass surgery persists despite national consensus guidelines: a 24-institution study. Institutions of the Multicenter Study of Perioperative Ischemia Research Group. Anesthesiology. 1998 Feb;88(2):327–33.
Snyder-Ramos SA, Mohnle P, Weng YS, Bottiger BW, Kulier A, Levin J, Mangano DT, Investigators of the Multicenter Study of Perioperative I, Group MR. The ongoing variability in blood transfusion practices in cardiac surgery. Transfusion. 2008 Jul;48(7):1284–99.
Surgenor DM, Wallace EL, Churchill WH, Hao SH, Chapman RH, Poss R. Red cell transfusions in total knee and total hip replacement surgery. Transfusion. 1991 Jul-Aug;31(6):531–7.
Churchill WH, McGurk S, Chapman RH, Wallace EL, Bertholf MF, Goodnough LT, Kao KJ, Olson JD, Woodson RD, Surgenor DM. The Collaborative Hospital Transfusion Study: variations in use of autologous blood account for hospital differences in red cell use during primary hip and knee surgery. Transfusion. 1998 Jun;38(6):530–9.
Audet AM, Andrzejewski C, Popovsky MA. Red blood cell transfusion practices in patients undergoing orthopedic surgery: a multi-institutional analysis. Orthopedics. 1998 Aug;21(8):851–8.
Aquina CT, Kelly KN, Probst CP, Iannuzzi JC, Noyes K, Langstein HN, Monson JR, Fleming FJ. Surgeon volume plays a significant role in outcomes and cost following open incisional hernia repair. J Gastrointest Surg. 2015 Jan;19(1):100–10; discussion 10.
Aquina CT, Probst CP, Kelly KN, Iannuzzi JC, Noyes K, Fleming FJ, Monson JR. The pitfalls of inguinal herniorrhaphy: Surgeon volume matters. Surgery. 2015 May 30.
Silber JH, Romano PS, Rosen AK, Wang Y, Even-Shoshan O, Volpp KG. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007 Oct;45(10):918–25.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998 Jan;36(1):8–27.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997 Oct 15;127(8 Pt 2):757–63.
Kelly KN, Iannuzzi JC, Rickles AS, Garimella V, Monson JR, Fleming FJ. Laparotomy for small-bowel obstruction: first choice or last resort for adhesiolysis? A laparoscopic approach for small-bowel obstruction reduces 30-day complications. Surg Endosc. 2014 Jan;28(1):65–73.
Kelly KN, Fleming FJ, Aquina CT, Probst CP, Noyes K, Pegoli W, Monson JR. Disease severity, not operative approach, drives organ space infection after pediatric appendectomy. Ann Surg. 2014 Sep;260(3):466–71; discussion 72–3.
Iannuzzi JC, Rickles AS, Kelly KN, Rusheen AE, Dolan JG, Noyes K, Monson JR, Fleming FJ. Perioperative pleiotropic statin effects in general surgery. Surgery. 2014 Mar;155(3):398–407.
Aquina CT, Probst CP, Becerra AZ, Iannuzzi JC, Hensley BJ, Noyes K, Monson JR, Fleming FJ. Missed opportunity: Laparoscopic colorectal resection is associated with lower incidence of small bowel obstruction compared to an open approach. Annals of Surgery. 2015;(In Press).
Practice strategies for elective red blood cell transfusion. American College of Physicians. Ann Intern Med. 1992 Mar 1;116(5):403–6.
Bennett-Guerrero E, Zhao Y, O’Brien SM, Ferguson TB, Jr., Peterson ED, Gammie JS, Song HK. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA. 2010 Oct 13;304(14):1568–75.
Qian F, Osler TM, Eaton MP, Dick AW, Hohmann SF, Lustik SJ, Diachun CA, Pasternak R, Wissler RN, Glance LG. Variation of blood transfusion in patients undergoing major noncardiac surgery. Ann Surg. 2013 Feb;257(2):266–78.
Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Variation in triggers and use of perioperative blood transfusion in major gastrointestinal surgery. Br J Surg. 2014 Oct;101(11):1424–33.
Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Identifying variations in blood use based on hemoglobin transfusion trigger and target among hepatopancreaticobiliary surgeons. J Am Coll Surg. 2014 Aug;219(2):217–28.
Ejaz A, Frank SM, Spolverato G, Kim Y, Pawlik TM. Potential Economic Impact of Using a Restrictive Transfusion Trigger Among Patients Undergoing Major Abdominal Surgery. JAMA Surg. 2015 May 6.
Society of Thoracic Surgeons Blood Conservation Guideline Task F, Ferraris VA, Brown JR, Despotis GJ, Hammon JW, Reece TB, Saha SP, Song HK, Clough ER, Society of Cardiovascular Anesthesiologists Special Task Force on Blood T, Shore-Lesserson LJ, Goodnough LT, Mazer CD, Shander A, Stafford-Smith M, Waters J, International Consortium for Evidence Based P, Baker RA, Dickinson TA, FitzGerald DJ, Likosky DS, Shann KG. 2011 update to the Society of Thoracic Surgeons and the Society of Cardiovascular Anesthesiologists blood conservation clinical practice guidelines. Ann Thorac Surg. 2011 Mar;91(3):944–82.
Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999 Feb 11;340(6):409–17.
Lacroix J, Hebert PC, Hutchison JS, Hume HA, Tucci M, Ducruet T, Gauvin F, Collet JP, Toledano BJ, Robillard P, Joffe A, Biarent D, Meert K, Peters MJ, Investigators T, Canadian Critical Care Trials G, Pediatric Acute Lung I, Sepsis Investigators N. Transfusion strategies for patients in pediatric intensive care units. N Engl J Med. 2007 Apr 19;356(16):1609–19.
Hajjar LA, Vincent JL, Galas FR, Nakamura RE, Silva CM, Santos MH, Fukushima J, Kalil Filho R, Sierra DB, Lopes NH, Mauad T, Roquim AC, Sundin MR, Leao WC, Almeida JP, Pomerantzeff PM, Dallan LO, Jatene FB, Stolf NA, Auler JO, Jr. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010 Oct 13;304(14):1559–67.
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, Nemo G, Dragert K, Beaupre L, Hildebrand K, Macaulay W, Lewis C, Cook DR, Dobbin G, Zakriya KJ, Apple FS, Horney RA, Magaziner J, Investigators F. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011 Dec 29;365(26):2453–62.
Villanueva C, Colomo A, Bosch A, Concepcion M, Hernandez-Gea V, Aracil C, Graupera I, Poca M, Alvarez-Urturi C, Gordillo J, Guarner-Argente C, Santalo M, Muniz E, Guarner C. Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med. 2013 Jan 3;368(1):11–21.
Carson JL, Patel MS. Red blood cell transfusion thresholds: can we go even lower? Transfusion. 2014 Oct;54(10 Pt 2):2593–4.
Opelz G, Terasaki PI. Improvement of kidney-graft survival with increased numbers of blood transfusions. N Engl J Med. 1978 Oct 12;299(15):799–803.
Reddy SS, Leitman IM. Blood transfusions in the surgical patient: a gift of life, but at what cost? J Surg Res. 2013 May;181(2):216–8.
Blumberg N. Deleterious clinical effects of transfusion immunomodulation: proven beyond a reasonable doubt. Transfusion. 2005 Aug;45(2 Suppl):33S-9S; discussion 9S-40S.
Isbister JP, Shander A, Spahn DR, Erhard J, Farmer SL, Hofmann A. Adverse blood transfusion outcomes: establishing causation. Transfus Med Rev. 2011 Apr;25(2):89–101.
Hendrickson JE, Hillyer CD. Noninfectious serious hazards of transfusion. Anesth Analg. 2009 Mar;108(3):759–69.
Raghavan M, Marik PE. Anemia, allogenic blood transfusion, and immunomodulation in the critically ill. Chest. 2005 Jan;127(1):295–307.
Jensen LS, Kissmeyer-Nielsen P, Wolff B, Qvist N. Randomised comparison of leucocyte-depleted versus buffy-coat-poor blood transfusion and complications after colorectal surgery. Lancet. 1996 Sep 28;348(9031):841–5.
van de Watering LM, Hermans J, Houbiers JG, van den Broek PJ, Bouter H, Boer F, Harvey MS, Huysmans HA, Brand A. Beneficial effects of leukocyte depletion of transfused blood on postoperative complications in patients undergoing cardiac surgery: a randomized clinical trial. Circulation. 1998 Feb 17;97(6):562–8.
Tartter PI, Mohandas K, Azar P, Endres J, Kaplan J, Spivack M. Randomized trial comparing packed red cell blood transfusion with and without leukocyte depletion for gastrointestinal surgery. Am J Surg. 1998 Nov;176(5):462–6.
Thurer RL, Luban NL, AuBuchon JP, Silver H, McCarthy LJ, Dzik S, Stowell CP, Moore SB, Vamvakas EC, Armstrong W, Kanter MH, Jeter E, Becker J, Higgins M, Galel S, Kleinman S, Marshall CS, Newman R, Ocariz JA, Blackall D, Petz LD, Toy P, Oberman H, Siegel DL, Price TH, Slichter SJ. Universal WBC reduction. Transfusion. 2000 Jun;40(6):751–2.
Bernard A, Meier C, Ward M, Browning T, Montgomery A, Kasten M, Snow C, Manning E, Woodward J. Packed red blood cells suppress T-cell proliferation through a process involving cell-cell contact. J Trauma. 2010 Aug;69(2):320–9.
Grant Support
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aquina, C.T., Blumberg, N., Probst, C.P. et al. Significant Variation in Blood Transfusion Practice Persists following Upper GI Cancer Resection. J Gastrointest Surg 19, 1927–1937 (2015). https://doi.org/10.1007/s11605-015-2903-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2903-3